Abstract
Background
Excess body fat, localized adiposity, and cellulite represent important social problems. To date, techniques using radiofrequencies, cavitation and noncavitation ultrasound, and carbon dioxide have been studied as treatments for noninvasive body contouring. Ice-Shock Lipolysis is a new noninvasive procedure for reducing subcutaneous fat volume and fibrous cellulite in areas that normally would be treated by liposuction. It uses a combination of acoustic waves and cryolipolysis. Shock waves, used normally in the treatment of renal calculi and musculoskeletal disorders, are focused on the collagen structure of cellulite-afflicted skin. When used on the skin and underlying fat, they cause a remodeling of the collagen fibers, improving the orange-peel appearance typical of the condition. Cryolipolysis, on the other hand, is a noninvasive method used for the localized destruction of subcutaneous adipocytes, with no effects on lipid or liver marker levels in the bloodstream. The combination of the two procedures causes the programmed death and slow resorption of destroyed adipocytes.
Methods
In this study, 50 patients with localized fat and cellulite were treated with a selective protocol for the simultaneous use of two transducers: a Freezing Probe for localized fatty tissue and a Shock Probe for fibrous cellulite.
Results
The procedure significantly reduced the circumference in the treated areas, significantly diminishing fat thickness. The mean reduction in fat thickness after treatments was 3.02 cm. Circumference was reduced by a mean of 4.45 cm. Weight was unchanged during the treatment, and no adverse effects were observed. Histologic and immunohistochemical analysis confirmed a gradual reduction of fat tissue by programmed cell death. Moreover, the reduction in fat thickness was accompanied by a significant improvement in microcirculation, and thus, the cellulite. The safety of the method also has been highlighted because it is accompanied by no significant increase in serum liver enzymes or serum lipids.
Conclusion
The study aimed to observe the effects of the new technique in the treatment of localized fat associated with cellulite in order to assess adipose tissue alterations, cellular apoptosis, and levels of serum lipid or liver markers. The findings show that the action of Ice-Shock Lipolysis is a safe, effective, and well-tolerated noninvasive procedure for body contouring. In particular, the authors believe that this could be an ideal alternative to liposuction for patients who require only small or moderate amounts of adipose tissue and cellulite removal or are not suitable candidates for surgical approaches to body contouring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Excess body fat and localized adiposity represent great health problems frequently associated with dissatisfaction about body shape, altered self-esteem, and disadvantage in interpersonal relationships. The latter problem, often associated with being overweight, includes cellulite.
Cellulite is an alteration in the topography of the skin of the pelvic region, lower limbs, and abdomen. It is the irregular, dimpled-skin surface phenomenon that affects 85% to 98% of postadolescent woman of all races [1]. Cellulite, also called liposclerosis [2], edematofibrosclerotic panniculopathy [3], and gynoid lipodystrophy (GLD) [4], is an aesthetic alteration of the cutaneous surface, and many patients affected by it seek plastic surgery to improve their appearance.
Various cosmetic procedures and devices have been developed to remove or reduce unwanted local subcutaneous fat. Conventional fat removal is achieved surgically by lipectomy or liposuction [5]. Currently, they are by far the most common and effective procedure for body contouring and completely safe. However, it remains an invasive procedure.
Noninvasive alternatives to liposuction have been attempted for body contouring, with variable, if any, scientific demonstration of safety. Although lipoplasty is purported by some to be an excellent method for improving body contouring [6], others have reported increased skin dimpling after liposuction in patients with cellulite and localized fat deposits [7]. A few therapeutic options have been developed for the treatment of cellulite associated with localized fat deposits [8, 9] including bipolar radiofrequency (RF), infrared (IR) heat and pulsatile suction devices [10, 11], optical devices [12, 13], botanical extracts [14], mesotherapy [15], a combination of mesotherapy and phosphatidylcholine injections [16], and external ultrasound [17, 18]. Only some of these procedures have been approved by the U.S. Food and Drug Administration. In particular, novel applications using ultrasound without surgical intervention have been investigated for delivery of an energy signature through the skin to disrupt adipose tissue [19].
Cryolipolysis is a recent development in noninvasive lipoplasty whereby fat layer reduction is produced by selective destruction of fat cells [20]. This technique uses controlled cold exposure to obtain a gradual reduction of the subcutaneous fat layer without damage to other tissues. Fat cells, in fact, are much more sensitive to cold-induced apoptosis than other anatomic structures such as skin, dermis, vessels, nerves, and muscles [21].
The adipose tissue is placed in contact with iced plates using a pressure applicator that thermically “kills” fat without damaging the skin. The dead cells then are metabolically eliminated, exactly as occurs for the fat found in food. [22]. The positive sides of cryotherapy in terms of reduced body fat lead to a reduction in complications and risks related to plastic surgery procedures [23, 24].
On the other hand, extracorporeal shock waves (ESW) are electrical energy transformed by mechanical energy through the piezo effect. Shock waves have been used in the medical field since 1980 to treat lithiasic pathologies (for renal stone fragmentation) with the aim of destroying the targeted structures without damaging surrounding tissues [25].
In the mid-1980s, new studies opened ulterior horizons on the effective therapeutic potential of shock waves, particularly in the orthopedic field (pseudoarthrosis, tendinopathy) [26], for musculoskeletal diseases (calcaneal spur, tennis elbow, golf arm) [27] and for the cure of chronic soft tissue conditions [28] such as neuropathic ulcers of the foot [29] or burning [30]. Several studies have demonstrated that the biologic effects of ESW also are caused by the release of mediators, such as vascular endothelial growth factor (VEGF) [31], which significantly increase angiogenesis and local blood circulation [32]. Moreover, in aesthetic medicine, shock waves are used in painless methods for efficient contrast of beauty flaws and cellulite [33, 34].
This report describes a pilot study for a new noninvasive device that uses a combination of cryolipolysis and acoustic waves for body contouring through the reduction of localized fat deposits associated with cellulite in areas that normally would be treated by liposuction. Our study demonstrates, for the first time, that this new technology, termed Ice-Shock Lipoysis, provides a safe and effective noninvasive treatment for body contouring and cellulite.
Materials and Methods
Apparatus
The Proshockice apparatus (PromoItalia Group S.p.A, Naples, Italy) used in this study emits shock waves at a variable frequency (1 to 16 Hz), at a pressure variable from 50 to 500 Bar, and with impulses that have a duration of 8 ms. The temperature for cryolipolysis is variable, from +5 down to −5°C. The Proshockice device also is equipped with two probes: the Freezing Probe, which can be aimed at localized fat and can be used for vasoconstriction to accomplish vascular gymnastics, and the Shock Probe, which works on the fibrous component of fat and cellulite [32–35]. The use of the Proshockice device is innovative and has been patented as a combined technology termed Ice-Shock Lipolysis, which reduces subcutaneous fat volume and fibrous cellulite. For the transducer (which emits the shock waves) to transfer the waves, a conductive gel must be used (Fig. 1).
In Vivo Experiments
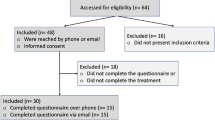
Patients
The study enrolled 50 patients (37 women and 13 men) 21 to 62 years of age, all with localized fat and cellulite. This cohort of patients was divided on the basis of the areas treated: abdomen, ankles, arms, buttocks, and outer thighs. Before assessment and treatment, all the patients received explanations about the procedure, after which they read and signed an informed consent. All the patients had a screening visit that included a physical examination and blood tests.
The exclusion criteria for this study ruled out osteoporosis; phlebitis and thrombophlebitis; patients carrying metallic fragments, articular prostheses, and intrauterine devices or pacemakers; pregnant women; patients with reduced nervous sensibility or neurologic pathologies; patients affected by obliterating arteriopathies; and patients affected by important inflammatory processes or neoplastic diseases.
During the period of treatment, it was very important to check that the patients drank at least 2 l of water per day and followed a moderated, hyperproteic diet. None of the patients underwent other slimming or aesthetic procedures (e.g., endermology, mesotherapy, radiofrequency) during the study.
Treatment and Evaluation Protocol
Each treatment was performed according to a default protocol. The duration of treatment was set, depending on the width of the area to be treated, from a minimum of 20 min to a maximum of 60 min. The treatment was performed by placing two transducers on the skin contemporaneously. In particular, the Freezing Probe was used for treating fatty tissue. Ice lipolysis was performed for 30 min in the sliding mode on the area with slow movements and with a temperature range set between 0 and −5°C. The Shock Probe was used with a conductive gel for 10 to 15 min of shock therapy.
For edematous cellulite, the Freezing Probe was used for 5 min of ice lypolysis (vascular gymnastic rather than apoptosis), and then the Shock Probe was used for a further 5 min of shock therapy. The cycle of ice lipolysis and shock therapy was repeated four times (20 min per side).
Finally, for fibrous cellulite, the Shock Probe and the Freezing Probe were used for 10 min of shock therapy and ice lipolysis (to create a lipolytic effect). The alternation of ice lipolysis and shock therapy was carried out for 30 min per side. The maximum total time was 1 h.
At least 15 days elapsed between sessions to guarantee hepatic recovery, even in the case of an eventual presence of pathologies in a subclinical phase. The evaluation period lasted 8 consecutive weeks at the frequency of one session every 15 days, for a mean total of 3.73 sessions. Before the start of the treatment program and at the end of the treatment, each subject’s height and weight were recorded, and perimetric measurements and photos were taken of the area treated. The perimetric measurements were performed with the patients standing up, feet apart often at the same distance, height marked from the floor up to the area of concern, and measurements taken just below the marking, making sure that the measuring tape was parallel to the floor. The photos were taken with the subject standing up, feet apart often at the same distance; camera distance from the subject always the same; camera height, angle, and focal length often the same; light always the same, with four flashlights in slave mode (2 behind the subject and 2 on either side of the camera); and four photos taken during each evaluation period (1 of the front, 1 of the back, and 1 each of the right and left sides).
Evaluation by the Surgeons and the Patient
The patients were examined by two surgeons not involved in the treatment. The follow-up period was 12 months, and the method of posttreatment evaluation was standardized. Clinical results were documented by pre- and postoperative digital photos. Results were evaluated at the end of the follow-up period by the operating surgeons, by the patients themselves, and by an independent medical observer.
The patient evaluation was obtained by a questionnaire with a scale of 0 to 5. A subjective evaluation of the skin’s compactness, the volumetric reduction of fat, the patient’s comfort, and the patient’s satisfaction with the outcome of the treatment was requested.
Pinch Test
Body fat was estimated by measuring skinfold thickness according to the guidelines published by the International Society for the Advancement of Kinanthropometry (ISAK). The measurement was performed at the level of the treated areas, and the pinch test was performed immediately before and after treatment and at the end of the follow-up period.
For the pinch test, the tester pinches the skin at the appropriate site to raise a double layer of skin and the underlying adipose tissue but not the muscle. The calipers are then applied 1 cm below and at right angles to the pinch, and a reading in millimeters is taken 2 s later. The mean of two measurements should be taken. If the two measurements differ greatly, a third measurement should be performed, with the median value taken.
Laboratory Evaluations
Hematic levels of cholesterol and triglycerides were constantly verified with specific reference to the low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol. In particular, samples were obtained 24 h before the beginning of the first session, immediately afterward (within 12 h), after 72 h, and after 7 days. An evaluation of hepatic markers (aspartate aminotransferase [AST]/glutamic-oxaloacetic transaminase [GOT], alanine aminotransferase [ALT]/glutamic-pyruvic transaminase [GPT], gamma-glutamyltranspeptidase [gamma-GT], total bilirubin, and albumin) was carried out before the beginning of the treatment, immediately afterward (within 12 h), after 72 h, after 7 days, and 15 days after the last session.
In Vitro Experiments
Histologic Staining and Immunohistochemistry
Skin biopsies were obtained by lipectomy rather than lipoaspiration to avoid any mechanical damage. Biopsies were taken from the region treated (right) and control biopsies from the region untreated (left) in the areas of interest: abdomen, ankles, arms, and buttocks. Biopsies were subdivided into two parts and either fixed in formalin or stored at −80°C. Tissues fixed in formalin were dehydrated in alcohol, clarified in xylene, and paraffin-embedded. Sections (5 μm thick) were stained with hematoxylin-eosin and Mallory’s trichrome stain and observed using light microscopy (Olympus BX41, Tokyo, Japan). Immunohistochemical analyses were performed with a Dako Cytomation kit (En Vision + System-HRP-AEC, Dako Italia, Milan, Italy) according to the manufacturer’s protocol. The antibodies used were anti-laminin and anti-type 4 collagen, all purchased from AbCam (Cambridge, UK). The remaining biopsies, kept at −80°C, were sectioned using a cryostat and stained with Oil Red-O, which can identify neutral fats, avoiding histologic artifacts.
Apoptosis Assay
Apoptosis analysis was performed with an Annexin V-FITC Apoptosis Detection Kit I (BDPharmigen, Buccinasco, Milan, Italy) according to the manufacturer’s protocol.
RNA Isolation and Polymerase Chain Reaction
Extraction of RNA was performed with TRI Reagent (Sigma, Milan, Italy). Synthesis of cDNA was led on total RNA by SuperScript II reverse transcriptase (Invitrogen, San Giuliano Milanese, Milan, Italy). The primer sequences used were GADPH: fw 5′-AGCCGCATCTTCTTTTGCGTC-3′; rw 5′-TCATATTTGGCAGGTTTTTCT-3′; ADIPONECTIN: fw 5′-CAACATTCCTGGGCTGTACT-3′; rw 5′-CCTGTGAAGGTGGAGTCATT-3′; LEPTIN: fw 5′-AAGCTTCAGGCTACTCCACA-3′; rw 5′-TGGAAGAGTGGCTTAGAGGA-3′; PPAR-γ: fw 5′-ACAGCAAACCCCTATTCCATGC-3′; RW 5′-ATTACGGAGAGATCCACGGAGC-3′.
Statistical Analysis
Differences were evaluated by the Wilcoxon test for paired continuous variables. The software used for statistical analysis was SPSS (SPSS, Chicago 17.0). A p value less than 0.05 was considered statistically significant.
Results
In Vivo Experiments
Clinical Study
The characteristics of the patients and the measurement data are summarized in Table 1. A total of 50 patients completed the study. The areas treated were the abdomen (14 patients), the thighs (18 patients), the arms (8 patients), the buttocks (6 patients), and the ankles (4 patients). Except for the patients treated in the abdominal area, all the patients had bilateral treatments at each session. All the patients resumed normal activities at completion of the sessions.
The median reduction in fat circumference at the end of the treatment was 6.86 cm for the abdomen, 5.78 cm for the thighs, 2.75 cm for the arms, 5 cm for the buttocks, and 2.25 cm for the ankles (Fig. 2a). The final reduction in fat thickness was significant compared with the measurement before the treatment (z = −5.384; p < 0.0001). The greatest reductions were observed in the thighs and in the abdomen, whereas the ankles showed the least reduction. The final reduction of fat thickness correlated positively with the baseline fat measurement.
a The study enrolled 50 patients. The areas treated included the abdomen (14 patients), the thighs (18 patients), the arms (8 patients), the buttocks (6 patients), and the ankles (4 patients). The median fat circumference reduction at the end of the treatment was 6.86 cm for the abdomen, 5.78 cm for the thighs, 2.75 cm for the arms, 5 cm for the buttocks, and 2.25 cm for the ankles (p < 0.05). b A pinch test showed that the median fat thickness reduction at the end of the treatment was 4.50 cm for the abdomen, 3.60 cm for the thighs, 2.10 cm for the arms, 4 cm for the buttock, and 1 cm for the ankles. (p < 0.05)
Using a pinch test, we confirmed that the fat-thickness reduction at the end of the treatment was 4.50 cm for the abdomen, 3.60 cm for the thighs, 2.10 cm for the arms, 4 cm for the buttock, and 1 cm for the ankles (Fig. 2b). No statistically significant difference in fat-thickness reduction between the men and the women was observed. In the subjects treated for fibrous cellulite, besides the reduction in centimeters, a modification of the cutaneous aspect with an attenuation of the “orange peel” skin effect was observed.
Interestingly, body weight remained constant throughout the treatment for all the patients, strongly suggesting that the fat-thickness reduction was due to the treatment. Improvements in body contour were visibly appreciable in all the patients at the end of the treatment, as supported also by the data from the subjective evaluations, which always showed a clear satisfaction of all the patients treated (score of 4 or 5).
The procedure was well tolerated by all the patients. Figure 3a depicts an example of body contouring, and Fig. 3b shows an example of body contouring after 12 weeks (Fig. 3a and b). Another example of body contouring is depicted in Fig. 3c–e. A clinically apparent reduction in the fat layer can be noted.
Clinical evidence for the use of Ice-Shock Lipolysis technology. a Body contouring immediately after the first treatment highlighting a reduction of 1 cm in waist circumference after the first treatment. b An example of body contouring after 12 weeks. c, d, e Other cases of body contouring at the end of treatment
Erythema was observed immediately after ice-shock treatments but was rapidly resolved. To the touch, the skin of the treated area was cold but not icy.
Cholesterol and triglyceride levels were mildly increased after the treatments, but remained within normal limits (Fig. 4a). Consistently, evaluation of the hepatic markers (GOT, GPT, gamma-GT, total bilirubin, and albumin) demonstrated no alterations in hepatic function (Fig. 4b).
a Average values of cholesterol, triglycerides, high-density lipoprotein (HDL) and low-density lipoprotein (LDL). No significant change over time was seen. In addition, mean values remained within the reference range. b Average values of aspartate aminotransferase (AST)/glutamic-oxaloacetic transaminase (GOT), alanine aminotransferase (ALT)/glutamic-pyruvic transaminase (GPT)/gamma-glutamyltranspeptidase (gamma-GT), bilirubin, and albumin. No significant change occurred over time, and the mean values remained within the reference range
Finally, no severe adverse events were reported during or after the procedures. In particular, no paresthesias, hematomas, ecchymoses, or edemas were noted or reported.
In Vitro Experiments
Histologic Staining, Immunohistochemistry, Apoptosis Assays, and Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR)
Histologic analysis of tissue demonstrated that Ice-Shock Lipolysis technology induced the death of adipocytes. In fact, evidence showed that an inflammatory process (Fig. 5b) stimulated by adipocyte apoptosis occurred. The adipocytes appeared irregularly shaped, with alterations (Fig. 5c) confirmed by Oil-Red-O staining (Fig. 5d), compared with the nontreated regions (Fig. 5a). Oil-Red-O staining showed that many of these lipids remain trapped within the subcutaneous adipose tissue because of slow absorption.
a Abdominal adipose biopsy of a nontreated region (Mallory’s trichrome stain, original magnification, ×100). b Abdominal adipose biopsy of a patient treated with Ice-Shock Lipolysis technology. At this level, there is evidence of an inflammatory process (hematoxylin-eosin staining, original magnification, ×100). c Same sample with Mallory’s trichrome stain (original magnification, ×100) in which the adipocytes appear irregularly shaped and with alterations. d Sample of treated abdominal adipose biopsy. Oil-Red-O staining shows that the content of the fat cells (lipids) remains trapped in the subcutaneous tissue (original magnification, ×200)
In addition, histologic staining showed no alteration of the skin (no ulcers or necrosis of the epidermis or dermis) or any septa of the subcutaneous connective tissue that were irregular and perpendicular to the surface with formation of chambers in which fat lobules could accumulate (Fig. 6a and b). We observed a complete derangement of fat tissue, with selective removal of adipocytes, reduction of thickness, and widespread shrinkage of collagen fibers in a parallel rearrangement (Fig. 6c). There was evident neovascularization of the subcutaneous tissue (Fig. 6d and e) with respect to the nontreated regions (Fig. 6f).
a Skin biopsy of a patient treated with Ice-Shock Lipolysis technology. At this level, no alteration of the skin (ulcers, necrosis of the epidermis or dermis) is visible (Mallory’s trichromie stain, original magnification, ×100). b Skin and subcutaneous tissue biopsy of a nontreated region. The septa of the subcutaneous connective tissue are irregular and perpendicular to the surface (hematoxylin-eosin staining, original magnification, ×200). c Skin and subcutaneous biopsy of a treated patient showing reduction of thickness and widespread shrinkage of collagen fibers associated with the septa parallel to the surface (anti-laminin immunohistochemistry staining, original magnification, ×100). d Subcutaneous tissue biopsy of a treated patient showing evidence of neovascularization (anticollagen 4 immunohistochemistry staining, original magnification, ×100). e Close-up of neovascularization in the subcutaneous tissue of a treated patient (anticollagen 4 immunohistochemistry staining, original magnification, ×200). f Skin and subcutaneous tissue biopsy of a nontreated region showing is no evidence of neovascularization (anticollagen 4 immunohistochemistry staining, original magnification, ×100). The positive control is provided by the epidermal basal membrane staining positively for type 4 collagen
Adipocytes were exposed to temperatures ranging from −5°C to +5°C for 1 h. We used the Annexin V-FITC to evaluate the degree of cell membrane destruction. We found that adipocytes cooled to −5°C, 0°C, or +5°C were completely destroyed, either by an active mechanism of necrotic death or with a mechanism that triggers programmed death by apoptosis (Fig. 7a and b). In addition, the shock waves amplified the phenomenon of cellular death. The absence of molecular alterations of adipose tissue was confirmed by RT-PCR (Fig. 7c).
Propidium iodide (PI) and V-FITC annexin staining for evaluation of apoptosis. a In the adipose tissue samples cooled to +5°C, viable cells are about 77% of the total cell population tested. Whereas 14% of the cells are totally apoptotic (early and late apoptosis), only 8% of the cells are necrotic. b In the adipose tissue samples cooled to −5°C, 25% of the cells are in total apoptosis, 3% of the cells are in necrosis, and the remaining 70% are viable. c Representative figure of reverse transcriptase-polymerase chain reaction (RT-PCR) showing mRNA transcript expression of adiponectin (columns 2 and 3), leptin (columns 4 and 5), and PPAR-γ (columns 6 and 7)
Discussion
Ice-Shock Lipolysis technology is a noninvasive procedure for the selective reduction of fat cells and for effective treatment of cellulite through remodeling of skin collagen. This procedure significantly reduces the circumference in treated areas by a reduction in fat thickness. Importantly, in this study, the reduction in fat thickness could not be ascribed to weight loss because no statistically significant weight reduction was observed in any of the patients. In fact, using a pinch test, we confirmed that the fat thickness in the entire area was at least 2 cm.
Our clinical studies have shown efficacy in the treatment of excess back fat, flank fat, and abdominal fat. The results were most visible in patients with discrete localized fat. The Ice-Shock Lipolysis technology does not appear to be as effective for obese patients or patients with excess skin laxity. Beyond reduction of subcutaneous fat, an ideal therapy for cellulite should ensure skin shrinkage and improve its quality.
In our case of Ice-Shock Lipolysis treatment, we could ascertain direct or indirect signs showing mechanical destruction of fat tissue and remodeling of the skin’s collagen on any one of the histologic slices. Histologic analysis confirmed a selective and gradual reduction of fat tissue by programmed death (apoptosis) triggered by inflammation. Hematoxylin-eosin-stained sections showed a marked increase in the numbers of lymphomonocyte inflammatory cells. Infiltrating granulocytes were rare. Moreover, irregularly sized necrotic fat cells were surrounded by a thick progressive fibrosis.
Acoustic pulses stimulate microcirculation in subcutaneous tissue and improve the existing structural and metabolic disorders to reduce visible signs of cellulite. Ice-Shock Lipolysis not only improves the stability of connective tissue and the skin’s structure and causes a reduction in adipose tissue but also stimulates metabolic activity in the subcutaneous fat tissue. In fact, neoangiogenesis improves the flow of oxygen and nutrients and markedly augments lymphatic drainage [36].
The mediators of inflammation trigger phagocytosis. Over time, this leads to a slow removal of destroyed adipocytes, with no consequent effect on lipid levels in the bloodstream and liver. In fact, although cholesterol levels were mildly increased after the treatments, they remained within normal limits. Moreover, assessment of hepatic function showed no changes in markers of liver function, suggesting that fat released from treated areas was cleared by the natural fat metabolism pathways. The stability of lipid profiles during treatment and the absence of liver marker changes suggest that our technology is a safe technique with no detectable adverse effects. Fat release from treated areas is cleared by the natural fat metabolism pathways. Liposuction, however, causes a rapid destruction of fat cells and a rapid release of lipids, as confirmed by a decreased concentration in the bloodstream [37], and an increased hepatic sequestration that can cause an increase in the indices of hepatic cytolysis. Regarding the results obtained using Ice-Shock Lipolysis technology, the content of the fat cells remained trapped in the subcutaneous adipose tissue, as evidenced by Oil-Red-O staining, and were absorbed very slowly.
The exact mechanism of Ice-Shock Lipolysis has been elucidated. The adipose cells undergo massive cellular stress, as evidenced by Annexin V-FITC and propidium iodide (PI) staining commonly used to evaluate necrosis and apoptosis. Indeed, annexin binds to phosphatidylserine residues only when it is exposed on the outer leaflet of the plasma membrane, whereas PI binds to DNA only when the cell is dead. Depending on the percentage of annexin binding to phosphatidylserine and of PI binding to DNA, we evaluate that the number of apoptotic cells (early and late) is higher than the cells undergoing necrosis, confirming that the cryolysis associated with shock waves is to apoptosis. Additionally, molecular studies showed no alteration of adiponectin, leptin, or peroxisome proliferator-activated receptor-gamma (PPAR-γ) transcripts. No change was evident in the transcript, underscoring the safety of the technology used.
Visual and photographic evaluations have shown measurable fat layer reduction and skin shrinkage in our clinical studies. These effects can be corroborated by the subjective comments of the patients, with improvement not immediate but occurring over the course of 2 to 3 months (12 weeks).
Ice-Shock Lipolysis is not indicated for obese patients or those with great skin laxity. It is indicated for patients with normal weight who have fatty deposits and cellulite. In fact, liposuction still is not a recommended treatment for cellulite, in part because cellulite adipose tissue is very close to the surface of skin, with only a thin layer of dermis overlying it. It is therefore important for clinicians to select patients carefully and to educate them regarding their expected outcomes and potential limitations.
One of the most important aspects that distinguishes Ice-Shock Lipolysis from liposuction is the lower number of drawbacks. Indeed, Ice-Shock Lipolysis was well tolerated, with the great majority of patients reporting that they experienced minimal or no discomfort during or after the procedures. In particular, no paresthesias, hematomas, ecchymoses, or edemas were noted, and also no hyper- or hypopigmentation. Moreover, the procedures were relatively rapid, noninvasive, and painless, and did not necessitate anesthesia or tumescent solution. Physical examination and laboratory assessment throughout the study period showed no clinically significant changes. Moreover, this procedure did not cause any limitations in work or social activities.
Our clinical studies helped to determine the full potential and efficacy of the Proshockice apparatus. It provides a unique method for noninvasive reduction of fat and for improved remodeling of the skin’s collagen that is best suited for patients of normal weight with discrete fat bulges and cellulite. For these patients, Ice-Shock Lipolysis appears to be a promising new technology offering an effective procedure performed in a safe and gradual manner.
Conclusion
The action of the Proshockice apparatus is safe, effective, and well tolerated as a procedure for body contouring. In particular, we believe that this could be an ideal noninvasive alternative to conventional liposuction for patients who require only small or moderate removal of adipose tissue and cellulite or who are not suitable candidates for surgical approaches to body contouring. Further studies are required to assess whether serial treatments produce incremental fat reduction and whether greater fat reduction can be achieved in conjunction with weight loss strategies or other aesthetic methods to treat obesity-related fat deposits.
References
Smalls LK, Lee CY, Whitestone J, Kitzmiller WJ, Wickett RR, Visscher MO (2005) Quantitative model of cellulite: three-dimensional skin surface topography, biophysical characterization, and relationship to human perception. J Cosmet Sci 56:105–120
Browse NL, Jarrett PE, Morland M, Burnand K (1977) Treatment of liposclerosis of the leg by fibrinolytic enhancement: a preliminary report. Br Med J 13:434–435
Binazzi M, Grilli-Cicioloni E (1977) A proposito della cosidetta cellulite e della dermato-panniculopatia edemato fibrosclerotica. Ann It Derm Clin Sper 31:121–125
Smalls LK, Hicks M, Passeretti D, Gersin K, Kitzmiller WJ, Bakhsh A, Wickett RR, Whitestone J, Visscher MO (2006) Effect of weight loss on cellulite: gynoid lypodystrophy. Plast Reconstr Surg 118:510–516
Flynn TC, Coleman WP II, Field LM, Klein JA, Hanke CW (2000) History of liposuction. Dermatol Surg 26:515–520
Gasparotti M (1992) Superficial liposuction: a new application of the technique for aged and flaccid skin. Aesthetic Plast Surg 16:141–152
Svedman KJ, Coldiron B, Coleman WP III, Cox SE, Jacob C, Lawrence N, Kaminer M, Narins RS (2006) ASDS guidelines of care for tumescent liposuction. Dermatol Surg 32:709–716
Avram MM (2004) Cellulite: a review of its physiology and treatment (review). J Cosmet Laser Ther 6:181–185
Khan MH, Victor F, Rao B, Sadick NS (2010) Treatment of cellulite: part II. Advances and controversies. J Am Acad Dermatol 62:373–384
Wanitphakdeedecha R, Manuskiatti W (2006) Treatment of cellulite with a bipolar radiofrequency, infrared heat, and pulsatile suction device: a pilot study. J Cosmet Dermatol 5:284–288
Alster TS, Tanzi EL (2005) Cellulite treatment using a novel combination radiofrequency, infrared light, and mechanical tissue manipulation device. J Cosmet Laser Ther 7:81–85
Alexiades-Armenakas M (2007) Laser- and light-based treatment of cellulite. J Drugs Dermatol 6:83–84
Alster TS, Tehrani M (2006) Treatment of cellulite with optical devices: an overview with practical considerations (review). Lasers Surg Med 38:727–730
Hexsel D, Orlandi C, Zechmeister do Prado D (2005) Botanical extracts used in the treatment of cellulite (review). Dermatol Surg 31:866–872 discussion 872
Rose PT, Morgan M (2005) Histological changes associated with mesotherapy for fat dissolution. J Cosmet Laser Ther 7:17–19
Rotunda AM, Kolodney MS (2006) Mesotherapy and phosphatidylcholine injections: historical clarification and review. Dermatol Surg 32:465–480
Silberg BN (1998) The use of external ultrasound assist with liposuction. Aesth Surg J 16:284
Zocchi ML (1996) Ultrasonic-assisted lipoplasty. Clin Plast Surg 23:575
Ferraro GA, De Francesco F, Nicoletti G, Rossano F, D’Andrea F (2008) Histologic effects of external ultrasound-assisted lipectomy on adipose tissue. Aesthetic Plast Surg 32:111–115
Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowski D, Anderson RR (2008) Selective cryolysis: a novel method of noninvasive fat removal. Lasers Surg Med 40:595–604
Zelickson B, Egbert BM, Preciado J, Allison J, Springer K, Rhoades RW, Manstein D (2009) Cryolipolysis for noninvasive fat cell destruction: initial results from a pig model. Dermatol Surg 35:1462–1470
Klein KB, Zelickson B, Riopelle JG, Okamoto E, Bachelor EP, Harry RS, Preciado JA (2009) Noninvasive cryolipolysis for subcoutaneous fat reduction does not affect serum lipid levels or liver function tests. Lasers Surg Med 41:789–790
Avram MM, Harry RS (2009) Cryolipolysis for subcutaneous fat layer reduction. Lasers Surg Med 41:703–708
Nelson AA, Wasserman D, Avram MM (2009) Cryolipolysis for reduction of excess adipose tissue. Semin Cutan Med Surg 28:244–249
Skolarikos A, Mitsogiannis H, Deliveliotis C (2010) Indications, prediction of success, and methods to improve outcome of shock wave lithotripsy of renal and upper ureteral calculi (review). Arch Ital Urol Androl 82:56–63
Haupt G (1997) Use of extracorporeal shock waves in the treatment of pseudoarthrosis, tendinopathy, and other orthopaedic diseases (review). J Urol 158:4–11
Sems A, Dimeff R, Iannotti JP (2006) Extracorporeal shock wave therapy in the treatment of chronic tendinopaties (review). J Am Acad Orthop Surg 14:195–204
Speed CA (2004) Extracorporeal shock-wave therapy in the management of chronic soft-tissue conditions (review). J Bone Joint Surg Br 33:40–48
Moretti B, Notarnicola A, Maggio G, Moretti L, Pascone M, Tafuri S, Patella V (2009) The management of neuropathic ulcers of the foot in diabetes by shock wave therapy. BMC Musculoskelet Disord 27:10–54
Arnò A, Garcia O, Hernan I, Sancho J, Acosta A, Barret JP (2010) Extracorporeal shock waves: a new nonsurgical method to treat severe burns. Burns 36:844–849
Yip HK, Chang LT, Sun CK, Youssef AA, Sheu JJ, Wang CJ (2008) Shock wave therapy applied to rat bone marrow-derived mononuclear cells enhances formation of cells stained positive for CD31 and vascular endothelial growth factor. Circ J 72:150–156
Mittermayr R, Hartinger J, Antonic V, Meini A, Pfeifer S, Stojadinovic A, Schaden W, Redi H (2011) Extracorporeal shock wave therapy (ESWT) minimizes ischemic tissue necrosis irrespective of application time and promotes tissue revascularization by stimulating angiogenesis. Ann Surg 253:1024–1032
Kuhn C, Angehrn F, Sonnabend O, Voss A (2008) Impact of extracorporeal shock waves on the human skin with cellulite: a case study of an unique instance. Clin Interv Aging 3:201–210
Angehrn F, Kuhn C, Voss A (2007) Can cellulite be treated with low-energy extracorporeal shock wave therapy? (review). Clin Interv Aging 2:623–630
Chua KJ, Chou SK, Ho JC (2007) An analytical study on the thermal effects of cryosurgery on selective cell destruction. J Biomech 40:100–116
Siems W, Brenke R, Sattler S, Christ C, Novak P, Daser A (2008) Improvement in skin elasticity and dermal revitalization in the treatment of cellulite and connective tissue weakness by means of Extracorporeal Pulse Activation Therapy: EPAT. Aesthet Surg J 28:538–544
Ybarra J, Blanco-Vaca F, Fernandez S, Castellvì A, Bonet R, Palomer X, Ordonez-Llanos J, Trius A, Vila-Rovira R, Perez A (2008) The effects of liposuction removal of subcutaneous abdominal fat on lipid metabolism are independent of insulin sensitivity in normal-overweight individuals. Obes Surg 18:408–414
Acknowledgments
The authors thank Professor Gianpaolo Papaccio, Department of Experimental Medicine, Section of Histology and Embryology, Second University of Naples, for laboratory technical support. The authors thank Michael V. G. Latronico, Scientific and Technological Park, Casa di Cura MultiMedica, for English language and grammatical technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferraro, G.A., De Francesco, F., Cataldo, C. et al. Synergistic Effects of Cryolipolysis and Shock Waves for Noninvasive Body Contouring. Aesth Plast Surg 36, 666–679 (2012). https://doi.org/10.1007/s00266-011-9832-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-011-9832-7