Abstract
Laser therapy has proved effective in the treatment of different tissue injuries but little is known about its effect on the testis. The aim of this review was to synthesize research on the in vivo effect of low-level laser therapy on the seminiferous epithelium. A search was performed in the PubMed/Medline, Scopus, Web of Science, and LILACS databases. The initial search retrieved 354 references, and five articles that met the eligibility criteria were selected. In general, the studies showed that laser therapy exerted a positive effect on the germ cell population; however, there was considerable variation in the laser parameters, as well as in the experimental models and methods of tissue analysis used. In conclusion, further studies determining the biostimulation parameters of laser therapy in the testis are necessary in order to provide a basis for the possible application of this technique to the restoration of the human seminiferous epithelium and consequent treatment of some male reproductive disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infertility is generally defined as the inability of a man or a woman to conceive after 12 months of unprotected intercourse. This condition affects up to 15% of the world’s population, and a male factor contributes to 50% of cases [1]. According to Agarwal et al. [2], at least 30 million men worldwide are considered infertile, with a higher incidence in Eastern Europe and Africa. However, due to factors such as the arbitrary attribution of infertility to women and the refusal of many men to undergo fertility assessment, it is speculated that this number is an underestimation of the true rate of global male infertility.
Several factors are related to impaired male fertility, including urinary tract infections, epididymal or ductal obstruction, hormonal imbalances (FSH/LH and testosterone), testicular trauma, immunological factors, chemotherapy/radiotherapy, and diabetes. Exposure to chemical products—especially nematocides, organophosphates, estrogen, benzene, welding fumes, zinc, lead, cadmium, and mercury—can have antispermatogenic effects. Several social drugs such as tobacco, alcohol, marijuana, and narcotics are potentially antispermatogenic, although their frequent use is generally necessary for the manifestation of adverse effects [3, 4]. In addition, various genetic causes responsible for 10 to 15% of cases of male infertility have been well established [5], including chromosome anomalies and mutations in a single gene that, at different levels, influence many physiological processes involved in male reproduction such as hormone homeostasis, spermatogenesis, and sperm quality [6]. Finally, there are cases in which the cause of infertility is not identified. These cases are classified as idiopathic [7].
An increase in scrotal temperature, although within the physiological range, can also negatively affect sperm quality [8]. It is estimated that 1 °C above the ideal temperature range can reduce spermatogenesis by 14% and, consequently, the production of spermatozoa [9]. Several environmental and occupational events can cause heating of the testes [10, 11]. Warm environments, tight clothing, and the use of laptops near the testes and cycling, among others, are events that cause occasional increases in testicular temperature [12]. Conditions such as varicocele, cryptorchidism, episodes of fever, and obesity can compromise testicular thermoregulation, with long-term and permanent impairment of spermatogenesis. The harmful effects of heat exposure on sperm parameters and male fertility tend to accumulate with repeated exposure over time [13].
Several studies confirm that diabetes has deleterious effects on testicular microstructure. Ebokaiwe et al. [14] showed that type 1 diabetes mellitus induced by streptozotocin in a murine model causes alterations in the testes, such as degeneration of the seminiferous tubular content (spermatogenic cells) and loss or atrophy of Leydig cells in adjacent interstitial areas. Moreover, Khaneshi et al. [15] demonstrated a reduced tubular diameter in streptozotocin-diabetic rats, as well as a smaller cell population in seminiferous tubules and atrophy of Leydig cells.
Genetic factors that specifically affect the protection and quality of spermatozoa should also be considered. Alterations in genes that regulate sperm production and quality are the main factors of male infertility. Some studies suggest that about 10% of cases of male infertility result from acrosomal problems (particularly genetic). The acrosome is a membrane that covers the spermatozoon (like a cap) and that contains enzymes which are critical for penetration of the oocyte. It was demonstrated that pregnancy is compromised if 7% (or more) of spermatozoa exhibit acrosome abnormalities [13].
Laser therapy or low-level laser therapy (LLLT) consists of the application of light in continuous or pulsed wave modes within the near-infrared range (600 to 1100 nm) in an attempt to promote tissue repair and analgesia and to reduce inflammation [16]. It is a noninvasive therapy that uses energy densities and wavelengths that can easily penetrate tissues, with consequent effects of photobiomodulation on cells and tissues of different layers [17].
Different mechanisms of LLLT that elicit responses at the molecular, cellular, and tissue level and result in cell proliferation and tissue repair have been reported in the literature, including an increase in metabolism, mitochondrial activity, proliferation, migration, adhesion, differentiation, extracellular matrix secretion, and mineralization, as well as the inhibition of apoptosis [18]. At the mitochondrial level, various experiments have shown that light stimulation acts mainly on cytochrome c oxidase, an enzyme of the electron transport chain complex, increasing the mitochondrial membrane potential which, in turn, leads to an increase in the synthesis of adenosine triphosphate (ATP), cyclic adenosine monophosphate (cAMP), and reactive oxygen species [19]. In parallel, there is an increase in the activation of different growth factors, in the synthesis of nitric oxide, RNA, DNA, and proteins, and in intracellular calcium concentrations [20].
The in vitro application of LLLT to male germ cells is well described in the literature and focuses on improving the quality of sperm parameters in semen samples. Studies also report an increase in ATP levels and in influx of calcium through Ca2+ pumps which, in turn, has a positive impact on sperm motility [21, 22]. On the other hand, direct in vivo application of LLLT to germinal tissue in order to promote cell proliferation and to reverse possible infertility has great potential but has been little explored. Therefore, the aim of this systematic review was to describe the effects of LLLT on the biostimulation of progenitor cells of spermatozoa, critically evaluating the evidence of laser application during spermatogenesis.
Methods
The present study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [23]. Specific research questions were formulated based on the following criteria: population, intervention, control, and outcome (PICO). The key question of our systematic review was “What is the effect of low-level laser therapy on the seminiferous epithelium?”
Databases
An electronic search was performed in four databases: PubMed/Medline, LILACS (Latin American and Caribbean Health Sciences Literature), Scopus, and Web of Science. All searches were completed on 1 February 2020.
Search strategy
Studies were identified using the following main search terms on the topics investigated, which were combined by the Boolean operators “AND” and “OR”: light therapy, laser therapy, photobiomodulation, low level laser therapy, laser radiation, spermatogenesis, testicle, sperm, testes, male reproduction, male fertility, and male infertility.
Inclusion and exclusion criteria
All articles representing primary studies that evaluated the histological arrangement of the testes in animals or humans submitted to low-level laser irradiation and reported the photobiomodulation parameters and experimental design were eligible. Of these, in vivo studies that applied LLLT to the testes and evaluated possible morphological alterations in the internal structure of the seminiferous tubules were selected. There was no restriction regarding the experimental model.
All studies that were written in non-Latin alphabet (Russian or Chinese) were excluded. In addition, in vitro studies, studies that did not use a low-level laser (near infrared), studies in which the laser was not applied to the testis, and studies that did not measure the biostimulatory effects of laser irradiation on testicular tissue were excluded. Review articles were also excluded.
Data extraction
The following data were extracted from the selected articles: author and year of publication; animal model used; sample size; induction or not of injury; type of laser, power, and wavelength used; dose and duration of irradiation; interval after irradiation; parameters analyzed; and main outcomes obtained.
Risk of bias assessment and analysis of the quality of included studies
The Cochrane Collaboration tool for assessing the risk of bias was used to evaluate the quality of the studies included in this systematic review [24]. In summary, the reviewers considered the following bias domains: (I) selection bias, (II) performance bias, (III) detection bias, (IV) attrition bias, and (V) other bias. These items were then scored as adequate (+), inadequate (−), or unclear (?) in each study. Based on these domains, the risk of bias was classified as (I) low risk of bias if all criteria were met, (II) intermediate risk of bias if one or more criteria were partially met, or (III) high risk of bias if one or more criteria were not met.
Results
Selection of the studies
The initial search retrieved 102 articles from the PubMed database, 96 from Scopus, 108 from Lilacs, and 48 from Web of Science, totaling 354 articles (Fig. 1). Duplicate articles were eliminated, and 163 studies remained. After analysis of the titles and abstracts, 17 studies were selected for full-text reading. Twelve of these articles were excluded, five because they were reviews, two because they were published in Russian, two because they only evaluated testosterone levels after laser application, and three because they only evaluated the effect of laser irradiation on sperm parameters. Thus, five articles remained for analysis.
Characteristics of the studies
As can be seen in Table 1, there was significant variation in the animal models used across the studies; three used albino Sprague Dawley rats [25,26,27], one used sheep [28], and one used Syrian mice [29]. The preference for larger animals can be explained by the fact that the study also aimed to evaluate the effects of LLLT on the ejaculate [28]. Three studies used intact testicular tissue [25,26,27], while the other two evaluated the effect of laser therapy in an animal model of thermal injuries [28] or in animals with streptozotocin-induced diabetes [29].
All studies used a diode laser operating in the infrared spectrum from 808 to 904 nm at a power ranging from 1.08 mW to 6.5 W. The total amount of energy deposited in the target tissue was the same in three articles (doses of 28 and 46 J/cm2) [25,26,27] but was different in the other two. Alves et al. [28] used doses of 28 and 56 J/cm2 and Dadras et al. [29] of 0.2 and 0.03 J/cm2. The preference of using small doses at fixed intervals instead of a single larger dose was the strategy adopted in all studies. Bermúdez et al. [25, 26] and Taha and Valojerdi [27] applied doses of 1.87 J/cm2 (G2: 28.05 J/cm2) and 3.12 J/cm2 (G3: 46.8 J/cm2), respectively, once a day for 15 days. On the other hand, Alves et al. [28] studied decreasing doses (from 5 to 2 J/cm2 in one group and from 10 to 4 J/cm2 in the other), with irradiation every 48 h for 15 days. Finally, Dadras et al. [29] applied fixed doses (0.2 and 0.03 J/cm2), three times per week for 3 weeks.
Table 2 shows the parameters analyzed, intervals after irradiation, and the main outcomes of each study. The two articles of Bermúdez et al. [25, 26] were methodologically similar in terms of both the method applied and the parameters analyzed, and only differed in terms of the interval after irradiation. Both studies investigated the effect of laser radiation on rat germ cells by cytophotometric quantification of the nuclear DNA content in testicular sections 24 h [25] or 15 days [26] after irradiation. In the two studies, 45 male albino Sprague Dawley rats were divided into three groups of 15 animals each. Group 1 was not irradiated (control), and groups 2 and 3 were exposed to doses of 28.05 and 46.8 J/cm2, respectively. The data of the two studies revealed an increase in the DNA content of germ cells exposed in vivo to LLLT, especially in the group irradiated with 28.05 J/cm2. The sensitivity of germ cells to laser irradiation appeared to be related to their stage of differentiation and to the radiation energy applied, with spermatogonia being the most sensitive. In all cases, the lowest dose induced the greatest alteration.
Taha and Valojerdi [27] investigated the immediate effects of laser irradiation on quantitative and qualitative characteristics of the seminiferous epithelium and on the ultrastructure of germ and Sertoli cells in the irradiated testes. The authors used the same method as Bermúdez et al. [25, 26] and performed morphometric analysis, as well as quantitative and qualitative analysis of cell types. The number of germ cells, especially pachytene primary spermatocytes and elongated spermatids, increased after laser irradiation at a dose of 28.05 J/cm2. The ultrastructural features of germ and Sertoli cells in this group were similar to those of the control group, while irradiation at 46.8 J/cm2 had a deleterious effect on the seminiferous epithelium, including the dissociation of immature spermatids and evident ultrastructural changes in these cells.
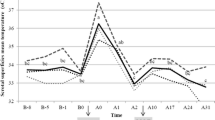
Alves et al. [28] added a new factor to the previous methods. In contrast to the three previous studies, the authors induced testicular degeneration by heat in the animal model used. The study was divided into two experiments. Scrotal thermography, imaging assessment, and histopathological analysis were performed. In the first experiment, six healthy White Dorper rams were submitted to scrotal insulation (INS) by attaching insulating bags to the scrotum for 72 h to induce testicular degeneration. After this period, the animals were divided into three groups: INS, no laser treatment (control group; n = 2); INS28 treated with LLLT at 28 J/cm2 (n = 2), and INS56 treated with LLLT at 56 J/cm2 (n = 2). The INS28 group exhibited a smaller proportion of lumen area and a lower degree of degeneration. In the second experiment, the best LLLT protocol defined in experiment 1 (INS28) was used. Twenty healthy rams were divided into four groups: CC (control group; n = 5) not submitted to scrotal insulation or LLLT, CL not submitted to scrotal insulation and treated with LLLT (n = 6), IC submitted to scrotal insulation and not treated with LLLT (n = 3), and IL submitted to scrotal insulation and treated with LLLT (n = 6). No significant difference in testicular morphology was observed between groups. On the other hand, the dose applied (28 J/cm2) was found to increase the number of cells in the seminiferous tubule of rams and to exert deleterious effects on seminal parameters.
Finally, Dadras et al. [29] evaluated the effect of LLLT on testicular tissues in a model of streptozotocin-induced type 1 diabetes. The authors evaluated stereological parameters, including the number of spermatogonia, primary spermatocytes, spermatids, spermatozoa, Sertoli cells, and Leydig cells, as well as the length of the seminiferous tubules, testicular volume, and interstitial tissue volume. In that study, 15 male Syrian mice were randomly divided into three groups of 5 animals each: (1) control group, (2) first laser group (890 nm, 80 Hz, 0.03 J/cm2; 3 times per week for 3 weeks), and (3) second laser group (same parameters as group 2 but using a dose of 0.2 J/cm2). The authors observed a significant increase of Sertoli cell count in both irradiated groups compared with the control group; this cell count was significantly higher in group 3 compared with group 2. Both irradiated groups showed a significant increase in the number of Leydig cells compared with the control group. There were significant increases in the length of the seminiferous tubules in both irradiated groups compared with the control group.
Two studies [28, 29] also evaluated the effects of LLLT on seminal parameters. However, since this was not the objective of the present study, these data were not considered in our analysis.
Risk of bias and quality of the included studies
Four of the five included studies reported participant randomization. None of the studies reported an adequate method of allocation concealment and/or assessor blinding to the treatment protocols. Thus, based on the criteria established in this systematic review, all studies were rated as high risk of bias (Fig. 2).
Risk of bias assessment of the selected studies according to the criteria of the Cochrane Collaboration tool [24]
Discussion
There are well-established applications of LLLT in medicine, including healing promotion at sites of injury, remodeling, and/or inflammation reduction, and application to nerves to induce analgesia, lymph nodes to reduce edema and inflammation, and trigger points (single point or up to 15 points) to promote muscle relaxation and to reduce sensitivity. Since the method is noninvasive, LLLT is particularly useful for patients with needle phobia or those who do not tolerate treatments with nonsteroidal anti-inflammatory drugs [30].
In the studies of Bermúdez et al. [25, 26], infrared laser radiation caused an increase in the DNA content of germ cells 24 h after the last application and after one cycle of the seminiferous epithelium. According to Clermont and Harvey [31], the duration of the cycle of the seminiferous epithelium is 12.9 days, less than the resting period of 15 days of both studies. This increase was dependent on the dose applied and was also related to the differentiation stage of germ cells. Fifteen days after irradiation, there was a higher proportion of spermatogonia with increased 4C DNA content compared with controls, while the proportion of cells with 2C DNA content decreased, especially after the dose of 28.05 J/cm2, what may be due to a laser-induced change in the cell cycle phases of spermatogonia and, subsequently, in the mitotic rhythm.
In the study of Taha and Valojerdi [27], the mean number of pachytene primary spermatocytes was increased in animals irradiated at 28.05 J/cm2 compared with the other two groups, while the number of spermatogonia decreased significantly. In contrast, deleterious effects on the seminiferous epithelium were observed in animals irradiated at 46.80 J/cm2, including the dissociation of immature spermatids and evident ultrastructural changes in these cells. At the dose of 28.05 J/cm2, the positive effects can be explained by acceleration of the meiotic rhythm, indicating stimulation of spermatogenesis by low laser light doses. In addition, the mean number of immature round spermatids decreased significantly and that of elongated mature spermatids increased at 28.05 J/cm2 compared with the other two groups. These changes can also be explained by the acceleration of the spermatid maturation process that resulted in an increase in the number of these cells in their final stage of maturation. On the other hand, the most likely explanation for the observations in the group irradiated with 46.8 J/cm2 is that, beyond a threshold dose, laser irradiation exerts negative effects on the tissue. There was no degeneration or decrease in the number of Sertoli cells after laser irradiation, with application of the two doses resulting in hypertrophy of these cells. The authors suggest that this change may be due to the need of Sertoli cell support for increased germ cells at 28.05 J/cm2 or increased phagocytic activity of Sertoli cells following irradiation with 46.8 J/cm2. The study also concludes that low laser doses can accelerate the meiotic and mitotic rhythm during spermatogenesis and increase the number of germ cells, especially primary spermatocytes and elongated spermatids, in agreement with the results reported by Bermudez et al. [25, 26]. These findings suggest that LLLT is likely to change the duration of the cell cycle phase of spermatogonia and to accelerate the mitotic rhythm.
In contrast to the previous studies, Alves et al. [28] used large animals (rams) and added the parameter of target tissue degeneration induced by heat exposure to the model. The aim of the first experiment was to establish an LLLT protocol, determining the best energy density applied to the testes of rams. Histopathological analysis showed that the dose of 28 J/cm2 provided better results in terms of lumen proportion and degeneration degree than the dose of 56 J/cm2. Hence, the first protocol was chosen for the subsequent experiments. By stimulating ATP synthesis, laser irradiation promotes cell proliferation, as demonstrated by the histopathological features of the testes in experiment 1. The proportion of the lumen area of the seminiferous tubule was smaller in the group treated with LLLT at 28 J/cm2 than in the untreated group and the group treated with LLLT at 56 J/cm2, as also observed by Taha and Valojerdi [27]. Consequently, the number of cells was higher in the group with a smaller proportion of lumen area. Although the same effect was not observed in experiment 2, the proportion of lumen area was apparently smaller in the group treated with LLLT than in the untreated group. This difference in histopathological patterns between experiments 1 and 2 may be explained by the different assessment periods.
Like Alves et al. [28], Dadras et al. [29] introduced a parameter of degeneration in the animal model used. In this case, the parameter chosen was streptozotocin-induced type 1 diabetes mellitus, a condition known to reduce sperm count and motility and to increase the number of spermatozoa with abnormal morphology. Significant increases were observed in the length of the seminiferous tubules in the two irradiated groups (0.03 and 0.2 J/cm2) and compared with the control group, and this increase was significantly greater in the second irradiated group compared with the first one. In addition, compared with the control group, irradiation with an energy density of 0.2 J/cm2 was significantly more effective than a density of 0.03 J/cm2 in modulating parameters of semen analysis in the model of streptozotocin-induced diabetes. The authors concluded the higher energy density caused significant improvements in stereological parameters and in the parameters of semen analysis compared with the lower energy density and control groups. This conclusion is opposite to the findings of Taha and Valojerdi [27], who found deleterious effects of high doses of laser irradiation on tissue morphology. It is worth noting that because Taha and Valojerdi [27] did not use an injury model unlike the study of Dadras et al. [29] in which testicular architecture was compromised by diabetes, comparison between the two studies is at least controversial.
The diversity of the parameters impairs correlation of the results, especially between experimental models with and without tissue injury. Nevertheless, the data indicate cellular biostimulation, with a direct effect on testicular morphology. These effects were generally observed in the groups exposed to a total dose of about 28 J/cm2, suggesting that this dose is ideal for biostimulation. Poorly satisfactory effects were found for groups exposed to higher total doses, which were even deleterious in some cases. This fact permits to establish a threshold between positive and negative effects of laser irradiation on tissues. The fact that the two groups in the study of Dadras et al. [29] treated with doses below 28 J/cm2 exhibited positive effects only reinforces this theoretical range. Another methodological detail worth mentioning is the area (anatomical part) of the testis that is irradiated. Bermúdez et al. [25, 26] and Taha and Valojerdi [27] performed irradiation at the inferior pole of the left testis; however, this information was not reported in the studies of Alves et al. [28] and Dadras et al. [29], which could be a possible flaw in the reports. Within this context, the lack of standardization in the other parameters may lead to survey bias regarding the conclusions mentioned above, reinforcing the need for better methodological standardization, which would increase the reliability of the proposed methods.
Conclusion
The results of this systematic review indicate that low-level laser application to the male germ tissue could be promising, particularly in cases with some degree of tissue injury that compromises the fertility of the individual. Although the current results suggest possible effective treatment for different cases of male infertility, many issues still need to be clarified. Published data are scarce, and there is a lack of standardization of laser therapy parameters and experimental models, as well as of morphological findings. More experiments, more data, and better standardization of the methods are necessary. Based on the availability of more consistent data, clinical trials should be performed.
References
Pathak UI, Gabrielsen JS, Lipshultz LI (2020) Cutting-edge evaluation of male infertility. Urol Clin North Am 47:129–138. https://doi.org/10.1016/j.ucl.2019.12.001
Agarwal A, Mulgund A, Hamada A, Chyatte MR (2015) A unique view on male infertility around the globe. Reprod Biol Endocrinol 13:37. https://doi.org/10.1186/s12958-015-0032-1
Baker HW (1998) Reproductive effects of nontesticular illness. Endocrinol Metab Clin N Am 27:831–850. https://doi.org/10.1016/s0889-8529(05)70043-8
Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP (2007) Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod 22:188–196. https://doi.org/10.1093/humrep/del364
Ferlin A (2012) New genetic markers for male fertility. Asian J Androl 14:807–808. https://doi.org/10.1038/aja.2012.84
O'Flynn O'Brien KL, Varghese AC, Agarwal A (2010) The genetic causes of male factor infertility: a review. Fertil Steril 93:1–12. https://doi.org/10.1016/j.fertnstert.2009.10.045
Bracke A, Peeters K, Punjabi U, Hoogewijs D, Dewilde S (2018) A search for molecular mechanisms underlying male idiopathic infertility. Reprod BioMed Online 36:327–339. https://doi.org/10.1016/j.rbmo.2017.12.005
Hjollund NH, Bonde JP, Jensen TK, Olsen J (2000) Diurnal scrotal skin temperature and semen quality. The Danish first pregnancy planner study team. Int J Androl 23:309–318. https://doi.org/10.1046/j.1365-2605.2000.00245.x
Wang C, McDonald V, Leung A, Superlano L, Berman N, Hull L, Swerdloff RS (1997) Effect of increased scrotal temperature on sperm production in normal men. Fertil Steril 68:334–339. https://doi.org/10.1016/s0015-0282(97)81525-7
Henderson J, Baker HW, Hanna PJ (1986) Occupation-related male infertility: a review. Clin Reprod Fertil 4:87–106
Sheiner EK, Sheiner E, Hammel RD, Potashnik G, Carel R (2003) Effect of occupational exposures on male fertility: literature review. Ind Health 41:55–62. https://doi.org/10.2486/indhealth.41.55
Jung A, Strauss P, Lindner HJ, Schuppe HC (2008) Influence of moderate cycling on scrotal temperature. Int J Androl 31:403–407. https://doi.org/10.1111/j.1365-2605.2007.00783.x
Durairajanayagam D, Agarwal A, Ong C (2015) Causes, effects and molecular mechanisms of testicular heat stress. Reprod BioMed Online 30:14–27. https://doi.org/10.1016/j.rbmo.2014.09.018
Ebokaiwe AP, Ijomone OM, Osawe SO, Chukwu CJ, Ejike CECC, Zhang G, Wang F (2018) Alteration in sperm characteristics, endocrine balance and redox status in rats rendered diabetic by streptozotocin treatment: attenuating role of Loranthus micranthus. Redox Rep 23:194–205. https://doi.org/10.1080/13510002.2018.1540675
Khaneshi F, Nasrolahi O, Azizi S, Nejati V (2013) Sesame effects on testicular damage in streptozotocin-induced diabetes rats. Avicenna J Phytomed 3:347–355
de Freitas LF, Hamblin MR (2016) Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron 22:7000417. https://doi.org/10.1109/JSTQE.2016.2561201
Li WT, Chen HL, Wang CT (2006) Effect of light emitting diode irradiation on proliferation of human bone marrow mesenchymal stem cells. J Med Biol Eng 26:35–42
Moore P, Ridgway TD, Higbee RG, Howard EW, Lucroy MD (2005) Effect of wavelength on low-intensity laser irradiation stimulated cell proliferation in vitro. Lasers Surg Med 36:8–12. https://doi.org/10.1002/lsm.20117
Wu S, Zhou F, Wei Y, Chen WR, Chen Q, Xing D (2014) Cancer phototherapy via selective photoinactivation of respiratory chain oxidase to trigger a fatal superoxide anion burst. Antioxid Redox Signal 20:733–746. https://doi.org/10.1089/ars.2013.5229
Gao X, Xing D (2009) Molecular mechanisms of cell proliferation induced by low power laser irradiation. J Biomed Sci 16:4. https://doi.org/10.1186/1423-0127-16-4
Gadella BM, Luna C (2014) Cell biology and functional dynamics of the mammalian sperm surface. Theriogenology 81:74–84. https://doi.org/10.1016/j.theriogenology.2013.09.005
Cohen N, Lubart R, Rubinstein S, Breitbart H (1998) Light irradiation of mouse spermatozoa: stimulation of in vitro fertilization and calcium signals. Photochem Photobiol 68:407–413
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JPTG, Higgins S (2011) Cochrane handbook of systematic reviews of interventions. Version 5.1.0. The Cochrane collaboration Available: www.handbook.cochrane.org. Accessed 2020 Feb 25
Bermúdez D, Carrasco F, Diaz F, Perez-de-Vargas I (1991) Germ cell DNA quantification shortly after IR laser radiation. Andrologia 23:303–307. https://doi.org/10.1111/j.1439-0272.1991.tb02566.x
Bermúdez D, Carrasco F, Pérez de Vargas I (1993) Effect of IR laser radiation on germ cell DNA content after one cycle of the seminiferous epithelium. Arch Androl 31:177–181. https://doi.org/10.3109/01485019308988397
Taha MF, Valojerdi MR (2004) Quantitative and qualitative changes of the seminiferous epithelium induced by Ga. Al. As. (830 nm) laser radiation. Lasers Surg Med 34:352–359. https://doi.org/10.1002/lsm.20027
Alves MB, de Arruda RP, Batissaco L, Florez-Rodriguez SA, de Oliveira BM, Torres MA, Ravagnani GM, Lançoni R, de Almeida TG, Storillo VM, Vellone VS, Franci CR, Thomé HE, Canella CL, De Andrade AF, Celeghini EC (2016) Low-level laser therapy to recovery testicular degeneration in rams: effects on seminal characteristics, scrotal temperature, plasma testosterone concentration, and testes histopathology. Lasers Med Sci 31:695–704. https://doi.org/10.1007/s10103-016-1911-1
Dadras S, Abdollahifar MA, Nazarian H, Ghoreishi SK, Fallahnezhad S, Naserzadeh P, Jajarmi V, Chien S, Bayat M (2018) Photobiomodulation improved stereological parameters and sperm analysis factors in streptozotocin-induced type 1 diabetes mellitus. J Photochem Photobiol B 186:81–87. https://doi.org/10.1016/j.jphotobiol.2018.06.018
Vladimirovich Moskvin S, Ivanovich Apolikhin O (2018) Effectiveness of low level laser therapy for treating male infertility. Biomedicine (Taipei) 8:7. https://doi.org/10.1051/bmdcn/2018080207
Clermont Y, Harvey SC (1965) Duration of the cycle of the seminiferous epithelium of normal, hypophysectomized and hypophysectomized-hormone treated albino rats. Endocrinology 76:80–89. https://doi.org/10.1210/endo-76-1-80
Funding
The study was financed in part by the Brazilian National Council for Scientific and Technological Development (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Façanha, E.L., de Morais, E.F., Pinheiro, J.C. et al. Effect of low-level laser therapy on seminiferous epithelium: a systematic review of in vivo studies. Lasers Med Sci 36, 259–267 (2021). https://doi.org/10.1007/s10103-020-03122-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03122-y