Abstract
To evaluate the effectiveness of photobiomodulation (PBM) on primary burning mouth syndrome (pBMS). We searched Chinese and English studies published before February 10, 2020. The databases used include PubMed, EMBASE, the Cochrane Library, Web of Science, Wanfang Database, and China National Knowledge Infrastructure (CNKI). Randomized controlled clinical trials (RCTs) that used the PBM to treat pBMS and reported specific treatment outcomes were considered for inclusion. We eventually included 12 RCTs, and 574 samples were included in these studies. The primary outcomes investigated were pain reduction and life quality improvement. A meta-analysis performed on 9 groups in 5 trials showed that PBM was effective in reducing pain compared with placebo (MD − 1.86, 95% CI − 2.59 to − 1.13, Z = 4.99, P < 0.00001). Meta-analysis was also performed on 7 groups in 4 trials and showed that PBM was effective in improving life quality compared with placebo (MD − 3.43, 95% CI − 5.11 to − 1.75, Z = 4.00, P < 0.0001). Qualitative analysis of the included RCTs found that PBM might also play a role in the decrease of TNF-α and IL-6 in saliva. Three studies that compared PBM with medications were evaluated by descriptive analysis. None of the treatment-related adverse event was reported. Up to date, PBM appears to have an effect on pain reduction and life quality improvement in pBMS patients. However, more evidence is still required to warrant its efficacy and safety in treating pBMS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
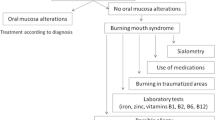
Primary burning mouth syndrome (pBMS) is a complex chronic pain disorder. The International Headache Society defines it as an intraoral burning or dysesthetic sensation, recurring daily for more than 2 h over more than 3 months, without clinically evident causative lesions [1]. And the International Association for the Study of Pain (IASP) defines that BMS (also known as glossodynia, glossopyrosis, oral dysesthesia, or stomatodynia) is a chronic intraoral burning sensation that has no identifiable cause either local or systemic condition or disease [2]. The prevalence of pBMS ranges from 0.7 to 15%, with an average age ranging from 55 to 60 years, mainly affecting perimenopausal women, and with a female:male ratio of about 7:1 [3].
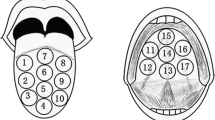
The chronic pain caused by pBMS is usually bilateral. The most common site that pBMS patients complain of pain is the tongue, especially the first two-thirds of the tongue. The pain can also occur in the palate, gum, lip mucosa, and other places. Accompanying symptoms include dry mouth, sensory abnormalities, and taste changes [4]. In addition, pBMS patients are prone to sleep disturbances, headaches, and more severe menopausal symptoms [5]. Furthermore, it may be accompanied by severe emotional distress (anxiety, depression, or anger) or disturbed oral functions such as eating, yawning, and even speaking [6], seriously affecting patients’ quality of life. Although about half of the patients show a trend of spontaneous remission within 6 to 7 years, pBMS still leads to a decline in overall quality of life and increased psychological stress for a long time [7]. Since the pathogenesis of pBMS is not fully understood yet, both the diagnosis and treatment of pBMS are challenging [8]. Currently, medications used to treat pBMS include antidepressants, antipsychotics, anticonvulsants, analgesics, and topical capsaicin, while the multiple side effects make it impossible for patients to tolerate long-term treatment [3].
Photobiomodulation (PBM) is a therapy that mainly uses red or near-infrared light to have beneficial effects on cells or tissues. PBM has potential analgesic, anti-inflammatory, biological stimulation and bactericidal effects, so PBM can help relieve pain, accelerate the resolution of the inflammatory process, and promote the healing of damaged tissues. However, the underlying action mechanism of PBM has not been completely clarified yet. The most accepted theory is that light is absorbed by the cytochrome C oxidase (CcOx) in the mitochondria, resulting in an increase in adenosine triphosphate (ATP). Meanwhile, PBM may lead to a transient burst of reactive oxygen species (ROS), followed by a decrease in the oxidative stress. In stressed or hypoxic cells, nitric oxide (NO) competitively replaces oxygen and binds to CcOx, thereby inhibiting cellular respiration and reducing ATP production. PBM could reverse this inhibition by dissociating NO from its binding sites to CcOx. Another possible mechanism of PBM could be the release of Ca2+. The concentration of cellular Ca2+ regulates a number of reactions and is important for signal transduction [9, 10]. In addition, although PBM has long been considered a non-thermal treatment, a new theory proposes that selective absorption by CcOx may lead to local increase of intracellular thermocline, and the microscale thermal change may have important significance in the mechanism of PBM [11].
PBM has been reported effective in reducing chronic low back pain, chronic neck pain, and other types of chronic pain [12]. A meta-analysis showed that PBM was effective in treating both acute and chronic neck pain, and the treatment effect for patients with chronic neck pain can be maintained for 22 weeks [13]. Another meta-analysis conducted by Huang et.al found that PBM was an effective way to reduce pain in non-specific chronic low back pain patients [14]. Moreover, PBM is recommended for the prevention of oral mucositis (OM) and related pain in cancer patients by the Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO). The evidence supports the use of specific settings of PBM therapy for the prevention of OM in specific patient populations, including patients who received hematopoietic stem cell transplantation, head and neck (H&N) radiotherapy (without chemotherapy), and H&N radiotherapy with chemotherapy. It is considered patient-friendly especially in the treatment of pediatric patients [15]. In dentistry, PBM is also used as an alternative physical therapy or supplementary approach. It has effects on reducing pain and swelling after the extraction of third molar [16], reducing temporomandibular joint pain and orthodontic pain [17, 18], and reducing lesion size and pain in patients with lichen planus [19].
For pBMS, as a chronic pain disorder, PBM may provide new therapeutic strategies and possibilities for the management. An animal study has indicated that reduced sensory nerve conduction and the increase of blood flow by PBM might be involved in the pain relief [20]. In the last few years, more clinical studies have reported the effects of PBM on pBMS. Although it had been shown that PBM is favorable in reducing pain in pBMS patients, the results are still controversial. Pezelj-Ribarić et al. found that there were no statistically significant differences in VAS (visual analog scale) between the PBM group and the control group [21]. Meanwhile, the application parameters (wavelength, power, dose, exposure time, optical spot size) and techniques that make PBM effective in treating pBMS need to be optimized. Therefore, we undertook a systematic review and meta-analysis to provide the up-to-date evidence of PBM for treating pBMS.
Methods
Search strategy
Literature search was based on the standards of the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) [22]. Two authors (WQZ and WWZ) independently searched Chinese and English studies published before February 10, 2020, in the following databases: PubMed, EMBASE, the Cochrane Library, Web of Science, Wanfang Database, and China National Knowledge Infrastructure (CNKI). The following terms were searched in combination: (“photodynamic therapy” OR photochemotherapy OR phototherapy OR laser OR photomodulation OR photobiomodulation OR “low level light therapy” OR LLLT OR “Low Power Laser Therapy” OR Irradiation OR Biostimulation OR “low energy laser therapy” OR “low intensity laser therapy” OR “low level laser therapy”) AND (“burning mouth syndrome” OR “stomatodynia” OR “stomatopyrosis” OR “glossopyrosis” OR “glossodynia” OR “sore mouth” OR “sore tongue” OR “oral dysesthesia” OR “glossalgia”). We also referred to the references of included studies to avoid omitting any study related to our review.
Inclusion criteria
Studies selected in this review must meet the following criteria: (I) randomized controlled clinical trials (RCTs) that treat pBMS using PBM in any wavelength, power, or energy; (II) studies that reported specific treatment outcomes; and (III) studies published in English or Chinese.
Exclusion criteria
Review articles, letters to editors, conference abstracts, patented inventions, unpublished articles, and articles unable to get the full text were excluded in this review.
Data extraction
Two authors (WQZ and WWZ) performed a complete evaluation and determined inclusion by reading full-text articles independently. The two authors compared their selected articles, and if they disagreed, the third author (ZMY) reached a consensus. Data extracted from the included studies were summarized in a table, including age, sex ratio, sample size, intervention, follow-up time, outcome measurements, and overall results.
Risk of bias
Two authors (WQZ and LJH) used the Cochrane risk of bias assessment criteria to assess the risk of bias in the included studies. The bias considered included random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting.
Data synthesis
We used the Review Manager Software version 5.3 to perform this meta-analysis. We assessed the effectiveness of PBM on pBMS by means of the weighted mean difference (WMD) and 95% confidence interval (CI). The I2 metric was used to indicate the statistical heterogeneity of the included studies. When P > 0.1 and I2 < 50%, the studies were considered to have sufficient homogeneity, and a fixed effect model was adopted. When P < 0.1 and I2 ≥ 50%, the studies were considered to have heterogeneity, and a random effects model was adopted. Meta-analyses were performed on two outcomes: pain reduction and life quality improvement.
Results
Characteristics of the included studies
The database search results contained a total of 397 references. After removing 144 duplicate references, 253 were analyzed by scanning article titles and abstracts or even reading the full text. Then, 230 articles were excluded, and eventually, we included 12 studies in this systematic review. Among these studies, 6 were conducted in Europe, 3 in South America, and 3 in Asia [21, 23,24,25,26,27,28,29,30,31,32,33] (Fig. 1).
The 12 RCTs included 574 subjects in total. The data extracted from these RCTs are shown in Table 1.
Risk of bias
According to the Cochrane handbook, the potential risks of bias in the 12 RCTs were obtained. The overall risk of each bias is shown in Fig. 2, and Fig. 3 shows the risk of each bias in the included studies respectively. The performance bias, attribution bias, and reporting bias of these RCTs were generally low.
Pain reduction
Five RCTs that provided data of pain reduction by means ± SD (standard deviation) were included in the meta-analysis [26,27,28,29,30]. The heterogeneity analysis of the 9 groups in 5 trials yielded x2 = 26.01, P = 0.001, and I2 = 69%. Therefore, a random effects model was used for the analysis and showed that PBM was effective in reducing pain compared with placebo, measured by VAS (MD − 1.86, 95% CI − 2.59 to − 1.13, Z = 4.99, P < 0.00001) (Fig. 4).
From the study of Valenzuela et al. [26], the improvements of VAS from initial to the end of treatment were 15.7% and 15.6% respectively in the two PBM groups, while that of the placebo group was 7.3%. Moreover, the study of Spanemberg et al. reported that the initial average VAS was 8.9 in the laser group and 8.3 in the control group (P > 0.05). At 2 months of follow-up, the values were 4.7 and 5.1 respectively. In addition, a significant improvement for the laser group at the two-month follow-up was observed (P = 0.0038) [23]. Bardellini et al. stated that at the end of the last session, the pain symptoms of patients in the PBM group were significantly relieved and the treatment effects lasted for 1 month [24]. The research from Sikora et al. showed that pain was significantly reduced in both experimental and placebo groups [25].
Life quality improvement
A meta-analysis was performed on 7 groups in 4 trials that compared experimental groups with placebo groups in favor of PBM for life quality improvement [24, 26, 28, 29]. Heterogeneity between the 4 studies was found after pooling the data (x2 = 13.39, P = 0.04; I2 = 55%). Therefore, a random effects model was used for the analysis and showed that PBM was effective in improving life quality compared with placebo, measured by OHIP-14 (MD − 3.43, 95% CI − 5.11 to − 1.75, Z = 4.00, P < 0.0001) (Fig. 5). However, the research from Sikora et al. showed that neither the experimental nor the placebo group improved the OHIP-14 scores [25].
Changes in other outcomes of PBM-treated pBMS patients
Both Spanemberg et al. [23] and Valenzuela et al. [26] reported that no statistical differences in terms of hospital anxiety–depression scale were found between the groups before or after the treatment. Moreover, Valenzuela et al. assessed the xerostomia before and after the treatment, but no significant changes were found in either group [26]. Pezelj-Ribarić et al. measured levels of proinflammatory cytokines in saliva and discovered that TNF-α and IL-6 reduced obviously in the PBM group [21].
Three studies that compared PBM with medications were evaluated by descriptive analysis. Arduino et al. randomly divided 33 pBMS patients into the PBM group and the clonazepam group, and finally found that PBM appeared to have effect on reducing burning sensation than clonazepam [31]. Barbosa et al. compared the efficiency of PBM with alpha-lipoic acid (ALA) in treating pBMS and showed that PBM was more effective in reducing burning sensation than ALA [32]. In the study of Yang et al., both laser and mecobalamin were effective to reduce the symptoms of pBMS, but the combination of laser and mecobalamin was more effective [33].
Heterogeneity was assessed by considering possible differences in various aspects, and it was noted that laser parameters and treatment courses were heterogeneous. Details for wavelength, power density, power, dose, energy, optical spot size, exposure time, and treatment courses are listed in Table 2. The parameters of PBM were in the following ranges: wavelength of 630~1064 nm, power of 30~3200 mW, dose of 1~200 J/cm2, optical spot size of 0.028~1 cm2, and exposure time per point of 4~58 s. As to the treatment course of PBM, it ranged from 2~10 weeks in the included studies and the frequency varied from daily to once a week.
Sensitivity analysis
Sensitivity analysis was performed by removing studies one by one in both meta-analyses. For continuous data from VAS in pBMS, we detected significant heterogeneity (x2 = 26.01, P = 0.001, and I2 = 69%). Removal of the two groups [26, 27] that used 6-J energy eliminated statistical heterogeneity (x2 = 10.83, P = 0.009, and I2 = 45%). For continuous data from OHIP-14 in pBMS, we detected slight heterogeneity (x2 = 13.39, P = 0.04; I2 = 55%). After removing one study [29] using a 630-nm wavelength, the statistical heterogeneity was eliminated (x2 = 7.58, P = 0.018, and I2 = 34%).
Discussion
PBM is a non-invasive, painless tool that can be easily available. More and more evidence shows that the main role of PBM is to stimulate mitochondrial cytochromes and then to initiate secondary cell-signaling pathways. Studies showed that PBM was effective in many parts of the body, such as for the treatment of musculoskeletal injuries, degenerative diseases, and dysfunction [34]. pBMS is a chronic pain disorder mainly affecting perimenopausal women and seriously affects the quality of life of the patients [35]. In recent years, PBM has emerged as a potential non-invasive treatment for pBMS with a handful of studies that have shown that PBM therapy is effective in reducing burning symptoms in pBMS patients.
This systematic review conducted a thorough literature search to evaluate the effectiveness of PBM on pBMS. We eventually included 12 RCTs with 574 samples. Our meta-analysis showed that PBM was effective in reducing pain and improving life quality compared with placebo. However, we detected heterogeneity in the pooling data when performing meta-analysis. Delivery parameters such as wavelength, power density, dose, optical spot size, and number of points of application might be the reason for the differences found in the outcome. However the reported clinical settings were variable, limiting data integration. More rigorously designed studies are required to clarify which parameter is the most effective in treating pBMS.
Dose is the basic parameter of PBM and represents the total amount of energy delivered to the surface unit area [9]. The characteristics of biphasic dose response of PBM show that very small doses of light have no effect but slightly higher ones have positive effect until a plateau is reached, and excess energy may lead to photobioinhibition rather than photobiostimulation. It is currently proposed that higher doses are more beneficial for pain relief, and there is a multiphasic dose response to PBM, which may be more useful than the generally accepted biphasic dose response [11, 36]. The studies included in this review showed huge differences in dose, ranging from 1 to 200 J/cm2. Valenzuela et al. [26] and Spanemberg et al. [28] used high doses that exceed 100 J/cm2, while the doses in the other studies (except for three unspecified studies) are between 1 and 12 J/cm2. The optical spot size varies from 0.028 to 1 cm2, while Arbabi-Kalati et al. [29] and Cui et al. [30] did not specify this. Regarding the number of points of application, Arbabi-Kalati et al. selected 10 areas on the oral mucosa (buccal mucosa: 2, tongue: 2, floor of the mouth: 2, soft palate: 1, and hard palate: 1) [29]. In the study of Valenzuela et al., the laser was applied at 10 points in the area where patient reported symptoms [26], while in the study of Pezelj-Ribarić et al., only the tongue mucosa received laser irradiation [21].
Furthermore, the technique of application may be more helpful and worthy of more attention. Two techniques are available for irradiation of target tissue, respectively spot technique and scanning technique [9]. Arduino et al. used the spot technique and the laser probe held perpendicularly at a distance of about 2 mm from the mucosa [31]. With the spot technique, energy is delivered point by point until the entire surface irradiated is covered. If the laser beam is collimated, the probe should be held perpendicular to the tissue and at a distance; the beam diameter does not vary with distance. Conversely, if the emitted beam is divergent, the probe should be in contact with the target tissue to avoid changes in dose and power density due to possible variations in distance. In the study of Sugaya et al., laser irradiation was delivered in the scanning mode with the laser point in contact with the mucosa [27]. With the scanning technique, the probe is slid over the surface to treat, using different patterns. Whatever pattern is chosen, the surface to be treated must be irradiated in a uniform way [9].
A single treatment is usually sufficient for acute and postoperative therapy. However, for chronic pain and degenerative diseases, up to 10 treatments may be required [37]. As to the treatment course of PBM for pBMS, it ranged from 2 to 10 weeks in the included studies, and the frequency varied from daily to once a week. Cui et al. found that daily and every other day irradiation achieved the same treatment effect under the same treatment course [30]. Spanemberg et al. found that in the symptom scales of OHIP-14, a significant difference was observed between the IR3W laser group (three times a week for 3 weeks) and the control group. However, the IR1W laser group (once a week for 10 weeks) did not differ significantly in relation to the control group [28]. Valenzuela et al. found that PBM reduced pain and improved life quality significantly from baseline to 2 weeks in groups I and II (once a week for 4 weeks) compared with the placebo group. Nevertheless, no statistical differences were found from 2 to 4 weeks [26]. The variety of treatment courses and frequency of the included studies made us think of a question about the optimum treatment course and frequency. While ensuring the effectiveness of PBM, physicians should also consider how to ensure the compliance of patients.
Five RCTs of the included studies provided follow-up data ranged from 1 to 3 months, with VAS as the primary outcome measurements. Arduino et al. compared the effectiveness of PBM and clonazepam on pBMS; PBM appeared to be superior in reducing pain sensation at the 12-week follow-up period [31]. The study from Spanemberg et al. found a significant improvement in the laser group at the 2-month follow-up [23]. In the study of Bardellini et al., the patients treated with PBM showed a significant decrease in symptoms after the complete course of therapy, which was maintained at the 1-month follow-up [24]. Spanemberg et al. found that symptoms were relieved in all groups at the last treatment and maintained throughout the 8-week follow-up [28]. Based on these preliminary trials, PBM is able to reduce the symptoms of pBMS with a constant and long-lasting effect. But the number of trials that provide a follow-up period is small, thus studies with a long-term follow-up are essential to certify the lasting effect of this alternative treatment.
pBMS is a complex chronic pain disorder, so VAS was selected as the primary outcome measurement to assess subjective pain relief in all included studies. It consists a 100-mm vertical line, marked with 0 (= no pain) to 100 (= most severe pain experienced) [26]. In our results, we used statistics to demonstrate an effect in pain relief using PBM. In the study of Spanemberg et al., the initial average VAS was 8.9 in the laser group and 8.3 in the control group. After the eighth session, the VAS score was 5.5 and 5.8 respectively, and at 2 months of follow-up, the values were 4.7 and 5.1 respectively [23]. The difference of VAS between the laser group and the control group is less than 1 point. Although a statistically significant improvement for the laser group at the 2-month follow-up was observed (P = 0.0038), the clinical significance of this outcome is debatable, as a 1-point difference in VAS is minor. In another study conducted by Valenzuela et al., the initial average VAS was 8.38 in the laser group II and 7.83 in the control group, and after the 4-week therapy, the VAS score was 7.06 and 7.65 respectively. The improvements of VAS from initial to the end of treatment were 15.6% and 7.3% respectively [26]. The clinical significance of VAS difference less than 1 point indicates limited clinical significance, so more studies with different parameters are needed to verify the pain relief effect of PBM.
For PBM, the incidence of adverse effects is low, and no severe adverse events were reported. The potential adverse events are mostly ocular. PBM devices emit divergent beams, and the ocular risk diminishes over distance (within several meters), so the operator should ensure that the laser beams are not aimed at the eyes, and anyone who are present within range should wear wavelength-appropriate safety spectacles including patients and the team workers [38]. In this systematic review, the adverse events of PBM had not been reported in the included studies. This may state that PBM is a safe application with minimal side effects, and give the physician the confidence to use PBM to treat pBMS. However, adverse events in large-sample trials still need to be investigated.
Although meta-analyses were performed on 5 and 4 studies respectively, containing a larger sample size than a single study, there were still some limitations to consider. Firstly, our review only included English and Chinese articles. So articles published in other languages were not included in this review. Secondly, we are not able to extract all target data from every included study. Thirdly, the included studies had a large heterogeneity owing to the lack of standardization of the dosimetric parameters, study subject selection, outcome measurements, and follow-up time. Therefore, rigorously designed clinical researches are required to certify the effectiveness and safety of PBM for treating pBMS patients.
Conclusions
Up to date, PBM demonstrated the effectiveness in pain reduction and life quality improvement in pBMS patients. It might act as an alternative therapy for pBMS. However, more evidence is still required to warrant its efficacy and safety in treating pBMS. Meanwhile, the application parameters (wavelength, power, dose, exposure time, optical spot size, treatment course) and techniques need to be optimized.
References
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211
Treede RD, Rief W, Barke A et al (2019) Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11). Pain 160(1):19–27
Coculescu EC, Tovaru S, Coculescu BI (2014) Epidemiological and etiological aspects of burning mouth syndrome. J Med Life 7(3):305–309
Klasser GD, Fischer DJ, Epstein JB (2008) Burning mouth syndrome: recognition, understanding, and management. Oral Maxillofac Surg Clin North Am 20(2):255–271 vii
Grushka M (1987) Clinical features of burning mouth syndrome. Oral Surg Oral Med Oral Pathol 63(1):30–36
Ariyawardana A, Chmieliauskaite M, Farag AM et al (2019) World workshop on oral medicine VII: burning mouth syndrome: a systematic review of disease definitions and diagnostic criteria utilized in randomized clinical trials. Oral Dis null:141–156
Ducasse D, Courtet P, Olie E (2013) Burning mouth syndrome: current clinical, physiopathologic, and therapeutic data. Reg Anesth Pain Med 38(5):380–390
Moghadam-Kia S, Fazel N (2017) A diagnostic and therapeutic approach to primary burning mouth syndrome. Clin Dermatol 35(5):453–460
Coluzzi DJ, Parker S (2017) Lasers in dentistry-current concepts. Springer, New York
Hamblin MR, De Sousa MVP, Agrawal T (2016) Handbook of low level laser therapy. Pan-Stanford Publishing, Singapore
Cronshaw M, Parker S, Arany P (2019) Feeling the heat: evolutionary and microbial basis for the analgesic mechanisms of photobiomodulation therapy. Photobiomodul Photomed Laser Surg 37(9):517–526
Kato IT, Pellegrini VD, Prates RA, Ribeiro MS, Wetter NU, Sugaya NN (2010) Low-level laser therapy in burning mouth syndrome patients: a pilot study. Photomed Laser Surg 28(6):835–839
Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM (2009) Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 374(9705):1897–1908
Huang Z, Ma J, Chen J, Shen B, Pei F, Kraus VB (2015) The effectiveness of low-level laser therapy for nonspecific chronic low back pain: a systematic review and meta-analysis. Arthritis Res Ther 17:360
Zadik Y, Arany PR, Fregnani ER et al (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27:3969–3983
Aras MH, Güngörmüş M (2009) The effect of low-level laser therapy on trismus and facial swelling following surgical extraction of a lower third molar. Photomed Laser Surg 27(1):21–24
Salmos-Brito JA, de Menezes RF, Teixeira CE, Gonzaga RK, Rodrigues BH, Braz R (2013) Evaluation of low-level laser therapy in patients with acute and chronic temporomandibular disorders. Lasers Med Sci 28(1):57–64
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofac Orthop 141(3):289–297
Akram Z, Abduljabbar T, Vohra F, Javed F (2018) Efficacy of low-level laser therapy compared to steroid therapy in the treatment of oral lichen planus: a systematic review. J Oral Pathol Med 47(1):11–17
Pozza DH, Fregapani PW, Weber JB et al (2008) Analgesic action of laser therapy (LLLT) in an animal model. Med Oral Patol Oral Cir Bucal 13(10):E648–E652
Pezelj-Ribarić S, Kqiku L, Brumini G et al (2013) Proinflammatory cytokine levels in saliva in patients with burning mouth syndrome before and after treatment with low-level laser therapy. Lasers Med Sci 28(1):297–301
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Spanemberg JC, Segura-Egea JJ, Rodríguez-de Rivera-Campillo E et al (2019) Low-level laser therapy in patients with burning mouth syndrome: a double-blind, randomized, controlled clinical trial. J Clin Exp Dent 11(2):e162–e169
Bardellini E, Amadori F, Conti G, Majorana A (2019) Efficacy of the photobiomodulation therapy in the treatment of the burning mouth syndrome. Med Oral Patol Oral Cir Bucal 24(6):e787–e791
Sikora M, Včev A, Siber S, Vučićević Boras V, Rotim Ž, Matijević M (2018) The efficacy of low-level laser therapy in burning mouth syndrome-a pilot study. Acta Clin Croat 57(2):312–315
Valenzuela S, Lopez-Jornet P (2017) Effects of low-level laser therapy on burning mouth syndrome. J Oral Rehabil 44(2):125–132
Sugaya NN, Silva ÉF, Kato IT, Prates R, Gallo CB, Pellegrini VD (2016) Low intensity laser therapy in patients with burning mouth syndrome: a randomized, placebo-controlled study. Braz Oral Res 30(1):e108
Spanemberg JC, López López J, de Figueiredo MA, Cherubini K, Salum FG (2015) Efficacy of low-level laser therapy for the treatment of burning mouth syndrome: a randomized, controlled trial. J Biomed Opt 20(9):098001
Arbabi-Kalati F, Bakhshani NM, Rasti M (2015) Evaluation of the efficacy of low-level laser in improving the symptoms of burning mouth syndrome. J Clin Exp Dent 7(4):e524–e527
Cui D, Zhang Y (2017) Efficacy of low-level laser therapy in the treatment of burning mouth syndrome. Chinese Journal of Practical Stomatology 10(3):158–162
Arduino PG, Cafaro A, Garrone M et al (2016) A randomized pilot study to assess the safety and the value of low-level laser therapy versus clonazepam in patients with burning mouth syndrome. Lasers Med Sci 31(4):811–816
Barbosa NG, Gonzaga AKG, de Sena Fernandes LL et al (2018) Evaluation of laser therapy and alpha-lipoic acid for the treatment of burning mouth syndrome: a randomized clinical trial. Lasers Med Sci 33(6):1255–1262
Yang JG, Sun P, Liu ZX (2018) Efficacy of ND:YAG laser and mecobalamin in the treatment of burning mouth syndrome. General Journal Of Stomatology 5(36):1–2,8
McKenzie AL, Carruth JA (1984) Lasers in surgery and medicine. Phys Med Biol 29(6):619–641
Périer JM, Boucher Y (2019) History of burning mouth syndrome (1800-1950): a review. Oral Dis 25(2):425–438
Kate RJ, Rubatt S, Enwemeka CS, Huddleston WE (2018) Optimal laser phototherapy parameters for pain relief. Photomed Laser Surg 36(7):354–362
Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR (2012) The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 40(2):516–533
Carroll JD, Milward MR, Cooper PR, Hadis M, Palin WM (2014) Developments in low level light therapy (LLLT) for dentistry. Dent Mater 30(5):465–475
Acknowledgments
We would like to acknowledge Dr. Cibele Nasri-Heir from Rutgers School of Dental Medicine for her kind help.
Funding
This work was financially supported by the National Natural Science Foundation of China (No. 81570985).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable for this review.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, W., Hu, L., Zhao, W. et al. Effectiveness of photobiomodulation in the treatment of primary burning mouth syndrome–a systematic review and meta-analysis. Lasers Med Sci 36, 239–248 (2021). https://doi.org/10.1007/s10103-020-03109-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03109-9