Abstract
Peri-implant disease may affect survival of dental implants. The aim of the study is to analyze the effectiveness of diode laser as a supportive modality to the non-surgical conventional treatment of peri-implant mucositis (PiM) and initial peri-implantitis (PI). Twenty-three patients with single implants suffering from PiM or initial PI were selected and randomly divided into two groups; control group (CG) received non-surgical conventional treatment, and test group (TG) received non-surgical conventional treatment and diode laser application with wavelength of 980 nm. Probing pocket depth (PPD) and bleeding on probing (BOP) were recorded at baseline (T0) and at 3 months follow-up (T1). The average of PPD value for TG was 4.04 ± 0.54 mm at T0 and it was 2.98 ± 0.70 mm at T1. In the CG, PPD average was 3.8 ± 1.24 mm at T0 and was 3.54 ± 0.35 mm at T1. In TG, the BOP was positive in 44 sites at T0 and in 6 sites at T1. In CG, the BOP was positively observed in 52 sites at T0 and in 28 sites at T1. The 980-nm diode laser may be considered an adjunct to the conventional non-surgical treatments of PiM and initial PI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many complications that may affect soft and hard tissues surrounding dental implants have been reported [1]. Inflammatory complications associated with bacterial invasion can be categorized into peri-implant mucositis (PiM) or peri-implantitis (PI). PiM is a reversible inflammatory process that affects mainly soft tissues surrounding the dental implants [1]. By contrast, PI is a chronic inflammation caused by bacterial biofilm on the implant surface and associated with progressive loss of supporting bone, leading to implant failure if not treated [2]. Many risk factors are proposed to the development of PiM and PI such as poor oral hygiene, history of periodontitis, smoking, or diabetes [3].
According to the literature, PiM occurs in approximately 80% of patients with implants and in about 50% of the inserted implants. On the other hand, PI arises in approximately 28 to 77% of patients with implants and in 12 to 43% of the inserted implants [2].
Since PiM is a reversible disease and its management may prevent the possibility to advance to PI which is a challenging complication without a fully accepted management guideline, the prevention and management of PiM have become a growing important issue [4].
The main goal of PiM treatment is to eliminate the biofilm around the implant surface that may allow the complete resolution of the inflammatory lesion [5]. Early diagnosis and non-surgical mechanical approach have been suggested to be the treatment for the PiM [6]. However, complete resolution of PiM is not regularly achieved by this protocol [6].
Several adjunctive modalities have been proposed in combination with the mechanical curettage, such as local or systemic antimicrobials, air polishing systems, or probiotic supplements [7,8,9]. Nevertheless, these modalities have shown limitations as they can increase bacterial resistance, develop superinfections, damage the implant surface, or cannot access the entire implant sites [10, 11].
Because high-intensity lasers have the capability to remove the granulation tissues around the implant surface without inducing melting, cracking, or crater formation on the implant surface, a bactericidal capacity, and a capacity to accelerate the healing process, they have been introduced as an adjunct to the treatment of peri-implant diseases [12]. The data about the efficacy of using high-intensity lasers, in particular diode lasers, in the treatment of PiM are inconclusive, and carrying out further evaluations is recommended [4].
The aim of the study is to evaluate the effectiveness of 980-nm diode laser as a supportive modality to the non-surgical conventional treatment of PiM and initial PI through comparing the treatment outcomes with and without laser application.
Materials and methods
The study was performed on patients referred to the department. It was conducted between March 2016 and July 2018. The study received the approval protocol number (0685) from the Institutional Review Board of the Department. The study was conducted in compliance with the directives given by the DM dated July 15, 1997, concerning the European standards of good clinical practice and according to the local Ethical Committee guidelines. Twenty-three patients with an average age of 56.1 years (14 males and 9 females) and with single titanium implant suffering from PiM or initial PI were selected. An informed consent was signed by all individual participants in the study.
The inclusion criteria consisted of patients with age from 20 to 80 years old, presence of at least one single implant affected by PiM or initial PI (periodontal pocket depth (PPD) range ≤ 6 mm), and patients with PPD ≥ 6 mm who refused surgical approach and non-smoking patients.
The exclusion criteria consisted of patients with subperiosteal dental implants, moderate and severe PI, osteoporosis, uncontrolled systemic disease that may interfere with healing process such as diabetes mellitus or immunocompromised patients, and patients with high risk or established medication-related osteonecrosis of the jaws (MRONJ).
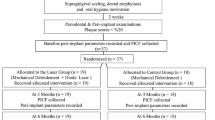
After complete clinical and radiographic examinations (ortho-panoramic and periapical radiographs), patients were randomly allocated from a computer-generated list of random numbers into 1 of 2 groups: test group (TG) or control group (CG).
Allocation concealment was achieved through the provision, by professionals not involved in patient enrolment, of a numbered sequence of opaque and sealed envelopes containing the assignment code. The list remained inaccessible and the envelopes were opened, sequentially, after enrolling the patient and obtaining consent (Fig. 1).
In TG, 11 patients (7 males and 4 females) with 11 implants were included with average age of 55.73 years. Six of them were non-smokers and 5 of them were ex-smokers. In CG, 12 patients (7 males and 5 females) with 12 implants were included with average age of 56.42 years. Eight of them were non-smokers and 4 of them were ex-smokers.
For both groups, PPD and bleeding on probing (BOP) were measured at the baseline (T0) and at 3 months follow-up (T1) by the same operator. Each implant sulcus was divided into six points (disto-buccal, buccal, mesio-buccal, mesio-lingual, lingual, and disto-lingual points), and PPD for each point was estimated using a calibrated manual periodontal probe (Goldman-Fox William, Asa Dental S.P.A., Italy). At the same six points, BOP was evaluated as present if bleeding was observed within 30 s from probing or absent if no bleeding was observed after 30 s from probing. [13]
Mechanical debridement
For both groups, full mouth mechanical debridement was performed through the use of both ultrasonic piezoelectric scaler and manual instruments (titanium-coated Gracey curettes) by the same operator in one session. In addition, mechanical debridement with carbon fiber curettes was carried out in each peri-implant sulcus and implant surface. A 1% chlorhexidine gel (Corsodyl—Glaxosmithkline C.Health.Spa, London, England) was applied in the pocket of each implant of TG and CG for 5 min. Post-operative instructions were given for the proper oral hygiene measures.
Soft tissue laser curettage
In TG, the peri-implant sulcus of each implant was irradiated immediately after the mechanical debridement with diode laser (Raffaello®, Dental Medical Technologies, Lissone, Italy) of wavelength 980 nm, at power of 1 W, in pulsed mode (Ton = 10 ms, Toff = 50 ms), energy density of 14.1 J/cm2, and spot diameter of 0.3 mm. The peri-implant sulcus of each implant was divided into six points (the same points used for PPD and BOP measurement). In each point, the tip of the laser fiber was inserted parallel to the pocket wall, in contact with the mucosa, at approximately 1 mm from the base of the pocket to avoid the possible thermal effect on the supporting bone. Then, the laser was activated and repeated vertical movements (apical-coronal movements) were performed for 10 s. The total time of laser application for each peri-implant sulcus was 60 s.
Statistical analysis
A power analysis was performed for the study design to define the minimum number of peri-implant sites necessary to attain a statistical power of 0.80 and statistical significance of 0.05 for each group (TG and CG). The power analysis results indicated a minimum number of 51 implant sites for the test group and 55 sites for the control group. Means and standard deviations of PPD and BOP values were determined in each group. Statistical analysis was performed with SPSS (Statistical Package for Social Science) for Windows 20.0. Mann-Whitney test was used for two-by-two comparison of the groups. Wilcoxon test was used to determine differences in mean clinical parameters at baseline and 3-month intervals in each group. A statistical significant difference was considered when p < 0.05.
Results
A total of 72 sites in CG and 66 sites in TG were evaluated. In TG, the BOP at T0 was positive in 44 sites with an average of 4 ± 1.48 sites on the implant sulcus. At T1, it was found only in 6 sites with an average of 0.55 ± 0.69 sites on implant sulcus.
In CG, the BOP was positively observed at T0 in 52 sites with an average of 4.33 ± 1.56 points on implant sulcus. At T1, it was observed in 28 sites with an average of 2.33 ± 1.07 sites on the implant sulcus (Fig. 2) A statistical significant decrease was observed between T0 and T1 in both groups for BOP values (p < 0.01).
The average of PPD value for TG was 4.04 ± 0.54 mm at T0 and it was 2.98 ± 0.7 mm at T1 (Fig. 3). In the CG, the average was 3.8 ± 1.24 mm at T0 and was 3.54 ± 0.35 mm at T1 (Fig. 4). A statistical significant decrease was observed between T1 and T0 in both groups for PPD values (p < 0.01) (Fig. 5).
No significant differences were observed between both groups at T0 for the PPD (p = 0.805) and BOP (p = 0.547). However, significant differences were observed between both groups at T1 for PPD (p < 0.01) and BOP (p < 0.0001). A greater decrease in the both clinical parameters was detected for subjects treated with lasers (TG) (Table 1).
No significant differences between both groups (TG and CG) were shown in relation to the age (t = 0.118, p = 0.907), male/female ratio (χ2 = 0.068, p = 0.795), and the number of ex-smokers and non-smokers (χ2 = 0.577, p = 0.750).
Discussion
In our study, both TG and CG showed a significant reduction in clinical parameters (PPD and BOP). However, the reduction of both clinical parameters in the laser group was greater with a significant difference in comparison with that in the CG. In the laser group, the PPD was decreased for more than 1 mm after 3 months and the BOP score was negative in 86% of the bleeding sites.
The literature seems to agree with the use of diode laser in the treatment of PiM and initial PI [14]. Sánchez-martos et al. demonstrated a significant positive response with the gingival index and better response without significance with the other parameters. The authors found additional benefits by adding a laser to the conventional treatments of PiM [13]. A clinical case by Roncati et al. showed that the use of diode laser resulted in a decrease in PPD and led to negative BOP scores around the implant [15].
On the other hand, contrary opinions have been also expressed [16, 17]. Although an in vivo study demonstrated better results with 980-nm diode laser during the first month after treatment in the reduction of clinical signs of inflammation, the results were comparable with the conventional modality without laser at 3 months follow-up. The authors concluded that the adjunct use of laser did not provide any statistically significant benefit when it was compared with the only non-surgical mechanical treatment [16].
In an in vitro study by Kreisler et al., the bactericidal effect was reported lower than that was obtained by a 1-min treatment with 0.2% chlorhexidine mouthwash, emphasizing the absence of obvious advantage of 809-nm diode laser treatment over the conventional disinfection methods [18].
Two recent systemic reviews investigated the efficacy of laser in the management of peri-implant diseases and have detected the presence of significant heterogeneity in studies’ outcomes [4, 6]. This heterogeneity has been referred to be related to the presence of various definitions of the peri-implant diseases, the presence of different clinical parameters for the evaluation of the disease, the presence of several lasers parameters, and/or the nature of the disease as a multifactorial disease with host-related factors that may affect the outcomes [6].
It was observed that the combination of laser with non-surgical treatment of peri-implant diseases has minimal benefit in the reduction of PPD, plaque index, the gain of clinical attachment level (CAL), and improvement of recession. But, it was observed that a more reduction of BOP in the short term was demonstrated with the combination of laser and the non-surgical approach [6]. This conclusion was obtained through a general evaluation of different types of laser application in a non-surgical approach for both types of peri-implant disease (PI and PiM).
Most of the existing studies on lasers as an adjunct for the management of peri-implant diseases were referred to peri-implant diseases without precise definition or to PI [6]. These may be due to the existing dilemma of the diagnostic criteria of both PiM and PI despite the presence of universally accepted definitions. The diagnosis of peri-implant defects is usually based on clinical and radiographical findings [19].
The BOP index might be considered an indicator for PiM and a sign of pathology in an active phase, since PiM is an inflammatory condition of the soft tissues surrounding implants. However, there is no sufficient evidence confirming that in the literature [8]. While PPD measurement is indicated to evaluate the clinical attachment level, it is usually recommended for the evaluation of PI. Bias could occur with the PPD measurement, as it is operator-dependent and is related to the probing methods, such as probing pressure, periodontal tissue condition, and diameter of probe [20]. In our study, all the included patients were suffering from PiM and initial PI. The decrease of BOP scores was obvious and greater than the reduction of PPD values.
There are different goals of the application of laser as an adjunct for the management of the peri-implant disease, such as disinfection purpose, elimination of inflammatory soft tissues around implants, and detoxification and cleaning of the implant surface [12]. Each kind of these goals may require a different type of laser, with different parameters and different application techniques. In the literature, the major part of the existing studies evaluating the efficacy of diode lasers in the management of PiM was using an 810-nm diode laser [4, 6, 14]. Few of them were evaluating the efficacy of diode laser on the elimination of granulation tissues around implants with PiM.
There is a slight difference between 980-nm and 810-nm diode lasers. Generally, diode lasers are absorbed by hemoglobin, melanin, and other chromophores that exist in the peri-implant soft tissue. However, 810-nm diode lasers have a higher affinity to hemoglobin than 980 nm [21].
The employed laser in this study was a 980-nm diode laser directed toward the soft tissues. The main goal was to aid the mechanical non-surgical approach on eliminating the granulation tissues around implants utilizing its favorable capacity to modulate the wound healing through the promotion of cell proliferation and differentiation, and anti-inflammatory effects on the peri-implant tissues [12]. The capacity of high irradiance lasers to modulate wound healing is referred to the delivery of lower laser doses, within the photobiomodulation dose, to the surrounding tissues of the operative sites [22].
Concerns were expressed about the application of laser in the treatment of peri-implant diseases. They were related to the possibility of causing damage to the implant surface or thermal injuries to the supportive bone. Eriksson et al. demonstrated that 10 °C over the physiologic baseline temperature (37 °C) for 1 min may induce irreversible supportive bone damage and implant loss [23]. Some authors believe that diode laser may not be considered a thermal safe tool if used at 1 W in continuous mode for more than 30 s [24, 25]. Monzavi et al. found that precautions should be taken with the use of diode laser in the implant tissues, despite that the mean temperature of coronal, middle, and apical points did not exceed 47 °C in their study after irradiation [26].
Conclusions
Based on the obtained results, 980-nm diode laser may be considered an adjunct to the conventional non-surgical treatment of PiM and initial PI. Some limitations should be overcome for future studies such as enrolling a control group treated with placebo, considering long-term follow-up periods, including other parameters such as microbiological investigations, and increasing the number of patients.
References
Schwarz F, Derks J, Monje A, Wang HL (2018) Peri-implantitis. J Clin Periodontol 45(Suppl 20):S246–S266
Lee CT, Huang YW, Zhu L, Weltman R (2017) Prevalences of peri-implantitis and peri-implant mucositis: systematic review and meta-analysis. J Dent 62:1–12
Lindhe J, Meyle J (2008) Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35(8 Suppl):282–285
Albaker AM, Arrejaie AS, Alrabiah M, Abduljabbar T (2018) Effect of photodynamic and laser therapy in the treatment of peri-implant mucositis: a systematic review. Photodiagn Photodyn Ther 21:147–152
Renvert S, Polyzois I (2018) Treatment of pathologic peri-implant pockets. Periodontol 76(1):180–190
Lin GH, Suárez López del Amo F, Wang HL (2018) Laser therapy for treatment of peri-implant mucositis and peri-implantitis: an American Academy of Periodontology best evidence review. J Periodontol 89(7):766–782
Schwarz F, Becker K, Renvert S (2015) Efficacy of air polishing for the non-surgical treatment of peri-implant diseases: a systematic review. J Clin Periodontol 42(10):951–959
Smeets R, Henningsen A, Jung O, Heiland M, Hammächer C, Stein JM (2014) Definition, etiology, prevention and treatment of peri-implantitis--a review. Head Face Med 10:34
Mombelli A, Lang NP (1998) The diagnosis and treatment of peri-implantitis. Periodontol 17:63–76
Verdugo F, Laksmana T, Uribarri A (2016) Systemic antibiotics and the risk of superinfection in peri-implantitis. Arch Oral Biol 64:39–50
Carcuac O, Derks J, Charalampakis G, Abrahamsson I, Wennström J, Berglundh T (2016) Adjunctive systemic and local antimicrobial therapy in the surgical treatment of peri-implantitis: a randomized controlled clinical trial. J Dent Res 95(1):50–57
Shibli JA (2018) Is laser the best choice for the treatment of peri-implantitis? Photomed Laser Surg 36(11):569–570
Sánchez-martos R, Samman A, Bouazza-juanes K, Díaz-fernández JM, Arias-herrera S (2020) Clinical effect of diode laser on peri-implant tissues during non-surgical peri-implant mucositis therapy: randomized controlled clinical study. J Clin Exp Dent 12(1):e13–e21
Świder K, Dominiak M, Grzech-leśniak K, Matys J (2019) Effect of different laser wavelengths on periodontopathogens in peri-implantitis: a review of in vivo studies. Microorganisms 7(7)
Roncati M, Lucchese A, Carinci F (2013) Non-surgical treatment of peri-implantitis with the adjunctive use of an 810-nm diode laser. J Indian Soc Periodontol 17(6):812–815
Aimetti M, Mariani GM, Ferrarotti F, Ercoli E, Liu CC, Romano F (2019) Adjunctive efficacy of diode laser in the treatment of peri-implant mucositis with mechanical therapy: a randomized clinical trial. Clin Oral Implants Res 30(5):429–438
Arısan V, Karabuda ZC, Arıcı SV, Topçuoğlu N, Külekçi G (2015) A randomized clinical trial of an adjunct diode laser application for the nonsurgical treatment of peri-implantitis. Photomed Laser Surg 33(11):547–554
Kreisler M, Kohnen W, Marinello C et al (2003) Antimicrobial efficacy of semiconductor laser irradiation on implant surfaces. Int J Oral Maxillofac Implants 18(5):706–711
Passi D, Singh M, Dutta SR et al (2017) Newer proposed classification of periimplant defects: a critical update. J Oral Biol Craniofac Res 7(1):58–61
Larsen C, Barendregt DS, Slot DE, Van der Velden U, Van der Weijden F (2009) Probing pressure, a highly undervalued unit of measure in periodontal probing: a systematic review on its effect on probing pocket depth. J Clin Periodontol 36(4):315–322
Aoki A, Mizutani K, Schwarz F et al (2015) Periodontal and peri-implant wound healing following laser therapy. Periodontol 68(1):217–269
Arany PR (2016) Craniofacial wound healing with photobiomodulation therapy: new insights and current challenges. J Dent Res 95(9):977–984
Eriksson AR, Albrektsson T (1983) Temperature threshold levels for heat-induced bone tissue injury: a vital-microscopic study in the rabbit. J Prosthet Dent 50(1):101–107
Lerario F, Roncati M, Gariffo A et al (2016) Non-surgical periodontal treatment of peri-implant diseases with the adjunctive use of diode laser: preliminary clinical study. Lasers Med Sci 31(1):1–6
Kreisler M, Al Haj H, D’hoedt B (2003) Temperature changes induced by 809-nm GaAlAs laser at the implant-bone interface during simulated surface decontamination. Clin Oral Implants Res 14(1):91–96
Monzavi A, Fekrazad R, Chinipardaz Z, Shahabi S, Behruzi R, Chiniforush N (2018) Effect of various laser wavelengths on temperature changes during periimplantitis treatment: an in vitro study. Implant Dent 27(3):311–316
Author information
Authors and Affiliations
Contributions
Conception, design, data acquisition, analysis, and interpretation, drafting and critical revision of the manuscript were performed by Tenore Gianluca, Montori Alessandra, and Mohsen Ahmed; data acquisition was performed by Mattarelli Giovanni; data analysis and interpretation, and critical revision of the manuscript were performed by Palaia Gaspare and Romeo Umberto. All authors gave final approval and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval
The study received the approval protocol number (0685) from the institutional review Board of the Department. The study was conducted in compliance with the directives given by the DM dated 07/15/97 concerning the European standards of good clinical practice, and according to the local Ethical Committee guidelines.
Informed consent
An informed consent was signed by all individual participants in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tenore, G., Montori, A., Mohsen, A. et al. Evaluation of adjunctive efficacy of diode laser in the treatment of peri-implant mucositis: a randomized clinical trial. Lasers Med Sci 35, 1411–1417 (2020). https://doi.org/10.1007/s10103-020-03009-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03009-y