Abstract
In this study, we investigate the efficiency of laser radiation on oxyhemoglobin (HbO2) rate in blood vessels and its wavelength dependence. The results of in vivo experimental measurements of the laser-induced photodissociation of HbO2 in cutaneous blood vessels in the visible and near-infrared (IR) spectral range are presented. Arterial oxygen saturation (SpO2) was measured by a method of fingertip pulse oximetry, which is based on the measurement of the modulated pulse wave of the blood. The light irradiating the finger was provided by corresponding light-emitting diodes (LED) at 15 wavelengths in the 400–940 nm spectrum range. Statistical results with a value of p < 0.05 were viewed as being significant for all volunteers. The results show that there is a decrease in SpO2 in the blood under the influence of the transcutaneous laser irradiation. Three maxima in the spectral range (530, 600, and 850 nm) are revealed, wherein decrease in the relative concentration of SpO2 reaches 5 % ± 0.5 %. Near-IR radiation plays a dominant role in absorption of laser radiation by oxyhemoglobin in deeper layers of tissue blood vessels. The obtained data correlate with the processes of light propagation in biological tissue. The observed reduction in SpO2 indicates the process of photodissociation of HbO2 in vivo and may result in local increase in O2 in the tissue. Such laser-induced enrichment of tissue oxygenation can be used in phototherapy of pathologies, where the elimination of local tissue hypoxia is critical.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tissue oxygenation plays a key role in metabolism, energy supply, and life activity of an organism. Controlling this mechanism gives the possibility of biological stimulation to achieve therapeutic effect. Factors that can affect the delivery of oxygen in tissue are of considerable interest, and one of them is the light radiation in the optical spectral range. Oxyhemoglobin (HbO2) photodissociation has been known since the 1950s [1, 2]. Numerous studies aim at measuring the quantum yield of HbO2 photodissociation. In the earlier studies, a rather low quantum yield of about 0.01 was obtained. With the advance in flash photolysis technique and shortening of the laser pulse duration, quantum yields of 0.08–0.13 for HbO2 [3] were reported. Using picosecond pulses, quantum yields of 0.65 were obtained [4]. The low quantum yields observed in the earlier studies were explained by the fast processes of heme-oxygen geminate recombination. Many works were devoted to the study of fast kinetics of photodissociation processes, geminate recombination, electron relaxation, and ligand rebinding [5–9], as well as conformational transitions in hemoglobin-ligand complexes and binding constants [10–13]. The majority of studies concerning the kinetics of HbO2 photodissociation were carried out using optical radiation within the near-UV range, the Hb Soret band (λmax = 412 nm), and β- and α-bands (542 and 576 nm), as the strongest absorption bands of HbO2 in aqueous solutions in vitro [3, 14]. However, among the large amount of scientific data, there is practically no information in the literature on the connection between the quantum efficiency of the photodissociation and the wavelength of the irradiating light. Certain works report only the spectral dependence of the kinetic properties of the absorption spectrum of the solution [15], but the photolysis efficiency dependence on the light wavelength has not been investigated.
Light in the red region of the spectrum is very rarely used, and practically, there is no data on its effect in the near-infrared region. It is reasonable to expect that the in vivo photolytic effect will be different from that observed in buffer solutions, considering the different biological environment and specific features of light propagation in biological tissue.
Investigation of photodissociation of hemoglobin complexes in vivo could be carried out using arterial blood saturation parameter arterial oxygen saturation (SpO2). By definition, SpO2 is determined as the ratio of oxygen-saturated hemoglobin (HbO2) to the total concentration of hemoglobin (unsaturated Hb + saturated HbO2) in the blood, i.e., the SpO2 determines the relative HbO2 concentration in blood.
In this paper, we present an experimental study in vivo of the rate of the SpO2 in blood under the influence of local transcutaneous light-emitting diodes (LED) irradiation with wavelength in the spectral range from 405 to 940 nm.
Materials and methods
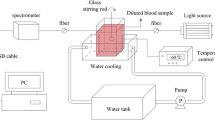
Determination of the SpO2 in blood is performed by a method similar to the method of pulse oximetry, which is based on the measurement of light-modulated pulse wave of blood. The measurements were taken on the fingers of ten healthy male volunteers including non-smokers and smokers after a 12-h nonsmoking interval in order to reduce the impact of HbCO on the accuracy of pulse oximetry. All procedures performed in the study were in accordance with the ethical standards with informed consent obtained from each subject and approval by the institutional review board (Institute of Applied Problems of Physics and Biophysics, Academy of Sciences of Ukraine).
The pulse oximetry sensor was placed on the first phalanx of the finger. The light was delivered to the finger from LEDs (or laser diodes) at 15 wavelengths in the 400–940 nm spectrum range: 405, 470, 525, 568, 590, 605, 635, 660, 700, 780, 860, and 940 nm. The optical power of every source is selected to provide an approximately equal number of photons of different wavelengths incident on the irradiated skin area. The corresponding power density of irradiation taking into account the output aperture varied from 50 mW/cm2 for λ = 405 nm to 125 mW/cm2 for λ = 940 nm.
The SpO2 was measured with a pulse oximetry sensor operating in backscattered light mode based on the standard LED pair with emission wavelengths of 660 and 940 nm and a silicon photodiode BPW34 (OSRAM). Due to the original method of data processing, the accuracy of measurements is 3–4 times higher compared with standard systems. The system allows continuous photoplethysmographic monitoring, recording, and data storage. Data acquisition was executed by a measuring block with a microcontroller connected to PC. The microcontroller includes a microprocessor, RAM, ROM, decoder, timer, quartz-stabilized clock generator, and input/output ports. The sampling frequency was 348 Hz, the LED flash pulse duration 160 μs, and the interval between pulses of red and IR emission 200 μs. The SpO2 level is calculated using a coefficient of linear regression of red and IR signals instead of the common ratio of modulation coefficients. Calculations were made on interval lengths of 200 to 400 points with a shift of 100 points. This procedure provides a measurement of SpO2 with a smaller increment than the cardiac cycle length.
Two series of experimental measurements were performed. In the first series, the irradiation beam was directed at the lower front of the phalanx about 5 mm distance from the measuring sensor. In the second series, the radiation was directed to the lower part of the second phalanx near the joint between the first and second phalanges. In this case, the distance from the irradiation spot to the photodiode was about 12 mm. In both cases, the direct light flux does not reach the surface of the photodetector.
For each source in each series from 7 to 15, records were made, according to the following scheme: 30 s without radiation, 30 s with radiation, and 30 s without radiation. For every record, the mean value of SpO2 and its change induced by the irradiation were calculated and then averaged over the number of records. In order to eliminate rogue results, only measurements which were within the range between + and −20 % standard deviations from the mean were included in the analysis. All results are given as the mean ± (SD). The Student’s test for connected sampling was used for the statistical calculations. Statistical results with a value of p < 0.05 were viewed as being significant for all volunteers. The evaluation was carried out using the program “Origin 7.5.”
Results
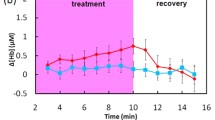
Figure 1 shows a typical example of changing the rate of the SpO2 level in the blood measured with and without LEDs exposure on the first finger phalanx (in this case 635 nm). As it can be seen from Fig. 1a, when irradiation is switched on, the coefficient of modulation I of red light signal of the pulse oximetry sensor increases more than that of infrared one, which is displayed in the immediate (within ~0.1 s) drop in SpO2 (Fig. 1b). During irradiation, the SpO2 level remains constant and returns to initial value practically immediately after the irradiation shutdown.
The decrease in the level of SpO2 depends on the wavelength and power of the irradiating light. Photoplethysmograms are recorded for all wavelengths in the 400–940 nm spectral range. Figure 2 shows the rate of ΔSpO2 plotted against irradiation wavelength for two series of measurements on the first and the second finger phalanges. In the same figure, for comparison, ΔSpO2 is plotted the HbO2 absorption spectrum in aqueous solutions (3). The average initial SpO2 levels (without irradiation) in all groups of measurements differ insignificantly, in the range of 94.5 to 96.0 % (with overall mean of 95.2 ± 0.5SD %).
A drop in ΔSpO2 during irradiation in the first (1) and the second (2) series. (3) - Extinction coefficient of HbO2 in aqueous solutions according to Prahl [13]
In the first series, the ΔSpO2 dropped down to 5 % from its usual level. Three maxima in the spectral range are revealed, two in the visible range of the spectrum and one broader peak in the near-IR range (850 nm). Unfortunately, the set of available narrow-band LEDs does not allow detailed description of HbO2 photodissociation in the region of α- and β-bands. Nevertheless, two peaks of ΔSpO2 drops by 5 % ± 0.5 % (p < 0.05) from its usual level near 530 and 600 nm can be clearly seen, which correlate well with the calculated absorption spectra (3). With increasing the light path length in tissue, which takes place in the second series (irradiation of the second finger phalanx), the short-wave peak near 530 nm disappears, the peak near 600 nm decreases considerably, and the strongest effect (ΔSpO2 ≈ 4 % ± 0.3 % (p < 0.05)) is observed near 850 nm. Light with wavelengths below 470 nm is strongly absorbed in superficial skin layers, and irradiation in this spectral range has no effect on SpO2.
Discussion
In contrast to other in vitro studies, this study was carried out under in vivo conditions, so it is possible to make statements about the practicability of the measurement effect.
Thus, we demonstrate that the rate of the SpO2 in blood varies under the influence of local transcutaneous LED irradiation and significantly depends on the radiation wavelength. The results obtained correlate well with the calculated in [13] absorption spectra. It is evident that the observed local decrease of arterial SpO2 during irradiation is caused by HbO2 photodissociation in blood capillary vessels. The fact that the saturation returns to initial value practically immediately when the illumination is switched off can be explained by the fast geminate recombination and oxygen rebinding as well as by blood evacuation from the site of measurement due to blood flow.
The results obtained correlate with the characteristics of light propagation in blood-filled tissue. The visible light at 450 and 580 nm has a small penetration depth into skin tissue, because of their proximity to the absorption bands of some basic skin chromophores such as oxyhemoglobin and melanin. Red and especially near-IR radiation penetrate much deeper into soft tissues. Therefore, irradiation in the region of the α- and β-bands, not to mention Soret band, which can be effective for very thin blood layers, in real tissue, can cause HbO2 photodissociation only in shallow superficial skin layers.
The results of this study cannot identify any immediate effect of the radiation on the oxygenation in tissue in vivo. It would be reasonable if further studies on the immediate effects would take into account additional parameters, which in addition to the observed effects may have a role in clinical practice.
Calculations of the effective oxyhemoglobin absorption spectra in the tissue depth based on the Kubelka-Munk model [16] show that with increasing light penetration depth, the α- and β-bands gradually merge and fade away, shifting to the long-wave spectral region with a peak about 585 nm, and from tissue depth deeper than 2.5 mm, the IR band of the HbO2 plays a dominant role in the laser radiation absorption. Therefore, it is clear that under light irradiation of more or less considerable tissue volume (≥1 сm3), the primary role in HbO2 photodissociation is due to red and especially near-IR radiation.
It is interesting and remains unclear what fraction of O2 molecules released by photodissociation can escape from the heme pocket and diffuse through cell membranes and capillary walls, thereby increasing the tissue oxygen tension. Heu et al. [17] studied perfusion and oxygenation in skin tissue after laser irradiation with wavelength of 660 nm and power density of 6.4 mW/cm2. No significant change in SpO2 was noticed after 15 min of irradiation. That does not contradict with the data of the present study, where the saturation drop is observed only during irradiation and at a much higher power density, but do not give any information about possible change in free oxygen content in tissue.
On the other hand, Asimov in [18] measured a significant increase in tissue oxygen tension pO2 during irradiation with He-Ne laser (633 nm, 1 mW). Measurements were carried out using transcutaneous membrane sensor with Clark electrode on the internal side of the forearm of three volunteers. A Clark electrode with diameter of 2.5 mm was placed close to the irradiation spot. After 10 min of irradiation, the local oxygen tension increased up to 1.6 times in all three patients (Fig. 3). In case of artificially induced ischemia, additional extraction of oxygen is also observed. The obtained data demonstrate the partial release of oxygen into tissue during HbO2 photodissociation.
Relative changes in tissue oxygen tension in three patients with normal microcirculation (1–3) and artificial ischemia (4) during irradiation with He-Ne laser [18]
Thus, we can expect that after prolonged irradiation (several minutes), a certain fraction of oxygen molecules released due to photodissociation of HbO2 will diffuse in the surrounding tissue and increase the oxygen partial pressure.
Liu et al. [19] also have studied changes in tissue oxygen tension pO2 as a function of laser power densities within the Hb Soret band (λmax = 412 nm) and β- and α-bands (542 and 576 nm). They also indicate an increase in tissue oxygen tension pO2 during irradiation, but no measurements are made in the red and near-IR spectra region.
It is very important to notice that photodissociation of molecular oxygen from hemoglobin does not produce singlet oxygen. Lepeshkevich in [20] by means of time-resolved luminescence spectroscopy in the near-infrared region does not measure detectable quantities of singlet oxygen during the photodissociation of O2 from myoglobin and hemoglobin.
Such possibility to increase the free oxygen content in tissues can be applied in clinical practice for treatment of a number of diseases related to problems with the microcirculation and oxygen supply and therefore requires further investigations [21].
Conclusion
The rates of SpO2 in blood in vivo and their dependence on the wavelength of the transcutaneous laser irradiation have been experimentally measured. The observed reduction in SpO2 up to 5 % indicates the process of photodissociation of HbO2 in vivo and may result in the local O2 growth in the tissue. The results obtained correlate with the peculiarities of the light propagation in blood-filled tissue. Near-IR radiation plays a dominant role in absorption of laser radiation by oxyhemoglobin in deeper layers of tissue blood vessels.
This approach gives the possibility for additional oxygen supply and allows development of optical methods for tissue hypoxia elimination.
References
Gibson Q, Ainsworth S (1957) Photosensitivity of haem compounds. Nature 180:1416–1417
Saffran W, Gibson Q (1977) Photodissociation of ligands from heme and heme proteins. J Biol Chem 252:7955–7962
Yang N, Zhang S et al (2007) Photo-dissociation quantum yields of mammalian oxyhemoglobin investigated by a nanosecond laser technique. Biochem Biophys Res Commun 353:953–959
Valat P, Alpert B (1985) Quantum yield of thirty picosecond oxyhemoglobin photodissociation effect of protein fluctuations on the quantum yield values. Laser Chem 5:173–183
Yabushita I, Kobayashi T (2010) Primary events in the photodissociation of oxyhemoglobin. Spectroscopy 24:333–338
Yabushita A, Kobayashi T (2010) Ultrafast spectroscopy of oxyhemoglobin during photodissociation. J Phys Chem B 114:11654–11658
Ghelichkhani E, Goldbeck R, Lewis J (1996) Nanosecond time-resolved absorption studies of human oxyhemoglobin photolysis intermediates. Biophys J 71:1596–1604
Hoffman B, Gibson Q (1978) On the photosensitivity of liganded hemoproteins and their metal-substituted analogues. Proc Natl Acad Sci U S A 75:21–25
Traylor T, Berzinis A (1980) Binding of O2 and CO to hemes and hemoproteins. Proc Natl Acad Sci USA 77:3171–3175
Rovira C, Kunc K, Hutter J, Ballone P (1997) Equilibrium geometries and electronic structure of iron-porphyrin complexes: a density functional study. J Phys Chem A 101:8914–8925
Jensen P, Ryde U (2004) How O2 binds to heme. J Biol Chem 279:14561–14569
Petrich J, Poyart C, Martin J (1988) Photophysics and reactivity of heme proteins: a femtosecond absorption study of hemoglobin, myoglobin and protoheme. Biochemistry 27:4049–4060
Prahl S (1999) Optical absorption of hemoglobin. Oregon Medical Laser Center USA. http://omlc.org/spectra/hemoglobin/
Filho I, Terner J et al (2008) Measurement of hemoglobin oxygen saturation using Raman microspectroscopy and 532-nm excitation. J Appl Physiol 104:1809–1817
Sato H, Wada S et al (2000) Measurement of oxygenation of hemoglobin by direct transmission of near-infrared energy (700–1000 nm) from an electronically tuned Ti:sapphire laser. Appl Spectrosc 54:1163–1167
Asimov M, Korolevich A, Konstantinova E (2007) Kinetics of oxygenation of skin tissue exposed to low-intensity laser radiation. J Appl Spectrosc 74:133–139
Heu F, Forster C, Namer B, Dragu A (2013) Effect of low-level laser therapy on blood flow and oxygen hemoglobin saturation of the foot skin in healthy subjects. Laser Ther 22:21–30
Asimov M, Thanh N (2011) Laser-induced photodissociation of oxyhemoglobin: optical method of elimination of hypoxia. Opt Spectrosc 111:254–259
Liu P, Zhu Z et al (2012) Specific absorption spectra of hemoglobin at different PO2 levels: potential noninvasive method to detect PO2 in tissues. J Biomed Optics 17:125002
Lepeshkevich S et al (2013) Does photodissociation of molecular oxygen from myoglobin and hemoglobin yield singlet oxygen. J Photochem Photobiol B 120:130–141
Lisenko S, Kugeiko M (2015) Method for estimating optimal spectral and energy parameters of laser irradiation in photodynamic therapy of biological tissue. Quantum electron 45:359–365
Acknowledgment
This work is partially supported by the project DFNI B02/9/2014 of Bulgarian Science Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
All procedures performed in the study were in accordance with the ethical standards with informed consent obtained from each subject and approval by the institutional review board (Institute of Applied Problems of Physics and Biophysics, Academy of Sciences of Ukraine).
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Yesman, S.S., Mamilov, S.O., Veligotsky, D.V. et al. Local changes in arterial oxygen saturation induced by visible and near-infrared light radiation. Lasers Med Sci 31, 145–149 (2016). https://doi.org/10.1007/s10103-015-1838-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-015-1838-y