Abstract
Purpose
Bloodstream infections (BSIs) are associated with significant morbidity, mortality and costs, while prolonged blood culture (BC) diagnosis may delay the initiation of targeted therapy. This study evaluates the impact of an optimized microbiology laboratory process on turnaround times, antibiotic use, clinical outcomes and economics for hospitalized BSI patients.
Methods
A pre-post study was conducted in a Chinese hospital in which BSI derived BC results before (Oct. 2020- Sep. 2021) and after (Oct. 2021- Sep. 2022) newly implemented microbiology diagnostics and workflow changes were analyzed. Turnaround times, antibiotic initiation, length of stay and in-hospital costs were compared.
Results
From 213 included patients, 134 were pre-optimization (pre-op) and 79 were post-optimization (post-op) cases. The median time from blood sample collection (BSC) to pathogen identification (ID) decreased from 70.12 to 47.43 h post-op (P < 0.001). The median time from BSC to the first ID report related initiation of pathogen-directed antibiotic use decreased from 88.48 to 47.85 h post-op (P < 0.001). The average hospital stay decreased from 19.54 to 16.79 days and 30-day readmissions declined from 18.7 to 13.9%, while the mean total antimicrobial drug usage costs decreased by 3,889 CNY per patient (P = 0.022) after optimization.
Conclusions
Implementing new diagnostics technologies and optimizing laboratory workflows significantly reduced antimicrobial drug usage costs, shortened the time to ID results and improved the timeliness of appropriate antibiotic choices to treat BSIs. Investments in faster testing and process improvements were clearly beneficial for patient outcomes and healthcare economics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bloodstream infection (BSI) is one of the leading causes of morbidity and mortality globally, especially among hospitalized patients [1, 2], and leads to longer hospital stays and increased costs. A study in a hospital in China, was based on a risk set matching model analysis, BSIs result in an additional 16.86 days of hospitalization and an extra cost of approximately $15,909.21 [3]. In contrast, in Ethiopia, BSIs lead to an average increase of 8.3 days in hospital stays and a 2.7-fold increase in direct medical costs [4]. Additionally, a population-wide retrospective cohort study in Canada found that BSIs were associated with a 17.0% mortality rate within 30 days, with the mortality risk varying with different pathogens [5]. Traditional diagnostic methods based on blood culture (BC) and phenotypic techniques can take up to 72 h to provide results [6] and untimely diagnostic reports have resulted in a series of risks, including untargeted antibiotic use or antimicrobial resistance, making outcomes for 30–50% of antibiotic BSI prescriptions in hospitals considered to be inappropriate [7, 8]. Thus, early and rapid identification (ID) and susceptibility testing of bloodstream pathogens are essential requirements for antimicrobial stewardship and the key to improving treatment outcomes.
Recent advances in rapid microbial diagnostic technologies, such as the polymerase chain reaction (PCR), matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) and syndromic panel-based molecular assays have significantly shortened the time to pathogen ID and susceptibility results [9,10,11,12,13,14]. These optimization programs are used in clinical practice to reduce the length of hospitalization and to accurately prescribe appropriate antibiotics, particularly since COVID-19 in 2020 that significantly impacted patient care worldwide [15, 16]. However, there are a limited number of published studies showcasing how microbiological services contribute to both clinical and economic advantages in hospitals by promptly providing ID and antimicrobial susceptibility results, especially in China [17, 18], while the traditional microbial detection methods remain the gold standard. Some evaluations have reported its beneficial effects while others have not, most likely due to its limitations on the implementation cost, workflow integration and provider awareness [19].
Additional data are still needed to quantify the clinical and economic impact of optimizing programs in real-world inpatient settings, which will provide further evidence to support the expanded use of faster diagnostics for BSIs. The present retrospective study was conducted to evaluate the impact of optimized microbiology laboratory processes on turnaround times, antibiotics use, clinical outcomes and economics for the treatment of hospitalized adult BSI patients.
Patients and methods
Clinical data were collected from Xuchang Central Hospital, Henan Province, China between Oct. 2020 and Sept. 2022. All patient records eligible for inclusion were retrieved from the Hospital Information System/Health Information Technology (HIS/HIT) system. Study inclusion criteria were: patients with suspected BSIs and positive BC results; age ≥ 18 years; and patients from inpatient wards. Those with malignancies and immunosuppression, severe comorbidities or concurrent illnesses, as well as the positive contaminants of BCs were excluded.
All research was conducted in accordance with both the Declarations of Helsinki and Istanbul. The study was approved by the Ethical Committee of Xuchang Central Hospital. Informed consent was not applicable as clinical records without any personally identifiable information were retrieved for analyses.
Optimization of processes
From Oct. 2021 to Sep. 2022, the microbiology laboratory in Xuchang Central Hospital implemented a series of improvements/optimizations in the processing of BSI specimens. With the BacT/Alert Virtuo BC system (bioMérieux) to quick load BC bottles, and the new resin anaerobic/aerobic BC bottles (bioMérieux) to neutralize antimicrobial agents, the subcultured strains were faster identified by the VITEK MS (bioMérieux). IDs and antimicrobial susceptibility tests (ASTs) could be performed in a more rational and facilitated way to offer valuable clinical treatment support. All the reports and records of patients were automatically uploaded to the Laboratory Information System (LIS) or HIS of the clinic instead of manual uploading and paper recording. The new LIS also offered a pop-up notification of ID/AST results to clinicians.
Meanwhile, a team was added to a night shift from 17:30 pm to 8:00 am in which a microbiology specialist performed subcultures of positive BC bottles, while ID and AST reports were produced twice a day, at 9:00 am in the morning and 4:00 pm in the afternoon in order to shorten reporting times.
Data collection
Two study groups, the pre-optimization (pre-op) group and the post-optimization (post-op) group, were designated according to the time point the optimized laboratory process was implemented in Oct. 2021. Patients with positive BC results in ICU, general surgery, respiratory, hematology and emergency wards from Oct. 2020 to Sept. 2021 and Oct. 2021 to Sept. 2022 were assigned to the pre-op and post-op groups, respectively. Time windows of 24 h after each report were selected to evaluate the impact on antibiotic usage.
Variables and records
Demographic information on the patients including age, gender and department of admission, together with the infection source and routine blood test results were collected. The time points of blood sample collection (BSC), blood sample receipt (BSR), Gram-stain report, the first ID report (typically ID results including the name and characteristics of the pathogen), and the final AST report time were carefully recorded to evaluate the time to results (TTRs) of each report. In the conventional laboratory process, the first ID report accompanies the AST report, while the optimized process offers the first ID report before the AST report (Fig. 1). Pathogen-directed antibiotic administration could be adjusted after each report (Gram-stain, first ID and final AST reports) were available within 24 h. Data were analyzed on the time of start of a new and/or an adjusted antibiotic treatment and/or the time of a stopped antibiotic treatment. Then the time interval between BSC/BSR to the pathogen-directed commencement of antibiotic drug administration was assessed.
Additionally, other variables were collected including total antimicrobial drug usage, treatment outcomes, total length of hospital stay and 30-day readmission rate. The economic outcomes included the total costs of antimicrobial drugs, overall hospitalization and laboratory diagnostics.
Statistical analysis
All analyses were performed using SPSS software, version 25.0. All statistical data underwent normality testing and homogeneity of variance analysis. Normally distributed data are presented as the mean ± SD and non-normally distributed data as medians (IQR). Categorical variable data were analyzed using the chi-squared or Fisher’s exact probability tests. Continuous variable data were analyzed using Mann-Whitney and Kruskal-Wallis tests. A P-value < 0.05 was assumed to denote significant differences.
Results
Baseline demographics and clinical characteristics of the patients
Records from 213 eligible patients were used in our analyses, with 134 in the pre-op group and 79 in the post-op group. Their average age was 65.44 years. Eighty-three cases (39.0%) were ICU patients and 55.9% were males, among which 83 (61.9%) were in the pre-op group and 36 (45.6%) in the post-op group. The most common infection sources were digestive (41.5%), respiratory (36.3%) and urinary tract (13.2%). There were balanced clinical characteristics between the pre-op and post-op groups for white blood cell counts (10.87 × 109/L vs. 11.37 × 109/L), neutrophils (10.09 × 109/L vs. 10.03 × 109/L), lymphocytes (93.72% vs. 107.11%), C-reactive protein (1.66 µg/mL vs. 0.82 µg/mL), or procalcitonin (23.65 ng/mL vs. 17.65 ng/mL) (Table 1).
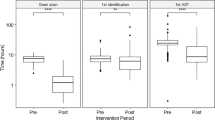
The TTRs of each laboratory microbial report
The time intervals between BSC, BSR and Gram-staining results as well as the first ID and final AST reports were compared before and after the optimization intervention. Median time intervals from BSC and BSR to Gram-staining reports were significantly reduced in the post-op group, from 46.02 (40.04, 61.92) hours to 38.21 (24.48, 47.54) hours, and 42.47 (25.79, 48.86) hours to 32.12 (21.93, 44.61) hours. For the first ID report, nearly 23 h could be saved from BSC and over 24 h from BSR in the post-op group compared to the pre-op group (P ≤ 0.001). The median time interval from BSC to the final AST report was reduced from 70.12 h for the pre-op group to 67.17 h for the post-op group (P = 0.009). Though a significant statistical difference was not found for the BSR report interval, an apparent decrease from 67.22 h for pre-op to 65.23 h for post-op was noted (P = 0.068) (Table 2; Fig. 1).
Pathogens identified in BCs
Within the pre-op group, the Gram-stain positive rate was 97.7% (131/134), compared to 84.8% (67/79) in the post-op group. There were totally 222 pathogens identified in 213 positive BC samples. The most prevalent species were Escherichia coli (40.1%) and Klebsiella pneumoniae (10.4%).
The optimization did not have much impact on positive Gram-stain rates, including the proportions of Gram-positive bacteria, Gram-negative bacteria and fungi. However, in both pre-op and post-op groups, the results of Gram-stain indicate that Gram-negative bacteria predominated in samples of BSIs (101, 73.2% vs. 58, 69.0%), in which Escherichia coli was the most common in isolates (50, 36.2% vs. 39, 46.4%) (Table 3).
Time intervals between BSC/BSR to initiation of pathogen-directed antibiotic usage
Comparing the differences in time intervals from BSC or BSR to the initiation of pathogen-directed antibiotic treatment before and after optimization, it was found that among patients having adjusted antimicrobial drug dosages within 24 h after the Gram-stain report, the median time intervals from both BSC and BSR to the administration of pathogen-directed antibiotics were significantly shorter after laboratory process optimization (BSC: post-op group 41.92 (38.01, 47.72) vs. pre-op group 60.15 (43.87, 71.52) hours, P = 0.003; BSR: post-op group 35.90 (27.63, 46.80) vs. pre-op group 48.73 (41.36, 69.54) hours, P = 0.009) (Supplementary Tables 1 and Fig. 2).
Concerning the time interval from BSC to the pathogen-directed antibiotic administration initiated according to the first ID report, it decreased to 47.85 h in the post-op group compared to the pre-op groups 88.48 h, within 24 h of the first ID report, respectively (P < 0.001). When considering BSR, the time interval was also greatly reduced to 48.05 h from 73.60 h from BSR to optimization management, compared to the pre-optimization group within 24 h of the first ID report groups (P < 0.001) (Supplementary Tables 1 and Fig. 2). The analysis data revealed a significant reduction in median time intervals of approximately 30 h for antibiotic optimization management (Supplementary Table 1).
Impact of optimization on treatment outcomes and in-hospital costs
With regard to the average total duration of antibiotic usage, the post-op group had a duration of 14.31 days, which was slightly shorter than the 16.49 days in the pre-op group, though the difference between the two groups did not reach statistical significance. Furthermore, as shown in Table 4, the total duration of hospitalization in the post-op group appeared to be shorter than pre-op, while the 30-day readmission rate, total hospitalization costs and total laboratory measurement costs seemed to be lower than pre-op. The clinical outcomes also appeared to be slightly better, although the differences in these indicators between the two groups were not statistically significant. However, concerning antibiotic usage, the average total cost in the post-op group was 5,902.80 CNY and significantly lower than the 9,791.85 CNY in the pre-op group (P = 0.022). This finding indicates that the optimization provided patients with timelier pathogen-directed antimicrobial therapy, reducing the costs associated with empiric antimicrobial treatment and resulted in tangible clinical benefits for the patients.
Discussion
The present study evaluated the impact of an optimized microbiology laboratory process on turnaround times, antibiotic usage and economics burden for 213 adult inpatients with BSIs in a class-A tertiary hospital in China. Implementation of advanced diagnostic techniques, including the BacT/Alert Virtuo BC system, new resin anaerobic/aerobic BC bottles, VITEK MS (bioMérieux), and improved sample management processes, significantly reduced the time from sample collection to Gram-stain, first ID and AST reports. These faster TTRs led to more timely appropriate antibiotic therapy, reducing the length of hospital stay and overall hospitalization costs, particularly antibiotic expenses for BSI patients.
We observed a reduction in the time from BSC/BSR to the Gram-stain report of 13 to 18 h. More importantly, the median time from BSC/BSR to the first ID report was reduced by 25.6 h to 40.6 h and from 73.60 to 88.48 h to 48.05 to 47.85 h. This enabled physicians to adjust antibiotic treatments based on the identified pathogen more than a day earlier, rather than relying on broad-spectrum empirical coverage. Previous studies have reported that in the absence of rapid diagnostics, physicians often administer empirical treatments based on patient symptoms [20, 21]. The current results are consistent with prior evidence, indicating that faster pathogen ID through advanced diagnostic technologies improves adherence to targeted or de-escalation therapy recommendations [22,23,24].
For example, the excellent reliability of MALDI-TOF in identifying bacteria in BCs exceeds the scope of validation studies, proving particularly high reliability for Enterobacterales [25, 26]. However, the reliability of MALDI-TOF was found to be lower in cases of polymicrobial bacteremia, where Gram-stain results are more informative. Therefore, even in the era of MALDI-TOF, it is necessary to perform direct Gram-stains for all positive BCs. The Gram-stain report is part of the routine management of BSIs. Although there have been numerous articles in recent years on the added value of MALDI-TOF for bacterial ID in BCs [27, 28], there is little data on the clinical impact of this new strategy. Vlek et al. [29] compared two consecutive periods in a prospective study: a standard period where only Gram-stain and AST results influenced antibiotic therapy, and an intervention period where MALDI-TOF was added to study its potential impact on empirical treatment. This latter study also demonstrated that incorporating MALDI-TOF in the BC process could effectively and quickly obtain information on infectious pathogens, enabling targeted treatment and providing maximum benefit for patients. This approach also plays a crucial role in curbing antimicrobial resistance, which has become a growing global concern in recent years. In 2019, the U.S. Centers for Disease Control and Prevention reported that over 2.8 million antibiotic-resistant infections occur annually in the United States, resulting in more than 35,000 deaths [30]. Carbapenem-resistant Enterobacterales and Enterobacterales producing extended-spectrum beta-lactamases (ESBL) are considered urgent and serious threats to the lives of infected individuals, respectively. Patients infected with resistant pathogens are known to be more likely to receive ineffective empirical antibiotic therapy. This empirical broad-spectrum therapy may promote further selection of antimicrobial resistance, increase toxicity, and lead to higher healthcare costs [31, 32] and is associated with adverse outcomes, including death [33]. Therefore, the use of MALDI-TOF can monitor the emergence and spread of resistant microorganisms in a timely manner [34].
Strategically, with the advantage of BacT/Alert Virtuo, BC bottles can be loaded into the instrument immediately, eliminating any delays. This streamlined workflow significantly reduced the time needed to obtain microbial results, promptly identified the infectious microorganism, and ultimately accelerated the de-escalation of empirical therapy [35]. It allows for timely obtaining test results to confirm the correctness (or otherwise) of the previous medication protocol, allowing for the adjustment of antibiotics within 24 h (upgrade/downgrade) to ensure patient safety to the greatest possible extent. Simultaneously, the use of resin-based medium – FA and FN Plus bottles – can better and earlier detect microorganisms, and are preferable for Gram-stain interpretation as well [36, 37]. Due to the antibiotic-adsorbing properties of the BacT/Alert PF Plus resin bottles, the positive detection rate for antibiotics was improved and the detection time shortened [38].
Additionally, comparing the time from the start of BSC/BSR to the pathogen-directed antibiotic treatment based on microbial reports before and after optimization revealed in the optimization group that 34.1% of patients received pathogen-directed antibiotic drugs based on the Gram-stain report with a median time of 41.92 h post-BSC, whereas before optimization only 28.9% of patients received pathogen-directed antibiotic treatment with a median time of 60.15 h. Similarly, a significant difference was also observed in the time intervals between BSC/BSR and the start of pathogen-directed antibiotic treatment between the two groups based on the first ID report. A median time of 40.63 h (BSC to first ID) and a median time of 25.55 h (BSR to first ID) were reduced post-op, respectively, which also indicated a significant schedule improvement in antibiotics treatment. Rapid adjustment of initial broad-spectrum empirical therapy is widely acknowledged as a benefit of accelerated diagnostics for BSIs globally [39, 40]. Earlier appropriate antibiotic therapy improves clinical cure rates and further reduces mortality [41, 42], with a median (IQR) time to antibiotic escalation from 61.7 h to 18.4 h. The 1-day gains in the present study were comparable to other studies that demonstrated a reduced time to optimal, narrow-spectrum therapy by ≥ 10 h [43, 44]. However, there is likely room for additional improvements as 65.9% of patients still did not receive pathogen-directed antibiotics within 24 h after reports despite optimized laboratory processes, probably due to the reports arriving just after the prescription issuance time, especially in non-ICU wards. Additionally, a difference was found between the time from BSR and BSC to the initiation of antibiotic treatment, indicating that blood samples were not tested promptly after collection. These findings highlights the need for continued coordination beyond the microbiology laboratory, such as enhancing the communication of results to clinicians and the involvement of antimicrobial stewardship personnel.
It also implies that faster diagnostics alone may significantly impact physicians’ antibiotic decisions or hospital workflows. Further optimization of procedures following ID reports should enhance antimicrobial stewardship through proactive review and provider recommendations rather than just passive rapid testing [45]. The antimicrobial stewardship team in our hospital consists of infectious control personnel, pharmacists, microbiologists and clinicians. Embedding microbiologists in clinical rounds will help to ensure swift and accurate clinical action once test results are available [46]. In our hospital, a phone call communication between microbiologists and physicians is common for acute cases. In addition, medical education and training provided by the team also contributes to more qualified sample collection and faster transportation. These findings suggests that the primary benefit of the intervention lies in the acceleration of the pre-analytical, analytical, as well as post-analytical phases.
Following microbiology diagnosis process optimization, patients experienced less examinations and lower antimicrobial drug costs, and shorter hospital stays by an average of 2.75 days, from 19.54 down to 16.79 days. A reduced length of stay provides significant cost savings for both the health system and the patient [47, 48]. Here, average total hospital costs were reduced by 13,174.91 CNY per patient after accounting for expenses related to medication, diagnostics, hospital bed occupancy and clinical procedures. The total antimicrobial drug usage costs were greatly reduced after optimization management, meaning that the capital expense of advanced diagnostic technology may be offset in the long term. It not only alleviates the pressure of diagnosis-related expenses but also saves antimicrobial costs from unnecessary medical treatment equipment consumption, potentially avoiding medical disputes caused by an excessive and unnecessary series of examinations. To ensure the smooth operation of faster diagnosis, hospitals require funding to support the procurement of several advanced automated devices for departments, inevitably increasing the costs of medical testing and adding to the department’s performance pressure. However, a full cost-benefit analysis would require factoring in the increased expense of such fixed laboratory costs.
Currently, the implementation of rapid molecular detection panels for BSIs has also led to a reduction in hospital stay lengths [49, 50]. These reductions are attributed to faster optimal and targeted antibiotic treatment. However, BC remains the clinical gold standard and is irreplaceable. Whether using molecular detection or incorporating MALDI-TOF, obtaining ID/AST results as quickly as possible is still necessary to meet clinical needs [51].
There were a number of limitations to our single-center, pre-post-study design. In particular, the small sample size may have reduced the general reliability and validity of our results. Consequently, the total duration of antibiotic usage, total hospitalization duration, total hospitalization and total laboratory costs did not reach statistical significance, likely due to the limited test power. The two groups were generally comparable at baseline demographically, though some clinical differences were noted. Adjustment for potential confounding factors was not conducted but would strengthen effect estimates. We did not evaluate the impact of AST report on antibiotics use between two periods, because the first ID and AST were reported at the same time in the pre-op group. We also did not analyze the increased fixed laboratory costs of new instruments and systems which was paid by the laboratory, because it did not impact on the expenses of patients’ in-hospital lab testing. In addition, patients with negative BC results in both the pre-op and post-op groups were not included. Finally, as it was not a randomized trial, unknown factors related to changing practice over time may also have played confounding roles.
Conclusions
Optimization measures, including new diagnostics technologies and workflow implementation in the microbiology laboratory, led to a reduced time to pathogen ID, timelier pathogen-directed antibiotic usage, shortened hospital stays and lower antimicrobial drug costs, which corresponded to less hospitalization costs for patients with BSIs. The BacT/Alert Virtuo BC system, the new resin anaerobic/aerobic BC bottles, VITEK MS (bioMérieux) and improved workflows represent valuable advances for patient outcomes and healthcare economics. However, realization of their full potential requires ongoing antimicrobial stewardship efforts and the need to address the remaining gaps in the clinical response to accelerated results. For example, the 9 am report needs to be much earlier in order to be available in all wards before morning rounds and the issuance of prescriptions, a more rapid process and 24-hour laboratory notifications should be considered for samples from the ICU.
Data availability
Original data are available on reasonable request from the corresponding author.
Abbreviations
- BSI:
-
Bloodstream infection
- BC:
-
Blood culture
- ID:
-
Identification
- PCR:
-
Polymerase chain reaction
- MALDI-TOF MS:
-
Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry
- HIS/HIT:
-
Hospital Information System/Health Information Technology
- ASTs:
-
Antimicrobial susceptibility tests
- LIS:
-
Laboratory Information System
- pre-op:
-
Pre-optimization
- post-op:
-
Post-optimization
- BSC:
-
Blood sample collection
- BSR:
-
Blood sample receipt
- TTRs:
-
Time to results
- ESBL:
-
Extended-spectrum beta-lactamases
References
Kern WV, Rieg S (2020) Burden of bacterial bloodstream infection-a brief update on epidemiology and significance of multidrug-resistant pathogens. Clin Microbiol Infect 26:151–157. https://doi.org/10.1016/j.cmi.2019.10.031
Liu BM, Carlisle CP, Fisher MA, Shakir SM (2021) The brief case: Capnocytophaga sputigena bacteremia in a 94-year-old male with type 2 diabetes mellitus, pancytopenia, and bronchopneumonia. J Clin Microbiol 59:e0247220. https://doi.org/10.1128/jcm.02472-20
Zhang Y, Du M, Johnston JM et al (2020) Estimating length of stay and inpatient charges attributable to hospital-acquired bloodstream infections. Antimicrob Resist Infect Control 9:137. https://doi.org/10.1186/s13756-020-00796-5
Gidey K, Gidey MT, Hailu BY, Gebreamlak ZB, Niriayo YL (2023) Clinical and economic burden of healthcare-associated infections: a prospective cohort study. PLoS ONE 18:e0282141. https://doi.org/10.1371/journal.pone.0282141
Verway M, Brown KA, Marchand-Austin A et al (2022) Prevalence and mortality associated with bloodstream organisms: a population-wide retrospective cohort study. J Clin Microbiol 60:e0242921. https://doi.org/10.1128/jcm.02429-21
Briggs N, Campbell S, Gupta S (2021) Advances in rapid diagnostics for bloodstream infections. Diagn Microbiol Infect Dis 99:115219. https://doi.org/10.1016/j.diagmicrobio.2020.115219
Fleming-Dutra KE, Hersh AL, Shapiro DJ et al (2016) Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA 315:1864–1873. https://doi.org/10.1001/jama.2016.4151
Zhao H, Wei L, Li H et al (2021) Appropriateness of antibiotic prescriptions in ambulatory care in China: a nationwide descriptive database study. Lancet Infect Dis 21:847–857. https://doi.org/10.1016/s1473-3099(20)30596-x
Pohl D, Keller PM, Bordier V, Wagner K (2019) Review of current diagnostic methods and advances in Helicobacter pylori diagnostics in the era of next generation sequencing. World J Gastroenterol 25:4629–4660. https://doi.org/10.3748/wjg.v25.i32.4629
Elbehiry A, Aldubaib M, Abalkhail A et al (2022) How MALDI-TOF mass spectrometry technology contributes to microbial infection control in healthcare settings. Vaccines (Basel) 10. https://doi.org/10.3390/vaccines10111881
Liu BM, Beck EM, Fisher MA (2021) The brief case: ventilator-associated corynebacterium accolens pneumonia in a patient with respiratory failure due to COVID-19. J Clin Microbiol 59:e0013721. https://doi.org/10.1128/jcm.00137-21
Peng Y, Liu B, Hou J et al (2015) Naturally occurring deletions/insertions in HBV core promoter tend to decrease in hepatitis B e antigen-positive chronic hepatitis B patients during antiviral therapy. Antivir Ther 20:623–632. https://doi.org/10.3851/imp2955
Liu B, Yang JX, Yan L, Zhuang H, Li T (2018) Novel HBV recombinants between genotypes B and C in 3’-terminal reverse transcriptase (RT) sequences are associated with enhanced viral DNA load, higher RT point mutation rates and place of birth among Chinese patients. Infect Genet Evol 57:26–35. https://doi.org/10.1016/j.meegid.2017.10.023
Liu BM, Rakhmanina NY, Yang Z, Bukrinsky MI (2024) Mpox (Monkeypox) virus and its co-infection with HIV, sexually transmitted infections, or bacterial superinfections: Double whammy or a new prime culprit? Viruses 16. https://doi.org/10.3390/v16050784
Liu B, Forman M, Valsamakis A (2019) Optimization and evaluation of a novel real-time RT-PCR test for detection of parechovirus in cerebrospinal fluid. J Virol Methods 272:113690. https://doi.org/10.1016/j.jviromet.2019.113690
Liu BM, Hill HR (2020) Role of host immune and inflammatory responses in COVID-19 cases with underlying primary immunodeficiency: a review. J Interferon Cytokine Res 40:549–554. https://doi.org/10.1089/jir.2020.0210
Koizumi Y, Sakanashi D, Ohno T et al (2019) The clinical characteristics of Acinetobacter bacteremia differ among genomospecies: a hospital-based retrospective comparative analysis of genotypically identified strains. J Microbiol Immunol Infect 52:966–972. https://doi.org/10.1016/j.jmii.2019.09.007
Kang FY, How CK, Wang YC et al (2020) Influence of severity of infection on the effect of appropriate antimicrobial therapy for Acinetobacter baumannii bacteremic pneumonia. Antimicrob Resist Infect Control 9:160. https://doi.org/10.1186/s13756-020-00824-4
Buehler SS, Madison B, Snyder SR et al (2016) Effectiveness of practices to increase timeliness of providing targeted therapy for inpatients with bloodstream infections: a laboratory medicine best practices systematic review and meta-analysis. Clin Microbiol Rev 29:59–103. https://doi.org/10.1128/cmr.00053-14
Charani E, Castro-Sanchez E, Sevdalis N et al (2013) Understanding the determinants of antimicrobial prescribing within hospitals: the role of prescribing etiquette. Clin Infect Dis 57:188–196. https://doi.org/10.1093/cid/cit212
Chavada R, Walker HN, Tong D, Murray A (2017) Changes in antimicrobial prescribing behavior after the introduction of the antimicrobial stewardship program: a pre- and post-intervention survey. Infect Dis Rep 9:7268. https://doi.org/10.4081/idr.2017.7268
Nasef R, El Lababidi R, Alatoom A, Krishnaprasad S, Bonilla F (2020) The impact of integrating rapid PCR-based blood culture identification panel to an established antimicrobial stewardship program in the United Arab of Emirates. Int J Infect Dis 91:124–128. https://doi.org/10.1016/j.ijid.2019.11.028
Hogan CA, Ebunji B, Watz N et al (2020) Impact of rapid antimicrobial susceptibility testing in Gram-negative rod bacteremia: a quasi-experimental study. J Clin Microbiol 58. https://doi.org/10.1128/jcm.00360-20
Ehren K, Meißner A, Jazmati N et al (2020) Clinical impact of rapid species identification from positive blood cultures with same-day phenotypic antimicrobial susceptibility testing on the management and outcome of bloodstream infections. Clin Infect Dis 70:1285–1293. https://doi.org/10.1093/cid/ciz406
Stevenson LG, Drake SK, Murray PR (2010) Rapid identification of bacteria in positive blood culture broths by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol 48:444–447. https://doi.org/10.1128/jcm.01541-09
Prod’hom G, Bizzini A, Durussel C, Bille J, Greub G (2010) Matrix-assisted laser desorption ionization-time of flight mass spectrometry for direct bacterial identification from positive blood culture pellets. J Clin Microbiol 48:1481–1483. https://doi.org/10.1128/jcm.01780-09
Croxatto A, Prod’hom G, Greub G (2012) Applications of MALDI-TOF mass spectrometry in clinical diagnostic microbiology. FEMS Microbiol Rev 36:380–407. https://doi.org/10.1111/j.1574-6976.2011.00298.x
Drancourt M (2010) Detection of microorganisms in blood specimens using matrix-assisted laser desorption ionization time-of-flight mass spectrometry: a review. Clin Microbiol Infect 16:1620–1625. https://doi.org/10.1111/j.1469-0691.2010.03290.x
Vlek AL, Bonten MJ, Boel CH (2012) Direct matrix-assisted laser desorption ionization time-of-flight mass spectrometry improves appropriateness of antibiotic treatment of bacteremia. PLoS ONE 7:e32589. https://doi.org/10.1371/journal.pone.0032589
Centers for Disease Control and Prevention (U.S.); National Center for Emerging Zoonotic and Infectious Diseases (U.S.). Division of Healthcare Quality Promotion. Antibiotic Resistance Coordination and Strategy Unit (2019) Antibiotic resistance threats in the United States, 2019. https://stacks.cdc.gov/view/cdc/82532. Accessed 21 June 2024
Smith R, Coast J (2013) The true cost of antimicrobial resistance. BMJ 346:f1493. https://doi.org/10.1136/bmj.f1493
Chang CY, Schiano TD (2007) Review article: drug hepatotoxicity. Aliment Pharmacol Ther 25:1135–1151. https://doi.org/10.1111/j.1365-2036.2007.03307.x
Kollef MH (2008) Broad-spectrum antimicrobials and the treatment of serious bacterial infections: getting it right up front. Clin Infect Dis 47(Suppl 1):S3–13. https://doi.org/10.1086/590061
Benkova M, Soukup O, Marek J (2020) Antimicrobial susceptibility testing: currently used methods and devices and the near future in clinical practice. J Appl Microbiol 129:806–822. https://doi.org/10.1111/jam.14704
Adamik M, Hutchins A, Mangilit J, Katzin B, Totty H, Deol P (2021) Effect of delayed entry on performance of the BACT/ALERT FAN PLUS bottles in the BACT/ALERT VIRTUO blood culture system. Eur J Clin Microbiol Infect Dis 40:699–705. https://doi.org/10.1007/s10096-020-04042-z
Kirn TJ, Mirrett S, Reller LB, Weinstein MP (2014) Controlled clinical comparison of BacT/alert FA plus and FN plus blood culture media with BacT/alert FA and FN blood culture media. J Clin Microbiol 52:839–843. https://doi.org/10.1128/jcm.03063-13
Giordano L, Liotti FM, Menchinelli G et al (2021) Simulated pediatric blood cultures to assess the inactivation of clinically relevant antimicrobial drug concentrations in resin-containing bottles. Front Cell Infect Microbiol 11:649769. https://doi.org/10.3389/fcimb.2021.649769
Spaargaren J, van Boven CP, Voorn GP (1998) Effectiveness of resins in neutralizing antibiotic activities in bactec plus Aerobic/F culture medium. J Clin Microbiol 36:3731–3733. https://doi.org/10.1128/jcm.36.12.3731-3733.1998
Dellit TH, Owens RC, McGowan JE Jr et al (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44:159–177. https://doi.org/10.1086/510393
Habboush Y, Guzman N, StatPearls (2023) Jun Treasure Island (FL): StatPearls Publishing; 20
Tacconelli E, Mazzaferri F, de Smet AM et al (2019) ESCMID-EUCIC clinical guidelines on decolonization of multidrug-resistant Gram-negative bacteria carriers. Clin Microbiol Infect 25:807–817. https://doi.org/10.1016/j.cmi.2019.01.005
Vink J, Edgeworth J, Bailey SL (2020) Acquisition of MDR-GNB in hospital settings: a systematic review and meta-analysis focusing on ESBL-E. J Hosp Infect 106:419–428. https://doi.org/10.1016/j.jhin.2020.09.006
Banerjee R, Teng CB, Cunningham SA et al (2015) Randomized trial of rapid multiplex polymerase chain reaction-based blood culture identification and susceptibility testing. Clin Infect Dis 61:1071–1080. https://doi.org/10.1093/cid/civ447
Banerjee R, Komarow L, Virk A et al (2021) Randomized trial evaluating clinical impact of RAPid IDentification and susceptibility testing for Gram-negative bacteremia: RAPIDS-GN. Clin Infect Dis 73:e39–e46. https://doi.org/10.1093/cid/ciaa528
Timbrook TT, Morton JB, McConeghy KW, Caffrey AR, Mylonakis E, LaPlante KL (2017) The effect of molecular rapid diagnostic testing on clinical outcomes in bloodstream infections: a systematic review and meta-analysis. Clin Infect Dis 64:15–23. https://doi.org/10.1093/cid/ciw649
Kuwabara G, Yukawa S, Yamada K et al (2020) The effect of intervention by an antimicrobial stewardship team on anaerobic bacteremia. Anaerobe 64:102214. https://doi.org/10.1016/j.anaerobe.2020.102214
Pliakos EE, Andreatos N, Shehadeh F, Ziakas PD, Mylonakis E (2018) The cost-effectiveness of rapid diagnostic testing for the diagnosis of bloodstream infections with or without antimicrobial stewardship. Clin Microbiol Rev 31. https://doi.org/10.1128/cmr.00095-17
Sakarikou C, Altieri A, Bossa MC et al (2018) Rapid and cost-effective identification and antimicrobial susceptibility testing in patients with Gram-negative bacteremia directly from blood-culture fluid. J Microbiol Methods 146:7–12. https://doi.org/10.1016/j.mimet.2018.01.012
Yoo IY, Han J, Ha SI, Cha YJ, Pil SD, Park YJ (2021) Clinical performance of ASTA SepsiPrep kit in direct bacterial identification and antimicrobial susceptibility test using MicroIDSys Elite and VITEK-2 system. J Clin Lab Anal 35:e23744. https://doi.org/10.1002/jcla.23744
Watanabe N, Koyama S, Taji Y, Mitsutake K, Ebihara Y (2022) Direct microorganism species identification and antimicrobial susceptibility tests from positive blood culture bottles using rapid Sepsityper Kit. J Infect Chemother 28:563–568. https://doi.org/10.1016/j.jiac.2021.12.030
Liu W, Liao K, Wu J et al (2024) Blood culture quality and turnaround time of clinical microbiology laboratories in Chinese teaching hospitals: a multicenter study. J Clin Lab Anal 38:e25008. https://doi.org/10.1002/jcla.25008
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Genwei Ai: Conceptualization, Formal analysis, Investigation, Resources, Writing – Original Draft, Writing – Review & Editing, Visualization, Supervision, Projection administration. Ying Zhang, Kunshan Guo, Lu Zhao, Zhi Li, He Hai, Erjuan Jia and Junying Liu: Investigation, Writing – Review & Editing, Visualization. All authors have read and approved the current version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All research was conducted in accordance with both the Declarations of Helsinki and Istanbul. The study was approved by the Ethical Committee of Xuchang Central Hospital.
Consent to participate
Informed consent was not applicable as clinical records without any personally identifiable information were retrieved for analyses.
Consent to publish
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ai, G., Zhang, Y., Guo, K. et al. The impact of optimizing microbial diagnosis processes on clinical and healthcare economic outcomes in hospitalized patients with bloodstream infections. Eur J Clin Microbiol Infect Dis (2024). https://doi.org/10.1007/s10096-024-04928-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10096-024-04928-2