Abstract
For patients with bloodstream infections, rapid initiation of the appropriate antimicrobial therapy is essential in reducing mortality and morbidity. New developments and automation in clinical microbiology labs speed up the identification and susceptibility results but are expensive. To gain insight in the added value of the new workflows, we simulated the possible impact of rapid identification and susceptibility tests on a real-life cohort of 158 positive blood culture episodes. Our routine workflow was theoretically challenged against two new workflows, one based on rapid identification with MALDI-TOF MS and one based on molecular testing. First, we observed an important role of the rapid communication of the gram stain results, as about one third of patients needed an adaptation of the antimicrobial therapy based on these results. Antibiotic adaptation based on the microorganism identification was necessary in 10% and in another 25% of cases after the availability of the susceptibility results. The added value of the newer workflow methods lies mainly in the field of the rapid identification and was rather limited in our cohort. In conclusion, for optimizing the blood culture workflow, each microbiology lab should critically scan its own workflow and know its own blood culture epidemiology, before investing in expensive or time-consuming processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thanks to automation and direct identification (protein- or nucleic acid-based), clinical bacteriology labs have sped up diagnostic workflow over the past 10 years [1]. These evolutions have increased the impact of diagnostic bacteriology on patient care and led to new laboratory workflows. However, cost-effectiveness of the implementation of new workflows in a microbiology department should be investigated. As the sample-to-result time is affected by the consecutive steps in the workflow, the investment in expensive technology might be ineffective or unnecessary if most cost-effective measures to optimize these steps are not taken first.
For patients with bloodstream infections (BSI), timely initiation of appropriate antibiotic therapy is of utmost importance. Several studies have reported higher mortality, morbidity, length of stay, and costs in patient groups not receiving appropriate antibiotic treatment [2, 3]. Systematic use of broad-spectrum antibiotics in the empirical setting is to be avoided because of toxicity and resistance selection pressure on pathogens and host flora. Instead, timely bacteriology results and well-chosen workflows can promote targeted antibiotic therapy.
BSI are still diagnosed by means of blood cultures, ideally collected before administration of antibiotics. The classical workflow of the blood culture consists of incubation followed by, once the culture has been flagged positive by the continuous growth monitoring incubator, Gram stain, subculture, identification (ID), and antibiotic susceptibility testing (AST). Most microbiology laboratories communicate the results of the Gram stain of positive blood cultures directly to the attending clinician. The impact of this approach on mortality rates was demonstrated by Barenfanger et al. who showed a significant lower crude mortality when the turnaround time (TAT) of the Gram stain result was less than 1 h [4]. Follow-up communication on the ID or AST is essential to tailor empirical therapy.
The recent revolution in microbiological diagnostic workflows is applied in BSI diagnostic processing. An exhaustive overview of newly introduced techniques goes beyond the scope of this work, but roughly two workflow trends can be distinguished [1]. The first consists of rapid molecular tests performed on blood cultures flagged positive, targeting some of the most prevalent pathogens and resistance genes. The second uses matrix assisted laser desorption/ionization time of flight mass spectrometry (MALDI-TOF MS) on blood cultures flagged positive as a tool to decrease turnaround time (TAT) of ID and in some cases AST.
To guide the choice of workflow, it is important for laboratories to analyze their BSI diagnostic approach, in order to identify most significant gains in time to impact on therapy. We simulated and studied several possible strategies on a real-life subset of positive blood cultures, in order to identify the change(s) in workflow with the biggest impact on TAT at an acceptable cost. A similar strategy could be used by diagnostic laboratories to find an acceptable cost/benefit balance in improvement of BSI diagnostics.
Materials and methods
Study design
We performed a retrospective observational study in the Ghent University Hospital, a tertiary care academic hospital with 1000 beds. Over a period of 4 months (April to August 2015), we analyzed the workflow of 158 positive blood culture episodes in 149 patients. A positive blood culture episode is defined as a whole of positive blood cultures with the same pathogen, from the same origin and within a 14-day period. On this random sample, we simulated the possible impact of different workflow changes from a diagnostic, therapeutic, and financial point of view.
The study was approved by the local Ethical Committee (B670201524756).
Standard local workflow
BSI samples are accepted around the clock. The continuity of processing depends on the shift of the moment. During day time shift (8 AM–5 PM, shift 1), a team of specialized bacteriology technicians is present to perform the different steps of the process. During the evening shift (5 PM–10 PM, shift 2), one partially specialized technician is available. During the night shift (10 PM–8 AM, shift 3), technicians present do not have specialized microbiological skills and positive blood cultures are not processed. Because the shifts obviously impact the workflow, the results of our study will be discussed separately for each shift.
BacT/ALERT FA Plus and BacT/ALERT SN bottles (bioMérieux, Durham, USA) are used for the detection of BSI. After arrival at the lab, blood culture bottles are incubated in the BacT/ALERT® 3D (bioMérieux, Durham, USA), a continuous growth monitoring incubator. During shifts 1 and 2, incubation is started immediately after arrival, while in shift 3, bottles are loaded in no later than 4 h after arrival in the lab. When a blood culture bottle is flagged for growth, a Gram stain is performed by a specialized microbiology technician and the results are communicated by phone to the attending physician, immediately (shift 1) or the next morning (shifts 2 and 3).
The results of the Gram stain are used to direct the further workflow, i.e., choice of appropriate growth media for subculture and selection of a predefined set of antibiotics or antifungals for AST, immediately (shift 1) or the next morning (shift 3). During shift 2, subcultures and AST tests are initiated but not guided by Gram staining results. In this way, final ID using MALDI-TOF MS (Bruker Daltonik GmbH, Bremen, Germany) and direct AST results are available within 10 to 24 h after detection of growth, depending on the moment during the day at which the bottle becomes positive. Direct AST (without previous subculture) is performed with disk diffusion and automated reading with ADAGIO (Bio-Rad, Hercules, USA) using EUCAST breakpoints. In addition, between 08:00 AM and 01:00 PM (first part of shift 1), MALDI-TOF MS following short incubation (6 h at 35 °C and 5% CO2) of one drop of blood on a blood agar is performed on all positive blood culture bottles flagged positive. This reduces the time to ID (Fig. 1).
To study the impact of the (partial) results on therapeutic decisions, we monitored timing of telephonic communication, reporting of results in the laboratory and hospital information system, and the electronic prescription of antibiotics for each BSI episode.
Other diagnostic workflows
We simulated the effects of two new workflows on our data set of positive cultures.
The first one simulated the impact of rapid ID with MALDI-TOF MS directly on positive blood cultures (direct MALDI-TOF MS). By means of a test cohort (n = 154), we evaluated two protocols for this approach: the MALDI Sepsityper kit (Bruker Daltonik GmbH, Bremen, Germany) and a washing procedure [5]. For the protocol with MALDI Sepsityper, we worked according to the manufacturer’s instructions. In the washing procedure, we centrifuged 6 mL blood for 10 min at 250 g. Four milliliters of supernatant was diluted with 2 mL of sterile deionized water and centrifuged for 5 min at 1000g. The pellet was diluted in 1 mL sterile deionized water and then washed in ethanol. The dried pellet was finally dissolved in a 1/1 dilution of 70% formic acid and acetonitrile. The results from this study cohort were then extrapolated to simulate our 158 episodes dataset.
The second simulation explored the theoretical impact of multiplex PCR on positive blood cultures (direct multiplex PCR). We selected the SeptiFast kit (Roche Diagnostics, Mannheim, Germany) and the Biofire Blood Culture Identification Panel (BioMérieux, Marcy-l’Etoile, France), both commercially available kits for detection of several microorganisms as well as resistance genes. The coverage of both kits is summarized in Table 1.
Hands-on time of the different workflows and the estimated cost of the consumables were included in the evaluation.
Statistical analyses
All statistical analyses were performed in SPSS statistics 24. For the calculation of significance, we used the Mann-Whitney test.
Results
Distribution of species and time to positivity of blood cultures
The mean time to positivity (TTP) for the 158 blood cultures was 13 h and 16 min, with a median of 12 h and 33 min. In 151 bottles, only 1 microorganism grew, while 7 cultures were polymicrobial.
Figure 2 gives an overview of the distribution of the species recovered and their median TTP.
Timing of blood culture arrival and intervals to incubation
Of all 158 blood culture bottles included in the study, 47% arrived in the lab during shift 1, 27% during shift 2, and 26% arrived during shift 3. Figure 3a shows the distribution of the delays to incubation during the three shifts. About half of daytime bottles (45%) were loaded within 1 h upon arrival in the lab, 87% within 2 h upon arrival. Nine bottles (20%) which arrived during shift 2 were incubated within 1 h after arrival and 14 within 2 h (32%). Of the night bottles (shift 3), 20 were incubated within 2 h (48%) and 37 within 4 h (90%).
We checked whether delayed incubation had an impact on the TTP in the different groups (Fig. 3b). No significant impact on TTP (from loading to flagging for positivity) could be observed.
Time and content of preliminary reports after flagging
In many microbiology labs, the effectiveness of processing positive blood culture bottles is highly dependent on the moment during the day the bottle is flagged positive. In our standard workflow, 29/56 bottles flagged during daytime (shift 1) could be processed before 01:00PM, with ID result the same day. The remaining 27/56 bottles were flagged positive in the afternoon and were processed the same day, but pathogen was only identified the next day. This was also the case for the blood cultures which became positive in the evening shift 2 (n = 19). The 83 night shift 3 positive flags were not processed until the next daytime shift 1.
The first results of a positive blood culture consist of the Gram stain, which is reported and discussed over phone by the microbiologist with the attending clinician during daytime shift. The mean period from Gram result to phone call was 44 min (no differences between shifts as Gram stains are only performed in shift 1). However, important differences are observed in the different shifts for the mean interval between flagging of the positive blood culture and reporting the result of the gram stain: 42 min, 6 h, and 14 h in shifts 1, 3, and 2 respectively. In 18% of cases, the patient did not receive any antibiotic or antifungal (9/10 cases where the Gram stain revealed yeasts) treatment at the time of communication of the Gram stain result. In 15% of the patients already treated with antibiotic/antifungal therapy, a switch or association was needed, based on the Gram stain result. This was mainly due to the presence of Gram-positive cocci when only Gram-negatives were covered by the antibiotic spectrum, or the need for initiation of an antifungal when yeasts were observed. Thus, one third of patients with a BSI needed an adaption or initiation of antibiotic therapy based on the first results of the Gram stain. In all cases, the adaptation consisted of a switch or an escalation in antibiotic spectrum, never de-escalation. The recommended therapeutic changes were started within the same day in 87% of cases and within 2 h in 50% of cases. In 59% of patients, the empirical therapy seemed well targeted and did not need adaptation based on the Gram stain result. Finally, in 5% of patients, no treatment was needed because of the clinical context. Figure 4 gives an overview of these results.
Timelines and impact of the ID results
ID of microorganisms growing in blood cultures is performed on subculture. For all cultures becoming positive during night (shift 3) and before 1:00 PM (shift 1), a direct early subculture of a droplet of blood (not streaked out) incubated on a plate is used. Obviously, for mixed cultures and fastidious species, this technique is less suitable. For the subgroup of 112 positive cultures for which this direct subculture technique was used, ID was achieved within the same working day in 88% of cases. Antibiotic adaptation based on the microorganism ID was necessary in 10% of these.
For all other cultures (flagged positive after 1:00 PM (shift 1) or evening (shift 2)), ID was available the next morning after standard subculture (median time 21 h and 43 min), necessitating therapeutic adaptations in 20% of cases compared to what was or would be advised based on Gram result (shifts 1 and 2 respectively).
Within the cases needing antibiotic adaptation incited by identification, switch was recommended because of known intrinsic or epidemiologically probable resistance of the isolated species in six patients. The other 14 adaptations aimed to de-escalate based on the ID and antigen testing results (for instance when a PBP2a-negative Staphylococcus aureus was isolated, vancomycin could be stopped, and flucloxacillin was started). The global acceptance rate of antimicrobial advice based on ID results was 80%.
Timelines and impact of the AST
For AST, standard duration of incubation is required to avoid errors and misinterpretation of the results. Therefore, the median time from positivity to AST results remains rather long, despite the fact that direct inoculation from positive blood culture is validated and commonly in use, except for yeasts [6]. The median period of time from growth detection in the blood culture to AST results was 21 h and 43 min for bacteria and 53 h and 44 min for yeasts, because of the need for AST subculture of the last group.
Overall, in 25% of cases an adaptation of the antibiotic treatment due to AST results was recommended (de-escalation for susceptible strains, 17%) or warranted (escalation because of resistance to the (semi-)empirical treatment, 8%). The real impact of the AST results was somewhat lower (19% of total), because an antibiotic adaptation was only performed by the clinician in 75% of all eligible patients. Fortunately, escalation was performed in all eligible cases.
Timelines and estimated impact of simulated new workflows
Finally, we simulated the impact of introduction of alternative technologies on the workflows. For the first workflow simulation (rapid ID with MALDI-TOF MS), we conducted a pilot study, comparing the MALDI Sepsityper kit and a washing procedure. Overall, in comparison with the standard workflow (considered gold standard), we found reliable and correct IDs in 64% with the MALDI Sepsityper and 50% with the washing procedure. Difference in performance between Sepsityper and washing was most obvious for the identification of yeasts (Fig. 5). Applying these performances on our study population, thus taking the final ID into account, this workflow could maximally lead to 60% and 46% confirmed IDs of monobacterial BSI with the MALDI Sepsityper and washing procedure respectively. In comparison, the current rapid ID workflow with MALDI-TOF MS leads to correct identification in 88% of positive cultures but can only be performed on a subgroup of 112 samples (see point 4.) thus yielding 99 correct and rapid IDs. Hence, only the Sepsityper protocol could lead to comparable results when performed on al positive bottles around the clock. In comparison, the use of the standard workflow in shifts 1 and 2 would result in 35% (26/75) correct identifications after short incubation. Hence, only the Sepsityper protocol could lead to gain in ID results.
When a positive culture is processed, hands-on time is about 15 min for the MALDI Sepsityper and 30 min for the washing procedure with time to results of 20 and 35 min respectively when one sample is processed. Considering both extra labor cost and reagent costs, in most countries applying MALDI-TOF nowadays, both protocols will demand comparable financial efforts. Real-cost calculations depend on number of tests performed and regional reimbursement modalities.
In the second workflow simulation, the performance of direct PCR on positive blood cultures was simulated on our population of positive cultures. We assumed a 100% identification rate on monobacterial cultures (n = 146) for which the ID was included in the target panel. On this subset, SeptiFast and BioFire would give an ID in 88% and 75% of monobacterial blood cultures respectively. The main reason for this difference is the fact that SeptiFast can identify coagulase-negative staphylococci while BioFire cannot. Another important difference is that SeptiFast can differentiate Enterococcus faecalis from E. faecium, whereas BioFire identifies both as Enterococcus spp. In the calculation of reliable IDs, all E. faecalis and E. faecium were also considered as correctly identified with BioFire.
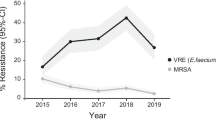
Resistance would be retrieved in 1 of 146 monobacterial cultures with both multiplexes (one methicillin-resistant Staphylococcus aureus (MRSA)), as no vancomycin-resistant enterococci or KPC carbapenemase-producing Enterobacteriaceae were present in the cohort.
Hands-on time and time to result are about 2 and 60 min for BioFire, while it is about 30 min and up to 6 h for SeptiFast. From financial point of view, the molecular techniques are estimated to be about five to ten times more expensive than the MALDI-TOF MS-based ones.
Discussion
When microbiology labs face investment in workflow automation, a critical analysis of the workflow is warranted to identify possible gains in turnaround time at acceptable cost. We analyzed our blood culture process and simulated the effect of introduction of innovative protocols by challenging them with a real-life positive blood culture data set.
Blood cultures arrive 24/7 in the lab and are flagged positive around the clock. Because specialized bacteriology technicians are not present all the time, delays in the preliminary reporting occur. During day shifts, preliminary reports of Gram stains of positive blood culture bottles are considered a priority, resulting in very short reporting delays. The importance of these Gram stain result is illustrated by the fact that about one third of positive blood cultures incited an antibiotic initiation or switch, based on the Gram stain result, mostly due to the presence of Gram-positives or yeasts. This is a higher number compared to the study of Scarsi et al., where only 14% of antibiotics regimens were inappropriate. However, in this study, only Gram-negative BSI were included [7].
In order to overcome the large delay of the communication of these important Gram stain results during evening and night shifts, the corresponding team could be complemented with microbiology experienced technicians or an automated microscope to generate the Gram stain results. These results are of course only useful when communicated to the physician on call who then adapts antimicrobial therapy promptly, even during the night. In our analysis, antibiotic stewardship recommendations based on Gram stain results were communicated in 33% of patients, which were implemented in 92% of them.
Regarding the ID results, only 10% of cases necessitated antimicrobial therapy adaptations based on the ID: S. aureus (with immediate PBP2a test to guide towards β-lactam versus glycopeptides), Pseudomonas aeruginosa or E. faecium.
In the study of Huang et al., the possible impact of ID results on antibiotic therapy adaptations was much higher than in our analysis (36% versus 10% eligible ID results) which can partly be explained by a higher percentage of S. aureus and E. faecium in that study [8], stressing the importance of knowledge of local epidemiology.
The new ID strategies we simulated on our cohort demand considerable manual intervention making them hard to implement for every single bottle flagged. Importantly, only in 10% of our study population, the ID (in addition to the Gram staining result already known) resulted in an advice to change the antibiotic treatment.
The costs should be balanced against the clinical benefit for the patient and the impact on antibiotic consumption. In a recent retrospective analysis investigating the impact of multiplex PCR on antimicrobial use in a setting with a well-established antimicrobial stewardship program for BSI, a non-significant reduction of costs was observed as a result of earlier antibiotic de-escalation [9].
The median time between positivity and reporting of AST results was 21 h for bacteria, which is similar [10] or even much shorter [8, 9] compared to other reports. In our standard workflow, antimicrobial stewardship based on AST results was needed in a quarter of cases and accepted in 75%. Recommendations to escalate therapy were accepted more often than de-escalation. When compared with the analysis of Huang, both the opportunity (39% versus 25%) and the acceptance rate (96% versus 75%) are lower in our setting [8]. Differences in local resistance rates were not compared, but might be an explanation for this observation. Indeed, in settings with higher prevalence of MRSA, vancomycin-resistant enterococci (VRE), or carbapenemase-producing Enterobacteriaceae, the impact of the AST is considered to be higher. Also, the impact of the detection of resistance genes in direct multiplex PCR will be much higher and may advocate the investment. In low prevalence settings however, detection of PBP2a on S. aureus cultures may be an acceptable alternative. For this decision, the number needed to analyze with direct multiplex PCR, in order to detect 1 MRSA or VRE, should be based on local epidemiology.
Our study has some limitations. First, the size of the studied population is rather small, although the most abundant pathogens are present in a distribution which is representative for the total distribution of blood culture isolates in our center. Next, we did not study any impact of the antimicrobial stewardship interventions on outcome of the individual patient nor on possible cost savings or savings in antibiotic use. However, this was not the intention of the study as we wanted to identify possible impact of direct ID methods on improvement of the microbiology lab workflow. Finally, each laboratory and hospital has their own specific number of staff members, which also impacts the feasibility of complex and demanding workflows. This was not taken into account in this analysis.
In conclusion, our results show that a positive impact of decreasing time from sample to therapy can be reached by round the clock start of culture of bottles and plating of bottles flagged positive for ID and AST, together with Gram staining which has a remarkable large impact on therapeutic decisions. Direct ID on bottles flagged positive has only a marginal effect, which should be balanced against cost and labor to implement 24/7 molecular diagnostics or direct MALDI-TOF MS. Gram staining on the other hand is simple and easily automated; images can be made by a non-specialized technician, e.g., wired to a microbiologist on call at night who discusses impact with physician on call.
In the preparatory phase of optimizing the blood culture workflow, each microbiology lab should critically scan its own workflow and know its own blood culture epidemiology, before investing in expensive or time-consuming processes.
References
Opota O, Croxatto A, Prod’hom G, Greub G (2015) Blood culture-based diagnosis of bacteraemia: state of the art. CMI 21(4):313–322
Trenholme GM, Kaplan RL, Karakusis PH, Stine T, Fuhrer J, Landau W, Levin S (1989) Clinical impact of rapid identification and susceptibility testing of bacterial blood culture isolates. J Clin Microbiol 27:1342–1345
Kumar A, Roberts D, Wood KE, Light B, Parrilo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34:1589–1596
Barenfanger J, Graham DR, Kolluri L, Sangwan G, Lawhorn J, Drake CA, Verhulst SJ, Peterson R, Moja LB, Ertmoed MM, Moja AB, Shevlin DW, Vautrain R, Callahan CD (2008) Decreased mortality associated with prompt Gram staining of blood cultures. Am J Clin Pathol 130:870–876
Christner M, Rohde H et al (2010) Rapid identification of bacteria from positive blood culture bottles by use of matrix-assisted laser desorption-ionization time of flight mass spectrometry fingerprinting. J Clin Microbiol 48(5):1584–1591
Doern GV, Scott DR, Rashad AL (1982) Clinical impact of rapid antimicrobial susceptibility testing of blood culture isolates. Antimicrob Agents Chemother 21(6):1023–1024
Scarsi KK, Feinglass JM, Scheetz MH, Postelnick MJ, Bolon MK, Noskin GA (2006) Impact of inactive empiric antimicrobial therapy on inpatient mortality and length of stay. Antimicrob Agents Chemother 50(10):3355–3360
Huang AM, Newton D, Kunapuli A, Gandhi TN, Washer LL, Isip J, Collins CD, Nagel JL (2013) Impact of rapid organism identification via Matrix-Assisted Laser Desorption/Ionization Time-of-Flight combined with antimicrobial stewardship team intervention in adult patients with bacteremia and candidemia. CID 57:1237–1245
MacVane SH, Nolte FS (2016) Benefits of adding a rapid PCR-based blood culture identification panel to an established antimicrobial stewardship program. JCM 54(10):2455–2463
Perez KK, Olsen RJ, Musick WL, Cernoch PL, Davis JR, Peterson LE, Musser JM (2014) Integrating rapid diagnostics and antimicrobial stewardship improves outcomes in patients with antibiotic-resistant Gram-negative bacteremia. J of Infection 69:216–225
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained from the local Medical Ethics Committee (B670201524756).
Informed consent
Not obtained. This is a retrospective registration study.
Rights and permissions
About this article
Cite this article
Cattoir, L., Coorevits, L., Leroux-Roels, I. et al. Improving timelines in reporting results from positive blood cultures: simulation of impact of rapid identification on therapy on a real-life cohort. Eur J Clin Microbiol Infect Dis 37, 2253–2260 (2018). https://doi.org/10.1007/s10096-018-3366-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3366-8