Abstract
An autochthonous case of lymphocutaneous sporotrichosis caused by Sporothrix schenckii is reported. The patient developed skin lesions localized along the lymphatics that appeared after he suffered an injury while collecting wicker canes in marshy water. The fungus was identified as Sporothrix schenckii by MALDI-TOF and sequencing. Phylogenetic analysis was also performed. Low MIC values were detected for all tested echinocandins and azoles except for fluconazole. The patient was treated with itraconazole without significant improvement. A regression of lesions was observed after 3 months of therapy with voriconazole. Few cases of sporotrichosis have been reported in Europe. However, several cases of sporotrichosis have been described in Italy. The incidence of sporotrichosis in Italy may be underestimated and microbiologists, and clinicians must be aware of this fungal infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sporothrix schenckii is a dimorphic fungus able to cause infections in humans. S. schenckii can be isolated from soil and plant matter. Sporotrichosis occurs after traumatic acquisition of the fungus from the environment. There is an occupational risk for gardeners, mineworkers, and florists [1,2,3]. Lymphocutaneous sporotrichosis is the most common form seen in clinical practice. Sporotrichosis has a worldwide distribution, and the majority of cases are reported from tropical and subtropical regions of the Americas. The disease is rare in Europe [2,3,4]. We describe an autochthonous case of lymphocutaneous sporotrichosis in an Italian patient.
Case report
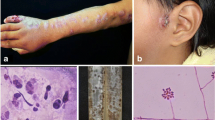
A 49-year-old male nurse, living in Apulia, Southern Italy, was admitted to the Clinic of Infectious Diseases of Bari, Italy, due to the appearance of multiple ulcerative nodules on his right hand and forearm. The lesions had appeared 1 month previously after an injury that occurred while he was collecting canes for basket weaving in marshy water. Before coming to our attention, an empiric antimicrobial therapy with clarithromycin and amoxicillin-clavulanate had been started with no clinical improvement. At clinical examination of the skin, multiple lesions in different stages of evolution were seen. Secondary lesions along lymphatic channels proximal to the original lesion were also seen (Fig. 1). Laboratory data were in the normal range. Because of the anamnestic data, infection by Mycobacterium spp. was suspected, and a therapy with ethambutol and clarithromycin was started.
Sporotrichosis. a picture at the first visit: purplish nodular lesions with a linear distribution on the right hand and forearm. b After 4 weeks: further ulceration of the lesions appeared. c Picture after 40 days: good improvement of the lesions during treatment with voriconazole. d Improvement of lesions after further 40 days of therapy
Several swabs from the lesions were obtained. Unfortunately, no direct microscopic examination of the sample was performed. Cultures were negative for fungi and bacteria, and no Mycobacterium spp. was detected by molecular methods. Since no improvement was observed, a mycotic infection was suspected, and several swabs were again taken from the lesions. Direct microscopic examination revealed the presence of oval and elliptical budding yeast cells. The samples were cultured in Sabouraud broth and agar and the plate were incubated at 30 °C. The presence of cream colored, smooth, and verrucous colonies was detected. The colonies became dark in the center, radiated with hyaline and dematiaceous conidia. The microscopic examination revealed the presence of delicate hyaline, dematiaceous, and septate hyphae. Small round or oval microconidia were present laterally along the hyphae with flower-like arrangement at the tip of the branched hyphae, and the sympodial conidiogenesis was observed.
The isolation of Sporothrix spp. was suspected. Subsequently, the mold was plated on blood agar and incubated at 37 °C. Yeast cream-colored colonies developed and the microscopic examination showed round, oval cigar-shaped budding yeasts.
The identification was performed by matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry and by partial sequencing of the internal transcribed regions (ITS) and the calmodulin-encoding gene, according to previous studies [1, 5].
The calmodulin sequence obtained in this study has been deposited in the GenBank database (accession number MN101820). Phylogenetic analysis was conducted with the MEGA7 software (www.megasoftware.net) using reference calmodulin-sequences from all members of the pathogenic clade. Results of the phylogenetic analysis confirmed the identification as S. schenckii sensu stricto by grouping our fungal strain into the S. schenckii clade IIa originally described by Marimon et al. (Fig. 2) [6]. The S. schenckii strain recovered in this study has been deposited at the Westerdijk Fungal Biodiversity institute, The Netherlands, as CBS 145945.
Phylogenetic analysis. Evolutionary relationships of S. schenckii CBS145945 isolated in this study with other members of the pathogenic clade and related environmental Sporothrix species. The tree was generated using the calmodulin sequences and the neighbor-joining method. The percentage of replicate trees in which the associated taxa clustered together in the bootstrap test (1000 replicates) are shown above the branches
An antifungal susceptibility test was performed at the Fondazione Policlinico Gemelli, IRCCS, Rome, Italy, using the Sensititre™YeastOne™ Y09-AST plate. Reading was carried out after 72 h of incubation time. Results were as follows: amphotericin B 1 mg/L, anidulafungin 0.03 mg/L, micafungin 0.016 mg/L, caspofungin 0.06 mg/L, isavuconazole 0.5 mg/L, posaconazole 1 mg/L, voriconazole 0.5 mg/L, itraconazole 0.5 mg/L, and fluconazole 32 mg/L.
Histological analysis performed on a biopsy sample showed a dermal moderate perivascular lymphocytes infiltrate associated with mild fibrosis. In the deep dermis, a dense granulomatous noncaseous infiltrate of epithelioid histiocytes surrounded by multinucleated giant cells, lymphocytes, plasma cells, and some neutrophils were seen. Rare fungal elements were seen only after an accurate examination of a set of five slides (Fig. 3).
Histological analysis of the skin lesions. a The cutis is infiltrated by perivascular small lymphocytes in the upper and middle layer of the dermis (H-E; original magnification, × 40). b, c The deep dermis shows a conspicuous inflammation and a proliferation of small vessels (H-E; original magnification, × 100). d The deep dermis displays also some noncaseating epithelioid granulomas (H-E; original magnification, × 200). e Few yeast cells (arrow) were observed (H-E; original magnification × 1000)
A therapy with itraconazole 200 mg/die was started, but after 2 weeks, there was no significant improvement of the clinical picture. Therefore, the antifungal therapy was changed to voriconazole with the IV loading dose of 400 mg every 12 h on day 1 followed by 200 mg every 12 h for 3 months, and a gradual regression of lesions was obtained. (Fig. 1c, d).
Discussion
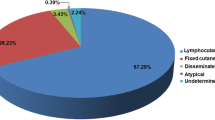
Sporotrichosis can be classified in four different clinical forms: lymphocutaneous, fixed cutaneous, disseminated cutaneous, and extracutaneous with the first two being the most common clinical presentation. Sporotrichosis is acquired after a traumatic implantation of conidia from an environmental source. Infection through inhalation of conidia has been also described in the case of pulmonary sporotrichosis. The extracutaneous form is related to an immunocompromised status and may involve bones and joints with periostitis, lungs, the central nervous system, and eyes. In immunosuppressed patients a systemic sporotrichosis has been described [7]. Data on antimicrobial activity are quite different depending on the method used. Recently, the species-specific epidemiologic cutoff values (ECVs) were established, collecting strains of the different species of Sporothrix from 17 laboratories around the world, Europe included. The proposed ECVs for S. schenckii were amphotericin B 4 mg/L, itraconazole and posaconazole 2 mg/L, and voriconazole 64 mg/L. Insufficient data about ECVs for ketoconazole and terbinafine were obtainable for S. schenckii; though, these ECVs could aid the clinician in identifying isolates less likely to respond to therapy [8].
Few cases of sporotrichosis have been reported in Europe, and so the ECDC does not track infection rates of sporotrichosis. Some autochthonous cases have been reported in several countries of Europe.
In Italy, fifty-eight cases of sporotrichosis have been described including 16 reported in Apulia, Southern Italy [9].
An autochthonous case was described in an 85-year-old indigenous Italian man living in the town of Piacenza in the north of Italy [10]. Another case was described in an immunocompetent 64-year-old male Italian mason in extreme Southern Italy [11] and in an 82-year-old man in Naples, Southern Italy [12].
A case of sporotrichosis was reported in a patient affected by ankylosing spondylitis and under treatment with adalimumab therapy, a monoclonal antibody that binds to TNF-α inhibiting its interaction with TNF receptors. TNF-α exerting several effects on cellular and humoral immunity and plays a role in the host defense against various infectious agents. An unnoticed puncture was hypothesized by a rose thorn [13]. In Italy, isolation and genetic characterization of S. schenckii isolated from commercial amended and garden soil have been also reported [14].
These reports raised the question as to whether sporotrichosis should be still considered a rare disease in Italy. Microbiologists and clinicians must be made more aware of this rare fungal infection. In addition, to our knowledge, this is the first documented report of lymphocutaneous sporotrichosis regressed by a voriconazole based therapy.
Availability of data and material
The isolated strain of S. schenckii is available for authors having scientific interest.
References
de Beer ZW, Duong TA, Wingfield MJ (2016) The divorce of Sporothrix and Ophiostoma: solution to a problematic relationship. Stud Mycol 83:165–191. https://doi.org/10.1016/j.simyco.2016.07.001
Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC et al (2015) Global epidemiology of sporotrichosis. Med Mycol 53(1):3–14. https://doi.org/10.1093/mmy/myu062
Mora-Montes HM (2018) Special Issue “Sporothrix and Sporotrichosis”. J Fungi (Basel) 4(4):E116. https://doi.org/10.3390/jof4040116
Barros MB, de Almeida PR, Schubach AO (2011) Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev 24(4):633–654. https://doi.org/10.1128/CMR.00007-11
Marimon R, Cano J, Gené J et al (2007) Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol 45:3198–3206. https://doi.org/10.1128/JCM.00808-07
Marimon R, Gené J, Cano J et al (2006) Molecular phylogeny of Sporothrix schenckii. J Clin Microbiol 44(9):3251–3256. https://doi.org/10.1128/JCM.00081-06
Queiroz-Telles F, Buccheri R, Benard G (2019) Sporotrichosis In Immunocompromised Hosts. J Fungi (Basel) 5(1):E8. https://doi.org/10.3390/jof5010008
Espinel-Ingroff A, Abreu DPB, Almeida-Paes R et al (2017) Multicenter, international study of MIC/MEC distributions for definition of epidemiological cutoff values for Sporothrix species identified by molecular methods. Antimicrob Agents Chemother 61(10):e01057–e01017. https://doi.org/10.1128/AAC.01057-17
Barile F, Mastrolonardo M, Loconsole F et al (1993) Cutaneous sporotrichosis in the period 1978-1992 in the province of Bari, Apulia, Southern Italy. Mycoses 36(5–6):181–185. https://doi.org/10.1111/j.1439-0507.1993.tb00747.x
Alberici F, Paties CT, Lombardi G et al (1989) Sporothrix schenckii var. luriei as the cause of sporotrichosis in Italy. Eur J Epidemiol 5(2):173–177. https://doi.org/10.1007/bf00156825
Criseo G, Malara G, Romeo O et al (2008) Lymphocutaneous sporotrichosis in an immunocompetent patient: a case report from extreme southern Italy. Mycopathologia 166:159–162. https://doi.org/10.1007/s11046-008-9121-4
Baroni A, Palla M, Iovene MR et al (2007) Sporotrichosis: success of itraconazole treatment. Skinmed 6(1):41–44. https://doi.org/10.1111/j.1540-9740.2007.05665.x
Ursini F, Russo E, Leporini C et al (2015) Lymphocutaneous sporotrichosis during treatment with anti-TNF-alpha monotherapy. Case Rep Rheumatol. https://doi.org/10.1155/2015/614504
Criseo G, Romeo O (2010) Ribosomal DNA sequencing and phylogenetic analysis of environmental Sporothrix schenckii strains: comparison with clinical isolates. Mycopathologia 169(5):351–358. https://doi.org/10.1007/s11046-010-9274-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
The study did not require approval from the ethics committee, according to the Italian law, since it was performed in the context of normal clinical routines (Art. 1, Leg. Decree 211/2003). However, all patients referring to our institute provided consent for the use of their data for research purposes. In any case, data were previously anonymized, according to the requirements set by Italian Data Protection Code (Leg. Decree 196/2003).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Monno, R., Brindicci, G., Romeo, O. et al. Infection caused by Sporothrix schenckii: an autochthonous case in Bari, Southern Italy. Eur J Clin Microbiol Infect Dis 39, 2457–2460 (2020). https://doi.org/10.1007/s10096-020-03939-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-03939-z