Abstract
Staphylococcus aureus bacteremia is one of the most serious bacterial infections and may lead to worse clinical outcomes in patients with prolonged severe neutropenia. However, clinical data on S. aureus bacteremia in neutropenic patients with hematologic malignancies are limited. We conducted two case-control studies using a 10-year prospective cohort of patients with S. aureus bacteremia. Neutropenic and non-neutropenic hematologic malignancy patients were compared on clinical characteristics and treatment outcomes. An additional matched case-control study using solid tumor patients was conducted. Risk factors for 12-week mortality were analyzed. Of 1643 patients with S. aureus bacteremia, 64 (3.9%) neutropenic and 108 (6.6%) non-neutropenic patients with hematologic malignancies were included in the study. There were no significant differences in the incidence of metastatic infection between the two groups (17.2% vs. 17.6%, p = 0.95), in contrast with a previous study that observed no metastatic infection in neutropenic patients. Twelve-week mortality in neutropenic patients with hematologic malignancies tended to be lower than in non-neutropenic patients with hematologic malignancies (15.6% vs. 26.9%, p = 0.09) and was significantly lower than in neutropenic patients with solid tumors (15.6% vs. 45.8%, p = 0.003). Independent risk factors for mortality in hematologic malignancy patients with S. aureus bacteremia were high Charlson comorbidity score, high APACHE II score, and skin and soft tissue infection. Neutropenia was not independently associated with mortality. Our findings suggest that neutropenia in hematologic malignancies may not affect the incidence of metastatic infection or 12-week mortality of S. aureus bacteremia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neutropenic patients are generally perceived to have a poorer prognosis than non-neutropenic patients, due to increased susceptibility to infection and the risk of a more severe clinical course. Neutropenic patients with hematologic malignancies are clinically important because they have a longer duration of neutropenia than those with non-hematologic malignancies [1]. The incidence of bacteremia in neutropenic patients has been reported to be 10–25% [2,3,4]. Although the proportion of gram-negative organisms has gradually increased in neutropenic infection, gram-positive organisms are still an important cause [2, 5, 6]. Staphylococcus aureus bacteremia is one of the most common and serious bacterial infections caused by such organisms, with a high frequency of metastatic infection and poor prognosis [7]. However, the precise burden of S. aureus bacteremia among neutropenic patients and its clinical consequences are not well established, especially in patients with hematologic malignancies. Studies in the 1980s and 1990s noted high mortality rates (44–49%) among neutropenic patients with S. aureus bacteremia [8,9,10]. The most recent article, published in 2003, reported low attributable mortality (5.2%) and no instances of metastatic infection among neutropenic hematologic malignancy patients with S. aureus bacteremia [11]. These inconsistent results and the lack of additional studies implied a need for further clinical investigations reflecting current advances in the management of S. aureus bacteremia in such patients. Therefore, we have analyzed the clinical characteristics and outcomes of S. aureus bacteremia in neutropenic patients with hematologic malignancies and compared them with those without neutropenia.
Patients and methods
Study population and design
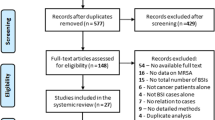
We performed two case-control studies within a prospective observational cohort of patients with S. aureus bacteremia. Among them, those with hematologic malignancies were included in the study, and the clinical characteristics and treatment outcomes according to presence of neutropenia were analyzed. An additional matched case-control study using patients with solid tumors was conducted in the same manner. Neutropenic cases were matched 1:3 to non-neutropenic control patients based on age, gender, ward, and case year. The prospective study was conducted at the Asan Medical Center, a 2700-bed tertiary care hospital with an isolation ward for patients with hematologic malignancies. From July 2008 to June 2017, all adult patients with S. aureus bacteremia were prospectively enrolled in the cohort and observed over a 12-week period. Patients were excluded if they had polymicrobial bacteremia, or if they died or were discharged before positive blood culture results were obtained. In our hospital, all patients with S. aureus bacteremia receive automatic infectious disease consultation, and febrile neutropenia is managed based on the clinical practice guidelines previously published [12].
Data collection and definitions
Demographic characteristics, laboratory results, underlying diseases or conditions, severity of underlying disease, severity of bacteremia, site of infection, antibiograms, patient management, and clinical outcomes were recorded. Neutropenia was defined as absolute neutrophil count (ANC) < 500/mm3. The McCabe and Jackson criteria were used to classify the severity of the underlying disease [13]. The Charlson comorbidity index was used to predict prognosis based on the aggregate score of comorbid conditions [14]. The criteria provided by the Centers for Disease Control and Prevention were used to define the type of infection causing S. aureus bacteremia including primary bacteremia, pneumonia, skin and soft tissue infection (SSTI), postoperative wound infection, and bone and joint infection [15], and SSTI was an infection involves the skin, subcutaneous tissue, fascia, or muscle. Catheter-related infection was defined based on the clinical practice guidelines [16], and infective endocarditis was defined according to the modified Duke criteria [17].
Metastatic infection was defined as the involvement of a distant focus anatomically unrelated to the source implicating secondary bacterial seeding [18]. Bacteremia was classified as nosocomial if a positive blood culture was obtained from a patient who had been hospitalized for 48 h or longer. Community-onset bacteremia was subdivided into healthcare–associated and community-acquired bacteremia, as previously described [19]. Primary clinical outcome was 12-week mortality, and secondary outcomes were recurrent bacteremia and 30-day mortality.
Statistical analysis
Categorical variables were compared using the χ2 test or Fisher’s exact test as appropriate, and continuous variables were compared using Student’s t test or the Mann–Whitney U test. To identify independent risk factors for 12-week mortality, all variables with p values < 0.1 in the univariate analysis were included in a multivariate analysis using a multiple logistic regression model. A 2-tailed p value < 0.05 was considered to indicate statistical significance. All statistical analyses were performed using IBM SPSS statistics for Windows, version 24.0 (IBM Corp., Armonk, NY, USA).
Results
Patient characteristics and metastatic infection in patients with hematologic malignancies
During the study period, 1643 patients with S. aureus bacteremia were included in our cohort. Of these patients, 64 (3.9%) were neutropenic and 108 (6.6%) were non-neutropenic patients with hematologic malignancies. The neutropenic patients with hematologic malignancies were younger (p < 0.001) and had more nosocomial infection (p = 0.003) and primary bacteremia as the source of infection (p < 0.001) (Table 1). Other characteristics were comparable between the two groups. No infective endocarditis was detected as the source of S. aureus bacteremia in neutropenic patients with hematologic malignancies.
The incidence of metastatic infection was similar between the two groups (p = 0.95). Skin and soft tissue was the most common site (45.5%) of metastatic infection in neutropenic patients with hematologic malignancies. Detailed information on the sites of metastatic infection is summarized in Supplementary Table 1.
Treatment and clinical outcome of patients with hematologic malignancies
More than 90% of patients received appropriate antibiotics within 2 days of bacteremia. Neutropenic patients with hematologic malignancies had a tendency for shorter duration of bacteremia compared with non-neutropenic patients (mean 2.1 days vs. 2.7 days, p = 0.09). Despite their prolonged neutropenia, neutropenic patients with hematologic malignancies tended to have a lower 12-week mortality rate than non-neutropenic patients (15.6% vs. 26.9%, p = 0.09) (Table 1).
Clinical characteristics and treatment outcome of patients with solid tumors
During the study period, there were 24 neutropenic patients with solid tumors and S. aureus bacteremia. There were no significant differences in characteristics between neutropenic and non-neutropenic patients, except for healthcare-associated infection and fever at the time of bacteremia (Table 2). Treatment outcomes were not different between neutropenic and non-neutropenic patients with solid tumors. Twelve-week mortality was significantly higher in the patients with solid tumors than in those with hematologic patients regardless of neutropenia (Fig. 1).
Risk factors for mortality in patients with S. aureus bacteremia
In univariate analysis, severe sepsis/septic shock, high APACHE II score, and SSTI were significantly associated with 12-week mortality in patients with hematologic malignancies (Table 3). Variables with p values < 0.1, together with gender and MRSA infection, were included in multivariate analysis. Independent risk factors for mortality in hematologic malignancy patients with S. aureus bacteremia were high Charlson comorbidity score, high APACHE II score, and SSTI (Table 4). Neutropenia was not independently associated with mortality. In solid tumor patients with S. aureus bacteremia, high Charlson comorbidity score and APACHE II score were independent risk factors for mortality (Supplementary Tables 2 and 3).
Discussion
We have shown that neutropenic patients with hematologic malignancies have a similar incidence of metastatic infection during S. aureus bacteremia to non-neutropenic patients with hematologic malignancies or solid tumors, and no increased mortality rate. Moreover, their mortality rate was significantly lower than that of the neutropenic patients with solid tumors. From the 1980s to the early 2000s, a few studies reported higher mortality of S. aureus bacteremia in patients with hematologic malignancies or neutropenia than in non-neutropenic patients [8, 9]. However, more recent studies, including our own, suggest that this may not be true for neutropenic patient with hematologic malignancies [11, 20], and following reasons may explain this. First, recent advances in the management of S. aureus bacteremia and hematologic malignancies may influence the improved prognosis of hematologic malignancy patients with S. aureus bacteremia, even in the prolonged neutropenic state. Second, as Venditti and colleagues have discussed [11], eradication of S. aureus from the bloodstream can be achieved rapidly due to the early administration of empirical broad-spectrum antibiotics and the relatively low inoculum of bacteria in these patients. They have also suggested that the scarcity of phagocytes including neutrophils and macrophages that could serve as an intracellular reservoir of S. aureus could contribute to the rapid clearance of bacteremia. Consistent with those suggestions, there was a tendency toward a shorter duration of S. aureus bacteremia in neutropenic patients with hematologic malignancies in our study. The reason for higher mortality in solid tumor patients with S. aureus bacteremia compared with those with hematologic malignancies is probably due to their dangerous comorbidities including distant metastasis of solid tumors. In fact, neutropenic patients with hematologic malignancies were younger and had a lower Charlson comorbidity score than those with solid tumors in our study.
Many previous studies have demonstrated that age, presence of comorbidities, severity of illness, pneumonia, persistent bacteremia, and metastatic infection are risk factors for mortality in patients with S. aureus bacteremia [21]. In agreement with these studies, high Charlson comorbidity score and high APACHE II score were independent risk factors for mortality in patients with hematologic malignancies or solid tumors. This means that traditional risk factors for mortality of S. aureus bacteremia are more important in these patients rather than neutropenia.
An additional finding in the present study was that SSTI was an independent risk factor for mortality in hematologic malignancy patients with S. aureus bacteremia. It is not clear why the mortality rate of patients with SSTI was high (7/15, 46.7%). However, of the seven deaths, only one died directly due to SSTI. In a previous study by Fowler et al., skin examination findings suggesting disseminated systemic infection in S. aureus bacteremia were one of the predictive factors for complicated S. aureus bacteremia [22]. In some of our patients, SSTI could have been manifested as one of these skin findings. Given these points, it may be a bit premature to conclude that SSTI is an independent risk factor for mortality. More data are needed to address this issue.
In contrast to previous retrospective studies that reported a lower incidence of metastatic infections in neutropenic patients with hematologic malignancies [8, 9, 11, 23], we found a similar incidence of metastatic infection to that in non-neutropenic patients. The “Trojan horse” theory proposes that neutrophils serve as a reservoir for S. aureus and consequently help to cause metastatic infections [24]. A previous study that found no metastatic infections in neutropenic patients with S. aureus bacteremia advocated this theory [11]. However, our results suggest that metastatic infection does not develop solely through “S. aureus–bearing neutrophils,” and that bacterial spreading via the bloodstream in the early stage of bacteremia may also be an important mechanism. Actually, in our study, all metastatic infections in neutropenic patients with hematologic malignancies were detected early (within 7 days of bacteremia) perhaps because all our patients were prospectively enrolled and underwent careful examination to evaluate the presence of metastatic infections through consultation with infectious disease specialists.
Our study has several limitations. First, because the data were collected from a single tertiary center, they may not fully reflect all aspects of S. aureus bacteremia in neutropenic patients with hematologic malignancies. Second, non-neutropenic state in hematologic malignancies may be different from that in solid tumors due to suppressed neutrophil function in hematologic malignancies [25]. However, the strengths of our study, which had a prospective design and involved a larger number of study patients than previous studies, could compensate for these limitations.
In conclusion, neutropenia in patients with hematologic malignancies was not related to the incidence of metastatic infection and mortality of S. aureus bacteremia. Although the mortality of neutropenic hematologic malignancy patients with S. aureus bacteremia was not different from that of non-neutropenic patients, the clinical importance of S. aureus bacteremia in this group should not be underestimated, and active management including consultation with infectious diseases specialists and appropriate antibiotic therapy is still important.
References
Safdar A, Armstrong D (2011) Infections in patients with hematologic neoplasms and hematopoietic stem cell transplantation: neutropenia, humoral, and splenic defects. Clin Infect Dis 53(8):798–806. https://doi.org/10.1093/cid/cir492
Ramphal R (2004) Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis 39(Suppl 1):S25–S31. https://doi.org/10.1086/383048
Rosenberg PS, Alter BP, Bolyard AA, Bonilla MA, Boxer LA, Cham B, Fier C, Freedman M, Kannourakis G, Kinsey S, Schwinzer B, Zeidler C, Welte K, Dale DC (2006) The incidence of leukemia and mortality from sepsis in patients with severe congenital neutropenia receiving long-term G-CSF therapy. Blood 107(12):4628–4635. https://doi.org/10.1182/blood-2005-11-4370
Gudiol C, Tubau F, Calatayud L, Garcia-Vidal C, Cisnal M, Sanchez-Ortega I, Duarte R, Calvo M, Carratala J (2011) Bacteraemia due to multidrug-resistant Gram-negative bacilli in cancer patients: risk factors, antibiotic therapy and outcomes. J Antimicrob Chemother 66(3):657–663. https://doi.org/10.1093/jac/dkq494
Cattaneo C, Quaresmini G, Casari S, Capucci MA, Micheletti M, Borlenghi E, Signorini L, Re A, Carosi G, Rossi G (2008) Recent changes in bacterial epidemiology and the emergence of fluoroquinolone-resistant Escherichia coli among patients with haematological malignancies: results of a prospective study on 823 patients at a single institution. J Antimicrob Chemother 61(3):721–728. https://doi.org/10.1093/jac/dkm514
Bousquet A, Malfuson JV, Sanmartin N, Konopacki J, MacNab C, Souleau B, de Revel T, Elouennass M, Samson T, Soler C, Foissaud V, Martinaud C (2014) An 8-year survey of strains identified in blood cultures in a clinical haematology unit. Clin Microbiol Infect 20(1):O7–O12. https://doi.org/10.1111/1469-0691.12294
Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr (2015) Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev 28(3):603–661. https://doi.org/10.1128/cmr.00134-14
Espersen F, Frimodt-Moller N, Rosdahl VT, Jessen O, Faber V, Rosendal K (1987) Staphylococcus aureus bacteremia in patients with hematological malignancies and/or agranulocytosis. Acta Med Scand 222(5):465–470
Skov R, Gottschau A, Skinhoj P, Frimodt-Moller N, Rosdahl VT, Espersen F (1995) Staphylococcus aureus bacteremia: a 14-year nationwide study in hematological patients with malignant disease or agranulocytosis. Scand J Infect Dis 27(6):563–568
Shah MA, Sanders L, Lanclos K, Chamis AL, Gockerman J, Wray D, Corey GR, Fowler VG Jr (2002) Staphylococcus aureus bacteremia in patients with neutropenia. South Med J 95(7):782–784
Venditti M, Falcone M, Micozzi A, Carfagna P, Taglietti F, Serra PF, Martino P (2003) Staphylococcus aureus bacteremia in patients with hematologic malignancies: a retrospective case-control study. Haematologica 88(8):923–930
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 52(4):427–431. https://doi.org/10.1093/cid/ciq147
Mc CW, Jackson G (1962) Gram-negative bacteremia: I. etiology and ecology. Arch Intern Med 110(6):847–855. https://doi.org/10.1001/archinte.1962.03620240029006
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16(3):128–140
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK (2009) Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 49(1):1–45. https://doi.org/10.1086/599376
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30(4):633–638. https://doi.org/10.1086/313753
Jenkins TC, Price CS, Sabel AL, Mehler PS, Burman WJ (2008) Impact of routine infectious diseases service consultation on the evaluation, management, and outcomes of Staphylococcus aureus bacteremia. Clin Infect Dis 46(7):1000–1008. https://doi.org/10.1086/529190
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ (2002) Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137(10):791–797
Gonzalez-Barca E, Carratala J, Mykietiuk A, Fernandez-Sevilla A, Gudiol F (2001) Predisposing factors and outcome of Staphylococcus aureus bacteremia in neutropenic patients with cancer. Eur J Clin Microbiol Infect Dis 20(2):117–119
van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB (2012) Predictors of mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev 25(2):362–386. https://doi.org/10.1128/cmr.05022-11
Fowler VG Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB, Cheng AC, Dudley T, Oddone EZ (2003) Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med 163(17):2066–2072. https://doi.org/10.1001/archinte.163.17.2066
Sotman SB, Schimpff SC, Young VM (1980) Staphylococcus aureus bacteremia in patients with acute leukemia. Am J Med 69(6):814–818
Thwaites GE, Gant V (2011) Are bloodstream leukocytes Trojan horses for the metastasis of Staphylococcus aureus? Nat Rev Microbiol 9(3):215–222. https://doi.org/10.1038/nrmicro2508
Tanaka F, Goto H, Yokosuka T, Yanagimachi M, Kajiwara R, Naruto T, Nishimaki S, Yokota S (2009) Suppressed neutrophil function in children with acute lymphoblastic leukemia. Int J Hematol 90(3):311–317. https://doi.org/10.1007/s12185-009-0412-4
Funding
This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number HI15C2918).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the Asan Medical Center Institutional Review Board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 79.5 kb)
Rights and permissions
About this article
Cite this article
Ryu, BH., Lee, S.C., Kim, M. et al. Impact of neutropenia on the clinical outcomes of Staphylococcus aureus bacteremia in patients with hematologic malignancies: a 10-year experience in a tertiary care hospital. Eur J Clin Microbiol Infect Dis 39, 937–943 (2020). https://doi.org/10.1007/s10096-019-03802-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03802-w