Abstract
Pneumocystis pneumonia is a serious complication that may affect immunosuppressed patients. The absence of reliable and safe therapeutic alternatives to trimethoprim–sulfamethoxazole (TMP/SMX) justifies the search for more effective and less toxic agents. In this study, the in vitro and in vivo anti-Pneumocystis jirovecii activity of iclaprim, a diaminopyrimidine compound that exerts its antimicrobial activity through the inhibition of dihydrofolate reductase (DHFR), as does TMP, was evaluated alone or in combination with SMX. The antimicrobial activity of iclaprim was tested in vitro using an efficient axenic culture system, and in vivo using P. carinii endotracheally inoculated corticosteroid-treated rats. Animals were orally administered iclaprim (5, 25, 50 mg/kg/day), iclaprim/SMX (5/25, 25/125, 50/250 mg/kg/day), TMP (50 mg/kg/day), or TMP/SMX (50/250 mg/kg/day) once a day for ten consecutive days. The in vitro maximum effect (Emax) and the drug concentrations needed to reach 50% of Emax (EC50) were determined, and the slope of the dose–response curve was estimated by the Hill equation (Emax sigmoid model). The iclaprim EC50 value was 20.3 μg/mL. This effect was enhanced when iclaprim was combined with SMX (EC50: 13.2/66 μg/mL) (p = 0.002). The TMP/SMX EC50 value was 51.4/257 μg/mL. In vivo, the iclaprim/SMX combination resulted in 98.1% of inhibition compared to TMP/SMX, which resulted in 86.6% of inhibition (p = 0.048). Thus, overall, the iclaprim/SMX combination was more effective than TMP/SMX both in vitro and in vivo, suggesting that it could be an alternative therapy to the TMP/SMX combination for the treatment of Pneumocystis pneumonia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumocystis pneumonia (PcP) is an opportunistic infection caused by Pneumocystis jirovecii, which occurs when cellular immunity is depressed because of AIDS [1], malignancies [2], prolonged immunosuppressing drugs [3], IgA nephropathy [4], organ transplantation [5], or corticosteroid therapy [6]. The PcP mortality rate is high among patients with delayed diagnosis [2] and treatment, and death is due to severe respiratory failure [7].
Serological data indicate that Pneumocystis primary infection occurs in 70–90% of immunocompetent 2–4-year-old children from temperate or tropical regions [8, 9], and could be associated with upper respiratory infection in infants, predominantly those 1.5–4 months of age [9]. PCR survey of healthy people in Spain has revealed P. jirovecii in 20% of the population [10]. In addition, Pneumocystis organisms were detected frequently in neonatal or young children [11, 12], pregnant women [13], and patients with chronic underlying diseases [14,15,16,17]. Thus, Pneumocystis organisms could behave as a comorbidity factor [11, 15]. For instance, pulmonary carriage of P. jirovecii in patients with chronic obstructive pulmonary disease (COPD) could worsen the progression of this illness [15], which is the fifth most common cause of death in high-income countries [18].
Available drugs that are effective against PcP are limited. The first-line treatment and prophylaxis for P. jirovecii infection is trimethoprim–sulfamethoxazole (TMP/SMX) [19]; however, numerous side effects have been associated with this therapy [20,21,22,23]. Moreover, reports suggest an emergence of P. jirovecii resistance to sulfa drugs [24,25,26,27,28,29]. Unfortunately, the lack of cultures of P. jirovecii from these cases has not allowed confirmation of the cases of clinically suspected drug resistance [24]. No information about P. jirovecii resistane to the combination of iclaprim plus sulfa drugs is known. Efforts have been made to study putative drug resistance against TMP/SMX by sequencing the Pneumocystis dihydropteroate synthase (DHPS) gene from clinical P. jirovecii isolates. This gene is highly conserved in many organisms, and similar DHPS mutations can confer resistance to sulfa drugs in either prokaryotic (Escherichia coli, Streptococcus pneumoniae) or eukaryotic (Plasmodium falciparum) pathogens [30,31,32,33]. The widespread use of TMP/SMX for PcP prophylaxis could, therefore, select P. jirovecii strains with DHPS mutations. Consistently, DHPS mutations have been associated with both the use of sulfa drugs (TMP/SMX or dapsone, a sulfone) [29] and the duration of SMX or sulfone prophylaxis [34]. The American Thoracic Society (ATS) recommended P. jirovecii drug resistance as a topic of clinical research, including the association of DHPS mutations with TMP/SMX treatment failure or death [35].
The absence of suitable therapeutic alternatives to the TMP/SMX drug combination constitutes an unmet medical need; pentamidine exhibits significant toxicity [36, 37] and atovaquone is used only against mild forms of PcP [38]. Thus, deleterious side effects, limited efficacies, and emerging resistance justify the search for more effective and less toxic anti-Pneumocystis agents.
Iclaprim, a diaminopyrimidine compound that exerts its antimicrobial activity through the inhibition of dihydrofolate reductase (DHFR) [39, 40], may represent a new option for responding to this medical need. For these reasons, the activity of iclaprim against Pneumocystis was tested both in vitro, using an efficient axenic culture system [41], and in vivo, using P. carinii endotracheally inoculated corticosteroid-treated rats [42,43,44,45].
Materials and methods
Drugs
Iclaprim, TMP, and SMX were dissolved in 100% dimethyl sulfoxide (DMSO, Sigma-Aldrich, France). TMP and SMX solutions were mixed appropriately to obtain a final 1:5 combination. Then, for evaluating the in vitro anti-Pneumocystis activity, the drug stock solutions were diluted in Dulbecco’s Modified Eagle’s Medium (DMEM, BioWhittaker, France) supplemented with 10% heat-inactivated fetal calf serum (FCS, Gibco BRL, France) to produce the required drug concentrations. To evaluate the in vivo anti-Pneumocystis activity, iclaprim, TMP, or SMX stock solutions were used. Drug solutions of 100 mg/mL were used for iclaprim and TMP, whereas a solution of 500 mg/mL was used for SMX. Then, the drug stock solutions were diluted in sterile water before gavage. Compound solutions were prepared just before use.
Source of P. carinii
Corticosteroid-treated conventional laboratory rats were used as the animal model to obtain P. carinii organisms. Ten-week-old female Wistar rats (Harlan, France) were immunosuppressed for 3 weeks with dexamethasone (Merck, France) administered in the drinking water (2 mg/L) [44]. Then, rats were inoculated with 2 × 107 of cryopreserved parasites using a non-surgical endotracheal method [46]. Dexamethasone treatment was maintained until the end of the experiment. Six to 8 weeks post-inoculation, rats were infected. Animals were allowed sterile standard food (UAR, France) and water ad libitum. The research complied with national legislation and with company policy on the care and use of animals and with the related code of practice (accreditation number: A59107, agreement number: B 59-35000). The study has been approved by the ethical committee for experiments on animals (approval number 02789.02).
Extraction, purification, and quantitation of P. carinii
Six to 8 weeks following inoculation, rats were euthanized and parasite extraction was performed [44]. Briefly, parasites were extracted in DMEM (BioWhittaker, France) by agitation of lung pieces with a magnetic stirrer. The resulting homogenate was poured successively through 250- and 63-μm stainless steel filters. After centrifugation, the pellet was resuspended in a hemolytic buffered solution (BioWhittaker, France). Pneumocystis carinii organisms were collected by centrifugation and then purified on a polysucrose gradient (Histopaque-1077, Sigma-Aldrich, France). Blood and Sabouraud dextrose agar (Difco, France) media were inoculated with purified parasites to check for the presence of eventual contaminating pathogens. Pneumocystis carinii was quantitated on air-dried smears stained with RAL 555 (Réactifs RAL, France), a rapid panoptic methanol Giemsa stain, which stains trophic forms, sporocytes, and cysts of P. carinii [41]. Pneumocystis was then cryopreserved by placing parasites in FCS with 10% DMSO at − 80 °C in a Nalgene 1 °C cryo-freezing container (cooling rate about 1 °C/min) for 4 h [41]. The parasite samples were then stored in liquid nitrogen. Cryopreserved P. carinii were used for in vitro or in vivo studies.
In vitro susceptibility study
In vitro pharmacodynamic properties were determined using the Hill equation (Emax sigmoid model). This approach offers three parameters which can be used to describe the in vitro activity of new therapeutic compounds: the maximum effect (Emax) as a measure for efficacy, the 50% effective concentration (EC50) as a parameter of intrinsic activity, and the slope (S) of the concentration–effect relationship. In vitro susceptibility studies were performed using the broth microdilution technique. Final drug concentrations ranged from 5 to 100 μg/mL for iclaprim, 5/25 to 100/500 μg/mL for the combination iclaprim/SMX, and 1/5 to 150/750 μg/mL for the combination TMP/SMX. All the experiments were carried out in 24-well plates with a final volume of 2 mL of DMEM supplemented with 10% FCS containing a final inoculum of 0.5 × 106 organisms per mL. Then, plates were incubated for 4 days in an atmosphere of 5% CO2 at 37 °C. One drug-free control was included in each assay. Parasite quantitation was performed on homogenate smears as described above. All susceptibility assays were set up in triplicate.
Analysis of in vitro results
The in vitro activity of tested compounds against P. carinii was expressed as a percentage of inhibition, defined as the total parasite number found in drug-treated wells in comparison with parasite counts in control wells without drug. Once all the differences between drug-treated and untreated wells were calculated, the concentration–effect relationship was established by using the Hill equation:
where E R is the effect of each drug concentration (C) on the percentage of inhibition estimated from experimental results; S is a parameter reflecting the steepness of the concentration–effect relationship curve; and EC50 is the concentration of the compound at which 50% of the maximum effect (ER,max) is obtained. The parameters of this pharmacodynamic model were calculated by nonlinear least-squares regression techniques using commercial software (SigmaPlot, Systat Software, Inc.).
In vivo susceptibility study
An in vivo experiment with corticosteroid-treated Wistar rats endotracheally inoculated with P. carinii was performed in order to explore whether in vitro results reflect in vivo efficacy. Six to 8 weeks post-inoculation, animals were highly infected with P. carinii, as assessed by the number of P. carinii cysts in lung homogenates, as previously described [44]. Animals were divided into groups of three and then randomized to one of the following oral interventions: (1) iclaprim dosed at 5, 25, or 50 mg/kg; (2) TMP dosed at 50 mg/kg; (3) the combination TMP/SMX dosed at 50/250 mg/kg (diluted in DMSO); and (4) the combination iclaprim/SMX dosed at 5/25, 25/125, or 50/250 mg/kg. The drugs were given once a day for ten consecutive days. The final concentration of DMSO in diluted drug solutions was between 1.5 and 15%. Control animals were dosed with sterile water with 15% DMSO. At the end of the experiment, therapeutic efficacy was assessed by counting P. carinii in lung homogenates and comparing the counts with those of the untreated controls. Lung histopathology was not analyzed. Twenty-four hours after the end of the treatment, animals were euthanized and the lung homogenized in a Stomacher 400 blender, as previously described [44]. Parasite quantitation was performed on air-dried smears stained with RAL 555 stain (trophic forms, sporocytes, and cystic forms; RAL Diagnostics, France). Therapeutic efficacy was assessed by counting P. carinii parasites in lung homogenates and comparing them with those of the untreated controls at the end of the experiment. For each drug concentration, the results were expressed as the percentage of inhibition versus drug-free animal controls.
Statistical analysis
Statistical analysis was performed using SPSS statistical software. Pneumocystis carinii parasites counts were presented as the mean and standard error. For each drug, the therapeutic efficacy was assessed by comparing the mean of the total parasite number for treated animals to that of untreated animals with a Student’s t-test (the data distributions were found to be normal by preliminary Shapiro–Wilk tests). The comparisons of iclaprim to TMP at 50 mg/kg/day and of the combination iclaprim/SMX to the combination TMP/SMX at 50/250 mg/kg/day were similarly performed. Two-sided p-values < 0.05 were deemed to be statistically significant.
Results
In vitro susceptibility study
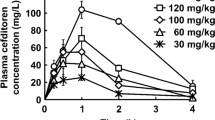
Figure 1 shows the concentration–response curves obtained after 4 days of incubation of P. carinii with iclaprim or the combinations iclaprim/SMX or TMP/SMX. The reduction in the number of microorganisms was gradual and concentration-dependent. TMP/SMX demonstrated an EC50 of 51.4/257 μg/mL (Table 1). The present work revealed a high in vitro anti-Pneumocystis activity of iclaprim, with an EC50 value of 20.3 μg/mL. Moreover, the results obtained with the iclaprim/SMX combination (proportion 1:5) showed significantly increased activity, with an EC50 value of 13.2/66 μg/mL (p = 0.002). At least 99% growth inhibition was reached with iclaprim at a concentration of 50 μg/mL and with the combination iclaprim/SMX at a concentration of 37/185 μg/mL (Table 1). Higher concentrations of TMP/SMX (150/750 μg/mL) were needed for reaching a ~ 99% inhibition.
In vivo susceptibility study
Untreated animals were highly infected at the end of the treatment period. The total number of P. carinii organisms per lung was 2.2 ± 0.4 × 109 (Table 2). Iclaprim and TMP showed a similar activity at the concentration of 50 mg/kg/day (p = 0.888). The iclaprim/SMX combination was significantly more effective (98.1% growth inhibition) than TMP/SMX (86.6% growth inhibition) (p = 0.048) (Table 2).
Discussion
The iclaprim/SMX combination was more active than TMP/SMX in in vitro and in vivo studies. Iclaprim alone or combined with SMX inhibited the growth of both Pneumocystis cysts and vegetative forms. This is an important difference with other anti-Pneumocystis drugs like echinocandin-derived compounds, inhibitors of β-1,3 glucan synthase, which selectively eliminates cysts in infected rats at therapeutic doses [47,48,49], and, thus, have been mainly utilized as salvage therapy or in combination with other antimicrobial agents [50,51,52,53].
In vitro susceptibility tests are a basic step in current pharmacological screening for new anti-infective drugs. A standard method was proposed for pathogenic yeast in 1997 ([54], but it could not be applied to Pneumocystis species, which do not grow well in fungal culture systems. In fact, Pneumocystis species are atypical fungi [55, 56]. For instance, they lack ergosterol [57], which is the target for most antifungal molecules [58]. The present results indicate that in vitro EC50 could be a predictive indicator of the anti-Pneumocystis in vivo effect, at least for iclaprim/SMX and for sordarin derivatives [43]. Pharmacodynamic parameters were calculated using the Hill equation, which has been previously used to assess the in vitro concentration–effect relationships of many anti-Pneumocystis drugs in the 4-day axenic Pneumocystis culture system used in the present work [43]. Factors such as medium composition, inoculum size, and incubation time of the in vitro susceptibility axenic system used in this work were defined previously [43, 45]. In this system, the growth of all Pneumocystis life cycle parasite stages is currently assessed on dry smears stained by RAL 555, a methanol Giemsa-like staining [45, 59, 60]. The in vitro strategy used in this work allows estimating the intrinsic activity against P. carinii of the tested molecule, and, therefore, it affords an efficient tool to perform a direct comparison among molecules.
The in vivo results were consistent with the in vitro results, showing that iclaprim/SMX is more potent than TMP/SMX against P. carinii. The in vivo model used the Wistar rat, which was inoculated non-surgically by the endotracheal route [46] with a suspension of P. carinii organisms [61]. Despite a limitation of not analyzing lung histopathology, this model did not present the drawbacks of conventional corticosteroid-induced PcP rodent models [42], which develop spontaneous PcP infections and, thus, are characterized by a marked variability in parasite infection rates and unknown origin of Pneumocystis strains. For these reasons, Pneumocystis endotracheally inoculated animal models of PcP were developed [61], such as the one used in the present study.
The present work confirmed that the activity of the combination of a diaminopyrimidine with SMX is enhanced, and showed that the activity was highest with the iclaprim/SMX combination. This combination may prevent the emergence of P. jirovecii resistance to sulfa drugs. Iclaprim exhibits favorable lung pharmacokinetics which will influence its utility for the treatment of pneumonia caused by various pathogens. An oral formulation of iclaprim is being developed. An iclaprim/SMX combination may enhance the favorable lung pharmacokinetics compared to iclaprim alone. A Phase 1 study investigated the tissue distribution of a single intravenous dose of iclaprim in relevant lung compartments [62]. Iclaprim concentrations were found in epithelial lung fluid and alveolar macrophages, up to 20- and 40-fold higher, respectively, than in plasma [62]. In addition, a Phase 2 study comparing the clinical cure rates of two iclaprim dosages with vancomycin in the treatment of patients with nosocomial pneumonia suspected or confirmed to be caused by Gram-positive pathogens showed iclaprim and vancomycin to have comparable clinical cure rates and safety profiles [63]. In conclusion, collectively, the current in vitro and in vivo study, and previous Phase 1 and 2 studies, support that iclaprim alone or combined with SMX could potentially offer an alternative and more potent first-line therapy to treat PcP in humans.
References
Bonnet F, Lewden C, May T, Heripret L, Jougla E, Bevilacqua S, Costagliola D, Salmon D, Chêne G, Morlat P; Mortalité 2000 Study Group (2005) Opportunistic infections as causes of death in HIV-infected patients in the HAART era in France. Scand J Infect Dis 37:482–487. https://doi.org/10.1080/00365540510035328
Li MC, Lee NY, Lee CC, Lee HC, Chang CM, Ko WC (2014) Pneumocystis jiroveci pneumonia in immunocompromised patients: delayed diagnosis and poor outcomes in non-HIV-infected individuals. J Microbiol Immunol Infect 47:42–47. https://doi.org/10.1016/j.jmii.2012.08.024
Lv J, Zhang H, Cui Z, Su T, Zhang Y, Wang H (2008) Delayed severe pneumonia in mycophenolate mofetil-treated patients with IgA nephropathy. Nephrol Dial Transplant 23(9):2668–2672. https://doi.org/10.1093/ndt/gfn161
Ye WL, Tang N, Wen YB, Li H, Li MX, Du B, Li XM (2016) Underlying renal insufficiency: the pivotal risk factor for Pneumocystis jirovecii pneumonia in immunosuppressed patients with non-transplant glomerular disease. Int Urol Nephrol 48(11):1863–1871. https://doi.org/10.1007/s11255-016-1324-x
Martin SI, Fishman JA; AST Infectious Diseases Community of Practice (2013) Pneumocystis pneumonia in solid organ transplantation. Am J Transplant 13(Suppl 4):272–279. https://doi.org/10.1111/ajt.12119
Yale SH, Limper AH (1996) Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: associated illnesses and prior corticosteroid therapy. Mayo Clin Proc 71:5–13. https://doi.org/10.4065/71.1.5
Boonsarngsuk V, Sirilak S, Kiatboonsri S (2009) Acute respiratory failure due to Pneumocystis pneumonia: outcome and prognostic factors. Int J Infect Dis 13:59–66. https://doi.org/10.1016/j.ijid.2008.03.027
Wakefield AE, Stewart TJ, Moxon ER, Marsh K, Hopkin JM (1990) Infection with Pneumocystis carinii is prevalent in healthy Gambian children. Trans R Soc Trop Med Hyg 84:800–802. https://doi.org/10.1016/0035-9203(90)90087-U
Larsen HH, von Linstow ML, Lundgren B, Høgh B, Westh H, Lundgren JD (2007) Primary Pneumocystis infection in infants hospitalized with acute respiratory tract infection. Emerg Infect Dis 13(1):66–72. https://doi.org/10.3201/eid1301.060315
Medrano FJ, Montes-Cano M, Conde M, de la Horra C, Respaldiza N, Gasch A, Perez-Lozano MJ, Varela JM, Calderon EJ (2005) Pneumocystis jirovecii in general population. Emerg Infect Dis 11:245–250. https://doi.org/10.3201/eid1102.040487
Chabé M, Vargas SL, Eyzaguirre I, Aliouat EM, Follet-Dumoulin A, Creusy C, Fleurisse L, Recourt C, Camus D, Dei-Cas E, Durand-Joly I (2004) Molecular typing of Pneumocystis jirovecii found in formalin-fixed paraffin-embedded lung tissue sections from sudden infant death victims. Microbiology 150:1167–1172. https://doi.org/10.1099/mic.0.26895-0
Vargas SL, Ponce CA, Gálvez P, Ibarra C, Haas EA, Chadwick AE, Krous HF (2007) Pneumocystis is not a direct cause of sudden infant death syndrome. Pediatr Infect Dis J 26(1):81–83. https://doi.org/10.1097/01.inf.0000247071.40739.fd
Vargas SL, Ponce CA, Sanchez CA, Ulloa AV, Bustamante R, Juarez G (2003) Pregnancy and asymptomatic carriage of Pneumocystis jiroveci. Emerg Infect Dis 9(5):605–606. https://doi.org/10.3201/eid0905.020660
Calderón EJ, Regordan C, Medrano FJ, Ollero M, Varela JM (1996) Pneumocystis carinii infection in patients with chronic bronchial disease. Lancet 347(9006):977
Calderón EJ, Rivero L, Respaldiza N, Morilla R, Montes-Cano MA, Friaza V, Muñoz-Lobato F, Varela JM, Medrano FJ, De La Horra C (2007) Systemic inflammation in patients with chronic obstructive pulmonary disease who are colonized with Pneumocystis jiroveci. Clin Infect Dis 45(2):e17–e19. https://doi.org/10.1086/518989
Probst M, Ries H, Schmidt-Wieland T, Serr A (2000) Detection of Pneumocystis carinii DNA in patients with chronic lung diseases. Eur J Clin Microbiol Infect Dis 19:644–645. https://doi.org/10.1007/s100960000329
Vilar FJ, Khoo SH, Walley T (1999) The management of Pneumocystis carinii pneumonia. Br J Clin Pharmacol 47(6):605–609. https://doi.org/10.1046/j.1365-2125.1999.00966.x
WHO Media centre (2007) Fact sheet: the top ten causes of death. World Health Organization (WHO). Available online at: http://www.who.int/mediacentre/factsheets/fs310.pdf. Accessed 14 Nov 2017
Lawson DH, Paice BJ (1982) Adverse reactions to trimethoprim–sulfamethoxazole. Rev Infect Dis 4:429–433
Fraser TN, Avellaneda AA, Graviss EA, Musher DM (2012) Acute kidney injury associated with trimethoprim/sulfamethoxazole. J Antimicrob Chemother 67:1271–1277. https://doi.org/10.1093/jac/dks030
Lee KY, Huang CH, Tang HJ, Yang CJ, Ko WC, Chen YH, Lee YC, Hung CC (2012) Acute psychosis related to use of trimethoprim/sulfamethoxazole in the treatment of HIV-infected patients with Pneumocystis jirovecii pneumonia: a multicentre, retrospective study. J Antimicrob Chemother 67:2749–2754. https://doi.org/10.1093/jac/dks283
Ho JM, Juurlink DN (2011) Considerations when prescribing trimethoprim–sulfamethoxazole. CMAJ 183:1851–1858. https://doi.org/10.1503/cmaj
Yang JJ, Huang CH, Liu CE, Tang HJ, Yang CJ, Lee YC, Lee KY, Tsai MS, Lin SW, Chen YH, Lu PL, Hung CC (2014) Multicenter study of trimethoprim/sulfamethoxazole-related hepatotoxicity: incidence and associated factors among HIV-infected patients treated for Pneumocystis jirovecii pneumonia. PLoS One 9(9):e106141. https://doi.org/10.1371/journal.pone.0106141
Helweg-Larsen J, Benfield TL, Eugen-Olsen J, Lundgren JD, Lundgren B (1999) Effects of mutations in Pneumocystis carinii dihydropteroate synthase gene on outcome of AIDS-associated P carinii pneumonia. Lancet 354:1347–1351. https://doi.org/10.1016/S0140-6736(99)03320-6
Alvarez-Martínez MJ, Moreno A, Miró JM, Valls ME, Rivas PV, de Lazzari E, Sued O, Benito N, Domingo P, Ribera E, Santín M, Sirera G, Segura F, Vidal F, Rodríguez F, Riera M, Cordero ME, Arribas JR, Jiménez de Anta MT, Gatell JM, Wilson PE, Meshnick SR; Spanish PCP Working Group (2008) Pneumocystis jirovecii pneumonia in Spanish HIV-infected patients in the combined antiretroviral therapy era: prevalence of dihydropteroate synthase mutations and prognostic factors of mortality. Diagn Microbiol Infect Dis 62:34–43. https://doi.org/10.1016/j.diagmicrobio.2008.04.016
Navin TR, Beard CB, Huang L, del Rio C, Lee S, Pieniazek NJ, Carter JL, Le T, Hightower A, Rimland D (2001) Effect of mutations in Pneumocystis jirovecii dihydropteroate synthase gene on outcome of P jirovecii pneumonia in patients with HIV-1: a prospective study. Lancet 358:545–549. https://doi.org/10.1016/S0140-6736(01)05705-1
Queener SF, Cody V, Pace J, Torkelson P, Gangjee A (2013) Trimethoprim resistance of dihydrofolate reductase variants from clinical isolates of Pneumocystis jirovecii. Antimicrob Agents Chemothdicper 57:4990–4998. https://doi.org/10.1128/AAC.01161-13
Crothers K, Beard CB, Turner J, Groner G, Fox M, Morris A, Eiser S, Huang L (2005) Severity and outcome of HIV-associated Pneumocystis pneumonia containing Pneumocystis jirovecii dihydropteroate synthase gene mutations. AIDS 19(8):801–805. https://doi.org/10.1097/01.aids.0000168974.67090.70
Ma L, Borio L, Masur H, Kovacs JA (1999) Pneumocystis carinii dihydropteroate synthase but not dihydrofolate reductase gene mutations correlate with prior trimethoprim–sulfamethoxazole or dapsone use. J Infect Dis 180(6):1969–1978. https://doi.org/10.1086/315148
Vedantam G, Guay GG, Austria NE, Doktor SZ, Nichols BP (1998) Characterization of mutations contributing to sulfathiazole resistance in Escherichia coli. Antimicrob Agents Chemother 42:88–93
Lopez P, Espinosa M, Greenberg B, Lacks SA (1987) Sulfonamide resistance in Streptococcus pneumoniae: DNA sequence of the gene encoding dihydropteroate synthase and characterization of the enzyme. J Bacteriol 169:4320–4326. https://doi.org/10.1128/jb.169.9.4320-4326.1987
Brooks DR, Wang P, Read M, Watkins WM, Sims PF, Hyde JE (1994) Sequence variation of the hydroxymethyldihydropterin pyrophosphokinase: dihydropteroate synthase gene in lines of the human malaria parasite, Plasmodium falciparum, with differing resistance to sulfadoxine. Eur J Biochem 224:397–405. https://doi.org/10.1111/j.1432-1033.1994.00397.x
Triglia T, Menting JG, Wilson C, Cowman AF (1997) Mutations in dihydropteroate synthase are responsible for sulfone and sulfonamide resistance in Plasmodium falciparum. Proc Natl Acad Sci U S A 94:13944–13949
Kazanjian P, Armstrong W, Hossler PA, Burman W, Richardson J, Lee CH, Crane L, Katz J, Meshnick SR (2000) Pneumocystis carinii mutations are associated with duration of sulfa or sulfone prophylaxis exposure in AIDS patients. J Infect Dis 182:551–557. https://doi.org/10.1086/315719
Huang L, Morris A, Limper AH, Beck JM; ATS Pneumocystis Workshop Participants (2006) An Official ATS Workshop Summary: recent advances and future directions in Pneumocystis pneumonia (PCP). Proc Am Thorac Soc 3(8):655–664. https://doi.org/10.1513/pats.200602-015MS
Briceland LL, Bailie GR (1991) Pentamidine-associated nephrotoxicity and hyperkalemia in patients with AIDS. DICP 25:1171–1174
Lachaal M, Venuto RC (1989) Nephrotoxicity and hyperkalemia in patients with acquired immunodeficiency syndrome treated with pentamidine. Am J Med 87:260–263. https://doi.org/10.1016/S0002-9343(89)80147-0
Haile LG, Flaherty JF (1993) Atovaquone: a review. Ann Pharmacother 27(12):1488–1494. https://doi.org/10.1177/106002809302701215
Hawser S, Lociuro S, Islam K (2006) Dihydrofolate reductase inhibitors as antibacterial agents. Biochem Pharmacol 71:941–948. https://doi.org/10.1016/j.bcp.2005.10.052
Kohlhoff SA, Sharma R (2007) Iclaprim. Expert Opin Investig Drugs 16(9):1441–1448. Erratum in: Expert Opin Investig Drugs. 2007 Nov;16(11):1867. https://doi.org/10.1517/13543784.16.9.1441
Dei-Cas E, Cailliez JC; European Concerted Action on Pneumocystis carinii (1996) In vitro systems in Pneumocystis research. Parasitol Today 12:245–249. https://doi.org/10.1016/0169-4758(96)80812-X
Dei-Cas E, Brun-Pascaud M, Bille-Hansen V, Allaert A, Aliouat EM (1998) Animal models of pneumocystosis. FEMS Immunol Med Microbiol 22:163–168. https://doi.org/10.1111/j.1574-695X.1998.tb01201.x
Aviles P, Aliouat EM, Martinez A, Dei-Cas E, Herreros E, Dujardin L, Gargallo-Viola D (2000) In vitro pharmacodynamic parameters of sordarin derivatives in comparison with those of marketed compounds against Pneumocystis carinii isolated from rats. Antimicrob Agents Chemother 44:1284–1290. https://doi.org/10.1128/AAC.44.5.1284-1290.2000
Aliouat EM, Martinez A, Jimenez E, Dei-Cas E, Mullet C, Delcourt P, Gargallo-Viola D (1997) Development of pneumocystosis animal models: corticosteroid-treated Wistar rat; SCID mouse and nude rat. J Eukaryot Microbiol 44:41S–42S. https://doi.org/10.1111/j.1550-7408.1997.tb05765.x
Aliouat el-M, Dujardin L, Martínez A, Duriez T, Ricard I, Dei-Cas E (1999) Pneumocystis carinii growth kinetics in culture systems and in hosts: involvement of each life cycle parasite stage. J Eukaryot Microbiol 46:116S–117S
Garry S, Nesslany F, Aliouat E, Haguenoer JM, Marzin D (2003) Hematite (Fe(2)O(3)) enhances benzo[a]pyrene genotoxicity in endotracheally treated rat, as determined by comet assay. Mutat Res 538:19–29. https://doi.org/10.1016/S1383-5718(03)00082-2
Schmatz DM, Powles M, McFadden DC, Pittarelli LA, Liberator PA, Anderson JW (1991) Treatment and prevention of Pneumocystis carinii pneumonia and further elucidation of the P. carinii life cycle with 1,3-beta-glucan synthesis inhibitor L-671,329. J Protozool 38(6):151S–153S
Cushion MT, Linke MJ, Ashbaugh A, Sesterhenn T, Collins MS, Lynch K, Brubaker R, Walzer PD (2010) Echinocandin treatment of Pneumocystis pneumonia in rodent models depletes cysts leaving trophic burdens that cannot transmit the infection. PLoS One 5(1):e8524. https://doi.org/10.1371/journal.pone.0008524
Beltz K, Kramm CM, Laws HJ, Schroten H, Wessalowski R, Göbel U (2006) Combined trimethoprim and caspofungin treatment for severe Pneumocystis jiroveci pneumonia in a five year old boy with acute lymphoblastic leukemia. Klin Padiatr 218:177–179. https://doi.org/10.1055/s-2006-933433
Utili R, Durante-Mangoni E, Basilico C, Mattei A, Ragone E, Grossi P (2007) Efficacy of caspofungin addition to trimethoprim–sulfamethoxazole treatment for severe Pneumocystis pneumonia in solid organ transplant recipients. Transplantation 84:685–688. https://doi.org/10.1097/01.tp.0000280546.91617.6c
Tu GW, Ju MJ, Xu M, Rong RM, He YZ, Xue ZG, Zhu TY, Luo Z (2013) Combination of caspofungin and low-dose trimethoprim/sulfamethoxazole for the treatment of severe Pneumocystis jirovecii pneumonia in renal transplant recipients. Nephrology (Carlton) 18:736–742. https://doi.org/10.1111/nep.12133
Li H, Huang H, He H (2016) Successful treatment of severe Pneumocystis pneumonia in an immunosuppressed patient using caspofungin combined with clindamycin: a case report and literature review. BMC Pulm Med 16:144. https://doi.org/10.1186/s12890-016-0307-0
Lee WS, Hsueh PR, Hsieh TC, Chen FL, Ou TY, Jean SS (2017) Caspofungin salvage therapy in Pneumocystis jirovecii pneumonia. J Microbiol Immunol Infect 50(4):547–548. https://doi.org/10.1016/j.jmii.2016.03.008
National Committee for Clinical Laboratory Standards (NCCLS) (1997) Reference method for broth dilution antifungal susceptibility testing of yeasts; Approved standard M27-A. NCCLS, Villanova
Stringer JR (1996) Pneumocystis carinii: what is it, exactly? Clin Microbiol Rev 9:489–498
Cailliez JC, Séguy N, Denis CM, Aliouat EM, Mazars E, Polonelli L, Camus D, Dei-Cas E (1996) Pneumocystis carinii: an atypical fungal micro-organism. J Med Vet Mycol 34:227–239
Dei-Cas E, Aliouat EM, Cailliez JC (2004) Cellular structure. In: Walzer PD, Cushion MT (eds) Pneumocystis pneumonia, 3rd edn. Marcel Dekker, New York, pp 61–94
Pasqualotto AC, Denning DW (2008) New and emerging treatments for fungal infections. J Antimicrob Chemother 61(Suppl 1):i19–i30. https://doi.org/10.1093/jac/dkm428
Dei-Cas E, Fleurisse L, Aliouat EM, Bahon-Le Capon J, Cailliez JC, Creusy C (1998) Morphological and ultrastructural methods for Pneumocystis. FEMS Immunol Med Microbiol 22:185–189. https://doi.org/10.1111/j.1574-695X.1998.tb01205.x
Dei-Cas E, Chabé M, Moukhlis R, Durand-Joly I, Aliouat el M, Stringer JR, Cushion M, Noël C, de Hoog GS, Guillot J, Viscogliosi E (2006) Pneumocystis oryctolagi sp. nov., an uncultured fungus causing pneumonia in rabbits at weaning: review of current knowledge, and description of a new taxon on genotypic, phylogenetic and phenotypic bases. FEMS Microbiol Rev 30:853–871. https://doi.org/10.1111/j.1574-6976.2006.00037.x
Bartlett MS, Fishman JA, Queener SF, Durkin MM, Jay MA, Smith JW (1988) New rat model of Pneumocystis carinii infection. J Clin Microbiol 26(6):1100–1102
Andrews J, Honeybourne D, Ashby J, Jevons G, Fraise A, Fry P, Warrington S, Hawser S, Wise R (2007) Concentrations in plasma, epithelial lining fluid, alveolar macrophages and bronchial mucosa after a single intravenous dose of 1.6 mg/kg of iclaprim (AR-100) in healthy men. J Antimicrob Chemother 60:677–680. https://doi.org/10.1093/jac/dkm242
Huang DB, File TM Jr, Torres A, Shorr AF, Wilcox MH, Hadvary P, Dryden M, Corey GR (2017) A phase II randomized, double-blind, multicenter study to evaluate efficacy and safety of intravenous iclaprim versus vancomycin for the treatment of nosocomial pneumonia suspected or confirmed to be due to gram-positive pathogens. Clin Ther 39:1706–1718. https://doi.org/10.1016/j.clinthera.2017.07.007
Funding
This study was funded by Motif BioSciences Inc., New York, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DBH is an employee of Motif BioSciences. SH is an employee of IHMA.
Ethical approval
This research involved animals. All procedures in this research were in compliance with the Animal Welfare Act, the Guide for the Care and Use of Laboratory Animals, and the Office of Laboratory Animal Welfare.
Additional information
E. Dei-Cas died before publication of this work was completed.
Rights and permissions
About this article
Cite this article
Aliouat, E.M., Dei-Cas, E., Gantois, N. et al. In vitro and in vivo activity of iclaprim, a diaminopyrimidine compound and potential therapeutic alternative against Pneumocystis pneumonia. Eur J Clin Microbiol Infect Dis 37, 409–415 (2018). https://doi.org/10.1007/s10096-018-3184-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3184-z