Abstract
The epidemiology of healthcare-associated meningitis (HAM) is dominated by commensal bacteria from the skin, as coagulase-negative staphylococci (CoNS). We hypothesized that the pauci-symptomatic and mild inflammatory patterns of HAM are related to the low pathogenic state of CoNS. Our aim was to describe clinical and biological features of CoNS HAM, compared to other HAM. All consecutive patients with HAM admitted in our hospital were retrospectively included from 2007 to 2014. HAM due to CoNS were compared to HAM caused by other bacteria (controls) for clinical and laboratory patterns. Seventy-one cases of HAM were included, comprising 18 CoNS and 53 controls. Patients were not different in terms of baseline characteristics. CoNS HAM occurred later after the last surgery than controls (17 vs. 12 days, p = 0.029) and had higher Glasgow Coma Scale (GCS) score (14 vs. 13, p = 0.038). Cerebrospinal fluid (CSF) analysis revealed a lower pleocytosis (25 vs. 1340/mm3, p < 0.001), a higher glucose level (3.75 vs. 0.8 mmol/L, p < 0.001), and a lower protein level (744 vs. 1751 mg/L, p < 0.001) in the CoNS group than in the control group, respectively. HAM due to CoNS was significantly less symptomatic and less inflammatory than HAM due to other bacteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The central nervous system (CNS) is a sanctuary protected against microbial invasion by the cranial vault and the blood–brain barrier (BBB). Physiologically, only a few bacterial strains can cross the BBB, whose integrity can be disrupted by invasive procedures (craniotomy, placement of cerebrospinal fluid shunts, spinal anesthesia, etc.) or traumatic brain injury, allowing any bacterial strain to invade the CNS [1], leading to healthcare-associated meningitis (HAM). Morbidity and mortality of HAM in combination with the increasing number of neurosurgical procedures raise concern, especially because their diagnostic is troublesome.
Despite significant efforts made by the Centers for Disease Control and Prevention (CDC) to propose an accurate definition [2], there is no consensus. The most commonly used definition in the literature is based solely on the isolation in cerebrospinal fluid (CSF) culture of a bacterium [3,4,5]. Indeed, clinical diagnosis can be impaired by nonspecific symptoms, overlapping with those of underlying diseases or hidden by intensive care treatments, such as sedative drugs [4, 6, 7]. Besides, Schade et al. [8], reporting the CSF “normality” in neurosurgical patients, showed the lack of value of CSF leukocyte count and protein or glucose concentration in HAM diagnosis. A dynamic approach of these CSF parameters was proposed by some authors to help diagnosis [5, 9]. However, everybody seems to agree that HAM have less obvious clinical and biological patterns than community-acquired meningitis [1, 4, 10].
Furthermore, the epidemiology of HAM is dominated by low-grade or accidental pathogens [coagulase-negative staphylococci (CoNS), Propionibacterium spp., Corynebacterium spp.], which are commensal strains of the human skin and lack classical virulence factors [11], unlike traditional pathogens (Staphylococcus aureus, Enterobacteriaceae, Pseudomonas aeruginosa, etc.). However, CoNS are considered as a major source of healthcare-associated infections, especially foreign body-related ones, characterized by a subacute course with a mild clinical picture [12]. In respect of HAM, they are found in 22–69% of cases [1, 3,4,5, 7, 9, 13,14,15,16,17].
To our knowledge, there are only two studies describing CoNS meningitis. The first one compared CoNS meningitis with bacterial meningitis admitted to the hospital and found that the former had all postneurosurgical conditions with device placement. Multivariate analysis showed that only a low CSF protein level was associated with CoNS [18]. The second work compared CoNS meningitis with S. aureus meningitis. CoNS infections occurred in younger patients and had a better chance of survival [19]. But those two studies used a definition for CoNS meningitis with several clinical and inflammation criteria, which could have missed pauci-symptomatic infections. Conversely, they included community-acquired meningitis in their comparison, which could have increased the differences with CoNS HAM.
We hypothesized that the indolent, pauci-symptomatic, and mild inflammatory patterns of HAM could be related to the predominance of low-grade pathogens, in this case CoNS.
The main goal of this study was to compare the clinical and biological features of CoNS HAM to other HAM. Secondary objectives were to analyze their bacteriological data and their outcome.
Methods
Design and patients
This retrospective study was performed at a French tertiary care university hospital, between January 2007 and December 2014.
All consecutive patients older than 18 years of age, who had a diagnosis of bacterial HAM with a microbiological documentation and an appropriate antibiotic treatment, were included. They were identified from a microbiological database reporting all positive CSF cultures within this period, and then from their medical records. Meningitis due to low-grade pathogens other than CoNS were excluded (Corynebacterium spp. and Propionibacterium spp.), as well as those complicated by an abscess or an empyema and the patients with missing files. Patients with positive CSF culture but without antimicrobial treatment were not included.
Patients were divided into two groups according to the causative bacteria: CoNS versus traditional pathogens (controls). Mixed bacterial meningitis were classified in the control group if at least one of the bacteria was a traditional pathogen.
Definitions
Meningitis was defined as every positive single or serial CSF culture considered and treated like one by the medical team. For CoNS, two consecutive positive samples of the same strain, characterized by the same antibiotype [20], were required for the diagnosis of meningitis.
HAM was defined if infection occurred after 48 h of hospitalization or less than a year after implementation of a neurosurgical device [2].
In this study, neurosurgical devices encompassed any material designed to drain the CSF, either temporary (external ventricular drain and external lumbar drain) or permanent (ventriculo-atrial shunt and ventriculo-peritoneal shunt). An infection was considered device-related if it developed at least 48 h after shunt placement and, at the latest, 10 days after shunt removal.
We arbitrarily defined day 0 (D0) as the day of antibiotic initiation. An appropriate antibiotic treatment was characterized by: (1) a molecule known to disseminate to the meninges, (2) active on the isolated bacteria, (3) with a dosage adapted to this type of infection, and (4) for a period of more than 72 h.
A related bacteremia was defined as one positive blood culture with the same strain as the one isolated in CSF between D−5 and the end of antibiotic treatment.
A concomitant infection was identified when the patient needed an antibiotic therapy for another infection (i.e., another location and bacterium) at the time meningitis was diagnosed or during its treatment.
We considered that the treatment failed when there was a relapse or a death related to the infection. A relapse was defined as a meningitis that occurred within three months after remission of the previous episode and for which the same bacterium was isolated. Every deceased patient was analyzed by two independent physicians in order to identify whether the source of death was linked to the meningitis or not. If their opinions differed, death was considered not related.
A new infection was characterized either by a 3-month delay in development or by the onset of an infection from a different microorganism than the one responsible for the first episode, the latter not being considered as a treatment failure [4].
The patient outcome was also assessed using mortality from all causes at D28 and at one year and the Glasgow Outcome Scale (GOS) score at 3 months.
Local procedures
Operating room procedure
All neurosurgical devices were placed in the operating room, following strict aseptic conditions. The antimicrobial prophylaxis in our institution was the one recommended by the French scientific societies [21].
External ventricular drains handling
In our hospital, external ventricular drains (EVDs) were sampled every day via the drip chamber stopcock. CSF samples were sent to the laboratory for biochemical and bacteriological analyses (direct examination using Gram staining and culture). When direct examination of CSF was positive, the procedure was as follows: (1) a neurosurgeon performed a new sampling via the proximal stopcock and (2) the CSF external drainage line was changed. Antibiotic treatment was initiated: (1) if the patient’s condition was getting worse, (2) if the culture of CSF sampled from the proximal stopcock was positive to the same bacterium as the one of the distal specimen, and (3) if the daily CSF sampling with the new line had a positive culture with the same microorganism.
In other cases, CSF sampling was performed using the aseptic procedure at the request of the medical team, when meningitis was suspected, with a lumbar puncture or a valve puncture in the operating room. Antibiotic treatment was introduced until the result of the CSF culture, and then adapted in case of positive CSF culture.
When the infection occurred on an indwelling device, it was withdrawn and replaced, if necessary, after at least two negative cultures, under antibiotic treatment. Every removed device was sent to the bacteriology laboratory for analysis.
Microbiology
Culture media included 5% sheep blood agar, chocolate agar (in 5% CO2), trypticase soy agar, MacConkey agar, and Schaedler broth. All were incubated at 35–37 °C for 5 days under aerobic conditions and for 10 days under anaerobic conditions. Bacteria were identified by means of standard biochemical tests. Susceptibility testing was performed by the agar dilution replicate plating method and, if necessary, the minimal inhibitory concentration (MIC) was determined by the Etest.
If CoNS grew in culture, the strain was preserved for a further comparison with a second sample. Two CoNS were considered to belong to the same strain when their MICs of ten antibiotics were identical (± one standard dilution) [20].
Data collection
Patients’ records were reviewed to recover demographic and clinical data. Biological and bacteriological results were retrieved from the hospital computerized database. We extracted the medical history: age, gender, significant comorbidities, diagnosis at admission, severity scores [Glasgow Coma Scale (GCS) score, Simplified Acute Physiology Score II (SAPS II)], intensive care unit (ICU) admission, date of the last brain surgery, and type of indwelling device. Usual clinical and biological criteria of meningitis were documented from D−5 until the last day of antibiotic therapy. Bacteriological data included all CSF samples from D−5 until the end of treatment, cultures of medical devices, and all the blood cultures from D−5 to D5. We also recorded if there was a concomitant infection. Regarding treatment, the use and duration of antimicrobial therapy and the type of surgical procedure were recorded. Finally, we documented the success or failure of treatment, relapse, second meningitis, the GOS score at 3 months, and the mortality from all causes at 28 days and at one year. Every patient was followed for one year.
Statistical analysis
Statistical analyses were performed using the SPSS software (version 20.0, IBM Corp., Armonk, NY). Quantitative values were expressed as medians and 25th and 75th percentiles, and compared with the non-parametric Mann–Whitney test. Qualitative values were expressed as numbers and percentages and compared with Fisher’s exact test. The survival was analyzed by the Kaplan–Meier method. A p-value < 0.05 was considered significant.
Results
Demographic characteristics
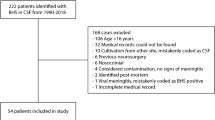
During the study period, 411 patients with positive CSF samples were screened. Among them, 71 HAM were analyzed (64 patients): 18 (25.4%) caused by CoNS and 53 (74.6%) in the control group (Fig. 1).
At diagnosis, the two groups were similar in terms of age, gender, immune status, cause of hospitalization, ICU admission, and initial GCS and SAPS II scores. The risk factors for HAM did not differ either (Table 1).
Most of the infections occurred in patients having indwelling devices: 16 (88.9%) in the CoNS group and 36 (67.9%) in the control group (p = 0.32). The various kinds of foreign bodies are indicated in Table 2. There were less EVDs in the CoNS group: 7 (43.8%) versus 28 (75.7%) in the controls (p = 0.025) and more ventriculo-atrial shunts: 7 (43.8%) versus 4 (10.8%), respectively (p = 0.023).
All the other cases arose in a postoperatory situation, with the exception of one brain-injured patient in the control group.
Clinical and biological characteristics
Table 3 summarizes the clinical signs and serum findings at the time of meningitis diagnosis. The median time since the last surgery to the occurrence of infection was significantly longer in the CoNS group than in the control group: 17 days [11–35] versus 12 days [6–18] (p = 0.029). There was also a significantly higher GCS score at D0 in the CoNS group: 14 [13–15] versus 13 [7–15] (p = 0.038), while there was no difference in terms of fever, meningeal stiffness, and local signs of infection from the controls.
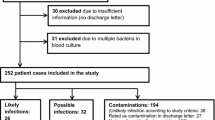
Regarding serum biology, the white blood cell (WBC) count at D0 was significantly lower in the CoNS group than in the controls, but serum C-reactive protein (CRP) did not differ between the groups. In respect of CSF, all cytological and biochemical features of these samples at D0 differed significantly between both groups (Fig. 2): there were less leukocytes (25/mm3 [19–382.5] vs. 1340/mm3 [298.8–4320], p < 0.001) and less granulocytes (65% [15.8–80.8] vs. 89% [76.5–95], p = 0.001) in the CoNS group than in the controls, respectively. There was also a lower protein level (744 mg/L [394.5–1555] vs. 1751 mg/L [1372–5990.3], p < 0.001) and a higher glucose level (3.75 mmol/L [2.1–4.4] vs. 0.8 mmol/L [0.1–2.8], p < 0.001) in the CoNS group than in the controls, respectively.
Microbiology
The bacteria responsible for these infections are shown in Table 4. Fourteen meningitis were polymicrobial, four in the CoNS group and ten in the control group. There were 54 (63.5%) Gram-positive cocci and 31 (36.5%) Gram-negative bacilli.
Among staphylococci, 18 (69.2%) CoNS and 5 (45.5%) S. aureus were methicillin-resistant. A related bacteremia was found in 8 (57.1%) CoNS episodes and 10 (20%) controls (p = 0.015). There was no difference in the median number of positive CSF samples: 3 [2–4] in the CoNS group and 2 [1–4] in the control group (p = 0.54). The percentage of positive indwelling device cultures was 81.8% for CoNS HAM and 47.6% for other HAM (p = 0.13).
A concomitant infection was diagnosed in 3 (17.6%) CoNS and 21 (40.4%) controls, but this result did not reach statistical significance either (Table 5).
Outcome
All patients received systemic antibiotic therapy, for a median duration of 19 days (14–21) in the CoNS group and 16 days (10–21) in controls (p = 0.72). Only a few patients had intraventricular infusion of antimicrobial agents.
All indwelling devices were removed except in two patients, whose outcome was not favorable: one relapsed in the CoNS group and the other died in the control group.
Treatment failure occurred in 1 (5.6%) CoNS HAM (relapse) and 12 (23.1%) controls (two relapses and ten deaths related to the meningitis) (p = 0.16).
A second meningitis was diagnosed in 4 patients (22.2%) in the CoNS group and 3 patients (5.9%) in the control group (p = 0.064).
Three months after the meningitis, the number and percentage of patients with a GOS score ≤ 3 were not different between both groups: 12 (75%) in the CoNS group and 29 (56.9%) in the control group (p = 0.19).
There were no deaths, from all causes, at D28 in the CoNS group versus 12 (23.1%) in the control group (p = 0.03), and 1 (5.9%) at one year versus 18 (34.6%) (p = 0.027), respectively.
Figure 3 shows the Kaplan–Meier probability of survival at D28 and one year.
Discussion
HAM are often considered as infections with mild clinical and biological features [1, 4, 10]. CoNS are found in the literature as a major cause of HAM [6, 7, 15, 17] and the particular characteristic of CoNS (mostly S. epidermidis) is the lack of virulence factors, apart from their ability to form biofilm [11, 12]. We hypothesized that these two facts could explain the indolent features of HAM. For that, we compared CoNS HAM to HAM due to traditional or high-grade pathogens (controls). Thus, in this eight-year study, we found that CoNS were responsible for 25.4% of our HAM. CoNS infections occurred later after the last surgery and had less profound consciousness disorders than controls. They also had a lower inflammatory response in blood with a lower WBC count and in CSF with a lower leukocyte count, a lower protein level, and a higher glucose level, which is consistent with our hypothesis. Finally, the probability of survival of CoNS HAM was higher than that of the controls.
On the contrary, control HAM were not pauci-symptomatic, since 51 (98.1%) of patients had fever, more than half had altered consciousness, and 25 (67.6%) had meningeal stiffness. They also had a degree of inflammation in CSF close to community-acquired meningitis, with 1340 [298.8–4320] leukocytes/mm3, 89% [76.5–95] granulocytes, 1751 mg/L [1372–5990.3] protein level, and 0.8 mmol/L [0.1–2.8] glucose level [22, 23]. Hence, the clinical and biological patterns of HAM depend on the bacterial species implicated.
Indeed, CoNS have no or limited virulence factors, leading some authors to name it as the “accidental pathogen” [11]. These skin colonizers have not evolved to cause a disease but to maintain the benign relationship with their hosts. Their pathogenic potential relies on their ability to produce biofilm on the surface of indwelling medical devices [12, 24]. During the early phase of infection, the capacity of CoNS to secrete pro-inflammatory peptides, as phenol-soluble modulins, is downregulated, protecting the bacteria from clearance and allowing the formation of biofilm [25]. Biofilm-forming bacteria have both phenotypic and genotypic adaptations, enabling them to coexist with the host response for a prolonged time, even though they induce a co-activation of the innate and the adaptive immune system, which is often unable to eradicate the infection but causes low-grade damages, through frustrated phagocytosis, explaining the symptomatology [26].
As a result, the vast majority of CoNS infections are characterized by a subacute or chronic course, with a subtle clinical picture and no fulminant signs of infections [12, 27], and HAM are no exception. In particular, we found that the protein level in CSF, which is a major marker of meningeal inflammation, was lower in the CoNS group, as Huang et al. [18] had previously described.
Further, the median time after surgery was longer in the CoNS group than in the controls, unlike other studies [4, 18], but this result is compatible with data from other CoNS infections, as in infective endocarditis [12]. This could contribute to the lower degree of inflammation in CSF.
As expected, the majority of our CoNS HAM were foreign body-related. However, this result was not significantly different from the control group, probably because of a lack of statistical power. The only two cases of CoNS meningitis without neurosurgical material concerned intensive care patients having incurred a long surgery, that caused bony sequestra, on which bacteria can build their biofilm [28].
Hence, the growing number of invasive procedures and indwelling device placements provides optimal conditions for CoNS and explains their increasing role in healthcare-associated infections. However, in our study, CoNS were only responsible for 18 HAM (25.4%), which was in the lower range of other studies. But two CSF samples positive to the same strain of CoNS were required, which could have lowered the proportion of CoNS HAM recorded in our study. Indeed, recent studies with the same criterion detected between 18.4% and 22% of CoNS HAM [5, 18, 19, 29].
CoNS, as usual contaminants of microbiological samples, are difficult to incriminate. Some authors proposed to isolate the same strain of CoNS in at least two different cultures, to help distinguish between contamination and infection [6, 18], this rule being already applied in the diagnosis of bacteremia [2]. Moreover, we did not include 11 cases with several CSF samples positive to the same CoNS, but with no treatment. Indeed, the positivity of several consecutive samples with the same strain of CoNS might not be enough to make a diagnosis of HAM. Other factors are part of the equation; for instance, changes in CSF chemistry and cellularity [5]. Another possible explanation is that these are biofilm-associated infections, with sessile bacteria, which do not cause an inflammatory reaction (yet) and it could be interesting to follow these patients, to find out if they are going to develop a pauci-symptomatic meningitis or a shunt dysfunction [30].
The microbiological data showed, somewhat surprisingly, a bacteremia with the same organism more often in the CoNS group than in the controls. This result can be explained by the fact that there were more ventriculo-atrial shunts among the CoNS HAM. Indeed, these devices are at greater risk for bacteremia than others [1]. Another possible explanation might be related to the method used to identify related strains of CoNS through their antibiotype. In fact, the phenotypic identification methods could fail to discriminate close, but distinguishable strains of CoNS. On the contrary, the genotypic methods suffer from excessive sensitivity and highlight minor genetic differences, which may only reflect the genetic flexibility of one and the same strain [31, 32]. Moreover, genotypic techniques are still time-consuming and expensive. Given the fact that our study is retrospective, we did not get to choose among those methods. However, the Etest is the reference for MIC determination with great sensitivity and specificity, and is more suitable for clinical practice than genotypic techniques, for now.
Finally, we found that CoNS meningitis had better survival probabilities at 28 days and one year, which is in line with other studies [18, 19] and could also reflect the low virulence of CoNS. However, there were no difference in the GOS score at 3 months between both groups, but confounding factors, such as the original mental state of the patients, were not recorded.
Other limitations of our study that need to be discussed are related to the retrospective design, which was a necessity considering the low incidence of HAM. Despite that and given our sample size, we could not carry out a logistic regression analysis with enough variables. We could have performed a multicenter study, but the lack of standardized procedures for EVDs management could have led to important methodological bias. Hence, our findings need further confirmation.
To this end, future studies should use a microbiological definition, based on the isolation of a microorganism in CSF culture, with the need to detect the same strain in at least two samples for commensal bacteria, such as CoNS. It could be necessary to include recent changes in biological features in this definition, rather than static thresholds that could miss these indolent infections.
Conclusion
We have shown that the indolent, pauci-symptomatic, and mild inflammatory presentation of healthcare-associated meningitis (HAM) is linked to low-grade pathogens, coagulase-negative staphylococci (CoNS), which are mostly indwelling device-related. Their lack of virulence could also explain the better prognostic we have found, when comparing these infections to other HAM.
The rarely life-threatening nature of these HAM should not make us underestimate CoNS, which are responsible for more and more healthcare-associated infections and are becoming a major concern for the next decades.
References
van de Beek D, Drake JM, Tunkel AR (2010) Nosocomial bacterial meningitis. N Engl J Med 362(2):146–154
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Mayhall CG, Archer NH, Lamb VA, Spadora AC, Baggett JW, Ward JD et al (1984) Ventriculostomy-related infections. A prospective epidemiologic study. N Engl J Med 310(9):553–559
Conen A, Walti LN, Merlo A, Fluckiger U, Battegay M, Trampuz A (2008) Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: a retrospective analysis over an 11-year period. Clin Infect Dis 47(1):73–82
Mounier R, Lobo D, Cook F, Fratani A, Attias A, Martin M et al (2015) Clinical, biological, and microbiological pattern associated with ventriculostomy-related infection: a retrospective longitudinal study. Acta Neurochir 157(12):2209–2217
Muttaiyah S, Ritchie S, Upton A, Roberts S (2008) Clinical parameters do not predict infection in patients with external ventricular drains: a retrospective observational study of daily cerebrospinal fluid analysis. J Med Microbiol 57:207–209
Walti LN, Conen A, Coward J, Jost GF, Trampuz A (2013) Characteristics of infections associated with external ventricular drains of cerebrospinal fluid. J Infect 66(5):424–431
Schade RP, Schinkel J, Roelandse FW, Geskus RB, Visser LG, van Dijk MC et al (2006) Lack of value of routine analysis of cerebrospinal fluid for prediction and diagnosis of external drainage-related bacterial meningitis. J Neurosurg 104(1):101–108
Pfisterer W, Mühlbauer M, Czech T, Reinprecht A (2003) Early diagnosis of external ventricular drainage infection: results of a prospective study. J Neurol Neurosurg Psychiatry 74(7):929–932
Tunkel AR, Hasbun R, Bhimraj A, Byers K, Kaplan SL, Michael Scheld W et al (2017) 2017 Infectious Diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis 64:e34–e65. https://doi.org/10.1093/cid/ciw861
Otto M (2009) Staphylococcus epidermidis—the ‘accidental’ pathogen. Nat Rev Microbiol 7(8):555–567
Becker K, Heilmann C, Peters G (2014) Coagulase-negative staphylococci. Clin Microbiol Rev 27(4):870–926
Lozier AP, Sciacca RR, Romagnoli MF, Connolly ES Jr (2002) Ventriculostomy-related infections: a critical review of the literature. Neurosurgery 51(1):170–182
Williamson RA, Phillips-Bute BG, McDonagh DL, Gray MC, Zomorodi AR, Olson DM et al (2014) Predictors of extraventricular drain-associated bacterial ventriculitis. J Crit Care 29(1):77–82
Korinek A-M, Fulla-Oller L, Boch AL, Golmard JL, Hadiji B, Puybasset L (2011) Morbidity of ventricular cerebrospinal fluid shunt surgery in adults: an 8-year study. Neurosurgery 68(4):985–995
Korinek A-M, Baugnon T, Golmard JL, van Effenterre R, Coriat P, Puybasset L (2006) Risk factors for adult nosocomial meningitis after craniotomy: role of antibiotic prophylaxis. Neurosurgery 59(1):126–133
Scheithauer S, Bürgel U, Ryang YM, Haase G, Schiefer J, Koch S et al (2009) Prospective surveillance of drain associated meningitis/ventriculitis in a neurosurgery and neurological intensive care unit. J Neurol Neurosurg Psychiatry 80(12):1381–1385
Huang C-R, Lu C-H, Wu J-J, Chang H-W, Chien C-C, Lei C-B et al (2005) Coagulase-negative staphylococcal meningitis in adults: clinical characteristics and therapeutic outcomes. Infection 33(2):56–60
Chang W-N, Lu C-H, Huang C-R, Chuang Y-C, Tsai N-W, Chen S-F et al (2007) Epidemiology of adult staphylococcal meningitis in southern Taiwan: a clinical comparison of Staphylococcus aureus infection and coagulase-negative staphylococcal infection. Jpn J Infect Dis 60(2):262–266
Khatib R, Riederer KM, Clark JA, Khatib S, Briski LE, Wilson FM (1995) Coagulase-negative staphylococci in multiple blood cultures: strain relatedness and determinants of same-strain bacteremia. J Clin Microbiol 33(4):816–820
Société Française d’Anesthésie et de Réanimation (2011) Antibioprophylaxis in surgery and interventional medicine (adult patients). Actualization 2010. Ann Fr Anesth Reanim 30(2):168–190
van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M (2004) Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 351(18):1849–1859
Bijlsma MW, Brouwer MC, Kasanmoentalib ES, Kloek AT, Lucas MJ, Tanck MW et al (2016) Community-acquired bacterial meningitis in adults in the Netherlands, 2006–14: a prospective cohort study. Lancet Infect Dis 16(3):339–347
von Eiff C, Peters G, Heilmann C (2002) Pathogenesis of infections due to coagulase-negative staphylococci. Lancet Infect Dis 2(11):677–685
Vuong C, Dürr M, Carmody AB, Peschel A, Klebanoff SJ, Otto M (2004) Regulated expression of pathogen-associated molecular pattern molecules in Staphylococcus epidermidis: quorum-sensing determines pro-inflammatory capacity and production of phenol-soluble modulins. Cell Microbiol 6(8):753–759
Braxton EE, Ehrlich GD, Hall-Stoodley L, Stoodley P, Veeh R, Fux C et al (2005) Role of biofilms in neurosurgical device-related infections. Neurosurg Rev 28(4):249–255
Rogers KL, Fey PD, Rupp ME (2009) Coagulase-negative staphylococcal infections. Infect Dis Clin North Am 23(1):73–98
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284(5418):1318–1322
Mounier R, Lobo D, Cook F, Martin M, Attias A, Aït-Mamar B et al (2015) From the skin to the brain: pathophysiology of colonization and infection of external ventricular drain, a prospective observational study. PLoS One 10(11):e0142320. https://doi.org/10.1371/journal.pone.0142320
Mounier R, Kapandji N, Birnbaum R, Cook F, Rodriguez C, Nebbad B et al (2016) Biofilm-associated infection: the hidden face of cerebrospinal fluid shunt malfunction. Acta Neurochir 158(12):2321–2324
Widerström M, Wiström J, Sjöstedt A, Monsen T (2012) Coagulase-negative staphylococci: update on the molecular epidemiology and clinical presentation, with a focus on Staphylococcus epidermidis and Staphylococcus saprophyticus. Eur J Clin Microbiol Infect Dis 31(1):7–20
Ziebuhr W, Dietrich K, Trautmann M, Wilhelm M (2000) Chromosomal rearrangements affecting biofilm production and antibiotic resistance in a Staphylococcus epidermidis strain causing shunt-associated ventriculitis. Int J Med Microbiol 290(1):115–120
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the local ethical committee. All procedures were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments. For this type of study (retrospective), formal consent is not required.
Rights and permissions
About this article
Cite this article
Couffin, S., Lobo, D., Cook, F. et al. Coagulase-negative staphylococci are associated to the mild inflammatory pattern of healthcare-associated meningitis: a retrospective study. Eur J Clin Microbiol Infect Dis 37, 755–763 (2018). https://doi.org/10.1007/s10096-017-3171-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3171-9