Abstract
Quinolones are a family of synthetic broad-spectrum antimicrobial drugs. These molecules have been widely prescribed to treat various infectious diseases and have been classified into several generations based on their spectrum of activity. Quinolones inhibit bacterial DNA synthesis by interfering with the action of DNA gyrase and topoisomerase IV. Mutations in the genes encoding these targets are the most common mechanisms of high-level fluoroquinolone resistance. Moreover, three mechanisms for plasmid-mediated quinolone resistance (PMQR) have been discovered since 1998 and include Qnr proteins, the aminoglycoside acetyltransferase AAC(6′)-Ib-cr, and plasmid-mediated efflux pumps QepA and OqxAB. Plasmids with these mechanisms often encode additional antimicrobial resistance (extended spectrum beta-lactamases [ESBLs] and plasmidic AmpC [pAmpC] ß-lactamases) and can transfer multidrug resistance. The PMQR determinants are disseminated in Mediterranean countries with prevalence relatively high depending on the sources and the regions, highlighting the necessity of long-term surveillance for the future monitoring of trends in the occurrence of PMQR genes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quinolones constitute an important class of broad-spectrum antibacterial drugs and are used for the treatment of various infections. Since the introduction of the first molecule, nalidixic acid, into clinical therapy [1], other molecules have been developed, extending their spectrum of activity [2]. However, increased use of quinolones has led to increasing resistance to these antimicrobials [3]. Indeed, apart from chromosomally encoded quinolone resistance, in the 2000s new mechanisms of quinolone resistance emerged, plasmid-mediated with three mechanisms known so far: Qnr peptides, the aminoglycoside acetyltransferase variant AAC(6′)-Ib-cr, and plasmidic efflux pumps QepA and OqxAB [4]. During the last decade plasmid-mediated quinolone resistance (PMQR) has been increasingly reported in Enterobacteriaceae worldwide [5], including Mediterranean countries that constitute a region with an heterogeneous population from the north of Africa and the south of Europe and the Middle East. This literature review presents a description of the chromosomal and plasmidic fluoroquinolone resistance mechanisms known to date and the epidemiology of occurrence of PMQR determinants in Enterobacteriaceae in Mediterranean countries, with aim of gaining a better understanding of the current situation.
Quinolone structure and clinical use
Quinolones are a family of synthetic broad-spectrum antimicrobial drugs developed by modification of 1-alkyl-1,8-naphthyridin-4-one-3-carboxylic acid [6]. Nalidixic acid was the first molecule introduced into clinical therapy in the early 1960s that was obtained during the synthesis of chloroquine. It had limited clinical use because it was only sufficient for treatment of urinary tract infections and because of the early emergence of resistance [1]. Pharmacological improvements on the basic quinolone ring with the addition of fluorine at position C6 and piperazinyl or related rings at position C7 yielded the fluoroquinolones [7]. Thereby, newer class quinolones that expand the spectrum of activity to include Gram-positive bacteria and even anaerobics were developed in the 1980s (Fig. 1).
Chemical structure of some of the quinolones used in clinical practice (http://www.chemspider.com/)
High bioavailability, relatively low toxicity, and favorable pharmacokinetics have resulted in the clinical success of fluoroquinolones. Thus, these molecules have been widely prescribed to treat respiratory tract infections, including tuberculosis, urinary tract infections (UTIs), intra-abdominal infections, skin and skin structure infections, sexually transmitted diseases, and bone and joint infections [2]. The molecules most frequently used in clinical practice are ciprofloxacin, levofloxacin, and moxifloxacin. They achieve higher serum levels leading to better tissue penetration and greater potency against Enterobacteriaceae and other species [8]. The quinolones that are clinically available have been classified into several generations based on their spectrum of activity (Table 1) [9].
Some quinolone derivatives demonstrated inhibitory potential against eukaryote topoisomerase II and substantial dose-dependent cytotoxic potential against some cancerous cells [10]. Moreover, some quinolones, such as 6-chloro-7-methoxy4(1H)-quinolones, have good antimalarial activity and good activity against multiple stages of Plasmodium infection [11]. Fluoroquinolones, such as enrofloxacin, have also been extensively used in veterinary medicine to treat and prevent bacterial infections in food-producing animals, aquaculture, and pets, along with growth promoters [12].
Mechanism of action
Quinolones inhibit bacterial DNA synthesis by interfering with the action of two essential bacterial enzymes, DNA gyrase and topoisomerase IV. Both are heterotetrameric type II topoisomerase enzymes breaking transiently both strands of a duplex and pass another double-helical segment through the break by ATP hydrolysis [13]. The DNA gyrase introduces negative supercoils (or relaxes positive supercoils) into DNA, whereas topoisomerase IV exhibits a potent decatenation activity. Those enzymes are essential for bacterial growth as they control the topological status of the chromosomal DNA to facilitate replication, transcription, recombination, and DNA repair [13].
These enzymes comprise two copies of each of either a GyrA (97 kDa) and GyrB (90 kDa) subunit or a ParC (75 kDa) and ParE (70 kDa; GrlA and GrlB in the Staphylococcus aureus) subunit respectively. A few bacteria are able to function with only DNA gyrase, such as Mycobacterium tuberculosis, Helicobacter pylori, and Treponema pallidum, but most bacteria have both enzymes [8]. The targeting of either DNA gyrase or topoisomerase IV as the primary target by fluoroquinolones varies with bacterial species and the specific fluoroquinolone; however, as a broad generalization, the key target in Gram-negative bacteria is DNA gyrase, whereas in Gram-positive microorganisms topoisomerase IV is preferentially targeted [14]. Nevertheless, some recently developed quinolones, such as clinafloxacin and moxifloxacin, have a similar affinity for both targets [15].
Quinolones bind the DNA–enzyme complex of topoisomerase, forming a quinolone–enzyme–DNA complex (known as a ternary complex) in which the type II topoisomerase is trapped with the bound DNA [14]. The drug–enzyme–DNA complexes block cell growth. The bactericidal activity is due to the releasing of double-stranded DNA breaks from those complexes (chromosomal fragmentation process). Furthermore, an indirect route could be responsible for the lethal effect of quinolones, related to reactive oxygen species and/or toxin–antitoxin systems [16, 17]. A bacteriostatic effect is observed at low quinine concentrations (around the minimum inhibitory concentrations [MICs]), with cleaved complexes blocking DNA replication reversibly and inducing the SOS stress response, which in Escherichia coli results in upregulation of various stress response genes that enhance DNA repair capability, leading to the formation of filamentous cells because of the inhibition of cell division [18].
Chromosome-encoded resistance mechanisms
Alterations in target enzymes
The most common mechanism of high-level fluoroquinolone resistance is due to mutations in one or more of the genes that encode the primary and secondary targets of these drugs, the type II topoisomerases (gyrA, gyrB, parC, and parE) [19, 20]. These alterations have been localized mainly in the amino terminal domains of GyrA (residues 67 to 106 for E. coli numbering) or ParC (residues 63–102) and are in proximity to the active site of tyrosines (Tyr122 for GyrA, Tyr120 for ParC), which are covalently linked to DNA in an enzyme intermediate in both enzymes. This domain has been termed the “quinolone resistance determining region” (QRDR) [19, 21, 22]. However, some mutations localized outside the QRDR region, such as position 51, can also lead to decreased susceptibility to the quinolones [15].
Mutations in the QRDR of the topoisomerase genes, resulting in amino acid substitutions, alter the target protein structure and subsequently the fluoroquinolone binding affinity of the enzyme, leading to quinolone resistance [8]. In E. coli and in some other Gram-negative bacteria, such as Citrobacter freundii, Shigella spp., Neisseria gonorrhoeae, and Acinetobacter baumannii, mutations in gyrA appear most frequently at codon Ser83 and mutations at codon Asp87 are the second most commonly observed [23–25]. These two amino acids (Ser83 and Asp87) likely play a crucial role in mediating quinolone–enzyme interactions. Indeed, a recent study explained that the interaction between quinolones and topoisomerases was due to the formation of a water–metal ion bridge between the oxygen molecules in the amine group of the drug and the hydroxyl residues in conserved serine or acidic residues in the enzyme, mediated by Mg2+ ion. Thus, a mutation in the place of serine or nearby another amino residue decreases the affinity of the enzyme for quinolones at the noncatalytic Mg2+ site [26].
Different amino acid substitutions at the same position result in different quinolone susceptibility levels. Furthermore, the presence of a single mutation in the QRDR of gyrA usually results in high-level resistance to nalidixic acid only (the MIC of nalidixic acid is greater than 64 mg/L), but to obtain high levels of resistance to fluoroquinolones (ciprofloxacin MICs ranging from 16 to >256 mg/L), the presence of additional mutation(s) in gyrA and/or in another target such as parC is required (Table 2) [15, 27]. Mutations in specific domains of GyrB and ParE have also been shown to cause quinolone resistance, although they are substantially less common in resistant clinical bacterial isolates than mutations in GyrA or ParC [34, 35].
Reduction in cytoplasmic drug concentrations
As the target of fluoroquinolones is intracellular, these molecules must have the ability to enter the bacterial cell. Quinolones may cross the outer membrane in two different ways: through specific porins (e.g., ciprofloxacin) or by diffusion through the phospholipid bilayer (e.g., nalidixic acid). The rate of diffusion of a quinolone is largely associated with its level of hydrophobicity [36].
Gram-negative bacteria can regulate membrane permeability by altering expression of outer membrane porin proteins that form channels for passive diffusion, such as outer membrane proteins OmpF and OmpC in E. coli. Downregulation of these channels or mutations in their structural genes can lead to reductions in cytoplasmic drug concentrations that may contribute as a resistance mechanism [36].
Another chromosome-encoded resistance mechanism leading to decreased intracellular drug accumulation of quinolones is the upregulation of native efflux pumps. These efflux systems are largely responsible for the intrinsic susceptibility of many species to fluoroquinolones and other drugs, but are also responsible for increased MICs resulting from derepression of the transporter [37]. Acquired quinolone resistance can occur by mutations in genes encoding regulatory proteins that control the transcription of efflux pump or porin genes. Less often, mutations in efflux pump structural genes have been associated with changes in pump substrate profiles that include quinolones [37, 38].
Several Enterobacteriaceae species possess a chromosomal native AcrAB-TolC efflux pump belonging to the resistance–nodulation–division (RND) family. AcrA is a membrane fusion protein, AcrB is an inner-membrane pump, and TolC is an outer-membrane protein and they build up an efflux pump [39]. Mutations in acrR (a repressor of acrAB) increase pump activity. On the other hand, mutations that inactivate marR (a repressor of marA) allow MarA to activate acrAB, tolC, and a gene that decreases the translation of ompF, thus collectively decreasing the influx and increasing the efflux of quinolones [40]. A recent study suggested that marA expression is a sensitive marker for early detection of development of levofloxacin resistance [41]. In addition to the Mar regulon, the operon SoxRS regulates the levels of expression of OmpF and some efflux pumps in E. coli [42].
A decrease in the level of expression of OmpF is related to an increase in the resistance to some quinolones, such as norfloxacin and ciprofloxacin, and a variety of other antibacterial agents [43, 44], but does not affect the MICs of other quinolones, such as tosufloxacin or sparfloxacin [45]. Despite the fact that both reduced quinolone uptake and the overexpression of efflux pumps lead to low-level quinolone resistance (change in ciprofloxacin MIC of 4- to 8-fold; Table 2), they can have an additive effect, with QRDR mutations contributing to higher-level quinolone resistance. Moreover, they provide a favorable environment for other types of resistance to antibacterial agents [29, 30].
Plasmid-mediated resistance mechanisms
Target protection: qnr proteins
Plasmid-mediated resistance to quinolones was first reported in 1998 by Martínez-Martínez et al. in a K. pneumoniae clinical strain that was isolated in July 1994 from the urine of a patient at the University of Alabama at Birmingham Medical Center (UAB) [46]. The gene responsible was termed qnr (later named qnrA1). This gene was mediated by plasmid pMG252, which could transfer low-level resistance to nalidixic acid, but susceptibility to fluoroquinolones to a variety of Gram-negative recipients (Citrobacter, Salmonella, and even P. aeruginosa) [46].
The PMQR protein QnrA binding to gyrase or topoisomerase IV inhibits the gyrase–DNA interaction, and could account at least in part for the protection against quinolones by minimizing opportunities for these agents to stabilize the lethal gyrase–DNA–quinolone complex [47]. This QnrA1 is a 218-amino-acid protein that belongs to the pentapeptide repeat family, of which more than 500 members are known, distributed in prokaryotic and eukaryotic cells [48]. These proteins are made of tandemly repeated amino acid sequences with a consensus sequence [Ser, Thr, Arg, or Val] [Asp or Asn] [Leu or Phe] [Ser, Thr, or Arg] [Gly] [48].
The pentapeptide repeat proteins also include immunity proteins such as McbG, which, together with McbE and McbF, protects a microcin B17-producing strain from self-inhibition [49]. Microcins are a class of small inhibitory proteins (less than 10 kDa) that are encoded by bacterial plasmids and differ in their mechanisms of action. Microcin B17, like quinolones, targets DNA gyrase, and McbEFG has been reported to produce low-level resistance to quinolones such as sparfloxacin [50]. The second Qnr relative is MfpA, a protein cloned from the genome of Mycobacterium smegmatis, that has a 4-fold effect on susceptibility to ciprofloxacin. Qnr, McbG, and MfpA have < 20% amino acid identity and, thus, are not closely related, but their existence suggests that Qnr could have evolved from an immunity protein designed to protect DNA gyrase and DNA topoisomerase IV from some naturally occurring inhibitor [3].
The description of the qnrA gene was subsequently followed by the discovery of plasmid-mediated qnrS in Shigella flexneri 2b [51], qnrB in K. pneumoniae [52], qnrC in Proteus mirabilis [53], and qnrD in Salmonella enterica [54]. The qnrVC (from Vibrio cholerae) has been found on plasmids in Aeromonas punctata [55] and Vibrio fluvialis [56]. It is an atypical member of the Qnr family [57] that differs from the plasmid-mediated qnr genes because of the presence of the attC site, which is characteristic of integron cassettes [58]. These qnr genes generally differ in sequence by 35% or more from qnrA and from each other. Furthermore, most of them contain allelic variants differing by 10% or less (qnrA: 8, qnrS: 9, qnrB: 88, qnrC: 1, qnrD: 2, and qnrVC: 7) in which qnrB constitutes the most heterogeneous cluster of the qnr gene family (http://www.lahey.org/qnrstudies/).
The origin of the plasmid-mediated qnr genes has been found on the chromosome of many species, especially in aquatic bacteria, including species of Aeromonas, Photobacterium, Shewanella, and Vibrio [4]. The progenitor of three QnrA-like determinants (termed QnrA3, QnrA4, and QnrA5) was identified as being the chromosome of the environmental bacterium Shewanella algae [59]. Vibrio splendidus could be the source of QnrS1-like determinants as chromosomal-encoded Qnr-like proteins shared about 84 and 88% amino acid identity with the plasmid-mediated determinants QnrS1 and QnrS2 respectively [60]. On the other hand, the source of qnrB determinants was supposed to be Citrobacter spp. including Citrobacter braakii, Citrobacter werkmanii, and Citrobacter youngae [61]. QnrC is 72% identical to chromosomal Qnr in V. orientalis or V. cholerae [53]. However, qnrD can be found in other Enterobacteriaceae, but are especially likely to be found in Proteeae, such as Proteus, Providencia, and Morganella and may have originated there [62]. Vibrionaceae are the source of qnrVC genes, the qnrVC1 attC site has 89% identity with V. parahaemolyticus repeats, and the qnrVC2 putative attC site has 96% identity with a V. cholerae repeat sequence [57].
Some qnr variants are regulated by the SOS system. The SOS response is triggered by DNA damage, such as that generated by quinolones [63]. The RecA protein is activated by single-stranded DNA and acts as a coprotease to cleave the LexA protein, which otherwise binds as a dimer to LexA boxes, repressing the expression of adjacent genes. Most of these genes are involved in DNA repair or the regulation of cell division [64]. The LexA binding site has been identified in the promoter region of all qnrB alleles [65]. This LexA box is also present in qnrD and Smaqnr (pentapeptide repeat protein reported from the chromosome of Serratia marcescens), but not in the other qnr variants [66]. SOS regulation could serve to protect the host cell from the potentially toxic effects of QnrB, while allowing augmented production upon exposure to quinolone antimicrobial agents [65]. In the uninduced state, the LexA protein is bound to its site at the promoter region of qnrB. Thus, the qnrB gene is expressed at a basal level [67]. On induction of the SOS response, by ciprofloxacin for example, single-stranded DNA (ssDNA) is produced and the co-protease activity of the RecA protein is activated by binding to ssDNA [68]. The interaction between LexA and the nucleoprotein filament RecA/ssDNA results in autoproteolytic cleavage of LexA and subsequently in qnrB derepression [67]. Induced expression of qnrB leads to an increase in the MIC of ciprofloxacin (up to 9-fold). However, a qnrB-containing strain does not express quinolone resistance in non-inducing conditions (silent resistance gene); this resistance will be activated only under selective antibiotic pressure [65, 67]. Moreover, it was shown that the direct SOS-dependent regulation of a low-level fluoroquinolone resistance mechanism could be in response to other antimicrobials such as β-lactams and trimethoprim [66].
Enzymatic inactivation: aminoglycoside acetyl transferase AAC(6 ′)-Ib-cr
The aminoglycoside acetyltransferase AAC(6′)-Ib is usually responsible for resistance to tobramycin, amikacin, and kanamycin [69]. Two codon changes, namely Trp102Arg and Asp179Tyr, are found in the variant AAC(6′)-Ib-cr (ciprofloxacin resistance phenotype), which are required to confer reduced susceptibility to certain fluoroquinolones compared with the wild-type AAC(6′)-Ib [31]. The function of the enzyme is to N-acetylate ciprofloxacin at the amino nitrogen on its piperazinyl substituent [70]. Norfloxacin also has free amino nitrogen acting as a substrate of the enzyme, whereas other fluoroquinolones lacking an unsubstituted piperazinyl nitrogen, such as levofloxacin and moxifloxacin, are unaffected [70]. The effectiveness of this enzyme is modest, leading to an increase in the MICs of ciprofloxacin and norfloxacin 3-fold to 4-fold within the range of low-level resistance (Table 2) [31].
Plasmid-mediated efflux pumps
QepA determinant
The qepA gene was first discovered in two E. coli clinical isolates from Japan and Belgium in 2007 [32, 71]. This gene encodes a 511-amino-acid deduced protein (53 kDa) that shares significant identity with various 14-transmembrane-segment (14-TMS) putative efflux pump belonging to the major facilitator superfamily (MFS) of proton-dependent transporters [32, 71]. The natural reservoir of qepA remains unknown. However, it may consist of Actinomycetales species as QepA had significant amino acid identity with likely membrane transporters of the members of the order of Actinomycetales (such as Streptomyces globisporus, Streptomyces coelicolor, Nocardia farcinica, or Polaromonas spp.), and its high GC% content (72%) is compatible with this origin [5].
This protein confers significantly decreased susceptibility to the hydrophilic quinolones (e.g., norfloxacin, ciprofloxacin, and enrofloxacin) with an 8- to 32-fold increase in MICs compared with a wild-type susceptibility profile (Table 2) [32]. Since its initial discovery, a variant of qepA possessing two amino acid substitutions has been identified and named QepA2 [72]. Wang et al. recently identified a new qepA allele, qepA3, in Enterobacteriaceae isolates from China [73].
OqxAB determinant
The OqxAB belongs to the RND family, being one of the first plasmid-borne efflux pumps described in 2004 in E. coli porcine isolates in Denmark and Sweden, on a conjugative plasmid designated pOLA52 [74, 75]. To our knowledge, this is the first identified genetic resistance mechanism towards olaquindox, an agent used as a growth enhancer in pigs. Moreover, it was shown to mediate resistance to other molecules, such as chloramphenicol, trimethoprim, nalidixic acid, norfloxacin, and ciprofloxacin [33].
The oqxA gene codes for the OqxA membrane fusion protein whereas the oqxB codes for the OqxB protein, containing 12-transmembrane α-helices for the inner-membrane pump. This system requires the TolC outer-membrane protein to function fully [74].
The OqxAB pump is common (usually 75% or more) on the chromosome of K. pneumoniae isolates [76] and it is also prevalent among other species such as Enterobacter spp. [77]. It has been reported that the oqxAB operon, together with a transcriptional regulator (orf68) in the chromosome of K. pneumoniae, was captured by IS26 transposase and transferred to foreign plasmids, which were subsequently disseminated to other bacterial species that do not harbor oqxAB-like elements in the chromosome [77].
As for other PMQR, OqxAB alone confers low-level resistance to fluoroquinolones (Table 2). In K. pneumoniae, overexpression of the nearby rarA gene is associated with increased oqxAB expression, whereas increased expression of the adjacent oqxR gene downregulates OqxAB production [78]. The overexpression of this efflux pump, resulting from a point mutation in the repressor oqxR gene, is responsible for the multidrug resistance phenotype and also for the increased virulence potential in some cases [79].
Impact of PMQR on the clinical resistance level and mutant development
The PMQR genes cause only a modest decrease in ciprofloxacin susceptibility (Table 2). However, it has been shown that PMQR plays an important role in the acquisition of clinical resistance leading to the selection of high-level quinolone resistance [27]. These data indicate that these low-level quinolone-resistant phenotypes may be critical stages (depending on the genotype) in resistance development, including chromosome- and plasmid-mediated mechanisms, at which some low-fitness mutants below the resistance breakpoint are able to evolve clinical resistance with just one or two mutations, and show increased fitness [27].
The clinical importance and the selection of qnr-positive cells to high-level fluoroquinolone resistance can be demonstrated by the mutant preventive concentration (MPC), which is the lowest concentration at which no mutants are observed. It represents the MIC of the least-susceptible single-step mutant [80]. The MPC is measured after plating a large inoculum (1010 bacteria) on concentrations of a quinolone that are above its MIC. Resistant mutants are selectively enriched only in the concentration range between the MIC and the MPC, which is designated as the mutant selection window. Below the MIC, no mutant will be enriched because selective pressure is absent; above MPC, no mutant will be selected because a double mutation is required for growth [81]. Thus, the best schedule for quinolone administration is one that maintains a quinolone concentration that exceeds the MPC for as much of the dosage interval as possible, thereby minimizing the opportunity for mutant selection [3].
Rodríguez-Martínez et al. showed that the expression of qnrA considerably increased the MPC compared with strains without this gene. In the presence of qnrA, mutations in gyrA and parC genes were easily selected to produce high levels of quinolone resistance [82]. Another study reported that the qepA2 gene also increases the MPCs for ciprofloxacin 4- to 16-fold [83].
Experimental animal models have been used to evaluate the in vivo importance of PMQR genes. Indeed, it has been shown that low-level fluoroquinolone resistance conferred by aac(6′)Ib-cr is associated with the reduced bactericidal activity of ciprofloxacin in vivo and to lead to ciprofloxacin therapeutic failure in pyelonephritis. The reduction in bactericidal activity could be explained by in situ N-acetylation of ciprofloxacin [84]. A further work described the significant role of the aac(6′)-Ib-cr gene in the acquisition of a clinical level of ciprofloxacin and norfloxacin resistance, when combined with three or four chromosomal mutations, both in vitro and in vivo [85].
In addition, several studies used the mouse model of pyelonephritis for in vivo experiments to study the interplay in fluoroquinolone resistance mutations and bacterial fitness. Michon et al. [86] investigated host fitness of E. coli isogenic strains after acquisition of the qnrA3 gene, inserted either alone onto a small plasmid or harbored on a large conjugative native plasmid found in a clinical isolate. Indeed, it was shown that qnrA3 acquisition enhanced bacterial fitness, which may explain qnr emergence and suggests the regulatory role of qnr. However, fitness was reduced when qnrA3 was inserted onto multidrug-resistant plasmids and this can slow down its dissemination without antibiotic exposure. Another study based on in vitro and in vivo models reported that most of the combination of target mutations and qnrA1 had a significant fitness cost, whereas most of the combinations harboring qnrS1 had significantly enhanced bacterial fitness. These positive relationships could represent an additional driving force in the development of increased resistance to quinolones [27].
On the other hand, a recent study reported that in E. coli J53 carrying qnrA and aac(6′)Ib-cr or qepA, gyrA mutations are rare, whereas alterations in pumps, porins, and lipopolysaccharides are more common. Mutations upregulating drug efflux (mutations in regulatory genes marR or soxR) may have a fitness cost, but are relevant to resistance evolution because of their pleiotropic effects on susceptibility to other agents and potential for occurrence at a rate higher than that required for specific changes in the QRDR of gyrA [87].
Antibiotic markers, plasmids, and mobilizing elements associated with PMQR genes
Determinants of PMQR have been strongly associated with extended spectrum beta-lactamases (ESBLs) and AmpC ß-lactamases, as shown in Table 3. They have been described in multiresistant clones with worldwide distribution, such as E. coli ST131 and K. pneumoniae ST11 [119, 120]. Moreover, the PMQR genes have often been transferred on multiresistant conjugative plasmids varying in size, which facilitated their global emergence involving several plasmids with different incompatibility groups [4].
The PMQR qnrA1, qnrA3, qnrA6, qnrB2, qnrB4, qnrB6, and qnrB10 have usually been associated with the mobilizing element insertion sequence common region (ISCR), whereas qnrB1 and qnrB20 have been linked to IS26 and Orf1005 [4]. The qnrB19 allele has been found in a transposon comprising ISEcp1 [121]. The qnrS1 has been associated with an upstream Tn3-like transposon or upstream of the insertion sequence ISEcl2 [122], in several plasmids containing an active TEM-1 gene [4]. Nevertheless, most plasmids carrying qnrS genes are relatively smaller than plasmids carrying qnrA and qnrB and are rarely associated with other antibiotic markers [58]. The qnrC gene has been found to be linked to ISPmi1 [4], whereas the qnrD gene has been found in small nontransmissible plasmids (2.6 to 4 kb) in Proteeae and located inside mobile insertion cassette (mic) elements [62].
The aac(6′)-Ib-cr gene is usually found in a cassette as part of an integron with IS26 in a multiresistance plasmid, which may contain other PMQR genes such as qnrB and also bla CTX-M-15 gene [58]. Moreover, the aac(6′)-Ib-cr gene can also be inserted in the chromosome [123].
The qepA1 determinant has also often been found on plasmids encoding aminoglycoside ribosomal methylase rmtB. IS26 elements and ISCR3C have been implicated in mobilizing the qepA1 gene to plasmids [124], whereas the qepA2 gene was not associated with the rmtB gene and IS26 elements, but was identified to be flanked by two copies of an ISCR-like element [72]. A novel genetic structure surrounding the qepA3 gene has been described. In some strains, qepA3 was linked to the non-rmtB- or non-ISCR3C-producing and was associated with bla CTX-M-14 or bla TEM-12 [73].
Besides being commonly intrinsic in Klebsiella spp. and Enterobacter spp., the OqxAB-encoding genes are often located on conjugative plasmids, within a composite transposon Tn6010 flanked by IS26 [75].
Epidemiology of PMQR determinants: Mediterranean countries
The PMQR determinants emerged in various Enterobacteriaceae species, especially E. coli, Enterobacter spp., Klebsiella spp., and Salmonella spp. [4] and are less common in other Gram-negative bacteria such as Aeromonas spp. [125] A. baumannii [126] and P. aeruginosa [127].
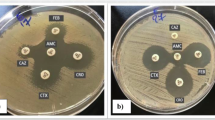
Currently, these determinants have been increasingly reported in Enterobacteriaceae worldwide, including several Mediterranean countries. Although many reports about PMQR determinants have been published in Spain, Tunisia, Italy, France, Algeria, Egypt, and Turkey, there are no published data yet from Libya, Syria, Lebanon, Albania, Bosnia and Herzegovina, Montenegro, and Malta. The geographic distribution of PMQR determinants in the Mediterranean basin is presented in Fig. 2.
The PMQR genes have been found in different sources, including humans (clinical [96, 111, 117, 128, 129] and community isolates [91, 95, 105, 130]), animals (companion animals [103, 131–133] and food-producing animals [90, 94, 134]), and the environment (waste water treatment plant [135] and hospital effluents [91, 136]).
The prevalence of PMQR genes varies by both organism and geographic region and depending on the selection criteria of the strains studied (ESBL-producing, nalidixic acid, fluoroquinolones, etc.) [5]. However, the most commonly reported PMQRs remain the aac(6′)Ib-cr gene followed by the qnr gene. Thus, the aac(6′)-Ib-cr gene had the highest prevalence at 22%, whereas qnr genes were present in 1.3% among a collection of uropathogenic E. coli isolated in a Tunisian university hospital [129]. In contrast, qnr-related genes (qnrA, qnrB, qnrS) and the aac(6′)-Ib-cr gene were identified in 14.3 and 3.6% respectively in Enterobacter cloacae and Klebsiella spp. isolates recovered from cases of clinical and sub-clinical mastitis in Egypt [137]. In many cases, qnrB genes seem to be more prevalent overall than other qnr genes. In Italy, the prevalence rates of qnrA, qnrB, and qnrS were 1.4, 4.3, and 1.4% respectively in Klebsiella spp. isolates from companion animals [103].
An outbreak of K. pneumoniae carrying qnrB1, aac(6′)Ib-cr, and bla CTX-M-15 was reported in a French intensive care unit between 2008 and 2009 [128].
In Spain, the first report of clustered infections caused by a non-ESBL-producing K. pneumoniae strain harboring bla OXA-1 and aac(6’)Ib-cr and belonging to ST14 was identified. The clonal isolates were detected from May 2007 until December 2009 from clinical samples of 38 patients admitted to the University Hospital of Bellvitge, Barcelona, Spain [138]. Dissemination of qnr and aac(6’)Ib-cr genes in E. coli is closely associated with the worldwide spread of a single clone, ST131, which is the main cause of clinic- and community-acquired urinary tract infections [139], as described in community E. coli strains harboring aac(6′)Ib-cr and bla CTX-M-15 isolated in Algeria in 2011 and 2014 [91]. Recent reports have highlighted the Mediterranean Sea as being a potential reservoir of various antibiotic markers, notably PMQR determinants. Indeed, qnr (qnrA, qnrB, and qnrS) and aac(6′)-Ib-cr genes, were identified in 16 (5.8%) and 3 (1.1%) isolates respectively in Gram-negative bacteria isolated from water samples taken from fish farms in the northern part of Egypt at the Mediterranean Sea [94]. Moreover, both aac(6′)Ib-cr and qnrB genes have been identified in CTX-M-15-producing E. coli strains belonging to the pandemic clone ST 131 recovered from wild fish in the Mediterranean Sea far from Bejaia (Algeria) [140].
QepA efflux pump is usually identified with a low prevalence. France was the first Mediterranean country to report the QepA determinant (QepA2 variant) in 2008 in one (0.8%) E. coli ESBL-producing isolate [72]. In Spain, only one isolate (2.4%) showed the presence of qepA among a collection of Salmonella enterica clinical isolates [141]. Very recently, QepA1 was identified in two E. coli clinical strains isolated in 2011 in Algeria (Yanat et al., unpublished data). This determinant was also described in nalidixic acid-resistant Salmonella isolates recovered from various food-animal products in Tunisia, with a rate of 1.16% associated with the qnr gene [142].
The identification of OqxAB plasmidic efflux pump is rare in the Mediterranean basin. This determinant is more frequent in China, mainly from animal isolates [143]. Nevertheless, oqxAB genes were detected in E. coli isolates from animals in Italy with a rate of 15% associated with ST 238 [131] and in K. pneumoniae and E. coli clinical isolates from Spain and Turkey respectively [76, 144].
Conclusion
In parallel to a high consumption of quinolones, different mechanisms of quinolone resistance were developed in Gram-negative bacteria. PMQR emerged in Enterobacteriaceae isolates with a high prevalence in Mediterranean countries, probably because of the great diversity of the population and the exchange relationship between the regions. As the presence of these determinants is often difficult to detect based on the phenotype observed on a routine basis in the laboratory, the real prevalence of PMQR-positive bacteria could be higher than recorded in the published reports. Therefore, long-term surveillance is needed for the future monitoring of trends in the occurrence of PMQR genes in different regions and in various settings. Also, future studies are required focusing on plasmid analysis to understand more about the successful dissemination of PMQR genes.
References
Lesher GY, Froelich EJ, Gruett MD, Bailey JH, Brundage RP (1962) 1,8-naphthyridine derivatives. a new class of chemotherapeutic agents. J Med Chem 5:1063–1065
Naeem A, Badshah SL, Muska M, Ahmad N, Khan K (2016) The current case of quinolones: synthetic approaches and antibacterial activity. Molecules 21:268
Jacoby GA (2005) Mechanisms of resistance to quinolones. Clin Infect Dis 41:120–126
Jacoby GA, Strahilevitz J, Hooper DC (2014) Plasmid-mediated quinolone resistance. Microbiol Spectr DOI:10.1128/microbiolspec.PLAS-0006-2013
Poirel L, Cattoir V, Nordmann P (2012) Plasmid mediated quinolone resistance; interactions between human, animal, and environmental ecologies. Front Microbiol 3(24):1–7
Oliphant CM, Green GM (2002) Quinolones: a comprehensive review. Am Fam Physician 65:455–464
Paton JH, Reeves DS (1988) Fluoroquinolone antibiotics. Microbiology, pharmacokinetics and clinical use. Drugs 36:193–228
Redgrave LS, Sutton SB, Webber MA, Piddock LJV (2014) Fluoroquinolone resistance: mechanisms, impact on bacteria, and role in evolutionary success. Trends Microbiol 22(8):438–445
Álvarez-Hernández DA, Garza-Mayén GS, Vázquez-López R (2015) Quinolonas. Perspectivas actuales y mecanismos de resistencia. Rev Chilena Infectol 32(5):499–504
Mohammadhosseini N, Pordeli M, Safavi M, Firoozpour L, Amin F, Kabudanian Ardestani S, Edraki N, Shafiee A, Foroumadi A (2015) Novel N-2-(furyl)-2-(chlorobenzyloxyimino) ethyl piperazinyl quinolones: synthesis, cytotoxic evaluation and structure-activity relationship. Iran J Pharm Res 14(4):1095–1103
Cross RM, Flanigan DL, Monastyrskyi A, LaCrue AN, Saenz FE, Maignan JR et al (2014) Orally bioavailable 6-chloro-7-methoxy-4(1H)-quinolones efficacious against multiple stages of plasmodium. J Med Chem 57:8860–8879
Boothe D, Boeckh A, Simpson B, Dubose K (2006) Comparison of pharmacodynamics and pharmacokinetic indices of efficacy for 5 fluoroquinolones toward pathogens of dogs and cats. J Vet Inter Med 20:1297–1306
Hawkey PM (2003) Mechanisms of quinolone action and microbial response. J Antimicrob Chemother 51(1):29–35
Kohanski MA, Dwyer DJ, Collins JJ (2010) How antibiotics kill bacteria: from targets to networks. Nat Rev Microbiol 8(6):423–435
Ruiz J (2003) Mechanisms of resistance to quinolones: target alterations, decreased accumulation and DNA gyrase protection. J Antimicrob Chemother 51:1109–1117
Belenky P, Ye JD, Porter CBM, Cohen NR, Lobritz MA, Ferrantee T et al (2015) Bactericidal antibiotics induce toxic metabolic perturbations that lead to cellular damage. Cell Rep 13(5):968–980
Kottur J, Nair DT (2016) Reactive oxygen species play an important role in the bactericidal activity of quinolone antibiotics. Angew Chem Int Ed Engl 55(7):2397–2400
Piddock LJ, Walters RN (1992) Bactericidal activities of five quinolones for Escherichia coli strains with mutations in genes encoding the SOS response or cell division. Antimicrob Agents Chemother 36:819–825
Yoshida H, Bogaki M, Nakamura M, Nakamura S (1990) Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob Agents Chemother 34:1271–1272
Barnard FM, Maxwell A (2001) Interaction between DNA gyrase and quinolones: effects of alanine mutations at gyrA subunit residues Ser83 and Asp87. Antimicrob Agents Chemother 45:1994–2000
Wohlkonig A, Chan PF, Fosberry AP, Homes P, Huang J, Kranz M et al (2010) Structural basis of quinolone inhibition of type IIA topoisomerases and target-mediated resistance. Nat Struct Mol Biol 17:1152–1153
Laponogov I, Veselkov DA, Crevel IM, Pan XS, Fisher LM, Sanderson MR (2013) Structure of an ‘open’ clamp type II topoisomerase-DNA complex provides a mechanism for DNA capture and transport. Nucl Acids Res 41:9911–9923
Everett MJ, Jin YF, Ricci V, Piddock LJV (1996) Contribution of individual mechanisms to fluoroquinolone resistance in 36 Escherichia coli strains isolated from humans and animals. Antimicrob Agents Chemother 40:2380–2386
Tavio MM, Vila J, Ruiz J, Martin-Sanchez AM, Jiménez de Anta MT (1999) Mechanisms involved in the development of resistance to fluoroquinolones in Escherichia coli strains. J Antimicrob Chemother 44:735–742
Ruiz J, Gómez J, Navia MM, Ribera A, Sierra JM, Marco F et al (2002) High prevalence of nalidixic acid resistant, ciprofloxacin susceptible phenotype among clinical isolates of Escherichia coli and other Enterobacteriaceae. Diagn Microbiol Infect Dis 42(4):257–261
Aldred KJ, Schwanz HA, Li G, Williamson BH, McPherson SA, Turnbough CL Jr et al (2015) Activity of quinolone cp-115,955 against bacterial and human type II topoisomerases is mediated by different interactions. Biochemistry 54:1278–1286
Machuca J, Briales A, Labrador G, Díaz-de-Alba P, López-Rojas R, Docobo-Pérez F et al (2014) Interplay between plasmid-mediated and chromosomal-mediated fluoroquinolone resistance and bacterial fitness in Escherichia coli. J Antimicrob Chemother 69(12):3203–3215
Piddock LJ (1999) Mechanisms of fluoroquinolone resistance: an update 1994-1998. Drugs 58(2):11–18
Hirai K, Aoyama H, Suzue S, Irikura T, Iyobe S, Mitsuhashi S (1986) Isolation and characterization of norfloxacin resistant mutants of Escherichia coli K-12. Antimicrob Agents Chemother 30:248–253
Komp Lindgren P, Marcusson LL, Sandvang D, Frimodt-Møller N, Hughes D (2005) Biological cost of single and multiple norfloxacin resistance mutations in Escherichia coli implicated in urinary tract infections. Antimicrob Agents Chemother 49:2343–2351
Robicsek A, Strahilevitz J, Jacoby GA, Macielag M, Abbanat D, Park CH et al (2006) Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nat Med 12:83–88
Yamane K, Wachino J, Suzuki S, Kimura K, Shibata N, Kato (2007) New plasmid-mediated fluoroquinolone efflux pump, QepA, found in an Escherichia coli clinical isolate. Antimicrob Agents Chemother 51(9):3354–3360
Hansen LH, Jensen LB, Sørensen HI, Sørensen SJ (2007) Substrate specificity of the OqxAB multidrug resistance pump in Escherichia coli and selected enteric bacteria. J Antimicrob Chemother 60:145–147
Yoshida H, Bogaki M, Nakamura M, Yamanaka LM, Nakamura S (1991) Quinolone resistance-determining region in the DNA gyrase gyrB gene of Escherichia coli. Antimicrob Agents Chemother 35:1647–1650
Breines DM, Ouabdesselam S, Ng EY, Tankovic J, Shah S, Soussy CJ, Hooper DC (1997) Quinolone resistance locus nfxD of Escherichia coli is a mutant allele of parE gene encoding a subunit of topoisomerase IV. Antimicrob Agents Chemother 41:175–179
Chapman JS, Georgopapadokou NH (1988) Routes of quinolone permeation in Escherichia coli. Antimicrob Agents Chemother 32:438–442
Kang HW, Woo GJ (2014) Increase of multidrug efflux pump expression in fluoroquinolone-resistant Salmonella mutants induced by ciprofloxacin selective pressure. Res Vet Sci 97(2):182–186
Grkovic S, Brown MH, Skurray RA (2002) Regulation of bacterial drug export systems. Microbiol Mol Biol Rev 66:671–701
Poole K (2005) Efflux-mediated antimicrobial resistance. J Antimicrob Chemother 56:20–51
Alekshun MN, Levy SB (1997) Regulation of chromosomally mediated multiple antibiotic resistance: the mar regulon. Antimicrob Agents Chemother 41:2067–2075
Yamasaki E, Yamada C, Jin X, Nair GB, Kurazono H, Yamamoto S (2015) Expression of marA is remarkably increased from the early stage of development of fluoroquinolone-resistance in uropathogenic Escherichia coli. J Infect Chemother 21(2):105–109
Chou JH, Greenberg JT, Demple B (1998) Postranscriptional repression of Escherichia coli OmpF protein in response to redox stress: positive control of the micF antisense RNA by the soxRS locus. J Bacteriol 175:1026–1031
Aoyama H, Sato K, Kato T, Hirai K, Mitsuhashi S (1987) Norfloxacin resistance in a clinical isolate of Escherichia coli. Antimicrob Agent Chemother 31:1640–1641
Cohen SP, McMurry LM, Hooper DC, Wolfson JS, Levy SB (1989) Cross-resistance to fluoroquinolone in multiple-antibiotic-resistance (Mar) Escherichia coli selected by tetracycline or chloramphenicol: decreased drug accumulation associated with membrane changes in addition to OmpF reduction. Antimicrob Agents Chemother 33:1318–1325
Mitsuyama J, Itoh Y, Takahata M, Okamoto S, Yasuda T (1992) In vitro antibacterial activities of tosufloxacin against and uptake of tosufloxacin by outer membrane mutants of Escherichia coli, Proteus mirabilis and Salmonella typhimurium. Antimicrob Agents Chemother 36:2030–2036
Martínez-Martínez L, Pascual A, Jacoby GA (1998) Quinolone resistance from a transferable plasmid. Lancet 351:797–799
Tran JH, Jacoby GA, Hooper DC (2005) Interaction of the plasmid-encoded quinolone resistance protein QnrA with Escherichia coli topoisomerase IV. Antimicrob Agents Chemother 49(7):3050–3052
Vetting MW, Hedge SS, Fajardo JE, Fiser A, Roderick SL, Takiff HE et al (2006) Pentapeptide repeat proteins. Biochemistry 45:1–10
Garrido MC, Herrero M, Kolter R, Moreno F (1988) The export of the DNA replication inhibitor microcin B17 provides immunity for the host cell. EMBO J 7(6):1853–1862
Tran JH, Jacoby GA (2002) Mechanism of plasmid-mediated quinolone resistance. Proc Natl Acad Sci 99:5638–5642
Hata M, Suzuki M, Matsumoto M, Takahashi M, Sato K, Ibe S et al (2005) Cloning of a novel gene for quinolone resistance from a transferable plasmid in Shigella flexneri 2b. Antimicrob Agents Chemother 49:801–803
Jacoby GA, Walsh KE, Mills DM, Walker VJ, Oh H, Robicsek A et al (2006) qnrB, another plasmid-mediated gene for quinolone resistance. Antimicrob Agents Chemother 50(4):1178–1182
Wang M, Guo Q, Xu X, Wang X, Ye X, Wu S et al (2009) New plasmid-mediated quinolone resistance gene, qnrC, found in a clinical isolate of Proteus mirabilis. Antimicrob Agents Chemother 53:1892–1897
Cavaco LM, Hasman H, Xia S, Aarestrup FM (2009) qnrD, a novel gene conferring transferable quinolone resistance in Salmonella enterica serovar Kentucky and Bovismorbificans strains of human origin. Antimicrob Agents Chemother 53:603–608
Xia R, Guo X, Zhang Y, Xu H (2010) qnrVC-like gene located in a novel complex class 1 integron harboring the ISCR1 element in an Aeromonas punctata strain from an aquatic environment in Shandong Province, China. Antimicrob Agents Chemother 54:3471–3474
Singh R, Rajpara N, Tak J, Patel A, Mohanty P, Vinothkumar K et al (2012) Clinical isolates of Vibrio fluvialis from Kolkata, India, obtained during 2006: plasmids, the qnr gene and a mutation in gyrase A as mechanisms of multidrug resistance. J Med Microbiol 61:369–374
Fonseca EL, Dos Santos Freitas F, Vieira VV, Vicente AC (2008) New qnr gene cassettes associated with superintegron repeats in Vibrio cholerae O1. Emerg Infect Dis 14:1129–1131
Rodriguez-Martinez JM, Cano ME, Velasco C, Martínez-Martínez L, Pascual A (2011) Plasmid-mediated quinolone resistance: an update. J Infect Chemother 17:149–182
Poirel L, Rodriguez-Martinez JM, Mammeri H, Liard A, Nordmann P (2005) Origin of plasmid-mediated quinolone resistance determinant QnrA. Antimicrob Agents Chemother 49:3523–3525
Cattoir V, Poirel L, Mazel D, Soussy CJ, Nordmann P (2007) Vibrio splendidus as the source of plasmid-mediated QnrS-like quinolone resistance determinants. Antimicrob Agents Chemother 51:2650–2651
Jacoby GA, Griffin CM, Hooper DC (2011) Citrobacter spp.as a source of qnrB alleles. Antimicrob Agents Chemother 55:4979–4984
Guillard T, Grillon A, De Champs C, Cartier C, Bercot B, Lebreil AL (2014) Mobile insertion cassette elements found in small nontransmissible plasmids in Proteeae may explain qnrD mobilization. PLoS One 9(2):1–8
Malik M, Zhao X, Drlica K (2006) Lethal fragmentation of bacterial chromosomes mediated by DNA gyrase and quinolones. Mol Microbiol 61:810–825
Baharoglu Z, Mazel D (2014) SOS, the formidable strategy of bacteria against aggressions. FEMS Microbiol Rev 38(6):1126–1145
Wang M, Jacoby GA, Mills DM, Hoope DC (2009) SOS regulation of qnrB expression. Antimicrob Agents Chemother 53(2):821–823
Briales A, Rodriguez-Martinez JM, Velasco C, Machuca J, Dìaz de Alba P, Blazquez J et al (2012) Exposure to diverse antimicrobials induces the expression of qnrB1, qnrD and smaqnr genes by SOS-dependent regulation. Antimicrob Chemother 67:2854–2859
Da Re S, Garnier F, Guérin E, Campoy S, Denis F, Ploy MC (2009) The SOS response promotes qnrB quinolone-resistance expression. EMBO Rep 10(8):929–933
Little JW, Edmiston SH, Pacelli LZ, Mount DW (1980) Cleavage of the Escherichia coli lexA protein by the recA protease. Proc Natl Acad Sci U S A 77:3225–3229
Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A (2009) Plasmid-mediated quinolone resistance: a multifaceted threat. Clin Microbiol Rev 22:664–689
Robicsek A, Jacoby GA, Hooper DC (2006) The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis 6:629–640
Perichon B, Courvalin P, Galimand M (2007) Transferable resistance to aminoglycosides by methylation of G1405 in 16S rRNA and to hydrophilic fluoroquinolones by QepA-mediated efflux in Escherichia coli. Antimicrob Agents Chemother 51:2464–2469
Cattoir V, Poirel L, Nordmann P (2008) Plasmid-mediated quinolone resistance pump QepA2 in an Escherichia coli isolate from France. Antimicrob Agents Chemother 52:3801–3804
Wang D, Huang X, Chen J, Mou Y, Li H, Yang L (2015) Characterization of genetic structures of the qepA3 gene in clinical isolates of Enterobacteriaceae. Front Microbiol 6:1147
Hansen LH, Johannesen E, Burmølle M, Sørensen AH, Sørensen SJ (2004) Plasmid-encoded multidrug efflux pump conferring resistance to olaquindox in Escherichia coli. Antimicrob Agents Chemother 48:3332–3337
Norman A, Hansen LH, She Q, Sørensen SJ (2008) Nucleotide sequence of pOLA52: a conjugative IncX1 plasmid from Escherichia coli which enables biofilm formation and multidrug efflux. Plasmid 60:59–74
Rodriguez-Martinez JM, Diaz de Alba P, Briales A, Machuca J, Lossa M, Fernandez-Cuenca F et al (2013) Contribution of OqxAB efflux pumps to quinolone resistance in extended-spectrum-ß-lactamase-producing Klebsiella pneumoniae. Antimicrob Chemother 68:68–73
Wong MH, Chan EW, Chen S (2015) Evolution and dissemination of OqxAB-like efflux pumps, an emerging quinolone resistance determinant among members of Enterobacteriaceae. Antimicrob Agents Chemother 59(6):3290–3297
Veleba M, Higgins PG, Gonzalez G, Seifert H, Schneidersa T (2012) Characterization of RarA, a novel AraC family multidrug resistance regulator in Klebsiella pneumoniae. Antimicrob Agents Chemother 56(8):4450–4458
Bialek-Davenet S, Lavigne JP, Guyot K, Mayer N, Tournebize R, Brisse S et al (2015) Differential contribution of AcrAB and OqxAB efflux pumps to multidrug resistance and virulence in Klebsiella pneumoniae. J Antimicrob Chemother 70(1):81–88
Drlica K (2003) The mutant selection window and antimicrobial resistance. J Antimicrob Chemother 52:11–17
Zhao X, Drlica K (2001) Restricting the selection of antibiotic-resistant mutants: a general strategy derived from fluoroquinolone studies. Clin Infect Dis 33(3):S147–S156
Rodríguez-Martínez JM, Velasco C, García I, Cano ME, Martínez-Martínez L, Pascual A (2007) Mutant prevention concentrations of fluoroquinolones for Enterobacteriaceae expressing the plasmid-carried quinolone resistance determinant qnrA1. Antimicrob Agents Chemother 51(6):2236–2239
Machuca J, Briales A, Díaz-de-Alba P, Martínez-Martínez L, Pascual Á, Rodríguez-Martínez JM (2015) Effect of the efflux pump QepA2 combined with chromosomally mediated mechanisms on quinolone resistance and bacterial fitness in Escherichia coli. J Antimicrob Chemother 70(9):2524–2527
Guillard T, Cambau E, Chau F, Massias L, de Champs C, Fantin B (2013) Ciprofloxacin treatment failure in a murine model of pyelonephritis due to an AAC(6′)-Ib-cr-producing Escherichia coli strain susceptible to ciprofloxacin in vitro. Antimicrob Agent Chemother 57(12):5830–5835
Machuca J, Ortiz M, Recacha E, Díaz-De-Alba P, Docobo-Perez F, Rodríguez-Martínez JM et al (2016) Impact of AAC(6′)-Ib-cr in combination with chromosomal-mediated mechanisms on clinical quinolone resistance in Escherichia coli. J Antimicrob Chemother 71(11):3066–3071
Michon A, Allou N, Chau F, Podglajen I, Fantin B, Cambau E (2011) Plasmidic qnrA3 enhances Escherichia coli fitness in absence of antibiotic exposure. PLoS One 6(9):e24552
Vinué L, Corcoran MA, Hooper DC, Jacoby GA (2016) Mutations that enhance the ciprofloxacin resistance of Escherichia coli with qnrA1. Antimicrob Agents Chemother 60(3):1537–1545
Iabadene H, Messai Y, Ammari H, Ramdani-Bouguessa N, Lounes S, Bakour R et al (2008) Dissemination of ESBL and Qnr determinants in Enterobacter cloacae in Algeria. J Antimicrob Chemother 62:133–136
Meradi L, Djahoudi A, Abdi A, Bouchakour M, Perrier Gros Claude JD, Timinouni M (2011) Qnr and aac(6′)-Ib-cr types quinolone resistance among Enterobacteriaceae isolated in Annaba, Algeria. Pathol Biol 59(4):e73–e78
Agabou A, Lezzar N, Ouchenane Z, Khemissi S, Satta D, Sotto A et al (2015) Clonal relationship between human and avian ciprofloxacin-resistant Escherichia coli isolates in North-Eastern Algeria. Eur J Clin Microbiol Infect Dis 35(2):227–234
Yanat B, Machuca J, Díaz-De-Alba P, Mezhoud H, Touati A, Pascual Á et al (2016) Characterization of plasmid-mediated quinolone resistance determinants in high-level quinolone-resistant Enterobacteriaceae isolates from the community: First report of qnrD gene in Algeria. Microb Drug Resist DOI: 10.1089/mdr.2016.0031
Anssour L, Messai Y, Estepa V, Torres C, Bakour R (2016) Characteristics of ciprofloxacin-resistant Enterobacteriaceae isolates recovered from wastewater of an Algerian hospital. J Infect Dev Ctries 10(7):728–734
Literacka E, Bedenic B, Baraniak A, Fiett J, Tonkic M, Jajic-Bencic I et al (2009) bla CTX-M genes in Escherichia coli strains from Croatian hospitals are Located in new (bla CTX-M-3a) and widely spread (bla CTX-M-3a and bla CTX-M-15 ) genetic structures. Antimicrob Agents Chemother 4(53):1630–1635
Ishida Y, Ahmed AM, Mahfouz NB, Kimura T, El-Khodery SA, Moawad AA et al (2010) Molecular analysis of antimicrobial resistance in Gram-negative bacteria isolated from fish farms in Egypt. J Vet Med Sci 72(6):727–734
Hassan WM, Hashim A, Domany RAA (2012) Plasmid mediated quinolone resistance determinants qnr, aac(6′)-Ib-cr, and qepA in ESBL producing Escherichia coli clinical isolates from Egypt. Indian J Med Microbiol 30(4):442–447
Abd El-Aziz NK, Gharib AA (2015) Coexistence of plasmid-mediated quinolone resistance determinants and AmpC-Beta-Lactamases in Escherichia coli strains in Egypt. Cell Mol Biol 61(5):29–35
Poirel L, Leviandier C, Nordmann P (2006) Prevalence and genetic analysis of plasmid-mediated quinolone resistance determinants QnrA and QnrS in Enterobacteriaceae isolates from a French University Hospital. Antimicrob Agent Chemother 50(12):3992–3997
Cambau E, Lascols C, Sougakoff W, Bebear C, Bonnet R, Cavallo JD et al (2006) Occurrence of qnrA-positive clinical isolates in French teaching hospitals during 2002–2005. Clin Microbiol Infect 12:1013–1020
Guillard T, Cholley P, Limelette A, Hocquet D, Matton L, Guyeux C et al (2015) Fluoroquinolone resistance mechanisms and population structure of Enterobacter cloacae non-susceptible to ertapenem in North-Eastern France. Front Microbiol 6:1186
Mavroidi A, Miriagou V, Liakopoulos A, Tzelepi E, Stefos A, Dalekos GN et al (2012) Ciprofloxacin-resistant Escherichia coli in Central Greece: mechanisms of resistance and molecular identification. BMC Infect Dis 12:371–376
Chmelnitsky I, Hermesh O, Navon-Venezia S, Strahilevitz J, Carmeli Y (2009) Detection of aac(6′)-Ib-cr in KPC-producing Klebsiella pneumoniae isolates from Tel Aviv, Israel. J Antimicrob Chemother 64:718–722
Musumeci R, Rausa M, Giovannoni R, Cialdella A, Bramati S, Sibra B et al (2012) Prevalence of plasmid-mediated quinolone resistance genes in uropathogenic Escherichia coli isolated in a teaching hospital of northern Italy. Microb Drug Resist 18(1):33–41
Donati V, Feltrin F, Hendriksen RS, Aaby Svendsen C, Cordaro G, Garcia-Fernandez A (2014) Extended-spectrum-beta-lactamases, AmpC beta-lactamases and plasmid mediated quinolone resistance in Klebsiella spp. from companion animals in Italy. PloS One 9(3):e90564
Bouchakour M, Zerouali K, Perrier Gros Claude JD, Amarouch H, El Mdaghri N, Courvalin P et al (2010) Plasmid-mediated quinolone resistance in expanded spectrum beta-lactamase producing Enterobacteriaceae in Morocco. J Infect Dev Ctries 4(12):799–803
Barguigua A, Ouair H, El Otmani F, Saile R, El Mdaghri N, El Azhari M et al (2015) Fecal carriage of extended-spectrum β-lactamase-producing Enterobacteriaceae in community setting in Casablanca. Infect Dis 47(1):27–32
Barguigua A, Zerouali K, Katfy K, El Otmani F, Timinouni M, Elmdaghri N (2015) Occurrence of OXA-48 and NDM-1 carbapenemase-producing Klebsiella pneumoniae in a Moroccan university hospital in Casablanca. Morocco Infect Genet Evol 31:142–148
Tayh G, Ben Sallem R, Ben Yahia H, Gharsa H, Klib N, Boudabous A et al (2016) First report of extended-spectrum β-lactamases among clinical isolates of Klebsiella pneumoniae in Gaza strip, Palestine. Microb Drug Resist DOI: 10.1089/mdr.2016.0089
Cano ME, Rodrìguez-Martìnez JM, Aguero J, Pascual A, Calvo J, Garcìa-Lobo JM et al (2009) Detection of plasmid-mediated quinolone resistance genes in clinical isolates of Enterobacter spp. in Spain. J Clin Microbiol 47(7):2033–2039
Briales A, Rodríguez-Martínez JM, Velasco C, de Alba PD, Rodríguez-Baño J, Martínez-Martínez L et al (2012) Prevalence of plasmid-mediated quinolone resistance determinants qnr and aac(6′)-Ib-cr in Escherichia coli and Klebsiella pneumoniae producing extended-spectrum β-lactamases in Spain. Int J Antimicrob Agents 39(5):431–434
Pérez-Moreno MO, Picó-Plana E, De Toro M, Grande-Armas J, Quiles-Fortuny V, Pons MJ et al (2013) β-Lactamases, transferable quinolone resistance determinants, and class 1 integron-mediated antimicrobial resistance in human clinical Salmonella enterica isolates of non-Typhimurium serotypes. Int J Med Microbiol 303(1):25–31
Machuca J, Agüero J, Miró E, Conejo MD, Oteo J, Bou G et al (2016) Prevalence of quinolone resistance mechanisms in Enterobacteriaceae producing acquired AmpC β-lactamases and/or carbapenemases in Spain. Enferm Infecc Microbiol Clin DOI: 10.1016/j.eimc.2016.05.006
Dahmen S, Poirel L, Mansour W, Bouallegue O, Nordmann P (2010) Prevalence of plasmid-mediated quinolone resistance determinants in Enterobacteriaceae from Tunisia. Clin Microbiol Infect 16(7):1019–1021
Arpin C, Thabet L, Yassine H, Messadi AA, Boukadida J, Dubois V et al (2012) Evolution of an incompatibility group IncA/C plasmid harboring blaCMY-16 and qnrA6 genes and its transfer through three clones of Providencia stuartii during a two-year outbreak in a Tunisian burn unit. Antimicrob Agent Chemother 56(3):1342–1349
Mnif B, Ktari S, Chaari A, Medhioub F, Rhimi F, Bouaziz M et al (2013) Nosocomial dissemination of Providencia stuartii isolates carrying bla OXA-48 , bla PER-1 , bla CMY-4 and qnrA6 in a Tunisian hospital. J Antimicrob Chemother 68:329–332
Mahrouki S, Perilli M, Bourouis A, Chihi H, Ferjani M, Ben Moussa M et al (2013) Prevalence of quinolone resistance determinant qnrA6 among broad- and extended-spectrum beta-lactam-resistant Proteus mirabilis and Morganella morganii clinical isolates with sul1-type class 1 integron association in a Tunisian Hospital. Scand J Infect Dis 45(8):600–605
Avsaroglu MD, Helmuth R, Junker E, Hertwig S, Schroeter A, Akcelik M et al (2007) Plasmid-mediated quinolone resistance conferred by qnrS1 in Salmonella enterica serovar Virchow isolated from Turkish food of avian origin. J Antimicrob Chemother 60:1146–1150
Nazik H, Öngen B, Mete B, Aydin S, Yemisen M, Kelesoglu FM et al (2011) Coexistence of bla OXA-48 and aac(6′)-Ib-cr genes in Klebsiella pneumoniae isolates from Istanbul, Turkey. J Int Med Res 39:1932–1940
Nazik H, Ongen B, Kuvat N (2008) Investigation of plasmid-mediated quinolone resistance among isolates obtained in a Turkish intensive care unit. Jpn J Infect Dis 61:310–312
Pelrano G, Van der Bi AK, Freeman JL, Poirel L, Nordmann P, Costello M et al (2014) Characteristics of Escherichia coli sequence type 131 isolates that produce extended-spectrum-lactamases: global distribution of the H30-Rx sublineage. Antimicrob Agent Chemother 58(73):3762–3767
Loncaric I, Beiglböck C, Febler AT, Posautz A, Rosengarten R, Walzer C et al (2016) Characterization of ESBL- and AmpC-producing and fluoroquinolone-resistant Enterobacteriaceae isolated from Mouflons (Ovis orientalis musimon) in Austria and Germany. PLoS One 11(5):e0155786
Cattoir V, Nordmann P, Silva-Sanchez J, Espinal P, Poirel L (2008) ISEcp1-mediated transposition of qnrB-Like gene in Escherichia coli. Antimicrob Agents Chemother 52(8):2929–2932
Kehrenberg C, Hopkins KL, Threlfall EJ, Schwarz S (2007) Complete nucleotide sequence of a small qnrS1-carrying plasmid from Salmonella enterica subsp. enterica Typhimurium DT193. J Antimicrob Chemother 60:903–905
Ruiz E, Saénz Y, Zarazaga M, Rocha-Gracia R, Martìnez-Martìnez L, Arlet G et al (2012) qnr, aac(6′)-Ib-cr and qepA genes in Escherichia coli and Klebsiella spp.: genetic environments and plasmid and chromosomal location. J Antimicrob Chemother 67:886–897
Deng YT, Zeng ZL, Tian W, Yang T, Liu JH (2013) Prevalence and characteristics of rmtB and qepA in Escherichia coli isolated from diseased animals in China. Front Microbiol 4:198
Onuk EE, Tanrıverdi Çaycı Y, Çoban AY, Çiftci A, Balta F, Didinen BI et al (2015) Detection of the first qnrS gene positivity in aquatic Aeromonas spp. isolates in Turkey. Mikrobiyol Bul 49(1):114–123
Yang H, Hu L, Liu Y, Ye Y, Li J (2016) Detection of the plasmid-mediated quinolone resistance determinants in clinical isolates of Acinetobacter baumannii in China. J Chemother 22:1–3
Yang X, Xing B, Liang C, Ye Z, Zhang Y (2015) Prevalence and fluoroquinolone resistance of Pseudomonas aeruginosa in a hospital of South China. Int J Clin Exp Med 8(1):1386–1390
Filippa N, Carricajo A, Grattard F, Fascia P, El Sayed F, Defilippis JP et al (2013) Outbreak of multidrug-resistant Klebsiella pneumoniae carrying qnrB1 and bla CTX-M15 in a French intensive care unit. Ann Intensive Care 3(1):18
Ferjani S, Saidani M, Quentin C, Slim Amine F, Boutiba Ben Boubaker I, Dubois V (2014) Prevalence and characterization of uropathogenic Escherichia coli harboring plasmid-mediated quinolone resistance in a Tunisian university hospital. Diagn Microbiol Infect Dis 79(2):247
Longhi C, Conte MP, Marazzato M, Iebba V, Totino V, Santangelo FC et al (2012) Plasmid-mediated fluoroquinolone resistance determinants in Escherichia coli from community uncomplicated urinary tract infection in an area of high prevalence of quinolone resistance. Eur J Clin Microbiol Infect Dis 31(8):1917–1921
Dotto G, Giacomelli M, Grilli G, Ferrazzi V, Carattoli A, Fortini D et al (2014) High prevalence of oqxAB in Escherichia coli isolates from domestic and wild lagomorphs in Italy. Microb Drug Resist 20(2):118–123
Guillard T, de Jong A, Limelette A, Lebreil AL, Madoux J, de Champs C et al (2016) Characterization of quinolone resistance mechanisms in Enterobacteriaceae recovered from diseased companion animals in Europe. Vet Microbiol 194:23–29
Yousfi M, Mairi A, Touati A, Hassissene L, Brasme L, Guillard T et al (2016) Extended spectrum β-lactamase and plasmid mediated quinolone resistance in Escherichia coli fecal isolates from healthy companion animals in Algeria. J Infect Chemother 22(7):431–435
Ghodousi A, Bonura C, Di Noto AM, Mammina C (2015) Extended-spectrum ß-Lactamase, AmpC-producing, and fluoroquinolone-resistant Escherichia coli in retail broiler chicken meat, Italy. Foodborne Pathog Dis 12(7):619–625
Alouache S, Estepa V, Messai Y, Ruiz E, Torres C, Bakour R (2014) Characterization of ESBLs and associated quinolone resistance in Escherichia coli and Klebsiella pneumoniae isolates from an urban wastewater treatment plant in Algeria. Microb Drug Resist 20:30–38
Anssour L, Messai Y, Derkaoui M, Alouache S, Estepa V, Somalo S et al (2014) ESBL, plasmidic AmpC, and associated quinolone resistance determinants in coliforms isolated from hospital effluent: first report of qnrB2, qnrB9, qnrB19, and bla CMY-4 in Algeria. J Chemother 26(2):74–79
Ahmed AM, Shimamoto T (2011) Molecular characterization of antimicrobial resistance in Gram-negative bacteria isolated from bovine mastitis in Egypt. Microbiol Immunol 55(5):318–327
Cubero M, Calatayud L, Tubau F, Ayats J, Peña C, Martín R et al (2013) Clonal spread of Klebsiella pneumoniae producing OXA-1 betalactamase in a Spanish hospital. Int Microbiol 16:227–233
Rogers BA, Sidjabat HE, Paterson DL (2011) Escherichia coli O25b-ST131: a pandemic, multiresistant, community-associated strain. J Antimicrob Chemother 66:1–14
Brahmi S, Dunyach-Rémy C, Touati A, Lavigne JP (2015) CTX-M-15-producing Escherichia coli and the pandemic clone O25b-ST131 isolated from wild fish in Mediterranean Sea. Clin Microbiol Infect 21:e18–e20
Lunn AD, Fàbrega A, Sánchez-Céspedes J, Vila J (2010) Prevalence of mechanisms decreasing quinolone-susceptibility among Salmonella spp. clinical isolates. Int Microbiol 13:15–20
Al-Gallas N, Abbassi MS, Gharbi B, Manai M, Ben Fayala MN, Bichihi R et al (2013) Occurrence of plasmid-mediated quinolone resistance determinants and rmtB gene in Salmonella enterica serovar enteritidis and Typhimurium isolated from food- animal products in Tunisia. Foodborne Pathog Dis 10(9):813–819
Zhao J, Chen Z, Chen S, Deng Y, Liu Y, Tian W et al (2010) Prevalence and dissemination of oqxAB in Escherichia coli isolates from animals, farmworkers, and the environment. Antimicrob Agents Chemother 54(10):4219–4224
Buruk CK, Öztel Ocak H, Bayramoğlu G, Aydın F (2016) Investigation of plasmid-mediated quinolone resistance genes in quinolone-resistant Escherichia coli and Klebsiella spp. isolates from bloodstream infections. Mikrobiyol Bul 50(2):186–195
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None to declare.
Funding
None to declare.
Rights and permissions
About this article
Cite this article
Yanat, B., Rodríguez-Martínez, JM. & Touati, A. Plasmid-mediated quinolone resistance in Enterobacteriaceae: a systematic review with a focus on Mediterranean countries. Eur J Clin Microbiol Infect Dis 36, 421–435 (2017). https://doi.org/10.1007/s10096-016-2847-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2847-x