Abstract
Bloodstream infections (BSIs) are prevalent among people living with HIV/AIDS. The etiology varies in different regions and different periods. We aimed to survey the etiological and clinical features of BSIs in HIV patients in mainland China. We assessed all HIV patients with a positive blood culture in a Chinese teaching hospital from September 2009 through December 2014. We excluded those with specimens likely to have been contaminated. We used Pearson’s chi-squared test to measure the differences in characteristics among subgroups of different pathogens. Among 2442 Chinese HIV-seropositive inpatients, 229 (9.38 %) experienced BSIs. The most common pathogens detected included Cryptococcus neoformans (22.7 %), Penicillium marneffei (18.8 %), Mycobacterium tuberculosis (15.3 %), and non-tuberculous mycobacterium (14.8 %). 30/229 (13.1 %) HIV patients with BSIs had a poor prognosis. BSIs are prevalent in hospitalized patients with HIV/AIDS in China. Fungi and mycobacteria are the predominant pathogens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
A number of studies from different regions of the world suggested that bloodstream infections (BSIs) are frequent among people living with HIV/AIDS [1–4]. Studies that made comparisons with HIV-seronegative populations indicated that HIV infection is associated with a higher prevalence of BSIs, including mycobacteremia, other bacteremia, and fungemia [5, 6]. The literature also indicated that antiretroviral therapy (ART) significantly reduced the prevalence and changed the etiological composition of BSIs in this population. Before the era of ART, non-typhi Salmonella spp. (NTS) and Mycobacterium tuberculosis (MTB) were the most important associated pathogens. However, in the era of ART, non-opportunistic infectious agents such as Staphylococcus aureus and Streptococcus pneumoniae are increasingly important.
The etiological spectrum of BSIs also varies in different periods and different regions. For example, BSIs of Penicillium marneffei is mostly reported in southeastern Asia [7]. Mycobacteremia is mostly caused by non-tuberculous mycobacterium (NTM) in the USA, while MTB is predominant in regions with a high tuberculosis (TB) burden [8, 9].
By the end of 2013, 437,000 persons were reported to be living with HIV/AIDS in mainland China; some 40 % met the criteria of AIDS and around 30 % were on antiretroviral treatment [10]. However, there is a lack of knowledge about the prevalence, etiology, and outcome of BSIs in this population.
Methods
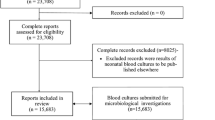
Enrollment
From September 2009 through December 2015, HIV-infected inpatients admitted to the Division of Infectious Disease, Shanghai Public Health Clinical Center with fever or other symptoms indicative of BSI were examined by blood culture. Patients with at least one positive blood culture were screened. Single culture of pathogens that are often present as contaminants (coagulase-negative staphylococci and S. aureus) were excluded from this analysis unless the patient had a typical clinical manifestation that is responsive to targeted antibiotic therapy. Post-surgery BSIs that had previously been reported by the surgical department are also excluded [11].
Settings and population
The research was done at the Division of Infectious Disease, Shanghai Public Health Clinical Center (SPHCC). SPHCC is a special hospital for infectious disease. It is the only designated hospital in the Shanghai municipality to care for HIV/AIDS patients. It is also a referral hospital for HIV/AIDS clinical care in eastern China and provides integrated care for patients from other provinces. Around half of the inpatients are referred from other provinces of China. The Division of Infectious Disease takes care of all HIV patients in the hospital who do not undergo surgery.
Definition
BSIs refer to the presence of mycobacteria, other bacteria, or fungi in the bloodstream. Severe sepsis is defined as sepsis accompanied by sepsis-induced organ dysfunction or tissue hypoperfusion. Survival is defined as BSI cured or controlled when the patient was discharged. A poor prognosis was assigned retrospectively if the patient died in hospital or was discharged with deteriorated disease and unstable vital signs.
Laboratory methods
Specimens included blood (two sites, 2 × 10 mL for aerobic bacteria, 2 × 10 mL for mycobacteria) and bone marrow when available (5–10 mL for aerobic bacteria, 5–10 mL for mycobacteria). Specimens for bacterial and fungal culture were collected in BacT/ALERT® FA bottles and then incubated for 7 days in a BacT/ALERT® 3D system (bioMérieux, France). The system automatically reported the existence and species of the organisms. Specimens for mycobacterium detection were collected in BD BACTEC™ Myco/F Lytic bottles and incubated for 42 days in the BD BACTEC 9120 automated blood culture system (BD, New Jersey). Positive cultures were subcultured onto Roche culture media slant and Showalter slant, and then tested by an MPB64-based immunochromatographic assay (Innovative Biological Prosecution Technology Co., Ltd., Hangzhou China). Strains expressing the protein MPB64 were defined as MTB and non-expressors were regarded as NTM [12].
Data analysis
We calculated proportions and medians to describe patient characteristics. We measured the difference in variables between subgroups of different pathogens by Pearson’s chi-squared test (χ2). Factors with a p-value less than 0.05 were regarded as significant. All data analyses were conducted in SPSS 17.0 software (SPSS Co. Ltd., Chicago, IL, USA).
Results
Etiology (Table 1)
Among 2442 Chinese HIV-seropositive inpatients, 229 (9.38 %) experienced BSIs . Among these infections, 69 (30.1 %) were mycobacterial infection, including 35 (15.3 %) MTB infections and 34 (14.8 %) NTM infections. Ninety-seven (42.4 %) were fungal infections, including 43 (18.8 %) cases of P. marneffei infection, 52 (22.7 %) Cryptococcus neoformans, 1 (0.4 %) Candida albicans, and 1 (0.4 %) histoplasmosis. Sixty-three (27.5 %) cases of BSIs were caused by other bacteria, including coagulase-negative staphylococci (n = 11), non-typhi Salmonella (n = 10), Escherichia coli (n = 7), Salmonella typhi (n = 6), Staphylococcus aureus (n = 5), Acinetobacter baumanii (n = 3), Enterobacter cloacae (n = 3), corynebacterium (n = 2), Enterococcus faecalis (n = 2), Streptococcus mitis (n = 2), Streptococcus lentus (n = 2), Streptococcus viridans (n = 1), Citrobacter freundii (n = 1), and Klebsiella pneumoniae (n = 1). 175 (76.4 %) episodes of BSIs could be categorized into opportunistic infections, including those yielding mycobacteria, P. marneffei, Cryptococcus neoformans, and non-typhi Salmonella.
Clinical and laboratory characteristics (Table 2)
Patients had a median age of 37 years (range 18–81). Twelve were female (5.24 %). The median CD4 count was 20/μL (1–628). 84.3 % of the patients were ART-naïve and 85.2 % had a CD4 count of <50 cells/mm3. Fungal BSIs tended to occur among patients with lower CD4 count and patients naïve of antiretroviral therapy. Twenty-eight (12.23 %) patients met the criteria of severe sepsis when BSI was diagnosed. Patients with BSIs of mycobacteria were less likely to develop severe sepsis. But the mortality rates were comparable among different groups. Eighteen patients were considered as hospital-infected BSIs, 17 were bacteremia, and the other was fungemia.
Discussion
We found that the prevalence of BSIs was 9.38 % among HIV/AIDS patients admitted to a Chinese referral hospital. A high proportion (13.3 %) of the BSIs led to a poor prognosis. Therefore, BSIs were an important comorbidity in these Chinese HIV/AIDS patients.
Opportunistic pathogens were the predominant etiology. This may be explained by the low CD4 count and ART coverage among these patients. These data may be representative in China, where most of the HIV patients were found to be naïve to ART and met the criteria of AIDS [10].
In our study, there was a significant proportion of fungal infection, including infection with P. marneffei. Patients with BSI of fungi had lower median CD4 counts than those with BSI of mycobacteria or other bacteria. The proportion of BSI patients with P. marneffei infection (18.8 %) was much higher than that reported in southeastern Asia (2.7 %) [1]. Hu et al. declared in their review that P. marneffei is an emerging pathogenic fungus in mainland China, especially the southern provinces [13]. We showed that BSIs of P. marneffei are prominent among our study population. Accordingly, this fungus should be considered when treating similar patients with BSIs in China, especially in the southern provinces.
NTM and MTB were about equally frequent in patients with mycobacteremia. The proportion of MTB was higher than in data from the USA and lower than in South Africa [8, 14]. The differences in ratio are likely related to the different levels of TB epidemics among countries and regions. It is always important to distinguish NTM from MTB, so as to provide appropriate treatment in time.
Worldwide, NTS, S. pneumoniae, E. coli, and S. aureus were reported as the main pathogens for bacterial BSIs in HIV patients [15, 16]. We did not find any S. pneumoniae bacteria in this study. This is consistent with studies in southeast Asia showing a low incidence of S. pneumoniae [12, 17].
A shortcoming of the study is that the data was retrospectively collected from a single hospital. However, the hospital treats all HIV patients in the Shanghai Municipality plus a similar number of patients transferred from other parts of China. Given that there are no national data yet, this may be the most reliable data to date. In the future, multicenter prognostic studies, especially those focusing on certain pathogens such as P. marneffei, may provide more detailed information.
References
Varma JK, McCarthy KD, Tasaneeyapan T, Monkongdee P, Kimerling ME, Buntheoun E et al (2010) Bloodstream infections among HIV-infected outpatients, Southeast Asia. Emerg Infect Dis 16(10):1569–1575. doi:10.3201/eid1610.091686
Peters RP, Zijlstra EE, Schijffelen MJ, Walsh AL, Joaki G, Kumwenda JJ et al (2004) A prospective study of bloodstream infections as cause of fever in Malawi: clinical predictors and implications for management. Trop Med Int Health 9:928–934. doi:10.1111/j.1365-3156.2004.01288.x
Oplustil CP, Leite OH, Oliveira MS, Sinto SI, Uip DE, Boulos M et al (2001) Detection of mycobacteria in the bloodstream of patients with acquired immunodeficiency syndrome in a university hospital in Brazil. Braz J Infect Dis 5:252–259. doi:10.1590/S1413-86702001000500003
Arthur G, Nduba VN, Kariuki SM, Kimari J, Bhatt SM, Gilks CF (2001) Trends in bloodstream infections among human immunodeficiency virus-infected adults admitted to a hospital in Nairobi, Kenya, during the last decade. Clin Infect Dis 33:248–256. doi:10.1086/321820
Gordon MA, Walsh AL, Chaponda M, Soko D, Mbvwinji M, Molyneux ME et al (2001) Bacteraemia and mortality among adult medical admissions in Malawi—predominance of non-Typhi salmonellae and Streptococcus pneumoniae. J Infect 42:44–49. doi:10.1053/jinf.2000.0779
Reddy EA, Shaw AV, Crump JA (2010) Community-acquired bloodstream infections in Africa: a systematic review and meta-analysis. Lancet Infect Dis 10(6):417–432. doi:10.1016/S1473-3099(10)70072-4
Kiertiburanakul S, Watcharatipagorn S, Chongtrakool P, Santanirand P (2012) Epidemiology of bloodstream infections and predictive factors of mortality among HIV-infected adult patients in Thailand in the era of highly active antiretroviral therapy. Jpn J Infect Dis 65(1):28–32
Montessori V, Phillips P, Montaner J, Haley L, Craib K, Bessuille E et al (1996) Species distribution in human immunodeficiency virus-related mycobacterial infections: implications for selection of initial treatment. Clin Infect Dis 22(6):989–992
Crump JA, Ramadhani HO, Morrissey AB, Saganda W, Mwako MS, Yang LY et al (2012) Bacteremic disseminated tuberculosis in sub-saharan Africa: a prospective cohort study. Clin Infect Dis 55(2):242–250. doi:10.1093/cid/cis409
UNAIDS. 2014 China AIDS Response Progress Report. Available online at: http://www.unaids.org.cn/uploadFiles/2015060516211133.pdf
Liu B, Zhang L, Guo R, Su J, Li L, Si Y (2012) Anti-infective treatment in HIV-infected patients during perioperative period. AIDS Res Ther 9(1):36. doi:10.1186/1742-6405-9-36
Abe C, Hirano K, Tomiyama T (1999) Simple and rapid identification of the mycobacterium tuberculosis complex by immunochromatographic assay using anti-MPB64 monoclonal antibodies. J Clin Microbiol 37(11):3693–3697
Hu Y, Zhang J, Li X, Yang Y, Zhang Y, Ma J, Xi L (2012) Penicillium marneffei infection: an emerging disease in mainland China. Mycopathologia 175(1–2):57–67. doi:10.1007/s11046-012-9577-0
von Gottberg A, Sacks L, Machala S, Blumberg L (2001) Utility of blood cultures and incidence of mycobacteremia in patients with suspected tuberculosis in a South African infectious disease referral hospital. Int J Tuberc Lung Dis 5(1):80–86
Ortega M, Almela M, Soriano A, Marco F, Martínez JA, Muñoz A et al (2008) Bloodstream infections among human immunodeficiency virus-infected adult patients: epidemiology and risk factors for mortality. Eur J Clin Microbiol Infect Dis 27:969–976. doi:10.1007/s10096-008-0531-5
Tumbarello M, Tacconelli E, Donati KG, Citton R, Leone F, Spanu T et al (2000) HIV-associated bacteremia: how it has changed in the highly active antiretroviral therapy (HAART) era. J Acquir Immune Defic Syndr 23:145–151
Hoa NT, Diep TS, Wain J, Parry CM, Hien TT, Smith MD et al (1998) Community-acquired septicaemia in southern Viet Nam: the importance of multidrug-resistant Salmonella typhi. Trans R Soc Trop Med Hyg 92:503–508. doi:10.1016/S0035-9203(98)90891-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
The study has been approved by the ethic committee of Shanghai Public Health Clinical Center.
Conflict of interest
The study was supported by the National Natural Science Foundation of China (award number: 81571977) and the Ministry of Science and Technology, People’s Republic of China (award number: 2012ZX10001-003).
There is no conflict of interest.
Human and animal rights and informed consent
All participants have signed informed consent.
Rights and permissions
About this article
Cite this article
Qi, T., Zhang, R., Shen, Y. et al. Etiology and clinical features of 229 cases of bloodstream infection among Chinese HIV/AIDS patients: a retrospective cross-sectional study. Eur J Clin Microbiol Infect Dis 35, 1767–1770 (2016). https://doi.org/10.1007/s10096-016-2724-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2724-7