Abstract
The prevalence of carbapenem-resistant Acinetobacter baumannii in Saudi Arabia and their resistance genetic mechanisms are yet to be identified. We studied the prevalence and genetic diversity of extended-spectrum beta-lactamase genes, particularly the PER-1 gene, among carbapenem-resistant A. baumannii strains from patients at a tertiary care hospital in Riyadh, Saudi Arabia between 2006 and 2014. Fresh subcultured samples were tested for antimicrobial susceptibility minimum inhibitory concentration (MIC). Total genomic DNA was extracted from each isolate and further used for polymerase chain reaction (PCR) genotyping, sequence-based typing (SBT) of PER-1 and OXA-51-like gene, and multilocus sequence typing (MLST) of positive isolates. Randomly selected clinical isolates (n = 100) were subjected to MLST. A total of 503 isolates were characterized as multidrug-resistant (MDR) using the MIC. Isolates were further PCR tested for bla -TEM and bla -PER-1 resistance genes (n = 503). The genotyping results showed that 68/503 (14 %) isolates were positive to bla TEM. The genotyping results of PER-1-like genes showed that 384/503 (76.3 %) were positive among MDR Acinetobacter isolates. Based on SBT, the majority of these isolates were clustered into three main groups including isolates harboring PER-1: AB11 (bla -PER-1), isolate AB16 (bla -PER-1), and, finally, the plasmid pAB154 (bla -PER-7). Remarkably, many isolates were concealing the PER-1 gene and harboring the TEM resistance genes as well. MLST results for selected isolates (n = 100) identified four main sequence types (STs: 2, 19, 20, and 25) and four novel isolates (ST 486–489). We report 76.3 % prevalence of the PER-1 resistance gene among Acinetobacter clinical isolates from Riyadh, Saudi Arabia. Further work is needed to explore the clinical risks and patient outcome with such resistance related to healthcare-associated infections and investigate the genetic and molecular mechanisms that confer the MDR phenotype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hospital-acquired infection due to Acinetobacter baumannii is a rising problem globally, including the Gulf region and Saudi Arabia [1–3]. Acinetobacter baumannii is a glucose non-fermentative Gram-negative bacilli which is widespread in hospitals and healthcare environments [4]. Acinetobacter baumannii plays an important role in hospital-acquired infections due to their extended survival time periods on surfaces and their high tendency to acquire resistance to multiple drugs. The resistance mechanism that A. baumannii uses is becoming a challenge for both physicians and microbiologists. One possible explanation of such a mechanism involves the selective permeability action in the outer membrane protein (porin) which controls the efflux system and the presence of chromosomal beta-lactamase [5, 6].
PER is a term that refers to Pseudomonas aeruginosa extensive resistance, which is carried onto both chromosomes and plasmids [7–9]. Although the gene was first discovered in a P. aeruginosa strain, different hypotheses argue about its origin [8, 10]. The PER-1 gene has been detected in A. baumannii strains isolated from intensive care unit (ICU) patients in Riyadh, Saudi Arabia [3]. This might have triggered an outbreak case that was first found in the country. It is an extended-spectrum beta-lactamase enzyme and encoded by the bla -PER-1 gene. This enzyme is known for its ability to hydrolyze the beta-lactam ring of antibiotics, such as penicillin, oxyimino-cephalosporins, and aztreonam [11]. PER resistance genes have been identified worldwide, including in Europe, North and South America, and the Far East, due to their chromosomal location [12]. PER-1 gene expression was first detected in 1993 in a Turkish patient in France who was infected with P. aeruginosa [13]. Different P. aeruginosa isolates harboring the enzyme were then reported in Turkey, and a widespread detection of the PER-1 enzymes has been reported in other European countries [14–16]. On the other hand, the prevalence and genetic diversity of PER-1 in the Middle East in general and Saudi Arabia in particular, are yet to be identified [2].
Many molecular typing methods have been used to study the molecular epidemiology and genetic diversity among A. baumannii isolates. Multilocus sequence typing (MLST) is based on sequencing of the seven impartially selected genes, and the genes of each are allocated a number for each different allelic form [15, 17]. Based on the sequence types (STs) of isolates (A. baumannii isolates for example), the relatedness and phylogenetic analysis of these isolates will be determined by comparing their STs with the databases created by different laboratories worldwide (http://pasteur.fr/mlst). The purpose of the current study was to investigate the prevalence of PER-1 resistance gene among carbapenem-resistant A. baumannii isolates from Riyadh, Saudi Arabia.
Materials and methods
Bacterial identification
The clinical isolates used in this study were collected at the microbiology laboratory of the 800-bed tertiary care hospital, King Abdulaziz Medical City (KAMC), Riyadh, Saudi Arabia during 2006–2014. Isolates characterized by aerobic growth and were catalase-positive, oxidase-negative were identified using commercial the biochemical system MicroScan® WalkAway (Siemens, Germany). The isolates were initially identified at the species level using MicroScan and were then confirmed by polymerase chain reaction (PCR) of the RNA polymerase β-subunit gene (rpoB), followed by sequencing.
MIC and susceptibility testing
We collected 503 isolates for antimicrobial susceptibility testing. We used a randomly selected subset (n = 130) for the MLST to further study their minimum inhibitory concentrations (MICs). The susceptibility data were interpreted according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI). It was performed using the automated MicroScan® Walkaway system. All isolates that exhibited resistance were confirmed by the Etest® (bioMérieux, France) to detect the exact MIC value. Isolates were tested for their MIC using the MicroScan Neg MIC panel type 32 including the following antibiotics: amikacin, amoxicillin/clavulanate, aztreonam, cefepime, cefotaxime, ceftazidime, ceftriaxone, ciprofloxacin, colistin, gentamicin, imipenem, meropenem, tobramycin, and trimethoprim/sulfamethoxazole. Standardized suspensions of tested isolates were inoculated and incubated at 35 °C for a minimum of 16 h and the MIC was expressed as susceptible, intermediate, and resistant according to the 2011 European Committee on Antimicrobial Susceptibility Testing (EUCAST) report. Only one isolate per patient per year was included in the current analysis. Quality control was performed by testing these same antimicrobials against Escherichia coli ATCC 25922, E. coli ATCC 35218, and P. aeruginosa ATCC 27853. The isolates were defined as multidrug-resistant (MDR) [4, 18].
DNA extraction
DNA was extracted from 100 μL of fresh subcultured samples using the DNA extraction kit MagNA Pure Compact (Roche), according to the manufacturer’s instructions. In brief, we used a combination of proteinase K enzyme and heat lysis, followed by magnetic bead capture and DNA wash. Finally, DNA was eluted with 200 μL of 10 mM Tris and 1 mM EDTA (pH 8.0) of elution buffer. The aliquots of extracted nucleic acids were stored at −20 °C until further analysis. The quantity and purity of the extracted nucleic acid samples were confirmed using a NanoDrop spectrophotometer (ND-1000, Fisher).
Detection of resistance genes
To identify the resistance genes, genotyping was performed by PCR amplification reactions with a list of primers representing the four different resistance mechanisms. Twenty pairs of primers were used for A. baumannii resistance genotyping (Eurofins, Germany) including TEM, VIM, and PER-1, as previously well established by Bonomo and others and explained elsewhere [3]. Final PCR reactions were carried out in 20-μL volumes containing 20 ng DNA, 17 μL of MegaMix-Blue (Microzone, UK) containing 1.1× PCR reaction buffer, 220 μM of dNTP, 2.75 mM MgCl2, 0.25 units of recombinant Taq DNA polymerase, and 0.40 μM each of the forward and reverse primers. PCRs were carried out using the PCR thermocycling program as recommended by the PCR mix supplier. In general, PCRs were done as follows: after the initial 10 min of incubation at 95 °C, a 30 cycle program comprising 94 °C for 30 s, 55 °C annealing temperature for 60 s, 72 °C for 60 s, and a final extension for 10 min at 72 °C was used. Some modifications in annealing temperature, number of cycles, etc. were made to optimize the amplification for certain genes. The PCR products were analyzed by electrophoresis on a 1.5 % (wt/vol) agarose gel containing 0.125 μg/mL ethidium bromide.
Sequence-based typing (SBT) and sequencing
The PCR amplicons were purified using the QIAquick PCR Extraction Kit (Qiagen, USA). Both strands of the amplicons were sequenced by using an ABI Prism BigDye Terminator Cycle Sequencing Ready Reaction Kit v1.1 (Applera, France) and an ABI 3100 automated sequencer (Biosystems, USA). PCR sequences were compared with all nucleotides sequences in the GenBank database using the PubMed National Center for Biotechnology Information BLAST program.
Multilocus sequence typing
MLST of 100 randomly selected isolates representing all clusters form the SBT-based phylogenies were carried out using the following seven housekeeping genes: cpn60 (60-KDa chaperonin), fusA (elongation factor EF-G), gltA (citrate synthase), pyrG (CTP synthase), recA (homologous recombination factor), rplB (50S ribosomal protein L2), and, finally, rpoB (RNA polymerase subunit B), as described by Diancourt et al. [19]. The primers used for MLST amplification and sequencing are listed in Table 1 and the PCR conditions used were as previously described by others [19, 20]. We used the Pasteur MLST database for allelic profiles identification (http://pubmlst.org/perl/bigsdb/bigsdb.pl?db=pubmlst_abaumannii_pasteur_seqdef).
Data analysis
Data were collected and analyzed by Excel and SPSS version 20. A phylogenetic tree was generated from the MLST allelic profile using the START 2 software using default criteria and the unweighted pair group method with arithmetic mean [21]. The MLST genotyping alleles were used to construct the tree. Moreover, the identified sequence type, patients’ demographic data, and their corresponding TEM and PER-1 genes were incorporated with the lineage tree. The isolates with new sequence types are shown with red arrows.
Results
MDR and carbapenem-resistant phenotypes
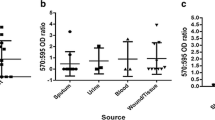
A total of 503 isolates were collected from KAMC during the period 2006–2014. The sources of the clinical isolates were as follows: respiratory 60 (46.2 %), wound and burn 31 (23.8 %), blood 18 (13.8 %), urine 5 (3.8 %), and others 16 (12.3 %). The demographic data showed that the isolates were collected from patients with the following age distribution: 2 to 24 years with 22.2 %, followed by aged 25 to 49 years (28.6 %), and, finally, 49.2 % of the patents were elderly, between 50 to 90 years. furthermore, we did not observe any significant differences in antibiotic resistance among A. baumannii isolated from males (49.2 %) versus females (50.8 %). Susceptibility testing showed that all isolates were resistant to four or more antimicrobial groups. Antibiotic susceptibility isolates against imipenem and meropenem are represented in Tables 2.
PER-1 and other carbapenems resistance genes
Carbapenems resistance phenotypes among the isolates were confirmed by MIC ≥8 μg/ml for both meropenem (96.4 %) and imipenem (88.3 %). PCR typing showed that 76.3 % of the isolates (n = 384/503) contained the PER-1 gene. On the other hand, the genotyping results showed that n = 132/503 (26.2 %) isolates were positive to bla -TEM and 457/503 (90.8 %) were positive for the OXA-51-like gene. Nevertheless, all isolates were negative to the OXA-24-like gene.
Sequence types of A. baumannii isolates and identification of regional clones
The sequence types for 100 randomly selected isolates typed by MLST were gathered in four clusters. The MLSTs of some isolates (n = 34) were not available because they were untypable or missing alleles. However, the most common sequence type (ST) was ST2 (n = 26), which is part of clonal complex 2 (CC2) and represents the European clone II (EUII) or Worldwide clone 2 (WW2). The second most common type was ST20 (CC1) (n = 19), followed by other STs. Moreover, MLST enabled the identification of four new isolates (486–489) with novel allelic profiles (Table 3). The MLST allelic profiles of the four novel STs isolates have been entered into the Institut Pasteur MLST databases. Full data of the new isolates ST-486, ST-487, ST-488, and ST-489 can be accessed at (http://pubmlst.org/perl/bigsdb/bigsdb.pl?page=info&db=pubmlst_abaumannii_isolates&id=1602).
Diversity of PER among Acinetobacter isolates
The PCR primers used for sequencing bla- PER-1 genes in A. baumannii identified two genotypic forms, PER-1-1 and PER-1-7. In addition, based on hit definition, the PER-1-positive clones were sub-divided into five groups (Table 4). The majority of PER-1 isolates are similar to isolate AB11 (bla-PER-1–1) (Table 4) and the remaining four groups represents one isolate of PER-1-1 in each, as shown in Table 4. On the other hand, the sequences of 29 isolates were submitted to the BLAST server and found to be similar to PER-7 (Table 4). This group was sub-divided into two groups: 17 isolates belong to isolate AB16 and the remaining 12 belong to pAB154.
Association of PER-1 diversity and MLST
A lineage tree was generated from MLST allelic profiles and SBT-PER using the unweighted pair group method with arithmetic mean (Fig. 1). MDR A. baumannii isolates were grouped into three clusters, where the first cluster consisted of isolates that harbored the PER-1 gene (n = 28) and belonged to ST2. Distinctively, many isolates typed as ST20 and possessing the PER-1 gene (n = 19) were the main contributors to the second cluster. However, the third cluster was a mix of STs that confer positive TEM and PER resistance genes together (Fig. 1).
Lineage tree generated from the multilocus sequence typing (MLST) allelic profile and showing the MLST a sequence type, patients’ demographic data, and their corresponding TEM and PER-1 gene occurrence in Acinetobacter clinical isolates from Saudi Arabia, with new sequence type isolates shown with bold font
Discussion
Genetically, PER-1 assumed to be part of the class A beta-lactamase enzyme but different studies contradict the idea by separating it into independent groups within classes [7–9]. This is due to the fact that the PER-1 gene shares only 26 % sequence homology with other class A beta enzymes such as TEM and SHV. Also, there are two essential conserved domains in the class A beta-lactamase structure: the omega loop fold and the cis confirmation peptide bond between 166 and 167 residues were not present in the PER-1 protein [22]. On the other hand, PER-1 was found to form a new fold in the omega loop which possessed an aspartic acid residue 138, conferring trans confirmation between 166 and 167 residues [23]. Recently, A. baumannii isolates with antibiotic resistance have been on the increase in the Gulf countries [22–26]. The characterization of its prevalence will help contain this problem. Studies dissecting the genetic structure and mode of acquisition of certain specific elements revealed that two transposons elements, ISPa12 in the upstream and ISPa13 in the downstream, surround the PER-1 gene to form the TN1213 transposon in both A. baumannii and P. aeruginosa. Also, there is a promoter in the ISPa12 element that activates the expression of the PER-1 gene [23]. In this study, 73 isolates were characterized by PCR and sequencing of the bla PER gene. The sequenced products were then analyzed for homology with equivalent sequences available at NCBI BLASTN (http://blast.ncbi.nlm.nih.gov/Blast.cgi). All of the isolates were found to be positive for this gene. Among the 73 isolates, 55 % of samples were related to the Chinese origin isolate AB11 (bla PER-1), 23 % related to the Chinese origin isolate AB16 (bla PER-1), 16 % related to the Egyptian origin plasmid pAB154 (blaPER-7), and 6 % of the isolates were related to Chinese, French, and British origin of A. baumannii. Wang et al. [27] reported a similar high prevalence of PER-1 A. baumannii in China as well. In their study, about 78 % of the Chinese imipenem-resistant Acinetobacter isolates were found to harbor the PER-1 gene. These results indicated that the prevalence of PER-1 genes is similar to that China (77.8 %) and higher than in Italy (34.61 %) and Turkey (46 %) [13, 27, 28]. Thus, the isolated strains in Riyadh, Saudi Arabia are either transferred by nationals of these countries or by Saudis who visited these countries. It is noteworthy that PER-7 represents a slight challenge, as it can hydrolyze cephalosporins more rapidly than PER-1 [29].
Conclusion
Here, we report for the first time the high prevalence of PER-1 resistance gene among Acinetobacter baumannii in Saudi Arabia. The PER-1 resistance gene was previously reported in some European countries (Turkey, France, and Italy) and North America. Further studies are needed to explore the origin and molecular mechanisms that confer the resistance phenotype
References
Al Johani SM, Akhter J, Balkhy H et al (2010) Prevalence of antimicrobial resistance among gram-negative isolates in an adult intensive care unit at a tertiary care center in Saudi Arabia. Ann Saudi Med 30(5):364–369
Aly M, Balkhy HH (2012) The prevalence of antimicrobial resistance in clinical isolates from Gulf Corporation Council countries. Antimicrob Resist Infect Control 1(1):26
Aly M, Tayeb HT, Al Johani SM et al (2014) Genetic diversity of OXA-51-like genes among multidrug-resistant Acinetobacter baumannii in Riyadh, Saudi Arabia. Eur J Clin Microbiol Infect Dis 33(7):1223–1228
Peleg AY, Seifert H, Paterson DL (2008) Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev 21(3):538–582
Poirel L, Marqué S, Héritier C et al (2005) OXA-58, a novel class D {beta}-lactamase involved in resistance to carbapenems in Acinetobacter baumannii. Antimicrob Agents Chemother 49(1):202–208
Mussi MA, Limansky AS, Viale AM (2005) Acquisition of resistance to carbapenems in multidrug-resistant clinical strains of Acinetobacter baumannii: natural insertional inactivation of a gene encoding a member of a novel family of {beta}-barrel outer membrane proteins. Antimicrob Agents Chemother 49(4):1432–1440
Bae IK, Jang SJ, Kim J et al (2011) Interspecies dissemination of the bla gene encoding PER-1 extended-spectrum beta-lactamase. Antimicrob Agents Chemother 55(3):1305–1307
Vahaboglu H, Coskunkan F, Tansel O et al (2001) Clinical importance of extended-spectrum beta-lactamase (PER-1-type)-producing Acinetobacter spp. and Pseudomonas aeruginosa strains. J Med Microbiol 50(7):642–645
Vahaboglu H, Saribaş S, Akbal H et al (1998) Activities of cefepime and five other antibiotics against nosocomial PER-1-type and/or OXA-10-type beta-lactamase-producing Pseudmonas aeruginosa and Acinetobacter spp. J Antimicrob Chemother 42(2):269–270
Pasterán F, Rapoport M, Petroni A et al (2006) Emergence of PER-2 and VEB-1a in Acinetobacter baumannii strains in the Americas. Antimicrob Agents Chemother 50(9):3222–3224
Hu WS, Yao SM, Fung CP et al (2007) An OXA-66/OXA-51-like carbapenemase and possibly an efflux pump are associated with resistance to imipenem in Acinetobacter baumannii. Antimicrob Agents Chemother 51(11):3844–3852
Chen TL, Chang WC, Kuo SC et al (2010) Contribution of a plasmid-borne blaOXA-58 gene with its hybrid promoter provided by IS1006 and an ISAba3-like element to beta-lactam resistance in Acinetobacter genomic species 13TU. Antimicrob Agents Chemother 54(8):3107–3112
Vahaboglu H, Oztürk R, Aygün G et al (1997) Widespread detection of PER-1-type extended-spectrum beta-lactamases among nosocomial Acinetobacter and Pseudomonas aeruginosa isolates in Turkey: a nationwide multicenter study. Antimicrob Agents Chemother 41(10):2265–2269
Culebras E, González-Romo F, Head J et al (2010) Outbreak of Acinetobacter baumannii producing OXA-66 in a Spanish hospital: epidemiology and study of patient movements. Microb Drug Resist 16(4):309–315
Giannouli M, Cuccurullo S, Crivaro V et al (2010) Molecular epidemiology of multidrug-resistant Acinetobacter baumannii in a tertiary care hospital in Naples, Italy, shows the emergence of a novel epidemic clone. J Clin Microbiol 48(4):1223–1230
Gogou V, Pournaras S, Giannouli M et al (2011) Evolution of multidrug-resistant Acinetobacter baumannii clonal lineages: a 10 year study in Greece (2000–09). J Antimicrob Chemother 66(12):2767–2772
Evans BA, Hamouda A, Towner KJ et al (2010) Novel genetic context of multiple bla OXA-58 genes in Acinetobacter genospecies 3. J Antimicrob Chemother 65(8):1586–1588
Rawat D, Nair D (2010) Extended-spectrum beta-lactamases in Gram negative bacteria. J Glob Infect Dis 2(3):263–274
Diancourt L, Passet V, Nemec A et al (2010) The population structure of Acinetobacter baumannii: expanding multiresistant clones from an ancestral susceptible genetic pool. PLoS One 5(4):e10034
Bacila I, Jakab E, Ferencz B et al (2008) MLST method (Multilocus Sequence Typing). Bacteriol Virusol Parazitol Epidemiol 53(1):13–17
Hujer KM, Hujer AM, Hulten EA et al (2006) Analysis of antibiotic resistance genes in multidrug-resistant Acinetobacter sp. Isolates from military and civilian patients treated at the Walter Reed Army Medical Center. Antimicrob Agents Chemother 50(12):4114–4123
Mugnier PD, Bindayna KM, Poirel L et al (2009) Diversity of plasmid-mediated carbapenem-hydrolysing oxacillinases among carbapenem-resistant Acinetobacter baumannii isolates from Kingdom of Bahrain. J Antimicrob Chemother 63(5):1071–1073
Opazo A, Vali L, Al Obaid K et al (2014) Novel genetic structure harbouring blaPER-1 in ceftazidime-resistant Acinetobacter baumannii isolated from Kuwait. Int J Antimicrob Agents 43(4):383–384
Khan FY, Abukhattab M, Baager K (2012) Nosocomial postneurosurgical Acinetobacter baumannii meningitis: a retrospective study of six cases admitted to Hamad general hospital, Qatar. J Hosp Infect 80(2):176–179
Opazo A, Sonnevend A, Lopes B et al (2012) Plasmid-encoded PER-7 beta-lactamase responsible for ceftazidime resistance in Acinetobacter baumannii isolated in the United Arab Emirates. J Antimicrob Chemother 67(7):1619–1622
Lakshmana Gowda K, Marie MA, Al-Sheikh YA et al (2014) A 6-year surveillance of antimicrobial resistance patterns of Acinetobacter baumannii bacteremia isolates from a tertiary care hospital in Saudi Arabia during 2005–2010. Libyan J Med 9:24039
Wang H, Guo P, Sun H et al (2007) Molecular epidemiology of clinical isolates of carbapenem-resistant Acinetobacter spp. from Chinese hospitals. Antimicrob Agents Chemother 51:4022–4028
Giordano A, Varesi P, Bertini A et al (2007) Outbreak of Acinetobacter baumannii producing the carbapenem-hydrolyzing oxacillinase OXA-58 in Rome, Italy. Microb Drug Resist 13:37–43
Opazo A, Sonnevend A, Lopes B et al (2012) Plasmid-encoded PER-7 β-lactamase responsible for ceftazidime resistance in Acinetobacter baumannii isolated in the United Arab Emirates. J Antimicrob Chemother 67(7):1619–1622
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work has been supported by a grant from King Abdulaziz City for Science and Technology (KACST), Riyadh, Saudi Arabia, grant number ARP-28-112.
Conflict of interest
All authors confirm that there is no conflict of interest or financial relationship with the organization that funded the research.
Ethics statement
Ethical approval and consent were not required for this study because no human or animal subjects were used.
Rights and permissions
About this article
Cite this article
Aly, M.M., Abu Alsoud, N.M., Elrobh, M.S. et al. High prevalence of the PER-1 gene among carbapenem-resistant Acinetobacter baumannii in Riyadh, Saudi Arabia. Eur J Clin Microbiol Infect Dis 35, 1759–1766 (2016). https://doi.org/10.1007/s10096-016-2723-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2723-8