Abstract
For easy handling and speed of lung diseases diagnostics, approaches based on volatile organic compounds (VOCs), including those emitted by pathogenic microorganisms, are considered but currently require considerable sampling efforts. We tested whether easy-to-handle and fast detection of lung infections is possible using solid-phase microextraction (SPME) of 100 ml of exhaled breath. An analytical procedure for the detection of VOCs from the headspace of epithelial lung cells infected with four human pathogens was developed. The feasibility of this method was tested in a cystic fibrosis (CF) outpatient clinic in vivo. Exhaled breath was extracted by SPME and analyzed by gas chromatography–mass spectrometry (GC-MS). The compositions of VOCs released in the infection model were characteristic for all individual pathogens tested. Exhaled breath of CF patients allowed clear distinction of CF patients and controls by their VOC compositions using multivariate analyses. Interestingly, the major specific VOCs detected in the exhaled breath of infected CF patients in vivo differed from those monitored during bacterial in vitro growth. SPME extraction of VOCs from 100 ml of human breath allowed the distinction between CF patients and healthy probands. Our results highlight the importance of assessing the entire pattern of VOCs instead of selected biomarkers for diagnostic purposes, as well as the need to use clinical samples to identify reliable biomarkers. This study provides the proof-of-concept for the approach using the composition of exhaled VOCs in human breath for the rapid identification of infectious agents in patients with lower respiratory tract infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Easy handling and speed are crucial for the transfer of improved infection diagnostics into the clinic [1]. For lung diseases, diagnostic approaches based on volatile organic compounds (VOCs), including those emitted by pathogenic microorganisms, are considered [2]. These VOCs comprise hydrocarbons, esters, ketones, aldehydes, and alcohols [3]. VOCs were also successfully used to distinguish between asthmatic and healthy children [4]. Several studies using complex sampling procedures focused on the characterization of compounds emitted by pathogenic microorganisms. Bacteria and fungi [5, 6] are known to produce a broad spectrum of secondary metabolites, including a wealth of volatile molecules. However, most of the microbial VOCs are released in very low concentrations, and the exact composition of the emitted volatile compounds varies with different environmental conditions. Nevertheless, the detection of microbial VOCs has great potential to be used in pathogen-directed breath testing, as currently seen for Mycobacterium tuberculosis [7, 8] or the cystic fibrosis (CF) pathogens Pseudomonas aeruginosa [9] and Aspergillus fumigatus [10]. Exhaled VOCs analysis may be an alternative approach for pathogen detection in CF healthcare, where, currently, the cultivation of infectious agents from sputum is used. With the intention to find pathogen-specific VOCs, the analysis was concentrated on compounds with molecular weights >50 Da. The aim of this study was to develop a non-invasive, easily to handle, rapid, and cost-efficient method to detect lung infections of CF patients from their breath. Instead of collecting and processing large volumes of breath, only 100 ml from the deeper lung were needed, and the VOCs were extracted by solid-phase microextraction (SPME) and analyzed. To prove this concept, an in vitro culture system was established, in which host–pathogen in vivo interactions were mimicked. VOCs emissions of routinely isolated microorganisms from CF sputum were assessed after their exposure to human lung epithelial cells. After developing the analytical procedure for the detection of VOCs from the headspace of infected epithelial lung cells, this technique was finally tested in a CF outpatient clinic in vivo.
Materials and methods
Cell culture and microbial strain preparation
Microorganisms were grown overnight in Luria broth (LB) liquid medium and diluted with fresh LB medium. Staphylococcus aureus DSM 20231, P. aeruginosa PaO1, Achromobacter xylosoxidans DSM 2402, and Candida albicans SC 5314 were grown to mid-log phase. Cultures were incubated at 37 °C on a shaking platform at 120 rpm. Microbial suspensions were used to determine colony-forming units (CFUs) and in vitro VOCs extractions. For the determination of CFUs, suspensions were diluted; triplicates (200 μl) were plated on LB agar plates and incubated at 37 °C overnight for 3 days (A. xylosoxidans) before colony counting. The A549 human epithelial cell line was maintained in Dulbecco’s modified Eagle’s medium (DMEM; PAA, Pasching, Austria), with 10 % fetal bovine serum (FCS) and 2 mM L-glutamine without antibiotics. Cells were incubated in culture flasks (37 °C, growth area of 25 cm2, humidified atmosphere with 5 % CO2). Cells were trypsinized and subcultured before reaching confluence.
Microbial in vitro models for measurements of VOC emissions
Host–pathogen interaction cultures were defined as A549 cell cultures inoculated with microbial pathogens. Bacterial suspensions (1 ml) and fungal suspensions (2 ml) in the mid-log phase were taken and centrifuged at 10,000 rpm for 8 min. Pellets were resuspended in 1 ml DMEM. Bacterial (200 μl) and fungal (2 ml) suspensions, respectively, were added to a confluent monolayer and an SPME fiber was exposed to the headspace at different time points (Table S1). Pathogen inocula: the CFUs added to A549 cells were 7.6 × 108 (7.6 × 107) for A. xylosoxidans, 4.8 × 108 (4.8 × 106) for S. aureus, 2.7 × 107 (2.7 × 106) for C. albicans, and 9.5 × 108 (9.5 × 106) for P. aeruginosa (in brackets are the CFUs for overnight incubations). All cells were kept at 37 °C in a humidified atmosphere with 5 % CO2.
SPME
VOCs were extracted using SPME [11]. For optimal VOCs extractions, different fiber coatings were tested. Major criteria for the optimal fiber were: (i) molecular weight and size of the analytes, (ii) polarity, (iii) concentration level, and (iv) complexity of sample [12], but also storage and transport between the clinic (Hannover Medical School; MHH) and the institute (Helmholtz Centre for Infection Research; HZI). A 75-μm Carboxen/polydimethylsiloxane (PDMS) fiber (Portable Field Sampler) from Supelco (Bellefonte, PA, USA) was finally selected. Here, the fiber coated with the polymers carboxen and PDMS is secured with a protective needle for transport (Portable Field Sampler, Supelco, Bellefonte, PA, USA). All fibers were preconditioned for 20 min at 250 °C. The sorbent coated fiber was exposed for 10 min to the sample and, subsequently, VOCs were released by thermal desorption in the gas chromatograph at 200 °C. Each SPME fiber showed an individual peak pattern even after preconditioning and, to minimize bias in the data analysis, all fibers used for in vivo applications were numbered and labeled. Where possible for in vitro experiments, the same fiber was taken for a series of associated VOCs extraction.
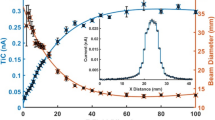
Gas chromatography/mass spectroscopy (GC-MS) parameters
For analysis, a Varian 450-GC gas chromatograph coupled with an ion-trap mass spectrometer Varian 240-MS (Varian, Palo Alto, CA, USA) and a forte GC Capillary Column 50 m × 0.32 mm × 1 μm (SGE Analytical Science, Ringwood, Australia) was used; manual injection of SPME fiber at 200 °C and with splitless mode for 2 min was followed by a split ratio of 100 for another 2 min, and a final split ratio of 20. The temperatures of the ion trap, manifold, and transfer line were 150, 50, and 180 °C, respectively. The GC oven temperature was 35 °C (2 min), then underwent heating to 75 °C at a rate of 3 °C min−1, 15 °C min−1 to 250 °C (hold for 5 min), helium flow (1 ml min−1), and electron ionization full-scan mode with a mass range m/z 40–205 was used.
CF cohort
Nine CF patients (30–48 years old, six male, three female) were recruited in the CF outpatient clinic of the MHH (Hannover, Germany), after ethical approval by the local health authority ethics committee. The study was approved by the local ethic committee (no. 1002-2011) and written informed consent was obtained from all study participants. Breath samples were taken during their routine examination in the ambulance. Anonymized clinical data of patients were collected, including culture-based microbiological diagnostics by routine cultivation methods, which were applied according to the German Quality Standards in Clinical Microbiology and Infectious Diseases [13]. Additionally, the breath samples of two healthy volunteers (30 years old; one male and one female) were taken in the HZI.
In vivo breath sampling
A modified Bio-VOC® sampler (Markes International Ltd., Rhondda Cynon Taff, UK) [14] was used for breath sampling with optimized autoclavable mouthpieces and an adapter (polyvinyl chloride), ensuring a sterile procedure and easy handling. Patients and healthy volunteers were asked to rest and, when they felt relaxed, to exhale completely a single slow breath into the sampler. The last portion of the exhaled air, originating from the alveolar space, was trapped (approx. 100 ml) and immediately exposed to the SPME fiber. No cross-contamination of exhaled VOCs was observed when the breath sampler was kept uncapped for 2 h to release the remaining analytes. In addition, ambient air was sampled for VOCs.
Data processing and statistical analyses
GC-MS data were analyzed using MS Data Review (version 6.9.3, Varian). All peaks of a chromatogram were aligned by their retention times and mass spectra. Parameters for the peak integration of host–pathogen interaction samples (in brackets: in vivo) were: peak width 4.0 s, slope sensitivity 20 (2) SN, tangent 30 % (10 %). The minimum peak size was 10,000 units for most microorganisms and 5,000 units for P. aeruginosa, respectively. Peaks were rejected if they: (i) appeared in several controls and only with smaller peak size in breath samples, (ii) were detected in controls and only from healthy individuals, (iii) were present in all samples without significant changes. All in vivo data were divided by the minimum peak size and normalized. Heatmaps were calculated using the software Package R [15] from the color palettes; the topo.colors package was chosen without scaling. Further statistical analyses were carried out using PRIMER (version 6.1.6, PRIMER-E, Plymouth Marine Laboratory, UK). Resemblance matrices were calculated using the Euclidean distance algorithm, including all variables. Samples were ordinated in non-metric multidimensional scaling (MDS) plots (50 random restarts) reflecting differences in their VOCs compositions. Trajectories were used to connect associated data points in chronological order. Two-dimensional stress values indicate the differences between ideal distances in higher-dimensional space and the actual distances in two-dimensional space.
Results
In vitro discrimination of CF pathogens by VOC emission
To establish the analytical protocol, human epithelial cells were infected with four different pathogens (S. aureus, P. aeruginosa, A. xylosoxidans, and C. albicans). In these host–pathogen interaction cultures, the VOCs were changing characteristically over time. Retention times and mass spectra differentiated the signals sufficiently, rendering further identification for diagnostic purposes unnecessary. Only steadily increasing signals were considered as culture-specific VOCs. Signals P13, P14, and P15 were only lacking in A. xylosoxidans and P7 in P. aeruginosa. Characteristic VOCs were P16 and P23 for A. xylosoxidans, P11 and P33 for C. albicans, and P32 for P. aeruginosa; however, S. aureus had no unique signal. Similarity values between the VOCs were calculated and visualized in an MDS plot after logarithmic transformation. The starting points (T0) of all four pathogens ordinated close together, but the distance increased during incubation, indicating a continuous differentiation of VOCs in each interaction culture (Figs. S1 and 1). Therefore, not just the presence and absence of released VOCs, but also the relative intensities, were characteristic for each host–pathogen interaction culture. This allows discrimination between the different pathogens in vitro and even between different time points during incubation of the interaction cultures.
In vivo analyses of VOC emissions in exhaled breath of CF patients
With this optimized protocol, the breath of nine CF patients (30–48 years old, six male, three female) from the CF outpatient clinic of the MHH were sampled. Anonymized clinical data of patients were collected, including cultured pathogens. Additionally, breath samples of two healthy volunteers were taken. Probands exhaled completely a single breath into the sampler, where the last portion, originating from the alveolar space, was trapped and immediately extracted by SPME. Ambient air was also sampled. For all samples, a rather complex signal composition was observed, characterized by the presence of 33 different signals (hP1–hP33, Fig. 2). Signals hP3 and hP5 were present in high intensities in all breath extractions, whereas controls showed no such signals or only in low intensities. Signals hP4 and hP6 were detected in all samples extracted at the clinic, but never in those made at the institute. Signal hP10 was ubiquitously present in all chromatograms, and its intensities were higher in all samples stored or transported for more than 1 h after exposition. Furthermore, SPME fibers showed individual signal patterns. No VOCs from the CF patients matched with the characteristic VOCs of the host–pathogen interaction cultures. For a detailed analysis, the samples were ordinated in an MDS plot (Fig. 3). The MDS plot revealed clustering, clearly separating healthy individuals from CF patients and from control samples. The VOCs datasets were further compared with the individual clinical data of CF patients, as well as with individual results from microbiological diagnostics (Table S2); however, no further correlations were observed.
Heatmap of VOC compositions from breath extractions. VOCs extractions from the exhaled breath of CF patients were taken at the MHH, whereupon ProA and ProB were extractions from healthy non-CF individuals, performed at the HZI. Room samples are indicated as MHH and HZI samples and SPME fibers without exposition are marked mhh or hzi, respectively. Signals are numbered hP1–hP33. The relative intensities of signals are indicated by a gray gradient, in which the intensity increases from dark to bright gray, whereas blank boxes indicate that no signal was detected. The locations of sampling are annotated with MHH/mhh for clinical samples and HZI/hzi for the institute. The numbers in the sample labels indicate the individual SPME fiber used for the experiments
MDS plot of VOCs extraction from breath analyses. The VOCs compositions of different samples were compared and samples ordinated according to similarity values. The symbols are affiliated to samples and identified in the figure. The dashed lines indicate the three different clusters of samples within the plot. The stress value indicates the differences between the ideal statistical distances of samples in higher-dimensional space and the actual distances in this two-dimensional space
Discussion
The diagnostic potential of biomarkers in exhaled breath is attracting growing attention, and different approaches have been tested in recent years. Several thousand different VOCs from diverse origins and biochemical pathways have been detected in levels of parts-per-billion (ppb) with various methods in human exhaled air [16]. Studies in the past concentrated on the search for single biomarker molecules for a certain respiratory pathogen, which leads to several difficulties further discussed below. Several studies investigated VOCs released by P. aeruginosa [17, 18] and S. aureus [19] in vitro, revealing numerous compounds in the headspace of these microorganisms. Recently, 2-aminoacetophenone has gained attention as a biomarker molecule for P. aeruginosa and was used in a first breath analysis study to identify P. aeruginosa-colonized CF patients [20, 21]. However, other studies detected this compound also in the headspace of different respiratory pathogens [22] and in food [23]. Furthermore, microbial VOCs production and intensity are strongly influenced by growth media and conditions [24].
Interestingly, none of the VOCs from in vitro cultures were detected in the exhaled breath of CF patients, although colonization of patients with pathogens was confirmed by cultivation. Potential explanations for this discrepancy may be the emission of different microbial VOCs due to limitations of the in vitro cultures resulting from the considerable number of different conditions in the human lung. Further reasons may be VOCs present at very low concentrations and the relatively healthy status of the studied patients. This highlights the importance of carrying out studies in humans to identify VOCs which are reliable biomarkers for the clinical management of infected patients. In our study, evidence was provided that no single molecule but, rather, the global VOCs pattern is an appropriate target in the search for volatile biomarkers. The MDS plots used here have the advantage of featuring multivariate similarity and simultaneously providing the underlying variables responsible for certain groupings. A clear influence of the ambient air was observed, demanding a priori calibration. In a comparative study comprising 12 VOCs in exhaled breath from CF patients and healthy individuals, slightly altered compositions were observed between both groups, identifying no distinct biomarkers [25]. Nevertheless, in our study, differences in exhaled air profiles were observed and resulted in a grouping of VOCs profiles separating CF patients from healthy volunteers.
By extracting large volumes, 1,099 VOCs in the breath of CF patients were analyzed and 100 % identification of CF patients and healthy individuals was shown [26]. Even further discrimination of P. aeruginosa-colonized patients was achieved. These results strongly suggest that the composition of exhaled compounds is superior to single biomarkers for the differentiation between respiratory infections. Our study demonstrated that large breath volumes combined with time-consuming extraction procedures are not required for breath analyses. The SPME approach applied here has the advantage of easy handling, as demonstrated by its successful application in the outpatient clinic. Furthermore, it demonstrated the potential to deliver results faster with reduced effort and costs in comparison to sputum-based diagnostics (Table 1).
Conclusions
This study showed that the simplified extraction procedure for volatile organiccompounds (VOCs) allowed the differentiation of microbial species and underlines that human breath delivers information on the health status of the lung. The profile of exhaled VOCs in combination with multivariate analyses rather than single molecules [27] was found to be more informative for clinical diagnostics [28]. Despite the great potential of such a non-invasive diagnostic method, the technical issues are demanding [29], and techniques for breath sampling and VOCs extraction have to be further optimized. Overall, exhaled VOCs analysis for the detection of pulmonary infectious diseases has the potential to become a rapid and efficient diagnostic tool in the future.
References
Fournier P-E, Drancourt M, Colson P, Rolain J-M, La Scola B, Raoult D (2013) Modern clinical microbiology: new challenges and solutions. Nat Rev Microbiol 11:574–585
Horváth I, Lázár Z, Gyulai N, Kollai M, Losonczy G (2009) Exhaled biomarkers in lung cancer. Eur Respir J 34:261–275
Schulz S, Dickschat JS (2007) Bacterial volatiles: the smell of small organisms. Nat Prod Rep 24:814–842
Dallinga JW, Robroeks CMHHT, van Berkel JJBN, Moonen EJC, Godschalk RWL, Jöbsis Q, Dompeling E, Wouters EFM, van Schooten FJ (2010) Volatile organic compounds in exhaled breath as a diagnostic tool for asthma in children. Clin Exp Allergy 40:68–76
Sethi S, Nanda R, Chakraborty T (2013) Clinical application of volatile organic compound analysis for detecting infectious diseases. Clin Microbiol Rev 26:462–475
Kramer R, Abraham W-R (2012) Volatile sesquiterpenes from fungi: what are they good for? Phytochem Rev 11:15–37
Syhre M, Manning L, Phuanukoonnon S, Harino P, Chambers ST (2009) The scent of Mycobacterium tuberculosis—part II breath. Tuberculosis (Edinb) 89:263–266
Phillips M, Basa-Dalay V, Bothamley G, Cataneo RN, Lam PK, Natividad MPR, Schmitt P, Wai J (2010) Breath biomarkers of active pulmonary tuberculosis. Tuberculosis (Edinb) 90:145–151
Goeminne PC, Vandendriessche T, Van Eldere J, Nicolai BM, Hertog ML, Dupont LJ (2012) Detection of Pseudomonas aeruginosa in sputum headspace through volatile organic compound analysis. Respir Res 13:87
Chambers ST, Bhandari S, Scott-Thomas A, Syhre M (2011) Novel diagnostics: progress toward a breath test for invasive Aspergillus fumigatus. Med Mycol 49(Suppl 1):S54–S61
Pawliszyn J (2009) Handbook of solid phase microextraction. Chemical Industry Press of China, Beijing
Woolfenden E (2010) Sorbent-based sampling methods for volatile and semi-volatile organic compounds in air. Part 2. Sorbent selection and other aspects of optimizing air monitoring methods. J Chromatogr A 1217:2685–2694
Hogardt M (2006) MIQ 24: Atemwegsinfektionen bei Mukoviszidose: Qualitätsstandards in der mikrobiologisch-infektiologischen Diagnostik. Urban & Fischer in Elsevier
Henderson KA, Matthews IP (2002) Biological monitoring of midwives’ exposure to N2O using the Bio-VOC breath sampler. J Expo Anal Environ Epidemiol 12:309–312
R Development Core Team. R: a language and environment for statistical computing. Home page at: http://www.R-project.org
Boots AW, van Berkel JJ, Dallinga JW, Smolinska A, Wouters EF, van Schooten FJ (2012) The versatile use of exhaled volatile organic compounds in human health and disease. J Breath Res 6:027108
Labows JN, McGinley KJ, Webster GF, Leyden JJ (1980) Headspace analysis of volatile metabolites of Pseudomonas aeruginosa and related species by gas chromatography–mass spectrometry. J Clin Microbiol 12:521–526
Shestivska V, Nemec A, Dřevínek P, Sovová K, Dryahina K, Španěl P (2011) Quantification of methyl thiocyanate in the headspace of Pseudomonas aeruginosa cultures and in the breath of cystic fibrosis patients by selected ion flow tube mass spectrometry. Rapid Commun Mass Spectrom 25:2459–2467
Filipiak W, Sponring A, Baur MM, Filipiak A, Ager C, Wiesenhofer H, Nagl M, Troppmair J, Amann A (2012) Molecular analysis of volatile metabolites released specifically by Staphylococcus aureus and Pseudomonas aeruginosa. BMC Microbiol 12:113
Cox CD, Parker J (1979) Use of 2-aminoacetophenone production in identification of Pseudomonas aeruginosa. J Clin Microbiol 9:479–484
Scott-Thomas AJ, Syhre M, Pattemore PK, Epton M, Laing R, Pearson J, Chambers ST (2010) 2-Aminoacetophenone as a potential breath biomarker for Pseudomonas aeruginosa in the cystic fibrosis lung. BMC Pulm Med 10:56
Groenhagen U, Baumgartner R, Bailly A, Gardiner A, Eberl L, Schulz S, Weisskopf L (2013) Production of bioactive volatiles by different Burkholderia ambifaria strains. J Chem Ecol 39:892–906. Erratum in: J Chem Ecol 39:1343–1345
Scott-Thomas A, Pearson J, Chambers S (2011) Potential sources of 2-aminoacetophenone to confound the Pseudomonas aeruginosa breath test, including analysis of a food challenge study. J Breath Res 5:046002
Preti G, Thaler E, Hanson CW, Troy M, Eades J, Gelperin A (2009) Volatile compounds characteristic of sinus-related bacteria and infected sinus mucus: analysis by solid-phase microextraction and gas chromatography–mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 877:2011–2018
Barker M, Hengst M, Schmid J, Buers H-J, Mittermaier B, Klemp D, Koppmann R (2006) Volatile organic compounds in the exhaled breath of young patients with cystic fibrosis. Eur Respir J 27:929–936
Robroeks CMHHT, van Berkel JJBN, Dallinga JW, Jöbsis Q, Zimmermann LJ, Hendriks HJ, Wouters MF, van der Grinten CP, van de Kant KD, van Schooten FJ, Dompeling E (2010) Metabolomics of volatile organic compounds in cystic fibrosis patients and controls. Pediatr Res 68:75–80
Enderby B, Smith D, Carroll W, Lenney W (2009) Hydrogen cyanide as a biomarker for Pseudomonas aeruginosa in the breath of children with cystic fibrosis. Pediatr Pulmonol 44:142–147
Thorn RMS, Reynolds DM, Greenman J (2011) Multivariate analysis of bacterial volatile compound profiles for discrimination between selected species and strains in vitro. J Microbiol Methods 84:258–264
Chambers ST, Scott-Thomas A, Epton M (2012) Developments in novel breath tests for bacterial and fungal pulmonary infection. Curr Opin Pulm Med 18:228–232
Acknowledgments
We thank Esther Surges for the maintenance of GC-MS. RK, CAG, MGH, and W-RA were funded by institutional funds of the HZI; AS-H and TW were funded by institutional funds of the MHH.
Conflict of interest
RK, AS-H, CAG, MGH, and W-RA declare that they have no competing interests. TW is on the advisory board of Bayer, NOVARTIS, and Basilea, and lecturing for Bayer and NOVARTIS.
Authors’ contributions
RK established the analytical methods, analyzed the samples, carried out the interpretation of data, and contributed to the writing of the article. AS-H selected the patients, sampled their breath, and contributed medical data of the patients. W-RA oversaw all aspects, contributed to the conception and design of the article, conceptualized and oversaw analyses, contributed to the interpretation of data, and wrote the article. CAG, MGH, and TW oversaw all aspects and reviewed the article for important intellectual content. All the co-authors critically revised the manuscript and approved the final draft before submission.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 117 kb)
Rights and permissions
About this article
Cite this article
Kramer, R., Sauer-Heilborn, A., Welte, T. et al. A rapid method for breath analysis in cystic fibrosis patients. Eur J Clin Microbiol Infect Dis 34, 745–751 (2015). https://doi.org/10.1007/s10096-014-2286-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2286-5