Abstract
Background
The majority of patients with glioblastoma (GBM) experience disease progression. At recurrence, treatment options have limited efficacy. Many studies report a limited and short duration response rate. Although clinical trials represent the “gold standard” for providing evidence on efficacy of specific treatment strategies, real-world data can be considered more representative of the “real” GBM population.
Objective
To describe the management of GBM recurrence in a large real-world sample.
Methods
We analysed retrospectively the data stored in the database of the Neuro-oncology Unit, IRCCS “Regina Elena” National Cancer Institute, Rome, Italy. We considered only data of patients with histological diagnosis of GBM and disease recurrence during their follow-up. We excluded patients who did not receive treatment after the diagnosis.
Results
We analysed 422 patients (64% males, 36% females) with a mean age of 59.6 (range 16–87) years. At GBM recurrence, 135 (32.0%) patients underwent palliative care, and 287 (68.0%) underwent other treatments. Patients on palliative care were older, had a worse performance status, and a shorter time between GBM diagnosis and its recurrence. Patients who received chemotherapy in combination with other treatments (surgery and/or radiation therapy) at GBM recurrence had a longer survival than those in palliative care (p < 0.001). Surgery or radiation therapy alone did not have any effect on survival as compared with palliative care (p < 0.001).
Conclusion
This study confirms the importance of a multidisciplinary approach even at GBM recurrence, suggesting that combination treatments play a key role in management of disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common primary malignant brain tumour with a poor prognosis [1].
Nowadays, the standard of care involves maximal safe surgical resection followed by radiation therapy (RT) with concomitant and adjuvant chemotherapy (CT) plus temozolomide (TMZ) [2]. About 70% of GBM patients will experience disease progression within 1-year post-diagnosis [2], with less than 5% of patients surviving 5 years after diagnosis [2,3,4].
Advanced age, poor performance status, and incomplete extent of resection are well-established negative prognostic factors [5, 6], whereas molecular features, such as O6-methylguanine-DNA methyltransferase (MGMT) methylation and isocitrate dehydrogenase-1 (IDH-1) mutation, are strong predictors of better outcomes from TMZ treatment thus confirming the prognostic role of IDH 1 mutation [4].
At recurrence, treatment options have limited efficacy. Many studies report a limited response rate and, when present, it is of short duration [7]. Second surgery, second courses of RT, and experimental treatment options can be considered [7]. Surgery is an option for some patients, and surgical debulking can alleviate mass effect and symptoms. Some evidence showed that greater extent of resection at recurrence is associated with improved survival [8, 9]; however, other studies have not found an absolute benefit in terms of survival [10, 11]. Re-irradiation is an appropriate option in selected patients, i.e. younger individuals with good performance status [12]. Similar to surgery, there are no randomized controlled trials (RCTs) demonstrating benefit on survival [7].
Second-line CT can be offered to patients with recurrent GBM, such as second course of TMZ, nitrosoureas, and platinum-based regimens. The use of second-line agents remains the most debated topic in this field. Recently, the Italian Medicines Agency (AIFA) approved regorafenib for the first recurrence of GBM [13]. The objective response rates to second-line treatment are dismal, and time to progression for standard cytotoxic agents is only 3 to 6 months [14].
Given the lack of an established evidence-based management, here we aimed to describe the approach to recurrent GBM in a large real-world population followed in a tertiary care centre.
Methods
Participants
We retrospectively analysed data stored in a database of the Neuro-oncology Unit of IRCCS Regina Elena National Cancer Institute, Rome, Italy. We considered data of patients with histological diagnosis of GBM and disease recurrence during their follow-up. We excluded patients who did not receive treatment after diagnosis. Patients’ data were regularly collected and stored into an electronic “ad hoc” database which includes demographic, clinical, and molecular data, as well as data on treatments (CT, RT, surgery), and outcomes, including the progression-free survival (PFS), post-recurrence survival (PRS), and overall survival (OS).
Outcome measures
PFS was defined as the time elapsed from GBM diagnosis to its recurrence or, in the absence of documented disease progression, to death.
PRS was defined as the time elapsed from GBM recurrence to death.
OS was defined as the time elapsed from GBM diagnosis to death due to any cause.
For patients who were still alive at the time of database lock, PRS and OS were censored at the time of the last visit.
Statistical analysis
Categorical data were presented as count (proportion) and continuous data were presented as mean ± standard deviation (SD) or median [range], as appropriate. When applicable, continuous data were categorized arbitrarily to facilitate the interpretation of results.
We explored factors associated with PFS and PRS by time-to-event analyses.
The univariate and multivariate Cox proportional hazards regression models were carried out to ascertain: (1) the effect of demographic and clinical variables collected at diagnosis on PFS (as per inclusion criteria, all patients reached the event and therefore there was no censored case in these analyses); (2) the effect of demographic and clinical variables collected at GBM recurrence on PRS.
Additional survival analyses were conducted by means of Kaplan–Meier curves and Cox regression models to explore the effect of variables of interests on the predefined outcomes: (1) we investigated the association between PFS and the cycles of first-line CT and the PFS; (2) we investigated the association between OS and second-line treatments strategy. Two-sided p-values < 0.05 were considered as significant.
Results
Study population
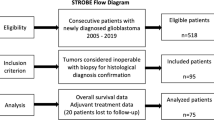
The Neuro-oncology database of the IRCCS Regina Elena National Cancer Institute contains data on 1391 patients with gliomas. Among them, 642 have histological diagnosis of GBM, including 422 (65.7%) with disease recurrence. Most patients (n = 228) attended our Institute from the diagnosis of GBM, whereas the remaining 194 were initially followed in other Institutes.
We collected data of 422 patients (64% males, 36% females) with a mean age of 59.6 ± 12.3 (range 16–87) years, who received a diagnosis of GBM from September 2007 to April 2021. Their demographic and clinical characteristics at diagnosis are shown in Table 1. The mean Karnofsky Performance Status (KPS) before starting treatment was 90.4 ± 12.2 [range: 60–100]. Molecular data on MGMT and IDH-1 were available for 289 and 221 patients, respectively.
Most of them (n = 385, 91%) underwent resection and received the standard of care according to the Stupp protocol (n = 351, 80.8%) or Perry protocol (n = 31, 7.3%), while the remaining patients (n = 50, 11.8%) were treated with only TMZ without receiving RT.
At database lock (December 2021), the median number of TMZ cycles received by patients was 6 [range 1 to 42]. Out of 422, 191 patients continued to receive CT even beyond the scheduled 6 TMZ cycles, whereas 160 patients received less than the scheduled 6 TMZ cycles due to disease progression (n = 142, 88.7%) or side effects (n = 18, 11.3%).
At follow-up, 377 (89.3%) out of 422 patients died, yielding to a median OS of 18 (range 1–152) months.
GBM recurrence
For inclusion criteria, all patients had recurrent GBM, i.e. there were no patients free from disease progression, after a median time of 11 months [range: 1 to 99 months].
In most cases, GBM recurrence occurred while receiving the TMZ (n = 338, 80.1%), whereas the remaining 84 patients discontinued their TMZ treatment before GBM recurrence, either under stable disease after completing the Stupp protocol (n = 56, 13.3%), or due to side effects (n = 28, 6.6%).
All patients who discontinued TMZ under stable disease received RT as part of the Stupp protocol before GBM recurrence; they also had better KPS than those on current TMZ treatment, and those discontinuing due to side effects (p ≤ 0.02). There was no other difference across these three subgroups of patients at GBM recurrence (see Table 2). As expected, patients who had GBM recurrence under stable disease after discontinuing TMZ received more TMZ cycles than both those who discontinued for side effects and those who experienced disease progression (p < 0.001).
The Cox regression model on PFS as outcome revealed the following predictors for a faster GBM recurrence: age at diagnosis > 60 years (HR = 1.32, p = 0.005), KPS at diagnosis ≤ 70 (HR = 2.82, p < 0.001), no previous RT (HR > 2.40, p < 0.001), and unmethylated MGMT (HR = 1.93, p < 0.001). The multivariable analysis confirmed these findings, with except for age at diagnosis that was the only variable not surviving after entering multiple covariates into the model (see Table 3). We did not enter the IDH-1 in the model, as all patients with available data had the wild-type enzyme.
However, considering only patients discontinuing their first-line treatment (n = 84), we observed a longer time to GBM recurrence with more cycles of TMZ: HR = 0.52 (95% CIs 0.27–0.99, p = 0.048) for 6–12 cycles and HR = 0.20 (95% CIs 0.11–0.35, p < 0.001) for > 12 cycles as compared with < 6 cycles (see Fig. 1).
Progression-free survival curves by cycles of chemotherapy received in a subgroup of patients who discontinued their first-line treatment due to side effect or partial/complete disease remission (n = 84). Post-recurrence survival curves by second-line treatments started after GBM recurrence (n = 287)
Post-recurrence survival after GBM recurrence
The median PRS was 5 months [range: < 1 to 111].
The Cox regression model on PRS as outcome revealed the following predictors at the univariate analysis (see the Table 4): age > 60 years (HR = 1.57, p < 0.001), KPS ≤ 70 (HR = 2.85, p < 0.001), < 12 months from onset to GBM recurrence (HR = 1.64, p < 0.001), ongoing treatment at GBM recurrence (HR = 2.16, p < 0.001), and unmethylated MGMT (HR = 1.68, p < 0.001). The time from GBM onset to recurrence was the only variable not surviving the multivariate analysis, likely because its effect was absorbed by the treatment status at GBM recurrence, i.e. the longer the time elapsed from onset to GBM recurrence was, the higher the likelihood to discontinue first-line treatment was.
Treatment at recurrence
After GBM recurrence, 135 (32.0%) patients underwent palliative care, while the remaining 287 (68.0%) underwent another treatment. There were several differences between patients on palliative care and those who underwent another treatment (see Table 5). Patients on palliative care were older, had a worse KPS, a shorter time from diagnosis to GBM recurrence, and received less cycles of first-line chemotherapy than those who started a second treatment after GBM recurrence (p < 0.001). As expected, patients on palliative care had an increased chance of death (HR = 4.67, p < 0.001) than those who started a second-line treatment after GBM recurrence.
A subgroup analysis on 181 patients with KPS ≤ 70 at GBM recurrence confirmed that palliative care was associated with shorter OS as compared with any second-line treatment (HR = 2.53, p < 0.001).
Among patients who received a second-line treatment after GBM recurrence (n = 287), CT was started by 260 (90.6%) patients either as unique therapy (n = 149, 51.9%), or in addition with surgery (n = 73, 25.4%), RT (n = 15, 5.2%), or both (n = 23, 8.0%). The remaining 27 patients (9.4%) underwent only surgery (n = 20, 7.0), only RT (n = 4, 1.4%), or both (n = 3, 1.0%).
On 119 patients subjected to second surgery, 20 (16.8%) patients showed deterioration of clinical condition and no other treatment was considered. Twelve (10%) patients showed a deterioration KPS from 100 to 70–80. This group was composed of older and shorter interval between diagnosis and recurrence patients. The majority of patients showed advantages in terms of clinical outcomes.
Patients received the following second-line CTs: nitrosureas (n = 138), rechallenging of TMZ (n = 47), bevacizumab (n = 28), regorafenib (n = 22), bevacizumab plus nitrosureas (n = 19), experimental treatments (n = 6).
Of 138 patients treated with nitrosurea, 71 (51.4%) received lomustine and 67 (48.6%) received fotemustine.
The median number of cycles of second-line CT was 3 [range: 1 to 39].
In the subgroup of patients with GBM recurrence during their first-line treatment, regorafenib was associated with worse PRS than nitrosureas (HR = 0.54, 95% CIs 0.29–0.99, p = 0.048) and bevacizumab (alone or in combination) or experimental chemotherapies (HR = 0.56, 95% CIs 0.29–1.08, p = 0.084). However, these findings were not confirmed after correction by sex, age, KPS, time from onset to GBM recurrence, and MGMT status. Furthermore, 58% of patients treated with regorafenib had unmethylated MGMT status, whereas in the other subgroups, unmethylated MGMT status ranged from 30 to 38%.
Patients who started CT associated with RT and/or surgery had a longer PRS than those who received only CT (HR = 0.40, p < 0.001), and those who underwent surgery plus RT (HR = 0.52, p = 0.008), whereas there was no difference in PRS between only CT and surgery plus RT (Fig. 1).
Discussion
Despite recent advances in multimodality therapy for GBM, the overall prognosis remains poor and long-term survival is rare.
In our study, patients had GBM recurrence after a median time of 11 months. Patients died after a median time of 5 months (< 1 to 111) from GBM recurrence and 18 months (range 2 to 152) from disease onset. Wong et al. reported median PFS and OS for recurrent GBM of 10 weeks and 30 weeks, respectively [15]. The median survival for most patients from the time of diagnosis is less than 15 months, with a 2-year survival rate of 26–33% [2, 16].
In this study, the predictors for a faster GBM recurrence were KPS at diagnosis ≤ 70, non-administration of RT, and unmethylated MGMT. These findings confirm data in literature, emphasizing that risk factors associated with lower survival are as follows: old age of the patient (≥ 60 years), partial resection of the tumour, low preoperative functional status (KPS < 70), absence of RT and CT, less than 4 courses of postoperative CT with TMZ [17]. Among favourable prognostic factors, young age, radical resection, satisfactory general condition of the patient MGMT promoter methylation, and IDH mutations gene are reported [18, 19].
In 2005, a randomized clinical trial showed significantly better 2- and 5-year survival for patients administered combined chemo-radiotherapy [2] and confirmed in 2009 [4]. In our study, we confirm that patients who do not undergo RT have a major risk of recurrence than those who do undergo RT.
In most cases, GBM recurrence occurred during adjuvant TMZ and 19% during discontinued treatment. From these results interesting but controversial data emerge on the prolonged use of therapy with TMZ. We observed a longer PFS with more cycles of chemotherapy for > 12 cycles as compared with < 6 cycles. There is no consensus regarding the appropriate duration of TMZ treatment, and it is a common practice to prolong TMZ treatment until there is evidence of tumour progression or development of toxicity [20, 21]. In addition, whether TMZ can be discontinued when the tumour shows good response to prolonged treatment is still unclear [20, 22].
Tumour recurrence is nearly universal in GBM but today the evidence-based guidelines for treatment decision-upon disease recurrence are lacking [23]. In our study, the majority of patients underwent second-line treatment in particular CT but 32% of patients received only supportive care. We observed that patients that received only supportive care were older, had a worse KPS, and a shorter time from diagnosis to recurrence. Keime-Guibert et al. reported that in older patients, the median survival is < 4 months with best supportive care alone [24].
Most patients in this study underwent CT and the most frequently used treatment is nitrosurea (fotemustine or lomustine). According to literature, CT remains the elective treatment choice at recurrence and, for patients with a substantially reduced performance status, supportive care measures alone may be more appropriate. There is no standard-of-care systemic therapy in the second-line setting; however, alkylating chemotherapy is commonly used. Lomustine, carmustine, fotemustine, and rechallenge with TMZ are all potential options, although the benefits are modest, and only patients with MGMT promoter methylation are likely to benefit [25,26,27]. Salvage chemotherapy with combined procarbazine, lomustine, and vincristine may have some activity, although this is limited by much greater toxicity [28, 29]. Several studies reported efficacy and safety of fotemustine in glioblastoma recurrence treatment [30]
Overall, the quality of data for individual chemotherapy agents or regimens is poor, and comparison across studies is difficult mainly because the majority of studies do not account for Stupp protocol and the emerging molecular evidence.
Nitrosureas are routinely used as salvage therapy and still play an important role in the treatment of recurrence.
Recently, the drug regorafenib was approved in Italy for the first recurrence of GBM. The “REGOMA” trial was a medium-sized phase II trial and several prognostic factor imbalances favoured the regorafenib group: patients were on steroids less frequently, were younger, had more often MGMT promoter-methylated tumours, and had a longer progression-free survival with first-line therapy. Furthermore, cross-trial comparison indicates particularly poor outcome with lomustine [13]. Conversely, in our study, patients treated with Regorafenib have a poorer prognosis, but the little sample size and bias of selection did not permit a conclusion.
In the literature, it is reported that the TMZ is often used for rechallenging with an overall response rate of 10%. We reported a rechallenging of TMZ in 46 patients discontinuing treatment before GBM recurrence for disease control.
We observed that the surgery alone does not have an impact on prognosis but has an important role in combination with CT. In literature, the role of second surgery remains controversial and should be considered in a selected population. The patients who undergo surgery may also be considered for adjuvant chemotherapy, with special attention to the various molecular predictive markers in the specimen. The adjuvant chemotherapy after re-irradiation may follow the principles of adjuvant chemotherapy after re-excision [31]. Some retrospective studies proposed a survival benefit after reoperation while others did not [8,9,10,11, 32, 33]. The most common limitation in the majority of studies includes high probability of selection bias.
The main limitation of the present study concerns its retrospective design that is prone to selection and hidden biases, therefore can be considered only as “hypothesis-generating”. However, even if RCTs represent the “gold standard” for providing evidence on efficacy of specific treatment strategies, real-world data as those from our study can be considered more representative of the GBM population than RCT samples. Patients enrolled in RCTs are indeed pre-selected to enhance the power to demonstrate a treatment effect, but the results of any trial are only partially reproducible in widespread clinical practice. Well-conducted and large retrospective experiences — like the present study — may provide the opportunity for a less expensive evaluation of therapies in a real-life clinical setting.
Conclusion
We confirmed the importance of the multidisciplinary approach at recurrence and that combination therapy plays a key role in management of disease. Indeed, we observed that patients who started CT associated with other treatments (surgery and/or RT) had a longer OS than those who received only CT and those who underwent surgery plus RT. Very important factors for a decision-making strategy include as follows: age at diagnosis, performance status, time to recurrence, and MGMT methylation.
Nowadays, CT with nitrosureas represents first choice therapy strategy for GBM recurrence, but future data may be modified because of AIFA’s approval of regorafenib as a second-line treatment option. The addition of RT and surgery needs to be evaluated in selected patients.
Data availability
The data that support the findings of this study are available on request from the corresponding author [V.V.]. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Code availability
Not applicable
References
Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS (2018) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro Oncol 20(suppl4):iv1–iv86
Stupp R, Mason WP, Van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Ronning PA, Helseth E, Meling TR, Johannesen TB (2012) A population-based study on the effect of temozolomide in the treatment of glioblastoma multiforme. Neuro Oncol 14:1178–1184
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Lacroix M, Abi-Said D, Fourney DR et al (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95:190–198
Lamborn KR, Chang SM, Prados MD (2004) Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol 6:227–235
Tan AC, Ashley DM, López GY, Malinzak M, Friedman HS, Khasraw M (2020) Management of glioblastoma: state of the art and future directions. CA Cancer J Clin 70(4):299–312
Bloch O, Han SJ, Cha S, Sun MZ, Aghi MK, McDermott MW, Berger MS, Parsa ATJ (2012) Impact of extent of resection for recurrent glioblastoma on overall survival: clinical article. Neurosurg 117(6):1032–1038
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, Weingart JD, Brem H, Quiñones-Hinojosa AR (2009) Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg 110(1):156–162
Brandes A, Bartolotti M, Franceschi E (2013) Second surgery for recurrent glioblastoma: advantages and pitfalls. Expert Rev Anticancer Ther 13(5):583–587
Franceschi E, Bartolotti M, Tosoni A, Bartolini S, Sturiale C, Fioravanti A et al (2015) The effect of re-operation on survival in patients with recurrent glioblastoma. Anticancer Res 35(3):1743–1748
Cabrera AR, Kirkpatrick JP, Fiveash JB, Shih HA, Koay EJ, Lutz S et al (2016) Radiation therapy for glioblastoma: executive summary of an American Society for Radiation Oncology evidence-based clinical practice guideline. Pract Radiat Oncol l6(4):217–225
Lombardi G, De Salvo GL, Brandes AA, Eoli M, Rudà R, Faedi M et al (2019) Regorafenib compared with lomustine in patients with relapsed glioblastoma (REGOMA): a multicentre, open-label, randomised, controlled, phase 2 trial. Lancet Oncol 20(1):110–119
Franceschi E, Tosoni A, Bartolini S, Mazzocchi V, Fioravanti A, Brandes AA (2009) Treatment options for recurrent glioblastoma: pitfalls and future trends. Expert Rev Anticancer Ther 9(5):613–619
Wong ET, Hess KR, Gleason MJ, Jaeckle KA, Kyritsis AP, Prados MD, Levin VA, Yung WKJ (1999) Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. Clin Oncol 17(8):2572–2578
Gilbert MR, Wang M, Aldape KD, Stupp R, Hegi ME, Jaeckle KA et al (2013) Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol 31(32):4085–91
Wang J, Hu G, Quan X (2019) Analysis of the factors affect¬ing the prognosis of glioma patients. Open Med (Wars) 14:331–335
Reifenberger G, Weber RG, Riehmer V et al (2014) German Glioma Network. Molecular characterization of long-term survivors of glioblastoma using genome- and transcriptome-wide profiling. Int J Cancer 135:1822–1831
Hartmann C, Hentschel B, Simon M et al (2013) German Glioma Network. Long-term survival in primary glioblastoma with versus without isocitrate dehydrogenase mutations. Clin Cancer Res 19:5146–5157
Hau P, Koch D, Hundsberger T, Marg E, Bauer B, Rudolph R et al (2007) Safety and feasibility of long-term temozolomide treatment in patients with high-grade glioma. Neurology 68:688–690
Poelen J, Prick MJ, Jeuken JW, Wesseling P, Bernsen HJ (2009) Sixyear survival after prolonged temozolomide treatment in a 30-year-old patient with glioblastoma. Acta Neurol Belg 109:238–242
Hart MG, Grant R, Garside R, Rogers G, Somerville M, Stein K (2013) Temozolomide for high grade glioma. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007415.pub2
Ziobro M, Rolski J, Grela-Wojewoda A, Zygulska A, Niemiec M (2008) Effects of palliative treatment with temozolomide in patients with high-grade gliomas. Neurol Neurochir Pol 42:210
Keime-Guibert F, Chinot O, Taillandier L, Cartalat-Carel S, Frenay M, Kantor G et al (2007) Radiotherapy for glioblastoma in the elderly. N Engl J Med 356(15):1527–35
Weller M, Tabatabai G, Kastner B et al (2015) MGMT promoter methylation is a strong prognostic biomarker for benefit from dose-intensified temozolomide rechallenge in progressive glioblastoma:the DIRECTOR Trial. Clin Cancer Res 21:2057–2064
Wick W, Puduvalli VK, Chamberlain MC et al (2010) Phase III study of enzastaurin compared with lomustine in the treatment of recurrent intracranial glioblastoma. J Clin Oncol 28:1168–1174
Jungk C, Chatziaslanidou D, Ahmadi R et al (2016) Chemotherapy with BCNU in recurrent glioma: analysis of clinical outcome and side effects in chemotherapy-naïve patients. BMC Cancer 16:81
Carvalho BF, Fernandes AC, Almeida DS et al (2015) Second-line chemotherapy in recurrent glioblastoma: a 2-cohort study. Oncol Res Treat 38:348–354
Schmidt F, Fischer J, Herrlinger U, Dietz K, Dichgans J, Weller M (2006) PCV chemotherapy for recurrent glioblastoma. Neurology 66:587–589
Silvani A, Gaviani P, Lamperti E et al (2011) Lecture: fotemustine in brain tumors. Neurol Sci 2 Suppl2:S255-7
Preusser M, de Ribaupierre S, Wohrer A et al (2011) Current concepts and management of glioblastoma. Ann Neurol 70:9–21
Guyotat J, Signorelli F, Frappaz D, Madarassy G, Ricci AC, Bret P (2000) Is reoperation for recurrence of glioblastoma justified? Oncol Rep 7(4):899–904
McNamara MG, Lwin Z, Jiang H, Templeton AJ, Zadeh G, Bernstein M, Chung C, Millar BA, Laperriere N, Mason WP (2014) Factors impacting survival following second surgery in patients with glioblastoma in the temozolomide treatment era, incorporating neutrophil/lymphocyte ratio and time to first progression. J Neurooncol 17(1):147–152
Acknowledgements
The authors thank Tania Merlino for English proof correction.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Mario Lecce, Luca Prosperini, Dario Benincasa, Antonio Tanzilli, Stefano Telera, Alessia Farneti, and Laura Marucci. The first draft of the manuscript: Veronica Villani and Andrea Pace and all authors commented on previous versions of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The local Ethics Committee approved the study in 19/10/2021—N. 1608/21.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Villani, V., Prosperini, L., Lecce, M. et al. Recurrent glioblastoma: which treatment? A real-world study from the Neuro-oncology Unit “Regina Elena” National Cancer Institute. Neurol Sci 43, 5533–5541 (2022). https://doi.org/10.1007/s10072-022-06172-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06172-y