Abstract
Background and Purpose
The benefit of mechanical thrombectomy (MT) in patients with acute ischemic stroke (AIS) due to large vessel occlusion (LVO) and baseline mild neurological symptoms remains unclear. The purpose of this study was to evaluate the effectiveness of MT in this subgroup of patients.
Methods
The databases of 9 high-volume Italian stroke centers were retrospectively screened for patients with LVO in the anterior circulation and a baseline National Institute of Health Stroke Scale (NIHSS) score ≤ 5 that received either immediate MT or best medical management (BMM) with the possibility of rescue MT upon neurological worsening. Primary outcome measure was a modified Rankin Scale score of 0–1 at 90 days. Propensity score matching (PSM) analysis was used to estimate the treatment effect of immediate MT compared to BMM/rescue MT.
Results
Two hundred and seventy-two patients received immediate MT (MT group). The BMM/rescue MT group included 41 patients. The primary outcome was achieved in 78.6% (n = 246) of overall patients, with a higher proportion in the MT group (80.5% vs. 65.9%, p = 0.03) in unadjusted analysis. After PSM, patients in the MT group had a 19.5% higher chance of excellent outcome at 90 days compared to the BMM/Rescue MT group with a similar risk of death from any cause.
Conclusions
Our experience is in favor of a potential benefit of MT also in patients with LVO and a NIHSS score ≤ 5 at the time of groin puncture. Nonetheless, this issue waits for a clear-cut recommendation in a dedicated clinical trial.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Results from randomized trials have shown the superiority of mechanical thrombectomy (MT) over best medical therapy (including intravenous thrombolysis (IVT)) in patients with acute ischemic stroke (AIS) due to large vessel occlusion (LVO) [1,2,3,4,5,6]. Current guidelines recommend MT in patients with a baseline National Institute of Health Stroke Scale (NIHSS) score ≥ 6 and a pre-event modified Rankin Scale (mRS) score < 2, within 6 h from onset of symptoms and between 6 and 24 h from onset in patients that meet advanced neuroimaging criteria [7]. On the contrary, the benefit of MT in patients with AIS due to LVO in the anterior circulation and mild neurological symptoms at presentation (NIHSS score ≤ 5) remains unclear [8,9,10,11]. Indeed, few patients with minor stroke were included in the pivotal clinical trials to draw conclusions in this specific subgroup [12] and decision to treat is usually considered on a case-by-case basis and after careful evaluation of risks and benefits. The matter of endovascular treatment in patients with AIS due to LVO in the anterior circulation and mild neurological symptoms is of particular interest, as they constitute a variable, but not negligible, percentage of total patients [8,9,10,11, 13]. As these patients have higher odds of not receiving MT, they possibly face later neurological worsening that can limit the benefit of any subsequent recanalization treatment and lead to poor long-term functional outcome [11, 13,14,15,16].
Given the uneven evidence available to date, the guidelines of the European Stroke Organization (ESO), as well as those of the Italian Stroke Association (ISA), suggest the inclusion of patients with LVO-related stroke and a baseline NIHSS score ≤ 5 in dedicated randomized clinical trials aimed to compare the efficacy of MT plus best medical therapy versus best medical therapy alone. When this is not possible, MT is considered reasonable in patients with potentially disabling symptoms (e.g., significant motor deficits, aphasia, or hemianopia) or in case of clinical deterioration after IVT [17, 18].
Here we report a retrospective multicenter analysis of prospectively collected data on patients with AIS due to LVO in the anterior circulation and low baseline NIHSS score. The purpose of this study was to compare the outcome of patients receiving MT with a NIHSS score ≤ 5 at the time of groin puncture with the outcome of patients that, according to the current ESO and ISA guidelines, are kept on best medical management (BMM) only or are subjected to MT upon neurological worsening (with NIHSS score ≥ 6 at the time of groin puncture) after BMM (including IVT).
Methods
Patients and treatment
In this retrospective observational study, the prospective databases of 9 high-volume Italian stroke centers were screened for consecutive patients with AIS due to LVO diagnosed between January 2016 and December 2020. This work is part of a nonprofit study protocol approved by the ethics committee (protocol number 6410/20, ID 3004) of the coordinator hospital. The local ethics committees approved the use of patients’ data for this analysis. The need of an informed consent was waived due to the retrospective nature of the study.
All patients were diagnosed with a comprehensive head and neck computed tomography (CT) protocol that included a basal scan with determination of the Alberta Stroke Program Early CT (ASPECT) score [19], followed by multiphase CT angiography (mCTA) to define the site of occlusion and evaluate the leptomeningeal collateral vessel filling status using the Menon score [20]. A CT perfusion (CTP) protocol was performed in patients admitted beyond 6 h from onset of symptoms to establish eligibility to MT [7]. Patients with an occlusion site other than the middle cerebral artery (MCA) or tandem occlusion (M1 or M2 segments of the MCA and internal carotid artery (ICA)), a NIHSS score at presentation ≥ 6, a pre-event mRS score > 1 or with incomplete records were excluded.
Patients enrolled according to these criteria were then divided into two cohorts based on the therapeutic approach that was used. Patients receiving MT with a NIHSS score ≤ 5 at the time of groin puncture, either preceded or not by IVT at the discretion of the treating physician, were defined as the MT group. The control group (defined as the BMM/rescue MT group) included patients that underwent only BMM (including IVT when applicable) and those initially receiving BMM but that were subjected to rescue MT upon early neurological deterioration (END), defined as an increase of NIHSS score of ≥ 4 points from baseline leading to a NIHSS score ≥ 6 at the time of groin puncture. The decision to perform MT with a NIHSS score ≤ 5 at the time of groin puncture or BMM with the possibility of rescue MT upon END was based on individual center’s protocol and the treating physician discretion. A flow diagram of patient selection is provided in Fig. 1.
In all participating centers, the endovascular procedure was performed under general anesthesia or conscious sedation. Due to the sparse and often contradictory evidence available [21, 22], there was no preference concerning the anesthesiologic approach and decision was made on a case-by-case basis after evaluation of the patient’s capability to cooperate or other specific factors (e.g., vomiting). MT was conducted with a stent-retriever and proximal guide catheter aspiration, direct contact aspiration, or a combination of stent-retriever and distal aspiration. The treatment strategy was at the discretion of each individual interventionalist. Flow restoration at the end of each procedure was graded using the modified Treatment In Cerebral Infarction (mTICI) scale [23] with successful MT corresponding to a score of 2b-3. Two experienced neuroradiologists blinded to clinical outcome reviewed the diagnostic radiological data and angiographic data of all patients.
Clinical variables and measures of outcome
Our analysis included demographic data (age and sex), cardiovascular risk factors, previous antithrombotic therapy, and imaging data as well as therapeutic procedures of the acute phase. Clinical outcome was measured with the mRS score acquired at 90 days through a structural interview, either in person or on the telephone. A mRS score of 0–1 (excellent functional outcome) at 90 days was chosen as the primary clinical outcome measure. This was considered more appropriate given the baseline condition of patients, characterized by mild symptoms. Secondary clinical outcome measure was a mRS score of 0–2 (functional independence) at 90 days. Safety outcome measures were (1) brain bleeding events following recanalization therapies, assessed by CT scan or magnetic resonance imaging at 72 h and classified according to previously established criteria [24] and (2) death of any cause within 90 days after stroke.
Statistical analysis
Standard descriptive statistics were used to measure central tendency and variability of baseline characteristics. We examined differences in means of ordinal and continuous variables by the Mann–Whitney U test or Welch two-sample t-test based on their distribution. Categorical variables were compared through the chi-squared test.
Since our data were not randomized, we used propensity score matching (PSM) to estimate the treatment effect of MT compared to the BMM/rescue MT, accounting for differences in baseline variables. We estimated the probability of being treated (propensity score) by a multivariable logistic regression model where the outcome variable is a binary variable indicating the treatment type. Covariates included in this model were sex, age, occlusion site at mCTA, baseline NIHSS, and IVT. Using this model, we calculated the propensity score for each patient. We examined the region of common support through histograms of the estimated propensity scores by treatment type. We used the “nearest neighbor” method to find pairs of observations that have very similar propensity scores, but that differ in the type of received treatment. We assessed the covariate imbalance through (1) Welch two-sample t-test and (2) visual inspection of the mean of each covariate (estimated through a locally estimated scatterplot smoothing) against the estimated propensity score, separately by type of treatment. The treatment effect was calculated through linear regression and presented as a risk difference with 95% CI [25]. Statistical significance was considered at 2-tailed p-value < 0.05. All analyses were performed using R software v.4.0.5 (https://www.r-project.org).
Results
A total of 5210 patients with AIS due to LVO from the 9 participating centers were screened. After exclusion of patients with an occlusion site other than the MCA (M1 or M2 segment) and tandem occlusion (cervical ICA and MCA), a NIHSS score at presentation > 5 or a pre-event mRS score > 1, 313 patients were available for analysis. Of these, 272 patients (139 females—51.1%) received MT when having a NIHSS score ≤ 5 at the time of groin puncture (MT group) (Fig. 1). The BMM/rescue MT group included 41 patients (24 females—58.5%) that received only BMM (16 patients—39.1%) or that initially received BMM but that underwent rescue MT upon END with a NIHSS score ≥ 6 at the time of groin puncture (25 patients—60.9%). The two cohorts had similar demographics, baseline clinical characteristics, and vascular risk factors except for diabetes that was more frequent in the BMM/rescue MT group (17.1% in the BMM/rescue MT group vs. 7.7% in the MT group; p-value = 0.05). IVT was performed in 109 patients of the MT group (40.1%), in 14 patients receiving BMM only, and in 16 of the patients subjected to rescue MT (corresponding to 73.2% of total control patients, p < 0.001). The BMM/rescue MT group had a higher proportion of tandem occlusions and M2 occlusions (22% vs. 11.5% and 51.2% vs. 43.8%, respectively), whereas M1 occlusions were more frequent in the MT group (44.9% vs. 26.9%). Median Menon score (interquartile range) was 4 (4–5) in both groups, meaning good collaterality. Successful recanalization (mTICI score 2b-3) was achieved in 87.1% of patients of the MT group and in 88% of the patients subjected to rescue MT (p = 0.9). All relevant data of the patients included in this study are reported in Table 1.
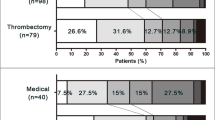
Ninety-day excellent outcome (mRS 0–1) was achieved in 78.6% (n = 246) of patients overall, with a higher proportion in the MT group in unadjusted analysis (80.5% vs. 65.9%, p = 0.03; Table 2 and Fig. 2). Dichotomization of the mRS score of 0–2 (functional independence) versus 3–6 (poor outcome) showed no significant difference between the MT group and the BMM/rescue MT group (86.8% vs. 80.5% respectively, p = 0.28). There was a non-significant difference in all-cause mortality at 90 days between the 2 groups (Table 2).
All main analysis patients (n = 313) entered the propensity score matching procedure, and 41 matched pairs (total number of patients = 82) of early MT and BMM/rescue MT patients were generated based on similar baseline covariates (Supplementary material). After PSM, early MT was associated with a 19.5% (95% CI: 0.9–38.1%, p = 0.04) higher chance of excellent outcome (mRS of 0–1) at 90 days compared to BMM/Rescue MT. Chances of good neurological outcome (mRS of 0–2) and death of any cause at 90 days were similar between the two groups (9.8% difference for mRS of 0–2 in favor of the MT group, 95% CI: − 5.6–25%, p = 0.22; 2.4% difference for death of any cause in favor of the MT group, 95% CI: − 2.4–7.3%, p = 0.32).
Discussion
Our multicenter retrospective observational study shows a greater benefit of MT in patients with anterior circulation LVO and a NIHSS score ≤ 5 at the time of groin puncture compared to an approach based on BMM with the possibility of a rescue MT after neurological deterioration. This finding is best shown by PSM analysis demonstrating that early MT is associated with a 19.5% higher probability of achieving an excellent long-term neurological outcome. Our results are in line with the evidence that MT has a beneficial effect on clinical outcome across the entire baseline NIHSS severity range [12].
The appropriateness of MT in patients with AIS due to LVO and a low NIHSS score at presentation is currently debated and awaits clarification. The limited number of randomized patients with a low baseline NIHSS score in the main MT trials has hampered the possibility of addressing this issue [12]. Skepticism may arise from the risks of an invasive procedure not counterbalanced by the possible benefits in patients with a so-called minor stroke. However, the definition “minor stroke” may be misleading if simply based on a NIHSS score cutoff value without considering the type of symptoms (disabling or nondisabling) and the association or not with a long-term favorable outcome [26]. Following this consideration, setting a NIHSS score threshold for MT eligibility may appear arbitrary.
To date, a growing body of evidence is available on MT in patients with LVO and a low baseline NIHSS score. In real-world practice, such option is usually considered on a case-by-case basis, after careful evaluation of clinical and radiological features and assessment of risks and benefits. However, the fact that in our retrospective analysis the number of patients receiving MT with a NIHSS score ≤ 5 at the time of groin puncture largely exceeds that of the BMM/rescue MT group reveals a current tendency towards early MT, likely due to the increasing familiarity of neurointerventionists with the procedure and the better safety profile of the last generation thrombectomy devices [27]. This consideration, along with recent data showing overall a noninferiority of MT alone compared to IVT followed by MT [28, 29], possibly explains also the lower percentage of patients receiving IVT in the MT group compared to the BMM/rescue MT group.
The critical point in the management of patients with LVO and a low NIHSS score not subjected to an effective recanalization therapy is the possibility of neurological deterioration upon failure of the leptomeningeal collateral network that sustains the initial paucity of symptoms. Indeed, in a recent single-center retrospective study, an unfavorable clinical evolution was documented in a fifth of patients with stroke due to LVO and mild symptoms and could not be predicted on the base of the studied clinical and radiological variables [11]. Hence, the need to define the most effective treatment strategy in this type of AIS patients has become impelling. The initial exploratory reports that have suggested the benefit of MT when performed before neurological deterioration [9, 15, 30] are in line with our results. Conversely, a recent multicenter retrospective study has failed to demonstrate significant differences in terms of functional outcome between MT and best medical therapy (including IVT) in patients with a baseline NIHSS score ≤ 5, regardless the site of occlusion (internal carotid artery and M1 segment vs. M2 segment) and degree of stroke severity at admission (NIHSS score of 0–3 vs. 4–5) [10].
Other retrospective reports that used a PSM analysis have also led to uneven conclusions. In the study by Nagel and coworkers, that included also patients with posterior circulation LVO, MT in patients with baseline NIHSS score ≤ 5 resulted in a higher rate of patients with functional independence (mRS score of 0–2) at 90 days compared to patients initially undergoing BMM and eventually receiving MT upon neurological worsening, with no relevant issues regarding safety [16]. In another retrospective observational study, intended bridging therapy with IVT followed by MT was not superior in terms of clinical outcome compared to IVT alone and was associated with higher odds of both symptomatic and asymptomatic intracranial bleeding events. However, when the study population was analyzed based on the site of occlusion, bridging therapy resulted in significantly higher rates of excellent neurological outcome in patients with proximal occlusion (ICA and MCA/M1 segment) compared to IVT alone [31]. Dargazanli and coworkers have shown that patients with anterior circulation LVO and minor-to-mild symptoms (baseline NIHSS score < 8) have an excellent outcome after MT more often than those left on BMM, despite an increase rate of brain bleeding events [32]. On the other hand, a more recent multicenter study by Volny and coworkers, that included patients with occlusion of ICA and/or MCA (M1 and proximal M2 segments), has shown that MT was associated with a 8.6% higher chance of excellent outcome but with a 22.3% higher risk of neurological deterioration at 24 h and a 2.2% higher risk of death of any cause within 90 days [33].
Because of this ambiguous scenario, to date, it is reasonable to consider MT in patients with a NIHSS score ≤ 5 but with disabling symptoms, using specific care to keep hemorrhagic rates below those reported in randomized clinical trials, as suggested by the Standards and Guidelines Committee of the Society of NeuroInterventional Surgery [34].
The main limitations of our study derive from its observational design. A significant bias may arise from the diverse therapeutic conduct across the different centers, as treatment decisions were made upon the discretion of the managing physicians and outside the more rigid criteria of a clinical trial. In addition, patients subjected to early MT were confronted with a control group that included patients left on BMM only and patients that were initially medically managed but later underwent rescue MT upon worsening of clinical condition. Although this reflects current real-world practice, from an experimental standpoint, the merger of the two subgroups of control patients into one may raise concerns about homogeneity of treatment. Furthermore, our propensity score analysis used a series of covariates that we believe are more important as predictors of long-term clinical outcome, but it is possible that other relevant factors may have not been considered or measured. Nonetheless, while our results must be interpreted with caution, the scenario emerging from this retrospective study indicates a definite tendency toward early MT, with encouraging results when this type of approach is compared to a “wait-and-see” approach that uses BMM as first option and eventually considers the possibility of rescue MT upon neurological worsening.
In consideration of the sparse evidence available to date, it is expected that forthcoming randomized controlled trails will clarify whether early MT is beneficial in patients with LVO and a low baseline NIHSS score.
Conclusions
The efficacy of MT in patients with AIS due to LVO and low NIHSS score at presentation has been insufficiently studied in the main randomized clinical trials. Our study is in favor of a potential benefit of early MT also in this category of patients. Nonetheless, this issue remains open for clarification and the need for an unambiguous recommendation in clinical practice is urgent.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372(1):11–20. https://doi.org/10.1056/NEJMoa1411587
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372(11):1009–1018. https://doi.org/10.1056/NEJMoa1414792
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372(11):1019–1030. https://doi.org/10.1056/NEJMoa1414905
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372(24):2296–2306. https://doi.org/10.1056/NEJMoa1503780
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372(24):2285–2295. https://doi.org/10.1056/NEJMoa1415061
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T et al (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15(11):1138–1147. https://doi.org/10.1016/S1474-4422(16)30177-6
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50(12):e344–e418. https://doi.org/10.1161/STR.0000000000000211
Kim JT, Heo SH, Yoon W, Choi KH, Park MS, Saver JL et al (2016) Clinical outcomes of patients with acute minor stroke receiving rescue IA therapy following early neurological deterioration. J Neurointerv Surg 8(5):461–465. https://doi.org/10.1136/neurintsurg-2015-011690
Pfaff J, Herweh C, Pham M, Schonenberger S, Nagel S, Ringleb PA et al (2016) Mechanical thrombectomy in patients with acute ischemic stroke and lower NIHSS Scores: recanalization rates, periprocedural complications, and clinical outcome. Am J Neuroradiol 37(11):2066–2071. https://doi.org/10.3174/ajnr.A4862
Goyal N, Tsivgoulis G, Malhotra K, Ishfaq MF, Pandhi A, Frohler MT et al (2020) Medical management vs mechanical thrombectomy for mild strokes: an international multicenter study and systematic review and meta-analysis. JAMA Neurol 77(1):16–24. https://doi.org/10.1001/jamaneurol.2019.3112
Saleem Y, Nogueira RG, Rodrigues GM, Kim S, Sharashidze V, Frankel M et al (2020) Acute neurological deterioration in large vessel occlusions and mild symptoms managed medically. Stroke 51(5):1428–1434. https://doi.org/10.1161/STROKEAHA.119.027011
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387(10029):1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Heldner MR, Jung S, Zubler C, Mordasini P, Weck A, Mono ML et al (2015) Outcome of patients with occlusions of the internal carotid artery or the main stem of the middle cerebral artery with NIHSS score of less than 5: comparison between thrombolysed and non-thrombolysed patients. J Neurol Neurosurg Psychiatry 86(7):755–760. https://doi.org/10.1136/jnnp-2014-308401
Mokin M, Masud MW, Dumont TM, Ahmad G, Kass-Hout T, Snyder KV et al (2014) Outcomes in patients with acute ischemic stroke from proximal intracranial vessel occlusion and NIHSS score below 8. J Neurointerv Surg 6(6):413–417. https://doi.org/10.1136/neurintsurg-2013-010720
Messer MP, Schonenberger S, Mohlenbruch MA, Pfaff J, Herweh C, Ringleb PA et al (2017) Minor stroke syndromes in large-vessel occlusions: mechanical thrombectomy or thrombolysis only? Am J Neuroradiol 38(6):1177–1179. https://doi.org/10.3174/ajnr.A5164
Nagel S, Bouslama M, Krause LU, Kupper C, Messer M, Petersen M et al (2018) Mechanical thrombectomy in patients with milder strokes and large vessel occlusions. Stroke 49(10):2391–2397. https://doi.org/10.1161/STROKEAHA.118.021106
Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M et al (2019) European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischaemic Stroke. Endorsed by Stroke Alliance for Europe (SAFE). Eur Stroke J 4(1):6–12. https://doi.org/10.1177/2396987319832140
Italian Stroke Association - Stroke Prevention and Education Awareness (2020) Guidelines for Revascularization Therapies. Available from: https://www.iso-stroke.it/wp-content/uploads/2020/10/linee_guida_terapie_rivascolarizzazione.pdf. Accessed 5 Nov 2021
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 355(9216):1670–1674. https://doi.org/10.1016/s0140-6736(00)02237-6
Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM et al (2015) Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology 275(2):510–520. https://doi.org/10.1148/radiol.15142256
Ilyas A, Chen CJ, Ding D, Foreman PM, Buell TJ, Ironside N et al (2018) Endovascular mechanical thrombectomy for acute ischemic stroke under general anesthesia versus conscious sedation: a systematic review and meta-analysis. World Neurosurg 112:e355–e367. https://doi.org/10.1016/j.wneu.2018.01.049
Zhang Y, Jia L, Fang F, Ma L, Cai B, Faramand A (2019) General anesthesia versus conscious sedation for intracranial mechanical thrombectomy: a systematic review and meta-analysis of randomized clinical trials. J Am Heart Assoc 8(12):e011754. https://doi.org/10.1161/JAHA.118.011754
Gerber JC, Miaux YJ, von Kummer R (2015) Scoring flow restoration in cerebral angiograms after endovascular revascularization in acute ischemic stroke patients. Neuroradiology 57(3):227–240. https://doi.org/10.1007/s00234-014-1460-x
von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD et al (2015) The Heidelberg Bleeding Classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46(10):2981–2986. https://doi.org/10.1161/STROKEAHA.115.010049
Gomila R (2021) Logistic or linear? Estimating causal effects of experimental treatments on binary outcomes using regression analysis. J Exp Psychol Gen 150(4):700–709. https://doi.org/10.1037/xge0000920
Fischer U, Baumgartner A, Arnold M, Nedeltchev K, Gralla J, De Marchis GM et al (2010) What is a minor stroke? Stroke 41(4):661–666. https://doi.org/10.1161/STROKEAHA.109.572883
Salsano G, Pracucci G, Mavilio N, Saia V, BdP M, Malfatto L et al (2021) Complications of mechanical thrombectomy for acute ischemic stroke: incidence, risk factors, and clinical relevance in the Italian Registry of Endovascular Treatment in acute stroke. Int J Stroke 16(7):818–827. https://doi.org/10.1177/1747493020976681
Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W et al (2020) Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med 382(21):1981–1993. https://doi.org/10.1056/NEJMoa2001123
Kandregula S, Savardekar AR, Sharma P, McLarty J, Kosty J, Trosclair K et al (2021) Direct thrombectomy versus bridging thrombolysis with mechanical thrombectomy in middle cerebral artery stroke: a real-world analysis through National Inpatient Sample data. Neurosurg Focus 51(1):E4. https://doi.org/10.3171/2021.4.FOCUS21132
Haussen DC, Bouslama M, Grossberg JA, Anderson A, Belagage S, Frankel M et al (2017) Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: an intention-to-treat analysis. J Neurointerv Surg 9(10):917–921. https://doi.org/10.1136/neurintsurg-2016-012633
Seners P, Perrin C, Lapergue B, Henon H, Debiais S, Sablot D et al (2020) Bridging therapy or IV thrombolysis in minor stroke with large vessel occlusion. Ann Neurol 88(1):160–169. https://doi.org/10.1002/ana.25756
Dargazanli C, Arquizan C, Gory B, Consoli A, Labreuche J, Redjem H et al (2017) Mechanical thrombectomy for minor and mild stroke patients harboring large vessel occlusion in the anterior circulation: a multicenter cohort study. Stroke 48(12):3274–3281. https://doi.org/10.1161/STROKEAHA.117.018113
Volny O, Zerna C, Tomek A, Bar M, Rocek M, Padr R et al (2020) Thrombectomy vs medical management in low NIHSS acute anterior circulation stroke. Neurology 95(24):e3364–e3372. https://doi.org/10.1212/WNL.0000000000010955
Mokin M, Ansari SA, McTaggart RA, Bulsara KR, Goyal M, Chen M et al (2019) Indications for thrombectomy in acute ischemic stroke from emergent large vessel occlusion (ELVO): report of the SNIS Standards and Guidelines Committee. J Neurointerv Surg 11(3):215–220. https://doi.org/10.1136/neurintsurg-2018-014640
Author information
Authors and Affiliations
Contributions
Conceptualization: Andrea Alexandre, Iacopo Valente, Giacomo Della Marca, and Aldobrando Broccolini; Methodology: Andrea Alexandre, Iacopo Valente, and Aldobrando Broccolini; Formal analysis and investigation: Andrea Alexandre, Iacopo Valente, Alessandro Pedicelli, Angelo Maria Pezzullo, Francesca Colò, Luca Scarcia, Andrea Romi, Mariangela Piano, Antonio Macera, Joseph Domenico Gabrieli, Giacomo Cester, Antonio Armando Caragliano, Sergio Lucio Vinci, Maria Ruggiero, Christian Commodaro, Andrea Saletti, Guido Andrea Lazzarotti, Mirco Cosottini, Valerio Da Ros, Luigi Bellini, Emilio Lozupone, Adriana Paladini, Valerio Brunetti, Roberta Morosetti, Giovanni Frisullo, Giacomo Della Marca, and Aldobrando Broccolini; Writing—original draft preparation: Andrea Alexandre, Iacopo Valente, Paolo Calabresi, Giacomo Della Marca, and Aldobrando Broccolini; Writing—review and editing: Andrea Alexandre, Iacopo Valente, and Aldobrando Broccolini.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study fully adheres to the ethical principles of the Declaration of Helsinki as well as GCP guidelines. Approval was granted by the Ethics Committee of the Fondazione Policlinico Universitario A. Gemelli IRCCS (protocol number 6410/20, ID 3004).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Rights and permissions
About this article
Cite this article
Alexandre, A.M., Valente, I., Pedicelli, A. et al. Mechanical thrombectomy in acute ischemic stroke due to large vessel occlusion in the anterior circulation and low baseline National Institute of Health Stroke Scale score: a multicenter retrospective matched analysis. Neurol Sci 43, 3105–3112 (2022). https://doi.org/10.1007/s10072-021-05771-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05771-5