Abstract
Endovascular revascularization techniques are increasingly used to treat arterial occlusions in patients with acute ischemic stroke. To monitor and communicate treatment results, a valid, reproducible, and clinically relevant, yet easy to use grading scheme of arterial recanalization and tissue reperfusion for digital subtraction angiography is needed. An ideal scoring system would consider the target arterial lesion, the perfusion deficit, and the collateral status before treatment and measure recanalization, reperfusion, early venous shunting, vasospasm, as well as distal embolization after flow restoration. Currently, a variety of different flow restoration scales are in use, including the Thrombolysis in Myocardial Infarction scoring system, the Thrombolysis in Cerebral Infarction score, and the Arterial Occlusive Lesion score, which describe the local recanalization result. These scores are not used homogeneously throughout the literature, are often modified and not fully documented, which make them inept to compare treatment effects across studies. In addition, none of these scores cover all of the above-mentioned aspects, nor are they able to describe satisfactorily all relevant angiographic findings, and data on their reliability and predictive power regarding clinical outcome are sparse. We aimed to review and illustrate the different revascularization scales, discuss their advantages and limitations as well as the available data regarding standardization, reliability testing, and outcome prediction. In addition, we give examples for the use of the scales and show potential pitfalls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endovascular revascularization techniques are increasingly used to treat arterial occlusions in patients with acute ischemic stroke. Based on the recanalization hypothesis [1], the goal of endovascular therapy for acute stroke is to restore the patency of the occluded cerebral artery (local recanalization) and the downstream arterial blood flow (global reperfusion) to salvage ischemic but still viable brain tissue, prevent neuronal cell death, and enable functional recovery [2, 3].
To monitor and communicate treatment results, a standardized reporting system of arterial recanalization and tissue reperfusion for digital subtraction angiography is needed. An ideal scoring system would be highly reliable, easy to use, and clinically relevant by predicting outcome, and it would cover all of the following angiographic criteria: the target arterial lesion, the perfusion deficit, and the collateral status before treatment as well as the degree of recanalization, reperfusion, early venous shunting, vasospasm, and distal embolization after flow restoration [3–5]. However, it has been acknowledged that one single score cannot consider all of these aspects reflecting the complexity in flow restoration after endovascular therapy [2, 6, 7]. To date, the most helpful concept seems to differentiate between recanalization and reperfusion [2]. This may be clinically important since recanalization of the primary arterial occlusive lesion does not necessarily imply reperfusion of the dependent territory and lack of recanalization does not always mean absence of reperfusion altogether [2, 3, 8]. Additionally, drugs, devices, or combinations of it may differ in their ability to achieve and maintain recanalization and reperfusion [2, 8, 9]. Unfortunately, there is great variability in the literature regarding the assessment and documentation of flow restoration [10]. The most widely used grading scores include the Thrombolysis in Myocardial Infarction (TIMI) scoring system, the Thrombolysis in Cerebral Infarction (TICI) score, which represents an adoption of the TIMI score for the cerebral vasculature and is regarded as a global measure of post-treatment reperfusion, and finally the Arterial Occlusive Lesion (AOL) score, which describes the local recanalization result. In addition, the Qureshi scale [11] is often discussed as a potentially alternative scoring system. As a major drawback, these scores are not used homogeneously throughout the literature, are often modified, and not fully documented. The terms recanalization and reperfusion are frequently used interchangeably, although they refer to different concepts, which complicates the comparison of endovascular stroke therapies [2]. Even the three recently published randomized trials of endovascular therapy for acute ischemic stroke, IMS 3 [12], MR-Rescue [13], and SYNTHESIS, [14] scored flow restoration differently: IMS 3 used AOL [recanalization] and TICI [reperfusion]; MR-Rescue rated angiographic revascularization with TICI and reperfusion was assessed with CT- and MR-Perfusion; in SYNTHESIS, recanalization was not systematically reported. In addition, none of the scores is able to describe satisfactorily all potentially relevant angiographic findings and data on their reliability and predictive power regarding clinical outcome is sparse.
We aimed to review and illustrate the different revascularization scales and discuss their advantages and limitations as well as the available data regarding standardization, reliability testing, and outcome prediction.
Scales of flow restoration
Historical aspects
A revascularization scale for the cerebral vasculature was first published in 1988. A pilot study of intra-arterial thrombolysis for acute ischemic stroke by del Zoppo et al. differentiated between “no,” “partial,” and “complete recanalization of the previously occluded carotid territory brain-supplying artery” [15] (Table 1). Simultaneously, Mori et al. reported a method for scoring recanalization in angiography after intracarotid urokinase treatment as detailed in Table 1 [16], and which they refined in 1992 [17] (Table 1). In 2002, another scale has been introduced by Qureshi et al. [11]. This eightfold grading scheme allocates a score from 0 to 5 based on the site of occlusion and the degree of perfusion either antegrade or retrograde by collateral supply to the effected territory. Grade 0 is no occlusion with full perfusion; grade 5 is occlusion of either the internal carotid artery without collateral flow in case of anterior circulation stroke or complete basilar artery occlusion in vertebrobasilar stroke.
The Thrombolysis in Myocardial Infarction (TIMI) score and its modifications
The TIMI score was initially developed in 1985 to report different degrees and the dynamics of reperfusion of the coronary bed following thrombolytic therapy [18]. Grade 0 meant no perfusion, grade 1 contrast penetration through the obstruction but without perfusion, grade 2 described partial perfusion, and grade 3 stood for complete and timely perfusion (Table 1).
Randomized trials of intra-arterial thrombolytic therapy (PROACT-I, PROACT-II) [19, 20] and the Emergency Management of Stroke (EMS) trial [21] applied the TIMI scale to assess cerebrovascular recanalization (Table 1). Clinical relevance of the TIMI score used in the cerebral vasculature could be shown in the pooled MERCI trials and the SWIFT study [22, 23], where increasing TIMI scores were associated with improved clinical outcome.
As a score primarily developed to evaluate reperfusion of the coronary arteries, TIMI and its adoptions do not take into account specific features of the cerebral vasculature. Thus, the Stroke Therapy Academic Industry Roundtable (STAIR) has recommended to abandon it in future clinical stroke trials [6]. However, recently published thrombectomy trials still used the TIMI score as a measure for the primary study endpoint [23].
The Thrombolysis in Cerebral Infarction (TICI) score and its modifications
To take into account some of the specific requirements of intracranial revascularization procedures, the American Society of Interventional and Therapeutic Neuroradiology and the Society of Interventional Radiology (ASITN/SIR) proposed the TICI scale [24] (Table 2). The essential change as compared to the TIMI score consisted in the introduction of a subdivision of the TIMI grade 2 score (partial reperfusion) into a new TICI 2a and TICI 2b score [24] (Table 2). The initially proposed TICI 2a score indicates partial reperfusion with filling of less than 2/3 of the dependent vascular territory, while TICI 2b refers to partial reperfusion with a filling of more than 2/3 up to the complete dependent vascular territory but with a flow slower than normal [24]. The differentiation of TICI 2b and 3 being rather based on flow dynamics than vascular territorial anatomy made the scale prone to ambiguity. Already in 1992, Mori et al. had pointed out that partial reperfusion with delayed flow was less frequent compared to the more frequent branch recanalization with normal flow in the dependent sub-territory [17], a finding insufficiently covered by the initial TICI grading system [4, 10].
The original TICI scale underwent several modifications (Table 2). In 2005, the Interventional Management of Stroke (IMS) study group proposed to reserve the term recanalization for the restoration of flow at the arterial occlusive lesion (AOL) and the term reperfusion for restoration of flow to the respective terminal branches and capillary bed [2]. Based on this concept, they suggested applying the TICI score for the evaluation of the reperfusion of the dependent vascular territory only, while they introduced a separate score for rating the local recanalization success at the target artery, the so-called AOL score (see below and Table 3). In 2007, the IMS group simplified the TICI subcategories 2a and 2b, by reducing the dynamic quality of the TICI scale. According to this adaptation, the category TICI 2a should be used to indicate partial reperfusion of ≤50 % of the territory of the affected middle cerebral artery (MCA), while TICI 2b describes partial reperfusion of >50 % of the vessel territory [25] (Table 2).
Some authors added a grade 2c [26, 27], differentially defining this as “near complete perfusion without clearly visible thrombus but with delay in contrast run-off” [26] or “near complete perfusion except for slow flow or distal emboli in a few distal cortical vessels” [27]. The grade 2c subdivision has not reached consensus status yet.
The consensus Treatment in Cerebral Ischemia (mTICI) score
Recently, an interdisciplinary task force published consensus recommendations on angiographic revascularization grading standards for acute ischemic stroke [28] and suggested the modified TICI grading system (mTICI) where TICI stands for Treatment In Cerebral Ischemia [28]. The mTICI scale has the same subdivisions as the original TICI scale (Table 2) but eliminates the dynamic assessment (slow or normal flow) beyond grade 1 completely and substantiates that only antegrade flow but not retrograde collateral flow is assessed and contributes to a better score. The consensus mTICI grading scale will be used throughout the paper.
Recanalization score (AOL)
Recanalization at the target arterial lesion after therapy should be described using the AOL recanalization score [2, 28]. The fourfold AOL score rates the degree of occlusion (complete or incomplete) and local recanalization (partial or complete) with no or any distal flow. Grade 0 corresponds to complete occlusion of the target artery while grade 3 is complete recanalization with any distal flow (Table 3).
Arterial patency at the site of occlusion might also be scored on baseline pre-intervention angiograms using AOL, based on the degree of luminal opening.
Practical recommendations for the interpretation and scoring of angiograms regarding flow restoration
General recommendations
The primary or “target arterial occlusive lesion” (TAL) should be defined on the pre-therapeutic angiogram using common terminology for the vessel segments [29]. In case of serial vessel occlusions, so-called tandem occlusions, the most proximal intracranial lesion would be indexed as TAL [28].
The vascular bed of the affected artery has to be examined for potentially persistent antegrade perfusion (Table 2) and collateral blood flow. If this is not visible in the angiogram of the ipsilateral supra-aortic vessel, another (e.g., the contralateral) vessel has to be examined or CT or MR angiography has to be screened for potential collateral contributions.
To allow correct determination of the site of the arterial lesion and to assess the recanalization result and reperfusion to the dependent territory, we recommend to evaluate the last post-intervention angiogram available first and to compare it to the pre-therapeutic angiogram. The angiograms in two planes should be acquired with the tip of the diagnostic catheter in a proximal, preferably extracranial vessel segment to assess perfusion independently of contrast injection pressure. Angiographic runs through a distal access catheter harbored in the proximal M1 segment are not advisable as the contrast is forced into the vessels downstream and might mimic a better reperfusion result than truly achieved. Furthermore, distal microcatheter injections carry the risk of subsequent parenchymal hemorrhage [30] or acute vessel perforation [31].
Interpretation of the post-interventional angiograms with regard to AOL and mTICI
When assessing AOL and mTICI on the post-interventional angiograms the following possible combinations of AOL and mTICI scores might occur:
-
AOL 0 can only result in mTICI 0, i.e., “no perfusion” [28]. By definition, collateral retrograde flow does not alter mTICI grade, as mTICI only rates antegrade perfusion past the target lesion. Thus, if the angiogram shows varying degrees of collateral retrograde perfusion provided via pial collaterals originating from the territory of the anterior (ACA) or posterior cerebral arteries (PCA) in the case of a (persisting) MCA occlusion, this would have no impact on the mTICI score (see Fig. 1 for an example of AOL 0, mTICI 0, i.e., no perfusion past the occlusion but full collateral coverage of the dependent vascular territory).
Fig. 1 Collaterals in acute and chronic MCA occlusion—maturing collaterals with change of collateral flow grade. a, b A 61-year-old man with an acute stroke. Baseline angiogram of early arterial phase (a, AP view) and parenchymal phase (b, lateral view). Thrombosed left MCA in distal M1 segment and also left A2 occlusion. Presence of collateral circulation: collateral flow grade 3, as both the ACA and MCA territory are collateralized, slowly but fully, via the posterior circulation. Initially, there was no antegrade flow beyond the point of occlusion: mTICI 0. No improvement was seen after the intervention (images not shown). c, d Some months later, the patient came back with an occlusion of the distal contralateral (right) M1 segment which could partly be recanalized (mTICI 2b). The follow-up CT showed infarction in the right MCA territory and only deep white matter lesions on the left side (not shown). The angiograms of the left ICA at the time of the second (contralateral) intervention revealed complete and minimally delayed collateral perfusion of the left ACA and MCA territories (early arterial phase [c, AP view] and parenchymal phase [d, lateral view). The left MCA and ACA are still occluded in the primary location. But now, a collateral flow grade of 4 could be assigned to the left ACA and MCA territories
-
AOL 1 always corresponds to mTICI 0, as AOL 1 implicates “no distal flow.”
-
AOL 2 recanalization can result in different degrees of reperfusion, and therefore in any score from mTICI 1 to 3 (see Fig. 2 as an example for AOL 2 recanalization with mTICI 2b reperfusion).
Fig. 2 Incomplete recanalization (AOL 2) and reperfusion, mTICI 2b. AP angiogram of a 90-year-old woman at baseline (a) Thrombosed right proximal MCA with no antegrade flow beyond the point of occlusion: mTICI 0. Small arterial branches (recurrent artery of Heubner and anterior choroidal artery) not arising from the MCA superimposing on the MCA territory which could be taken erroneously as antegrade persistent flow in the MCA. Panel b shows recanalization of the MCA trunk, but with an underlying residual stenosis (e.g., arteriosclerosis or vasospasm) or residual thrombus (AOL 2). Re-established flow can be seen in all the distal MCA branches. Lateral angiogram (c) shows distal filling of the MCA branches, with minimal perfusion deficit in the dorsal insula and frontal operculum: mTICI 2b. The CT acquired 24 h later (not shown) proved the good recanalization/reperfusion result with only a small putaminal infarction which is typical in proximal M1 occlusions
-
Likewise AOL 3 can produce any degree of reperfusion from mTICI 1 to mTICI 3, as complete recanalization does not imply complete reperfusion.
How to discriminate between the different mTICI reperfusion grades?
-
Slow filling in a few distal branches beyond the primary occlusion with some parenchymal staining (minimal reperfusion) corresponds to mTICI 1 (Table 2, Fig. 3).
Fig. 3 Incidental filling of the contralateral MCA. Lateral angiogram of an 82-year-old man with a thrombosed left MCA at baseline. On some frames (a), there is contrast filling in the MCA territory. In fact it corresponds to incidental contrast filling of the contralateral MCA as shown in AP view (b). It is mandatory to analyze the vascular bed of all branches of the affected artery on at least two planes for the assessment of mTICI. Note the thrombi in the pericallosal artery (arrow in a) and the partially perfused distal M1 with mTICI 1 perfusion (arrow in b)
-
Re-established reperfusion in less than half of the entire vascular territory distal to the primary arterial lesion corresponds to mTICI 2a, reperfusion in half or greater corresponds to 2b (Table 2). Scoring does not depend on the number of recanalized M2 segments but by definition on the amount of reperfused vessel territory. In Fig. 4, multiple M2 segments are recanalized proximally, but they fail to reperfuse the dependent brain tissue due to numerous distal embolizations (DE), representing only mTICI 2a reperfusion. However, a more common observation in recanalizations of M1 occlusions is that filling of just one M2 segment leads to mTICI 2a reperfusion, whereas flow in at least two M2 segments results in mTICI 2b reperfusion (Fig. 2).
Fig. 4 Complete recanalization of target arterial occlusive lesion but incomplete reperfusion. a AP angiogram at baseline of a 74-year-old man with a thrombosed right MCA and ACA (the temporal branch of the right MCA is still perfused). There is no antegrade flow beyond the point of occlusion in the distal M1 segment and the proximal A1 segment: AOL 0, mTICI 0. b AP and c lateral angiograms after mechanical thrombectomy: complete recanalization of the M1 segment (AOL 3), but only partial filling of the vascular territory of the MCA (<1/2): mTICI 2a (c). The occlusion of the pericallosal artery persisted as it was not selectively treated. The magnitude of the perfusion deficit is more apparent in a late venous phase on lateral view (d). There is contrast stagnation in at least five MCA branches (M2 and M3 segments, arrows) and the pericallosal artery (arrow head) due to primary occlusion or distal embolization (DE). The initial occlusion pattern points to a probable fragmentation of the thrombus at the level of the carotid terminus with fragments obstructing the MCA and the ACA
-
In case of filling of all of the expected segments of the recanalized artery, the capillary bed should be searched for small perfusion defects which would correspond to mTICI 2b (see Fig. 2). And very often, the observer will find small occluded branches in the periphery of the target territory. Thus, mTICI 3 reperfusion results which would require complete reperfuion with “absence of visualized occlusion in all distal branches” are rather the exception and will often turn out to be mTICI 2b when re-assessed.
-
If there is complete filling of all of the expected vascular territory with normal contrast filling into the capillary phase and without distal embolization, this would correspond to mTICI 3 (Fig. 5).
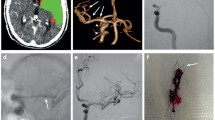
Fig. 5 Complete recanalization (AOL 3) and complete reperfusion (mTICI 3). A 56-year-old man with an acute stroke due to occlusion of the right ICA at the origin (not shown) and arterioarterial embolization into the MCA. Angiogram after emergency stenting of the extracranial ICA before the intracranial intervention: AP (a) view shows distal occlusion of the right MCA (mTICI 0). The anterior temporal artery, arising from the M1 segment proximal to the thrombus, and the lenticulostriate arteries are still patent. AP angiogram after intervention: complete recanalization, AOL 3 (b), and reperfusion, mTICI 3, with filling of all distal branches (c)
Potential pitfalls in the interpretation of angiogramms
To unambiguously classify mTICI, the observer should analyze the vascular bed of all branches of the primarily affected artery on at least two planes. This avoids misinterpretation due to the following pitfalls:
-
A branch arising from a vessel not related to the thrombosed artery (i.e., the TAL) might be superimposed to the site of occlusion and thus be taken erroneously as persistent flow beyond the occlusion (Fig. 6). This is less a problem when looking at the dynamic angiographic run but more so when only examining distinct time points of the whole image series.
Fig. 6 Superimposition of small arterial branches on the thrombosed segment. a Potential pitfall: a small arterial branch superimposes on the thrombosed left MCA and could be mistaken for residual flow past the thrombus (and scored erroneously as mTICI 1 or 2a). A different angulation (b) reveals the complete occlusion of the left middle cerebral artery trunk (mTICI 0, arrow in (b)) in this angiogram of a 37-year-old man with acute stroke
-
An arterial branch arising from the thrombosed artery proximally to the occlusion (for example the anterior temporal branch arising closely proximal to the thrombus in an occluded MCA) should not be taken for persistent flow beyond the occlusion (Fig. 7).
Fig. 7 Possible misinterpretation due to a patent proximal MCA branch. Baseline AP angiogram of a 56-year-old man. An arterial branch, the anterior temporal artery, arising from the M1 segment proximally to the thrombus should not be taken erroneously as persistent flow beyond the point of occlusion in the distal M1 segment (a). The thrombosed right MCA trunk is clearly visible in (b): mTICI 0
-
Filling of the contralateral MCA might be falsely judged as persistent flow in the vascular bed of the thrombosed artery when assessing the lateral view only (Fig. 3).
-
Once filling of the contralateral MCA is excluded, perfusion of the distal bed of the target MCA is best evaluated in the lateral view because arterial branches originating from the posterior circulation (contrasted via the posterior communicating artery [PCOM]) may be falsely interpreted as contributing to the MCA territory on AP view (Fig. 2).
-
Synchronous perfusion of both the ACA and MCA territories in a typical post-interventional angiogram of the ICA (Fig. 2c) might mimic a better reperfusion result than with the ipsilateral ACA territory not contrasted in parallel. Exclusive contrast in the MCA territory would help to define its true extent. Figure 8 shows an angiogram of an ICA exclusively contrasting the MCA (and PCOM) due to hypogenesis of the ipsilateral A1 segment and timely wash-out by competing inflow from the anterior communicating artery (ACOM).
Fig. 8 Incomplete reperfusion mTICI 2b. In this 57-year-old man, the occlusion of the left terminal ICA (a, lateral view) was caused by arterioarterial embolization due to an ipsilateral ulcerated stenosis of the extracranial ICA (not shown). After the intervention (b), there is good reperfusion beyond the area of initial obstruction: AOL 3 for the terminal ICA segment, but incomplete filling of the MCA territory with the artery of the angular gyrus (A. gyri angularis) still occluded (arrow in b): mTICI 2b (reperfusion in more than 1/2 of the MCA territory). The left A1 segment is rudimentary and not significantly contributing to the perfusion of the left ACA territory (not shown). Without superimposition of the ACA territory, the true extent of the MCA territory is clearly visible. Eight days after the intervention, the patient received carotid artery stenting (CAS). In the meantime, perfusion of the MCA territory had spontaneously improved (c), even the artery of the angular gyrus is now completely reperfused (arrow in c), and the margins of the MCA territory are well delineated, corresponding to the CT scan which only showed a small opercular infarction
Scoring in case of tandem occlusions
Tandem occlusions may require subsequent interventions at two or more different sites. A typical example is the combined intracranial ICA/MCA/ACA occlusion (Fig. 9). We suggest to separately assessing AOL for each arterial site and treatment approach in order to describe the individual treatment effect. Reperfusion (mTICI) is rated relative to the downstream territory depending on the initial most proximally treated intracranial occlusive lesion. The examples are as follows:
The different stages of recanalization. Baseline angiogram (a) of a 68-year-old woman depicts a right terminal ICA occlusion. Angiograms during and after the intervention (b–d) show the various stages of endovascular recanalization. After first aspiration, there is some penetration with minimal perfusion beyond the obstruction (b): AOL 1 at the level of the terminal segment of the right ICA. In c, the ICA and the ACA are now open (AOL 3 at the level of the terminal ICA and the ACA) and stay open till the end of the procedure. There is only AOL 1 recanalization in the MCA bifurcation. The occlusion is resolved to regain full perfusion (AOL 3, mTICI 3—as established in a larger biplane angiogram, not shown) after the last aspiration (d). In a, contrast filling of the right posterior cerebral artery can be seen via the posterior communicating artery which should not be misinterpreted as patent right MCA branches (when in doubt consult the lateral view)
-
Recanalization of the intracranial ICA, but persistent occlusion of the (non-collateralized) ACA and MCA: AOL[ICA] 3, AOL[MCA] 0, AOL[ACA] 0; mTICI: 0.
-
Recanalization of the ICA, recanalization of the ACA, but persistent (partial-) occlusion of the MCA: AOL[ICA] 3, AOL[MCA] 0 or 1, AOL[ACA] 3; mTICI 2a (for the whole of the ICA territory: ACA plus MCA) (Fig. 9c).
-
Recanalization of ICA, MCA, and ACA: AOL[ICA] 3, AOL[MCA] 3, AOL[ACA] 3; mTICI is likely to be 2a, 2b, or 3 depending on the reperfusion in MCA and ACA territory (Fig. 9d).
In patients with an intracranial ICA occlusion, the exclusion of additional ACA or PCA occlusions may require angiography of the contralateral ICA and of the posterior circulation in order to differentiate between thrombo-embolic occlusions and anatomical variants, to define the exact type of the terminal carotid occlusion (T, L, or I type, see next paragraph), and to assess potential pial collateral contribution to the affected vascular territories.
The PCA is supplied by the basilar artery in the majority of patients and should be normally perfused in ICA occlusions, but could equally be occluded if directly originating from the ICA (fetal origin). With an ACOM present, the A1 and M1 segments ipsilateral to the side of a terminal ICA occlusion may show flow with full perfusion of both the MCA and ACA territory (so-called carotid I occlusion). The L occlusion is encountered if the ipsilateral A1 and A2 segments are contrasted via the ACOM, with only the carotid terminus and the MCA occluded. A true carotid T occlusion is present if the carotid terminus and both the ipsilateral M1 and A1 segments are occluded [32].
Scoring in case of periprocedural embolization to new territory versus distal embolization
In the process of recanalization, clot material can be lost from the thrombectomy device and instead of being cleared from the vasculature may occlude previously perfused arteries. Embolization to new territory (ENT) is defined as any treatment-related embolus outside of the target territory. Distal embolization (DE) is defined as any treatment-related embolus within the target territory [23, 28, 33]. An example of ENT is given in Fig. 10. In case of ENT, the mTICI reperfusion grade is not altered as mTICI is rated relative to the initial primary arterial occlusion [28]. In contrast, distal embolization will influence the final mTICI reperfusion grade if it leads to a substantial perfusion deficit [28]. For example in a terminal ICA occlusion, a treatment-related ACA embolus would represent an embolization to new territory if the ipsilateral ACA was patent and received antegrade flow from the contralateral ICA on the pre-intervention angiography. The same embolus would lead to a distal embolization if no such ACA flow had been present at baseline [28].
Embolization to new territory. Baseline angiogram (right ICA) of a 66-year-old woman with acute occlusion of the right MCA in lateral view (a). After one pass of a stent-like retriever, there is restored flow in the MCA but occlusion of the pericallosal artery (arrow in b) which was initially patent (a); there is also tapering of the callosomarginal artery. The occurrence of the pericallosal occlusion right after passage of the retriever is consistent with an embolization to new territory (ENT)
Don’t forget the veins!
Angiographic demonstration of peri-ischemic early venous filling (due to arterio-venous shunting and sometimes described as “luxury perfusion”) may indicate vasoparalysis and irreversible brain tissue damage with subsequent infarction despite successful recanalization [34] and may be a predictive sign for parenchymal hematoma [35]. Direct arterio-venous shunting can be observed in a majority of patients who are treated with endovascular technique for acute stroke [34]. A close observation of the venous phase in the final angiogram after recanalization may therefore allow some predictions on subsequent infarction. There may be (a) timely and synchronous opacification of the venous outflow of all territories, (b) early filling of the veins and venous sinuses, or (c) no venous filling despite successful arterial recanalization. Both of the latter findings can indicate infarction and might present as early venous drainage of the basal ganglia in anterior circulation stroke (Fig. 11) or as a lack of timely filling of the superior sagittal sinus, indicating large brain infarction despite successful recanalization of the middle cerebral artery. The lack of the capillary phase with no transit of contrast to the venous side is called the “no-reflow” phenomenon [8, 36, 37] indicating microvascular compromise as it may result from distal emboli blocking the capillary bed [38] (Fig. 12). Unfortunately, none of the existing scoring systems takes these venous phenomena into account.
Arterio-venous shunting in the basal ganglia turning into infarction. The angiogram (AP view) of a 69-year-old man with right distal MCA occlusion shows early venous drainage of the basal ganglia into the deep veins (internal vein, straight sinus). In the subsequent CT, the right basal ganglia turned out to be infarcted (not shown)
No reflow phenomenon, foreshadowing a large infarction. The right terminal ICA is occluded in this 61-year-old man (a) (early venous filling is apparent in the straight sinus, presumably via the basal ganglia which receive anterior choroidal artery perfusion). After thrombus aspiration, the ICA, MCA, and ACA were fully recanalized (b) and perfusion seemed to be reestablished. But in the parenchymal phase, no contrast could be seen in the MCA territory. And during the venous phase, the superior sagittal sinus and the sulcal veins draining the MCA territory are completely missing (c) (the residual parenchymal staining and remaining veins projecting onto the superior frontal and parietal lobe originate from the partially perfused ACA territory as verified in AP view). This picture is consistent with a “no-reflow” phenomenon. The initial CT already showed complete lack of collaterals in the ACA and MCA territories (not shown). Follow-up CT after 24 h confirms complete infarction of the MCA and ACA territories (d)
Reliability and prognostic value of flow restoration scoring scales
Reliability is fundamental for the use of any scoring scale. Data on inter- and intra-observer variability in assessing flow restoration using TICI is inconsistent throughout the literature: while some authors describe it as poor [39], others found fair to moderate [40] or even good inter- and intra-observer variability [41]. Inter-observer agreement seems to improve substantially when TICI is dichotomized into success (TICI 2b, 3) or failure (TICI 0–2a) [40]. The differential performance of the scores in the anterior versus the posterior circulation has not been evaluated.
With regard to prognostic power, the mTICI scale seems to be superior to both the original TICI and the TIMI scale in predicting good functional outcome after successful reperfusion [41, 42]. In addition, it could be shown that mTICI grades 2b and 3 are best suited to predict global procedural success and consequently should be the targeted end point of intra-arterial therapy (IAT) [42].
Based on these findings and in order to overcome the cacophony in reporting recanalization, expert groups recommended abandoning the many variants of TIMI in favor of AOL and mTICI to score local recanalization (AOL) and antegrade reperfusion (mTICI) in a standardized manner [6, 28].
Limitations of the scoring systems and open questions
Even if the recommended scores, namely AOL and mTICI, are applied correctly, there remain certain imprecisions regarding the classification of reperfusion in ICA and MCA occlusions. For example, the extent of the TAL in ICA terminus occlusion might result in three AOL grades, for the ICA, the MCA, and the ACA, but only in one mTICI score. In some cases, the target downstream territory might not be clearly identifed as collateralization obscures its true extent. Thus, rating it with the mTICI scale might be challenging. There is consensus that “Future studies must clarify the optimal definition of the target downstream territory for each level of vessel occlusion” [28].
Another drawback of the available scores seems to be the limited correlation between successful reperfusion and good clinical outcome. In trials of IAT for acute ischemic stroke, reperfusion rates regularly surpass rates of good clinical outcome [38, 43], and reported recanalization rates are typically higher compared to intra-venous thrombolysis (IVT) [1]. However, if in IAT recanalization is forced “at all cost” with no time limits, it is obvious that there may be seemingly perfect but clinically futile recanalizations [38]. Futility of an intervention can only be determined retrospectively. Futile recanalizations with seemingly good reperfusion might not be perfectly detected by the mTICI score, thus leaving room for improvement in grading treatment success.
Is it justified to use TIMI or mTICI in the posterior cerebral circulation?
The TIMI classification has been previously used [44, 45] and was consistently reported in a systematic review regarding intra-arterial revascularization in the posterior circulation [46]. Reperfusion was not addressed. We could not find a report on reliability testing for TIMI in the posterior circulation in an extensive literature search. The mTICI scale is neither well documented nor used in posterior circulation revascularization grading. The AOL grading system is useful in the posterior circulation and has been used in randomized trials [12].
Is it justified to apply mTICI to Computed Tomography Angiography (CTA) or MR Angiography (MRA)?
In some clinical stroke trials, recanalization and reperfusion in MRA and CTA have been assessed by a modified TIMI scale, but the same inconsistencies and validation problems as in angiographic studies have been encountered [8]. We do not recommend to apply mTICI to CTA or MRA as long as both modalities do not routinely provide dynamic and directional blood flow information to answer the basic question if antegrade flow is present [47].
Conclusion
Standardized recanalization and reperfusion grading scales for digital subtraction angiography are needed to communicate baseline findings and results of flow restoration in endovascular treatment of acute ischemic stroke patients. Progress has been made in assessing reliability and prognostic power of the available scales. If applied consistently as recommended, the current form of the recanalization (AOL) and reperfusion (mTICI) grading scales will hopefully serve as a common denominator in anterior circulation acute stroke studies. The evolutionary process might be jeopardized by trying to introduce a whole new score which again has to go through the evaluation process as did TIMI and TICI. We can conclude with Gaha et al. [29] that there is no use to propose just another score but to evaluate and evolve the ones which are most frequently used. However, it remains unclear which grading scale might be reliably implemented for the vertebrobasilar territory.
References
Rha J-H, Saver JL (2007) The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38:967–973. doi:10.1161/01.STR.0000258112.14918.24
Khatri P, Neff J, Broderick JP et al (2005) Revascularization end points in stroke interventional trials: recanalization versus reperfusion in IMS-I. Stroke 36:2400–2403. doi:10.1161/01.STR.0000185698.45720.58
Tomsick T (2007) TIMI, TIBI, TICI: I came, I saw, I got confused. AJNR Am J Neuroradiol 28:382–384
Kallmes DF (2012) TICI: if you are not confused, then you are not paying attention. AJNR Am J Neuroradiol 33:975–976. doi:10.3174/ajnr.A2905
Zaidat OO, Lazzaro MA, Liebeskind DS et al (2012) Revascularization grading in endovascular acute ischemic stroke therapy. Neurology 79:S110–S116. doi:10.1212/WNL.0b013e3182695916
Saver JL, Albers GW, Dunn B et al (2009) Stroke Therapy Academic Industry Roundtable (STAIR) recommendations for extended window acute stroke therapy trials. Stroke 40:2594–2600. doi:10.1161/STROKEAHA.109.552554
Saver JL, Liebeskind DS, Nogueira RG, Jahan R (2010) Need to clarify Thrombolysis In Myocardial Ischemia (TIMI) scale scoring method in the penumbra pivotal stroke trial. Stroke 41:e115–e116. doi:10.1161/STROKEAHA.109.566406
Soares BP, Chien JD, Wintermark M (2009) MR and CT monitoring of recanalization, reperfusion, and penumbra salvage: everything that recanalizes does not necessarily reperfuse! Stroke 40:S24–S27. doi:10.1161/STROKEAHA.108.526814
Chueh JY, Wakhloo AK, Hendricks GH et al (2011) Mechanical characterization of thromboemboli in acute ischemic stroke and laboratory embolus analogs. AJNR Am J Neuroradiol 32:1237–1244. doi:10.3174/ajnr.A2485
Fugate JE, Klunder AM, Kallmes DF (2013) What is meant by “TICI”? AJNR Am J Neuroradiol 34:1792–1797. doi:10.3174/ajnr.A3496
Qureshi AI (2002) New grading system for angiographic evaluation of arterial occlusions and recanalization response to intra-arterial thrombolysis in acute ischemic stroke. Neurosurgery 50:1405–1414, discussion 1414–5
Broderick JP, Palesch YY, Demchuk AM et al (2013) Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 368:893–903. doi:10.1056/NEJMoa1214300
Kidwell CS, Jahan R, Gornbein J et al (2013) A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 368:914–923. doi:10.1056/NEJMoa1212793
Ciccone A, Valvassori L, Nichelatti M et al (2013) Endovascular treatment for acute ischemic stroke. N Engl J Med 368:904–913. doi:10.1056/NEJMoa1213701
Del Zoppo GJ, Ferbert A, Otis S et al (1988) Local intra-arterial fibrinolytic therapy in acute carotid territory stroke. A pilot study. Stroke 19:307–313. doi:10.1161/01.STR.19.3.307
Mori E, Tabuchi M, Yoshida T, Yamadori A (1988) Intracarotid urokinase with thromboembolic occlusion of the middle cerebral artery. Stroke 19:802–812
Mori E, Yoneda Y, Tabuchi M et al (1992) Intravenous recombinant tissue plasminogen activator in acute carotid artery territory stroke. Neurology 42:976–982
The TIMI Study Group (1985) The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group. N Engl J Med 312:932–936
Del Zoppo GJ, Higashida RT, Furlan AJ et al (1998) PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators. Prolyse in Acute Cerebral Thromboembolism. Stroke 29:4–11
Furlan A, Higashida R, Wechsler L et al (1999) Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 282:2003–2011
Lewandowski CA, Frankel M, Tomsick TA et al (1999) Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) Bridging Trial. Stroke 30:2598–2605. doi:10.1161/01.STR.30.12.2598
Fields JD, Lutsep HL, Smith WS (2011) Higher degrees of recanalization after mechanical thrombectomy for acute stroke are associated with improved outcome and decreased mortality: pooled analysis of the MERCI and Multi MERCI trials. AJNR Am J Neuroradiol 32:2170–2174. doi:10.3174/ajnr.A2709
Saver JL, Jahan R, Levy EI et al (2012) Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 380:1241–1249. doi:10.1016/S0140-6736(12)61384-1
Higashida RT, Furlan AJ, Roberts H et al (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34:e109–e137. doi:10.1161/01.STR.0000082721.62796.09
IMS II Trial Investigators (2007) The Interventional Management of Stroke (IMS) II Study. Stroke 38:2127–35. doi:10.1161/STROKEAHA.107.483131
Noser EA, Shaltoni HM, Hall CE et al (2005) Aggressive mechanical clot disruption: a safe adjunct to thrombolytic therapy in acute stroke? Stroke 36:292–296. doi:10.1161/01.STR.0000152331.93770.18
Almekhlafi MA, Mishra S, Desai JA et al (2014) Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv Neuroradiol 20:21–27
Zaidat OO, Yoo AJ, Khatri P et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. doi:10.1161/STROKEAHA.113.001972
Türe U, Yaşargil MG, Al-Mefty O, Yaşargil DC (2000) Arteries of the insula. J Neurosurg 92:676–687. doi:10.3171/jns.2000.92.4.0676
Khatri P, Broderick JP, Khoury JC et al (2008) Microcatheter contrast injections during intra-arterial thrombolysis may increase intracranial hemorrhage risk. Stroke 39:3283–3287. doi:10.1161/STROKEAHA.108.522904
Hui FK, Yim J, Spiotta AM et al (2012) Intermediate catheter injections in closed segments during acute stroke intervention: a cautionary note. J Neurointerv Surg 4:e39. doi:10.1136/neurintsurg-2011-010163
Liebeskind DS, Flint AC, Budzik RF et al (2014) Carotid I’s, L’s and T’s: collaterals shape the outcome of intracranial carotid occlusion in acute ischemic stroke. J Neurointerv Surg. doi:10.1136/neurintsurg-2014-011231
Nogueira RG, Lutsep HL, Gupta R et al (2012) Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet 380:1231–1240. doi:10.1016/S0140-6736(12)61299-9
Dorn F, Kuntze-Soderqvist A, Popp S et al (2012) Early venous drainage after successful endovascular recanalization in ischemic stroke—a predictor for final infarct volume? Neuroradiology 54:745–751. doi:10.1007/s00234-011-0966-8
Ohta H, Nakano S, Yokogami K et al (2004) Appearance of early venous filling during intra-arterial reperfusion therapy for acute middle cerebral artery occlusion: a predictive sign for hemorrhagic complications. Stroke 35:893–898. doi:10.1161/01.STR.0000119751.92640.7F
Ames A, Wright RL, Kowada M et al (1968) Cerebral ischemia. II. The no-reflow phenomenon. Am J Pathol 52:437–453
Soares BP, Tong E, Hom J et al (2010) Reperfusion is a more accurate predictor of follow-up infarct volume than recanalization: a proof of concept using CT in acute ischemic stroke patients. Stroke 41:e34–e40. doi:10.1161/STROKEAHA.109.568766
Hussein HM, Georgiadis AL, Vazquez G et al (2010) Occurrence and predictors of futile recanalization following endovascular treatment among patients with acute ischemic stroke: a multicenter study. AJNR Am J Neuroradiol 31:454–458. doi:10.3174/ajnr.A2006
Bar M, Mikulik R, Jonszta T et al (2012) Diagnosis of recanalization of the intracranial artery has poor inter-rater reliability. AJNR Am J Neuroradiol 33:972–974. doi:10.3174/ajnr.A2896
Gaha M, Roy C, Estrade L et al (2014) Inter- and intraobserver agreement in scoring angiographic results of intra-arterial stroke therapy. AJNR Am J Neuroradiol. doi:10.3174/ajnr.A3828
Suh SH, Cloft HJ, Fugate JE et al (2013) Clarifying differences among thrombolysis in cerebral infarction scale variants: is the artery half open or half closed? Stroke 44:1166–1168. doi:10.1161/STROKEAHA.111.000399
Yoo AJ, Simonsen CZ, Prabhakaran S et al (2013) Refining angiographic biomarkers of revascularization: improving outcome prediction after intra-arterial therapy. Stroke 44:2509–2512. doi:10.1161/STROKEAHA.113.001990
Molina CA (2010) Futile recanalization in mechanical embolectomy trials: a call to improve selection of patients for revascularization. Stroke 41:842–843. doi:10.1161/STROKEAHA.110.580266
Arnold M, Nedeltchev K, Schroth G et al (2004) Clinical and radiological predictors of recanalisation and outcome of 40 patients with acute basilar artery occlusion treated with intra-arterial thrombolysis. J Neurol Neurosurg Psychiatry 75:857–862
Schonewille WJ, Wijman CAC, Michel P et al (2009) Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol 8:724–730. doi:10.1016/S1474-4422(09)70173-5
Lindsberg PJ, Mattle HP (2006) Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke 37:922–928. doi:10.1161/01.STR.0000202582.29510.6b
Frölich AMJ, Psychogios MN, Klotz E et al (2012) Antegrade flow across incomplete vessel occlusions can be distinguished from retrograde collateral flow using 4-dimensional computed tomographic angiography. Stroke 43:2974–2979. doi:10.1161/STROKEAHA.112.668889
Ethical standards and patient consent
We declare that all human studies have been approved by our institutional Ethics Committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Due to the retrospective nature of this anonymized patient image and data study, patient consent was waived.
Conflict of interest
JG received personal fees and non-financial support from Penumbra Inc., non-financial support from Covidien and MicroVention Deutschland GmbH and personal fees from DePuy Codman and J&J Medical GmbH, all unrelated to the submitted work. YIM received personal fees from Synarc during the study. RVK received personal fees from Synarc, Lundbeck, Penumbra and Covidien, all unrelated to the submitted work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gerber, J.C., Miaux, Y.J. & von Kummer, R. Scoring flow restoration in cerebral angiograms after endovascular revascularization in acute ischemic stroke patients. Neuroradiology 57, 227–240 (2015). https://doi.org/10.1007/s00234-014-1460-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1460-x