Abstract
Alzheimer’s disease (AD) is the most common form of dementia characterized by the prevalent memory impairment. Mild cognitive impairment (MCI) may represent the early stage of AD, in particular when MCI patients show biomarkers consistent with AD pathology (MCI due to AD). Neuropsychiatric symptoms (NPS) frequently affect both MCI and AD patients. Cerebrospinal-fluid (CSF) tau and β-amyloid42 (Aβ42) levels are actually considered the most sensitive and specific biomarkers for AD neurodegeneration. In the present retrospective observational study, we evaluated CSF biomarkers and neuropsychological data (also including NPS measured by the neuropsychiatric inventory—NPI) in a population of patients affected by MCI due to AD compared with mild to moderate AD patients. We documented higher NPI scores in MCI compared with AD patients. In particular, sub-items related to sleep, appetite, irritability, depression, and anxiety were higher in MCI than AD. We also found the significant correlation between NPS and CSF AD biomarkers in the whole population of MCI and AD patients. Consistently, t-tau/Aβ42 ratio correlated with NPS in all the MCI and AD patients. These results suggest the more prevalent occurrence of NPS in MCI patients showing AD pathology and converting to dementia than AD patients. Moreover, a more significant degree of AD neurodegeneration, featured by high t-tau/Aβ42 ratio, correlated with more severe NPS, thus supposing that in MCI and AD patients a more extensive AD neurodegeneration is related to more severe behavioral disturbances.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most common cause of dementia. It is characterized by a progressive deterioration of cognition, frequently associated with neuropsychiatric symptoms (NPS) [1,2,3]. Both β-amyloid and tau pathologies occur in AD neurodegeneration. Accordingly, the AD neuropathological changes include the cerebral deposition of both β-amyloid plaques and tau-related neurofibrillary tangles (NFT). Corresponding to the neuropathological changes occurring in AD brain, on the one hand low levels of cerebrospinal fluid (CSF) β-amyloid42 (Aβ42) are present in AD patients and associated with β-amyloid plaques deposit in the whole brain [4]; on the other hand, tau pathology producing neuronal and axonal degeneration in selected brain areas of AD patients (such as limbic, temporal, and frontal regions [5]) is associated with increased levels of CSF total (t-tau) and phosphorylated tau (p-tau) proteins [6]. These CSF biomarkers (Aβ42, t-tau and p-tau) are useful not only in supporting AD diagnosis, but also in predicting the conversion of mild cognitive impairment (MCI) to AD dementia [7,8,9,10].
NPS are frequently observed in both MCI and AD patients [11]. Apathy, depression, agitation, irritability, and sleep disturbances are frequent NPS in MCI and AD patients, further affecting cognition and daytime functioning [12]. Moreover, NPS may also represent early non-cognitive manifestations of AD neurodegeneration [13, 14] and have been associated with altered CSF biomarkers in both MCI and AD patients [15,16,17]. It has been supposed that higher t-tau and p-tau CSF levels correlated with apathy in mild AD patients [15], whereas CSF AD biomarkers changes have been associated with anxiety, agitation, and irritability in MCI patients [16, 17]. However, there is paucity of studies measuring NPS by using the NPI, which is a validated questionnaire to quantify these disabling symptoms in MCI and AD patients. Moreover, MCI populations frequently included non-converter patients, since the diagnosis of MCI was not validated by AD biomarkers. Although previous reports tried to quantify the occurrence of NPS in both MCI and AD patients, no study compared NPS, measured by using the neuropsychiatric inventory (NPI), in patients affected by MCI due to AD to patients affected by mild to moderate AD patients. Therefore, in this retrospective observational study we aimed at measuring NPS by using the NPI in patients affected MCI due to AD compared with patients affected by mild to moderate AD. Furthermore, this study would verify whether CSF AD biomarkers correlate to NPS in the population of patients included in this study (MCI due to AD and mild to moderate AD).
Methods
Subjects
This is a retrospective observational study including drug-naïve MCI due to AD patients (Mini-Mental State Examination—MMSE ≥ 24) recruited at the Neurology Clinic of the University Hospital of Rome “Tor Vergata.” The criteria used to define MCI due to AD included the following widely accepted criteria: cognitive concerns; objective evidence of cognitive impairment; normal functional activities; absence of dementia; biomarkers for AD pathology [18, 19]. Moreover, all MCI due to AD patients were followed to confirm the conversion to AD at follow-up.
Drug-naïve mild to moderate AD patients were also included. Patients received the diagnosis of AD at the Neurology Clinic of the University Hospital of Rome “Tor Vergata” and at the Department of Neurology of the Medical University of Graz. The diagnosis of AD was performed according to the recently proposed version of the diagnostic guidelines [20]. The biomarkers were considered as positive for AD when decreased CSF levels of Aβ42 and the following abnormalities were observed: medial temporal lobe atrophy on MRI, cortical temporo-parietal hypometabolism on [18F]-FDG-PET, and increased CSF levels of t-tau or p-tau [20].
All patients underwent a standard screening including history, neurological examination, laboratory tests, neuropsychological testing including MMSE, brain MRI, and lumbar puncture (LP) for CSF biomarker analysis in order to assess Aβ42, t-tau and p-tau levels.
MCI due to AD and AD patients were required to meet the following entry criteria: no concomitant neurologic or psychiatric diseases except cognitive impairment; no use of acetylcholinesterase inhibitors or other drugs active on CNS. Exclusion criteria were the following: abnormal cell count (> 4 cells/mcL) at the CSF sample analysis; major medical illness; drug/alcohol dependence and abuse; lack of a reliable caregiver; MRI evidence of parenchymal abnormalities.
The study was considered as observational by the Independent Ethical Committee of “Tor Vergata” University Hospital of Rome and performed according to the STROBE statement. Patients provided their informed consent to the study.
Neuropsychiatric and neuropsychological assessment
To obtain a global index of cognitive impairment, the MMSE was administered, with scores ranging from 30 (no impairment) to 0 (maximum impairment).
NPI was used to measure behavioral symptoms in MCI and AD patients (delusions, hallucinations, agitation/aggression, dysphoria/depression, anxiety, euphoria/elation, apathy/indifference, disinhibition, irritability/lability, aberrant motor behaviors, nighttime behavioral disturbances, and appetite/eating disturbances) [21]. The score for each dimension ranges from 0 to 12, with a maximum total score of 144 in the 12-item version.
CSF collection and analysis
CSF collection was performed as previously reported by LP performed in the decubitus position with an atraumatic needle [22]. CSF was collected in polypropylene tubes using standard sterile techniques. The first 4 ml CSF sample was used for biochemistry routine analysis. Another 4 ml CSF sample was centrifuged to eliminate cells and cellular debris, and immediately frozen at − 80 °C to measure t-tau, p-tau, and Aβ42 levels. CSF Aβ42, t-tau, and p-tau levels were determined according to previously published standard procedures, using commercially available sandwich enzyme-linked immunosorbent assays (ELISA) (Innotest β-Amyloid 1-42, Innotest h-T-tau, Innotest Phospho-T-tau 181; Innogenetics, Ghent, Belgium). The pathological cut-off level for CSF t-tau, p-tau, and Aβ42 was set at > 350 pg/ml, > 50 pg/ml, and < 500 pg/ml, respectively. The t-tau/Aβ42 ratio was also calculated, and the cut-off > 0.52 was considered to represent the CSF AD profile [9].
Data and statistical analysis
For the statistical analysis, we used a commercial software (Statistica 10.0 program; Statsoft Inc., Tulsa, OK, USA).
The Kolmogorov-Smirnov test was used to check for normal distribution of the obtained data. Student’s t test was used to compare data between MCI and AD patients. Correlations between the CSF biomarkers levels and neuropsychological data were performed by utilizing Pearson correlation test. Data were analyzed with a significant p value of 0.05 compensated by the Bonferroni correction for multiple comparisons among total scores.
Results
Demographic and clinical data of patients and controls
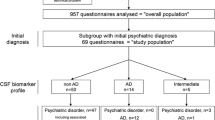
Sixty-five patients were observed in the two centers from September 2012 to May 2017 and included in this observation. On the basis of the diagnostic criteria for AD and MCI due to AD, 20 patients were included in MCI due to AD group, while 45 patients were included in AD group.
Demographic and clinical features of MCI and AD patients are summarized in Table 1.
CSF data
All MCI and AD patients showed the t-tau/Aβ42 ratio over 0.52, the cut-off validated for AD pathology diagnosis (Table 1). However, we did not find differences in CSF data between MCI due to AD and mild to moderate AD patients (Table 1).
Neuropsychological data
As expected, we documented lower MMSE scores in mild to moderate AD compared with MCI due to AD patients. NPI total score was lower in mild to moderate AD compared with MCI due to AD patients (Table 2). Considering the sub-items of the NPI, depression, anxiety, sleep, appetite, and irritability presented higher scores in the MCI due to AD group compared with mild to moderate AD group (Table 2).
Correlations between CSF AD biomarkers and neuropsychological data
Considering the correlations between NPI and CSF biomarkers in the whole group of MCI and AD patients, we found the positive correlation of t-tau/Aβ42 ratio with the sub-items of NPI related to irritability (R = 0.42, p < 0.05), sleep disturbances (R = 0.49, p < 0.005), and eating disturbances (R = 0.37, p < 0.05). Moreover, the t-tau/Aβ42 ratio correlated positively with the global NPI score (R = 0.51, p < 0.01).
Discussion
NPS occur in the majority of patients affected by MCI or AD and may negatively impact on patients’ and caregivers’ quality of life [11, 23, 24]. Consistently, NPS should be inquired and treated as necessary, since they have important implications for patients and caregivers [25].
This study investigated the occurrence of NPS in both MCI due to AD and mild to moderate AD patients. Moreover, it evaluated the possible relationships between NPS and CSF AD biomarkers in both populations of drug-naïve patients included in the study. Accordingly, in the MCI due to AD group we have exclusively included patients affected by MCI with the biomarkers’ assessment consistent with AD neurodegeneration [20]. Consistently, all MCI patients converted to AD at follow-up, thus confirming the underlying AD pathology. The main result of this study was the different prevalence of NPS in both cohorts of patients. In particular, it appeared evident that MCI patients showed higher NPI total scores than AD patients. This finding is quite novel considering the previous literature about NPS in MCI and AD patients. Moreover, we documented the association between pathological CSF AD biomarkers and NPS in MCI and AD patients. Briefly, the t-tau/Aβ42 ratio, a well validated index of neurodegeneration in patients affected by AD pathology [26], correlated with more severe NPS. The NPI was used to evaluate NPS; it is an Italian [27] and German [28] validated questionnaire widely used in MCI and AD patients to investigate the presence of NPS, such as irritability, sleep disturbances, apathy, and depression. As shown by numerous studies, the prevalence of NPS in MCI and AD patients is very high and trends to increase with the progression of cognitive impairment, thus further limiting the activity of daily living and reducing the quality of life of patients and caregivers [29]. However, we documented higher scores of the NPI sub-items related to depression, anxiety, sleep impairment, appetite dysregulation, and irritability in MCI with respect to AD patients. This finding is partially in contrast with previous observations. However, it has been already documented that NPS, and particularly depression, are frequently present in MCI patients and associated with a higher rate of progression to dementia [30,31,32]. Moreover, sleep impairment has been widely documented in MCI patients, and particularly in those showing biomarkers consistent with AD pathology [33, 34]. Hence, the higher NPI scores found in the MCI due to AD group could be related to the fact that exclusively patients showing the core features of AD pathology and the conversion to AD dementia were included in this study.
Although the importance to investigate NPS in MCI and AD patients is widely accepted, the literature studying the relationships between brain AD processes and NPS is limited. NPS have been associated with metabolic dysfunction in brain networks subserving mood and cognition [12, 13]. It has been documented that agitation is associated with greater NFT burden in the orbitofrontal cortex in AD patients, as well as apathy is related to a more marked deposition of tau proteins in the anterior cingulate cortex in AD patients [35]. Moreover, psychosis has been associated with NFT in the frontal cortex and amyloid plaques in presubiculum in AD [36]. These data were predominantly achieved in post-mortem brain studies, but less evidence is present in clinical studies. In the present report, carried out in a population of MCI due to AD and mild to moderate AD patients, we found several correlations linking CSF AD biomarkers to NPS. In particular, in patients presenting the higher t-tau/Aβ42 ratio, a marker of AD neurodegeneration, NPI showed the higher total scores. Therefore, NPS may possibly represent a marker of the more severe neurodegeneration in MCI and AD patients. In the same view, the association between NPS and CSF t-tau/ Aβ42 ratio may be related to the more significant neurodegeneration present in the frontal brain regions of AD patients [31]. In agreement with this observation, previous studies showed that focal cortical hypometabolisms in frontal areas are associated with apathy, agitation and disinhibition, and psychosis in AD patients [37]. Therefore, NPS in MCI and AD patients are related to a more significant degree of neurodegeneration. However, the lack of correlation between CSF Aβ42 levels and NPS may be explained by the fact that amyloid deposits itself diffusely in the whole brain and not in selected areas [37]. Conversely, the relationships between CSF t-tau/Aβ42 ratio and NPS may be driven by tau pathology, which is considered a strong marker of the neuronal focal injury in the AD process and can be responsible for the occurrence and persistence of neuropsychiatric and cognitive symptoms. Since the combined t-tau/Aβ42 ratio may possibly represent a more sensitive predictor of cognitive and non-cognitive outcomes [38], our hypothesis is that it may better reflect the severity of the neurodegenerative processes, which may in turn be responsible for the greater severity of NPS.
We are aware that this study has several limitations. The main limitation is the retrospective nature of the study. Moreover, the small sample of patients included and the cross-sectional analysis further limited our study. However, the strength of this study is the inclusion of MCI and AD patients showing the biomarkers consistent with AD pathology. Moreover, the AD pathology underlying MCI condition was confirmed by the follow-up showing the conversion from MCI to AD in all patients included. In conclusion, this study can represent a preliminary clinical impression about the more frequent occurrence of some NPS in MCI due to AD patients. However, the occurrence of a more severe behavioral profile in MCI than in AD patients can also represent the consequence of less awareness or reduced internally driven feeling in AD patients. Hence, further studies should be performed to better investigate behavioral disturbances in MCI and AD patients and to confirm the possible link between a more severe degree of neurodegeneration and NPS in the AD neurodegenerative process.
References
Mega MS, Cummings JL, Fiorello T, Gornbein J (1996) The spectrum of behavioral changes in AD. Neurology 46(1):130–135
Lyketsos CG, Carrillo MC, Ryan JM, Khachaturian AS, Trzepacz P, Amatniek J, Cedarbaum J, Brashear R, Miller DS (2011) Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement 7(5):532–539
Del Prete M, Spaccavento S, Craca A, Fiore P, Angelelli P (2009) Neuropsychiatric symptoms and the APOE genotype in Alzheimer’s disease. Neurol Sci 30(5):367–373
Kemppainen NM, Aalto S, Wilson IA, Någren K, Helin S, Brück A, Oikonen V, Kailajärvi M, Scheinin M, Viitanen M, Parkkola R, Rinne JO (2006) Voxel-based analysis of PET amyloid ligand [11C]PIB uptake in Alzheimer disease. Neurology 67(9):1575–1580
Hansson O, Grothe MJ, Strandberg TO, Ohlsson T, Hägerström D, Jögi J, Smith R, Schöll M (2017) Tau pathology distribution in Alzheimer’s disease corresponds differentially to cognition-relevant functional brain networks. Front Neurosci 11:167
Tapiola T, Overmyer M, Lehtovirta M, Helisalmi S, Ramberg J, Alafuzoff I, Riekkinen P, Soininen H (1997) The level of CSF tau correlates with neurofibrillary tangles in AD. Neurol Rep 8(18):3961–3963
Buerger K, Ewers M, Andreasen N, Zinkowski R, Ishiguro K, Vanmechelen E, Teipel SJ, Graz C, Blennow K, Hampel H (2005) Phosphorylated tau predicts rate of cognitive decline in MCI subjects: a comparative CSF study. Neurology 65(9):1502–1503
Brys PE, Rich K, Rolstad S, Mosconi L, Switalski R, Glodzik-Sobanska L, De Santi S, Zinkowski R, Mehta P, Pratico D, Saint Louis LA, Wallin A, Blennow K, de Leon MJ (2007) Prediction and longitudinal study of CSF biomarkers in MCI. Neurobiol Aging 30(5):682–690
Duits FH, Teunissen CE, Bouwman FH, Visser PJ, Mattsson N, Zetterberg H, Blennow K, Hansson O, Minthon L, Andreasen N, Marcusson J, Wallin A, Rikkert MO, Tsolaki M, Parnetti L, Herukka SK, Hampel H, De Leon MJ, Schröder J, Aarsland D, Blankenstein MA, Scheltens P, van der Flier WM (2014) The CSF AD profile: easily said, but what does it mean? Alzheimers Dement 10(6):713–723
Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, Minthon L (2006) Association between CSF biomarkers and incipient AD disease in patients with MCI: a follow-up study. Lancet Neurol 5(3):228–234
Chung JA, Cummings JL (2000) Neurobehavioral and neuropsychiatric symptoms in Alzheimer’s disease: characteristics and treatment. Neurol Clin 18(4):829–846
Yazar T, Yazar HO, Demir EY, Özdemir F, Çankaya S, Enginyurt Ö (2018) Assessment of the mental health of carers according to the stage of patients with diagnosis of Alzheimer-type dementia. Neurol Sci 39(5):903–908
Ballarini T, Iaccarino L, Magnani G, Ayakta N, Miller BL, Jagust WJ, Gorno-Tempini ML, Rabinovici GD, Perani D (2016) Neuropsychiatric subsyndromes and brain metabolic network dysfunctions in early onset AD. Hum Brain Mapp 37(12):4234–4247
Ng KP, Pascoal TA, Mathotaarachchi S, Chung CO, Benedet AL, Shin M, Kang MS, Li X, Ba M, Kandiah N, Rosa-Neto P, Gauthier S (2017) Neuropsychiatric symptoms predict hypometabolism in preclinical Alzheimer disease. Neurology 88(19):1814–1821
Skogseth R, Mulugeta E, Jones E, Ballard C, Rongve A, Nore S, Alves G, Aarsland D (2008) Neuropsychiatric correlates of cerebrospinal fluid biomarkers in Alzheimer’s disease. Dement Geriatr Cogn Disord 25(6):559–563
Ramakers IH, Verhey FR, Scheltens P, Hampel H, Soininen H, Aalten P, Rikkert MO, Verbeek MM, Spiru L, Blennow K, Trojanowski JQ, Shaw LM, Visser PJ (2013) Anxiety is related to Alzheimer cerebrospinal fluid markers in subjects with mild cognitive impairment. Psychol Med 43(5):911–920
Babulal GM, Ghoshal N, Head D, Vernon EK, Holtzman DM, Benzinger TL, Fagan AM, Morris JC, Roe CM (2016) Mood changes in cognitively normal older adults are linked to Alzheimer’s disease biomarker levels. Am J Geriatr Psychiatry 24(11):1095–1104
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Carrillo MC, Thies B, Phelps CH (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:270e279
Petersen RC, Aisen P, Boeve BF, Geda YE, Ivnik RJ, Knopman DS, Mielke M, Pankratz VS, Roberts R, Rocca WA, Weigand S, Weiner M, Wiste H, Jack CRJ (2013) Mild cognitive impairment due to Alzheimer disease in the community. Ann Neurol 74:199e208
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):263–269
Cummings JL (1997) The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology 48:S10–S16
Liguori C, Romigi A, Mercuri NB, Nuccetelli M, Izzi F, Albanese M, Sancesario G, Martorana A, Sancesario GM, Bernardini S, Marciani MG, Placidi F (2014) Cerebrospinal-fluid orexin levels and daytime somnolence in frontotemporal dementia. J Neurol 261(9):1832–1836
Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S (2002) Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA 288(12):1475–1483
Spalletta G, Long JD, Robinson RG, Trequattrini A, Pizzoli S, Caltagirone C, Orfei MD (2015) Longitudinal neuropsychiatric predictors of death in Alzheimer’s disease. J Alzheimers Dis 48(3):627–636
Chen CT, Chang CC, Chang WN, Tsai NW, Huang CC, Chang YT, Wang HC, Kung CT, Su YJ, Lin WC, Cheng BC, Su CM, Hsiao SY, Hsu CW, Lu CH (2017) Neuropsychiatric symptoms in Alzheimer’s disease: associations with caregiver burden and treatment outcomes. QJM 110:565–570
Okonkwo OC, Alosco ML, Griffith HR, Mielke MM, Shaw LM, Trojanowski JQ, Tremont G (2010) Cerebrospinal fluid abnormalities and rate of decline in everyday function across the dementia spectrum: normal aging, mild cognitive impairment, and Alzheimer disease. Arch Neurol 67(6):688–696
Binetti G, Mega MS, Magni E, Padovani A, Rozzini L, Bianchetti A, Trabucchi M, Cummings JL (1998) Behavioral disorders in Alzheimer disease: a transcultural perspective. Arch Neurol 55:539–544
Albrecht D, Pendergrass A, Becker C, Hautzinger M, Pfeiffer K (2018) Interventionsstudien zur Unterstützung häuslicher Pflege. Z Gerontol Geriatr 51:642–649
Chiotis K, Saint-Aubert L, Savitcheva I, Jelic V, Andersen P, Jonasson M, Eriksson J, Lubberink M, Almkvist O, Wall A, Antoni G, Nordberg A (2016) Imaging in-vivo tau pathology in Alzheimer’s disease with THK5317 PET in a multimodal paradigm. Eur J Nucl Med Mol Imaging 43(9):1686–1699
Defrancesco M, Marksteiner J, Kemmler G, Fleischhacker WW, Blasko I, Deisenhammer EA (2017) Severity of depression impacts imminent conversion from mild cognitive impairment to Alzheimer’s disease. J Alzheimers Dis 59:1439–1448
Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D (2006) Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry 63(5):530–538
Teng E, Lu PH, Cummings JL (2007) Neuropsychiatric symptoms are associated with progression from mild cognitive impairment to AD. Dement Geriatr Cogn Disord 24(4):253–259
Sinforiani E, Terzaghi M, Pasotti C, Zucchella C, Zambrelli E, Manni R (2007) Hallucinations and sleep-wake cycle in Alzheimer’s disease: a questionnaire-based study in 218 patients. Neurol Sci 28(2):96–99
Liguori C, Nuccetelli M, Izzi F, Sancesario G, Romigi A, Martorana A, Amoroso C, Bernardini S, Marciani MG, Mercuri NB, Placidi F (2016) Rapid eye movement sleep disruption and sleep fragmentation are associated with increased orexin-A cerebrospinal-fluid levels in mild cognitive impairment due to Alzheimer’s disease. Neurobiol Aging 40:120–126
Tekin S, Mega MS, Masterman DM, Chow T, Garakian J, Vinters HV, Cummings JL (2001) Orbitofrontal and anterior cingulate cortex neurofibrillary tangyle burden is associated with agitation in Alzheimer disease. Ann Neurol 49(3):355–361
Zubenko GS, Moossy J, Martinez AJ, Rao G, Claassen D, Rosen J, Kopp U (1991) Neuropathologic and neurochemical correlates of psychosis in primary dementia. Arch Neurol 48(6):619–624
Sultzer DL, Mahler ME, Mandelkern MA, Cummings JL, Van Gorp WG, Hinkin CH, Berisford MA (1995) The relationship between psychiatric symptoms and regional cortical metabolism in Alzheimer’s disease. J Neuropsychiatr Clin Neurosci 7(4):476–484
Steenland K, Zhao L, Goldstein F, Cellar J, Lah J (2014) Biomarkers for predicting cognitive decline in those with normal cognition. J Alzheimers Dis 40(3):587–594
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scaricamazza, E., Colonna, I., Sancesario, G.M. et al. Neuropsychiatric symptoms differently affect mild cognitive impairment and Alzheimer’s disease patients: a retrospective observational study. Neurol Sci 40, 1377–1382 (2019). https://doi.org/10.1007/s10072-019-03840-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03840-4