Abstract
Quality of life (QOL) reflects the individual’s perception of the position within living contexts. This study was done to describe pre- and post-stroke QOLs of stroke survivors. A prospective longitudinal study was done among stroke survivors admitted to 13 hospitals in the western province of Sri Lanka. The calculated sample size was 260. The pre-stroke and post-discharge one-month QOL was gathered using short form-36 (SF-36) QOL tool. SF-36 includes questions on eight domains: general health, physical functioning, pain, role limitation due to physical problems, social functioning, vitality, role limitations due to emotional problems, and mental health. Univariate analysis was followed by determining the independent risk factors through multivariate analysis. The response rate was 81%. The disability was measured by the modified Rankin scale which ranges from 0 (no symptoms) to 6 (fatal outcome). The median (IQR) disability score was 4 (3 to 5). The post-discharge QOL scores were significantly lower than pre-stroke values (p < 0.05). With a higher pre-stroke QOL, younger age was significantly associated in six domains and higher income and better health infrastructure in two domains (p < 0.05). Six factors were determined to be independent risk factors for lower post-discharge QOL scores of SF-36: younger age (for general health and role limitation-physical domains), female gender (for physical functioning and pain domains), lower health infrastructure (for general health, vitality, and mental health domains), lower education (for pain domain), higher disability (for general health, physical functioning, vitality, social functioning, and mental health domains), and hypercholesterolemia (for role limitation-emotional domain). Stroke survivors have not regained their pre-stroke QOL at 1 month following the hospital discharge irrespective of income level and pre-stroke QOL. Higher pre- and post-stroke QOLs are associated with better statuses of social determinants of health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
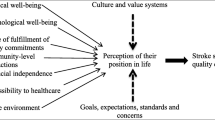
Stroke is a leading cause of death and a main reason for disability-adjusted life years globally [1,2,3,4]. The burden of stroke is expected to become worse in the coming years [5]. It has become a health, social, and economic burden to lower- and middle-income countries (LMICs) [6, 7]. There is a deficit of data on stroke in relation to LMICs [8]. Quality of life (QOL) reflects the individual’s self-perceived position within the social contexts [9, 10]. Health-related QOL is considered as a vital component in determining the success of the management of stroke [11]. It reflects the subjective improvement and thus the success of management as perceived by the stroke survivors [12].
Short form 36 (SF-36) is one of the commonly used generic tools in the assessment of QOL [13]. It provides eight domain scores in relation to QOL [14]. It has been developed with a conceptual framework which included behavioral functioning, perceived well-being, social/role disability, and personal evaluations [15]. It captures subjective well-being as perceived by the individual. Hence, though questions on aspects like cognition, sleep, and economy are not directly found in SF-36, they are reflected through its existing eight domains. SF-36 can be administered as a self-administered questionnaire or as an interviewer-administered questionnaire [15]. It has been validated for Sri Lanka [16]. The method of getting the pre-admission QOL retrospectively has been commonly used in literature [17, 18].
Generic QOL scales provide the opportunity of comparison of QOL between the disease conditions [19, 20]. Stroke has been found to be lowering the QOL in relation to physical as well as mental components [21]. Some studies have proved this reduction of QOL in relation to domains of SF-36 [22, 23]. Attempts are found in global literature in which multivariate analysis has been done with the SF-36 QOL scores. Multivariate analysis enables adjusting for confounding. Age, gender, and occupation are three factors which have been identified as independent risk factors in addition to the disease-related conditions [23, 24]. Furthermore, regression analysis has shown strong as well as weak associations between patient-related factors and the QOL scores, where the latter had been considered as dependent variables [22].
Global attempts have been made to predict the QOL using patient-related clinical and anatomical correlates [25]. Some literature suggests female gender as a positive factor for QOL whereas some studies have concluded it as not influencing the QOL [19, 26]. In addition, demographic factors (such as age, marital status), low education, severity, and comorbidities are found to be influencing the QOL of stroke survivors [20, 27]. Several measures are used in eliciting the disability level following stroke [28]. The modified Rankin scale is used commonly as an outcome measure in stroke research for this purpose [29, 30]. It is regarded as a valid and a reliable scale [31, 32]. It provides a score from 0 to 6 with 0 representing “no symptoms” and 6 being a “fatal outcome”. Severity of stroke measured by modified Rankin scale has been documented as influencing the QOL of stroke survivors [33].
Stroke is the leading cause of disability among adults in Sri Lanka [34]. With the demographic transition, the incidence of stroke is expected to rise in the future [34, 35]. Furthermore, concomitant comorbidities are common among stroke patients [36]. Older age, female gender, and stroke severity have been found as risk factors for disability level at hospital discharge in Sri Lanka [37]. It is mentioned that reducing the stroke burden in the South Asian region, to which Sri Lanka also belongs, would make a considerable positive impact on global health [38]. Sri Lanka is currently attempting to increase its stroke-related services [34]. QOL measured by SF-36 was found to be varying from country to country even when adjusted for confounders [39]. Hence, the local literature becomes an absolute necessity in the evaluation of the QOL of stroke survivors. Documented scientific evidence on the QOL among stroke survivors is rare in the study settings. This study was done to describe the factors influencing the pre- and post-stroke QOLs among stroke survivors admitted to 13 secondary- and tertiary-level government healthcare institutions in the western province of Sri Lanka.
Methods
Study design and study population
A prospective longitudinal study was done with two phases. Phase I was a cross-sectional study done at the hospital setting. Phase II was a cross-sectional study with a mail-based data collection. The study settings for the phase I were 13 government hospitals with secondary- and tertiary-care-level facilities in the western province of Sri Lanka. The study population included the patients who were directly admitted with the diagnosis of stroke to the study settings. The definition used in determining stroke was that of the World Health Organization: “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than that of vascular origin” [40, 41]. Inclusion criteria included the duration of hospital stay of more than 48 h. Patients with a physical or psychological comorbid condition which would independently influence the QOL were excluded.
Sample size
Sample size was calculated with the formula n = z 2 × SD2/l2. By setting the standard normal distribution value (z value) equal to a significance level of 5% and the design effect at 2 and by using the maximum standard deviation available in documented literature, the sample size needed at data analysis stage was estimated to be 208 [42, 43]. With an assumed response rate of 80% at the end of the phase II, the required sample size at the recruitment of phase I was estimated to be 260.
Data collection
All the patients who fulfilled the eligibility criteria were invited to be recruited. Data collection was simultaneously started in January 2015 and continued until the end of March 2015. Data collection was done by the investigators and seven trained bachelor of medicine/bachelor of surgery (MBBS)-qualified medical graduates. The interviewer-administered questionnaire utilized in the phase I included the socio-demographic details, medical parameters of the participants, and the SF-36 generic QOL tool. The disability level measured by the modified Rankin scale was used as a proxy measure of the severity of stroke.
For quantification of the level of health infrastructure, a judgmentally validated tool was used [44, 45]. This tool consisted of seven questions (Table 6) that covered the availability and accessibility of health services. The tool had been subjected to the approval of a panel of five experts who represented both the curative and the preventive health sectors. The score is given out of a total of 5 points.
Measurement of quality of life
The participants were asked to focus on the 4 weeks before the onset of the stroke and answer the questions of SF-36. Eight domains were assessed by SF-36 covering both physical and mental components. Each domain was given a score out of 100 which reflects the highest possible QOL. The scope of each domain has been summarized below [15]:
General health domain included five items and evaluates the perception on personal health.
Physical functioning domain included ten items and explores the limitations of the physical activities due to health.
Role limitation-physical included four items and assesses the problems with daily activities as a result of physical health.
Pain domain included two items and explores the presence of pain or any limitation due to pain.
Role limitation-emotional domain included three items and assesses the problems with daily activities as a result of emotional problems.
Vitality domain included four items and describes the level of energy and being worn out.
Social functioning domain included two domains and assess the level of interference of physical or emotional problems on social activities.
Mental health domain included five items and describes the feelings like happiness, peacefulness, and calmness.
Since all participants were able to answer the questions, proxy responses were not needed. The reliability of the questionnaire had been assessed in the pre-testing period. Furthermore, in the proper study, random cross-checking of the participants’ responses was done with the responses of selected bystanders.
At the hospital discharge, the participants were given the self-administered questionnaire to be filled for phase II, with a stamped envelope with the principal investigator’s name written on it. A reminder was given over the phone around day 25 following hospital discharge requesting to fill the questionnaire immediately after day 28. This questionnaire for phase II included the SF-36 tool.
Data analysis and data quality assurance
Data were entered into a datasheet of Statistical Package in Social Sciences version 17 and were analyzed. After assessing the normality of the variables, the non-parametric techniques were used for univariate analysis. Spearman correlation coefficient was used for quantitative associations with the QOL scores. Mann-Whitney U test was used in comparing two independent categories. Pre- and post-discharge QOL scores were tested with Wilcoxon t test. Ensuring that the regression assumptions were not violated, multivariate analysis was done by getting the variables which showed an association with the QOL scores with a p value less than 0.2 into the linear regression models. All possible measures were applied from the planning stage of the study to minimize potential biases.
Ethical approval
Ethics approval was obtained prior to the commencement of data collection from the Ethics Review Committee of the Sri Lanka Medical Association. The procedures followed were in accordance with institutional guidelines of the study settings.
Results
Characteristics of the responders
Out of the 260 recruited participants, 247 responded in getting the pre-stroke QOL in phase I (response rate 95%). Following the hospital discharge, 210 responded by posting the questionnaire with an overall response rate of 81%. The participation-related details have been summarized in Fig. 1.
The non-responders following the hospital discharge either died or could not be contacted. There was no apparent non-response bias in analyzing the characteristics of the responders versus non-responders.
The median (IQR) age of the responders was 62 (52 to 70) years. Out of them, 125 (59.5%) were males and nearly 44% (n = 93) had a monthly income below Rs 30,000 (approximately US$200). The median (IQR) duration of stay was 7 (5, 12, to) days. The median (IQR) modified Rankin scale score was 4 (3to 5). The median (IQR) score for the health infrastructure was 1.25 (0.5 to 1.5). Nearly 40% (n = 82) had diabetes, 56% (n = 118) had hypertension, and 25% (n = 53) had hypercholesterolemia.
Pre-stroke and post-stroke QOLs
The distributions of the pre-stroke and post-discharge scores of the QOL domains are summarized in Table 1. Measures of central tendencies for all eight domain scores were higher prior to the occurrence of the stroke (p < 0.05). The lowest post-discharge QOL was recorded for the role limitation-physical domain whereas the highest value was observed for role limitation-emotional domain.
Associations of QOL
Table 2 shows the associations of five selected variables with pre-stroke QOL. With six domain scores, the increasing age showed a significant correlation in a negative direction (p < 0.05) even though the values for the strength of association were low. There was no significant difference of the QOL domain scores between males and females. The correlations of the QOL scores with the highest education level also were non-significant. When the income was higher, the pain domain score (p = 0.002) and the social functioning domain score were higher (p = 0.037). When the health infrastructure was better, the QOL scores were higher (p < 0.05) for two domains.
The associations of age, gender, highest education, monthly income, and health infrastructure with the post-discharge QOL have been summarized in Table 3. In contrast to the pre-stroke findings, a younger age was associated with lower QOL scores for two domains. Furthermore, the male gender showed higher QOL scores for seven domains (p < 0.05). The correlations of the QOL scores with a higher education level were significant in the positive direction for six domains. In contrast with the pre-stroke values, a relatively higher income was associated with lower QOL scores for four domains. Better health infrastructure was associated with higher QOL scores for four domains (p < 0.05).
Correlation between pre-stroke QOL and post-stroke QOL
Table 4 shows the correlation of post-discharge QOL scores with pre-stroke scores. Furthermore, it summarizes the correlation of the post-discharge QOL with the severity of the disability. A significant correlation was observed only for the mental health domain (p = 0.047) between the post-discharge QOL and the pre-stroke QOL scores. A higher disability level (which reflects the severity of stroke) following the stroke was associated with lower QOL scores at 1-month hospital discharge for five domains: physical functioning, role limitation-emotional, vitality, social functioning, and mental health (p < 0.05).
Independent risk factors
The multivariate analysis for the predictors of the 1-month post-discharge QOL has been summarized in Table 5. Severity of the stroke and the presence of hypercholesterolemia showed negative beta coefficients whereas higher age, better health infrastructure, male gender, and higher education showed positive coefficients. It shows older age (for two domains, general health and role limitation-physical), better health infrastructure (for three domains, general health, vitality, and mental health), lower severity of stroke (five domains, general health, physical functioning, vitality, social functioning, mental health), male gender (for two domains, physical functioning and pain), higher education level (one domain, pain domain), and not having hypercholesterolemia (for one domain, role limitation-emotional) as independent predictors of a better QOL.
Discussion
The study findings reveal a significant worsening of the QOL at 1 month of hospital discharge following a stroke, compared to the baseline pre-stroke QOL in relation to both physical and mental components. Demographic and social factors influence the pre-stroke QOL. There were six independent risk factors (age, gender, education level, disability level, hypercholesterolemia, and level of health-infrastructure) which can predict the QOL following the hospital discharge for the domains of SF-36. The pre-stroke QOL scores were not associated with the post-discharge QOL for seven out of eight domains.
Context-specific QOL data are essential in preparation of a comprehensive stroke burden mitigation program [11, 39]. Sri Lanka is trying to broaden the services for curbing the negative influences of stroke [34]. Furthermore, most studies which have been done in this setting are either hospital-based or community-based. The inclusion of both a hospital-based component and a follow-up component (i.e., when the participants are living in the community setting following the hospital discharge) in the present study enabled the evaluation of associations which have been adjusted for essential parameters like the disability level. Hence, this study provides vital scientific evidences for the policy makers and for those who are involved in the development of rehabilitation guidelines.
The findings suggest a higher prevalence of stroke among males and the presence of concomitant NCD conditions among many survivors. These are in agreement with the available local literature [36]. Due to the epidemiological transition Sri Lanka is experiencing currently, the prevalence of risk factors would further go up in the future [46]. Even though the patients are discharged from the hospital when they are capable of living in the community, all the QOL domain scores showed a significant worsening. This fact has been recorded in the previous literature [21,22,23]. It shows that many more aspects are to be covered in the rehabilitation of a stroke survivor.
Older age was associated with a lower pre-stroke QOL. Though this has been documented in literature, the post-stroke QOL was found to be lower among the young in this study. This is contradictory to some reported findings [27]. This may be due to the higher impact of the transition of lifestyles of the young, following a stroke. The impact of the social determinants of health on the QOL of patients has been highlighted [47]. This study has added some more evidence in this regard.
Being young, being a female, poor health infrastructure, lower education, severity of the stroke, and hypercholesterolemia were found to be independent risk factors for getting a lower QOL. This highlights the importance of ensuring the equity of opportunities for health in managing the stroke patients. Furthermore, it brings light on the necessity of proper management of concomitant comorbidities. Female gender, the young, and patients with severe disability following stroke could be followed up with a higher frequency following hospital discharge.
Better availability and the accessibility of the health services as measured by the tool measuring the health infrastructure were associated with better pre-stroke QOL (Table 6). In addition, better health infrastructure was found to be an independent predictor of better post-stroke QOL at 1 month from hospital discharge. These findings further emphasize the value of improving primary healthcare service delivery of LMICs like Sri Lanka.
The reduced QOL among the participants with a lower education may be due to several reasons. Firstly, their level of compliance on the management guidelines would have been less. Secondly, they might not be having a clear understanding on the recovery process. Hence, the conception of the future may be blurred in them lowering their perception of the position within social contexts. The higher disability gives rise to a lower QOL which is comparable to the global evidences [33]. This suggests the necessity of providing a greater concern on laying a management plan at hospital discharge for those who are with a higher level of disability.
Firstly, one limitation of the study was the omission of the type of stroke and some of the clinical features of stroke in the analysis. Yet it would not have an impact on the validity of the result as the QOL is a subjective perspective. The patients would have related the QOL more towards the disability level rather than to clinical characteristics of stroke. Secondly, the omission of patients with duration of stay less than 48 h would have diluted the associations. Yet it had to be done due to ethical reasons as well as to filter out the non-eligible admissions like transient ischemic attacks. In the phase I, SF-36 was administered with an interview and in phase II, it was self-administered. Any bias out of this was minimized by providing elaborative instructions for the participants on the filling of the questionnaire. Furthermore, the SF-36 manual states that SF-36 could be used in either way. The authors want to highlight the fact that though the number of eligible participants during the study period has been mentioned in Fig. 1, it should not be used in determining the incidence of stroke patients in the western province. This, as understood, is due to the filtering effect imposed by the eligibility criteria in the selection of participants.
Conclusions and recommendations
Comorbid non-communicable conditions are common among people who experience stroke. Proper elderly care and improving the socioeconomic status and the coverage of health services could be considered in raising the pre-stroke QOL among those who are at risk of getting a stroke. Younger age, female gender, poor health infrastructure, lower education, worse severity of the stroke, and hypercholesterolemia are independent risk factors for getting a lower QOL following hospital discharge. These factors must be considered in decision-making and prioritization of rehabilitation. Stroke survivors have not regained their previous quality of life even 1 month following the hospital discharge. They are at risk of getting a lower QOL irrespective of the pre-stroke QOL if the mentioned risk factors are not addressed. Recommendations for raising the post-stroke QOL may include ensuring the equity of social determinants of health and providing care more frequently for stroke survivors with predictors of lower QOL.
References
Hankey GJ (2013) The global and regional burden of stroke. Lancet Glob Health 1(5). https://doi.org/10.1016/S2214-109X(13)70095-0
Khoshnam SE, Winlow W, Farzaneh M, Farbood Y, Moghaddam HF (2017) Pathogenic mechanisms following ischemic stroke. Neurol Sci 38(7):1167–1186. https://doi.org/10.1007/s10072-017-2938-1
Colaianni V, Mazzei R, Cavallaro S (2016) Copy number variations and stroke. Neurol Sci 37(12):1895–1904. https://doi.org/10.1007/s10072-016-2658-y
Zhong W, Geng N, Wang P, Li Z, Cao L (2016) Prevalence, causes and risk factors of hospital readmissions after acute stroke and transient ischemic attack: a systematic review and meta-analysis. Neurol Sci 37(8):1195–1202. https://doi.org/10.1007/s10072-016-2570-5
WHO (2004). Global burden of stroke. atlas Hear Dis stroke. 15:50-51. doi:https://doi.org/10.1016/B978-1-4160-5478-8.10019-3.
Mukherjee D, Patil CG. Epidemiology and the global burden of stroke. World Neurosurg. 2011;76(6 SUPPL.). doi:https://doi.org/10.1016/j.wneu.2011.07.023.
Corbyn Z (2014) Stroke—statistics: a growing global burden. Nature 510(7506):S2–S3. https://doi.org/10.1038/510S2a
Fuentes B, Tejedor ED (2014) Stroke: the worldwide burden of stroke—a blurred photograph. Nat Rev Neurol 10(3):127–128. https://doi.org/10.1038/nrneurol.2014.17
WHO (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med 28(3):551–558 doi:10.5.12
Mahesh PKB, Gunathunga MW, Jayasinghe S, Arnold SM, Haniffa R, De Silva AP (2017) Pre-event quality of life and its influence on the post-event quality of life among patients with ST elevation and non-ST elevation myocardial infarctions of a premier province of Sri Lanka. Health Qual Life Outcomes 15(1):154. https://doi.org/10.1186/s12955-017-0730-9
Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. In: Cerebrovascular Diseases. Vol 27 ; 2009:204–214. doi:https://doi.org/10.1159/000200461
Opara JA, Jaracz K (2010) Quality of life of post-stroke patients and their caregivers. J Med Life 3(3):216–220 http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3018998&tool=pmcentrez&rendertype=abstract
Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R (2002) Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ 324(7351):1417. https://doi.org/10.1136/bmj.324.7351.1417
Svetel MV, Jovic JS, Pekmezovic TD, Kostic VS (2015) Quality of life in patients with primary restless leg syndrome: community-based study. Neurol Sci 36(8):1345–1351. https://doi.org/10.1007/s10072-015-2103-7
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey manual and interpretation guide. Bost New Engl Med Cent. 1993:1 v. (various pagings). http://books.google.com/books/about/SF_36_health_survey.html?id=WJsgAAAAMAAJ
Gunawardena NS, Seneviratne SRA, Atauda T (2003) An approach to validation of a multi-dimensional tool. J Coll Commun Phys Sri Lanka 8:18–26
Hofhuis JGM, Spronk PE, van Stel HF, Schrijvers AJP, Bakker J (2007) Quality of life before intensive care unit admission is a predictor of survival. Crit Care 11(4):R78. https://doi.org/10.1186/cc5970
Wehler M, Martus P, Geise A et al (2001) Changes in quality of life after medical intensive care. Intensive Care Med 27(1):154–159 http://www.ncbi.nlm.nih.gov/pubmed/11280627
Kranciukaite D, Rastenyte D (2006) Measurement of quality of life in stroke patients. Medicina (Kaunas) 42(9):709–716 http://www.ncbi.nlm.nih.gov/pubmed/21717044
Carod-Artal FJ (2012) Determining quality of life in stroke survivors. Expert Rev Pharmacoecon Outcomes Res 12(2):199–211. https://doi.org/10.1586/erp.11.104
Haley WE, Roth DL, Kissela B, Perkins M, Howard G (2011) Quality of life after stroke: a prospective longitudinal study. Qual Life Res 20(6):799–806. https://doi.org/10.1007/s11136-010-9810-6
Bugge C, Hagen S, Alexander H (2001) Measuring stroke patients’ health status in the early post-stroke phase using the SF36. Int J Nurs Stud 38(3):319–327. https://doi.org/10.1016/S0020-7489(00)00066-3
Jönsson A-C, Lindgren I, Hallström B, Norrving B, Lindgren A (2005) Determinants of quality of life in stroke survivors and their informal caregivers. Stroke 36(4):803–808. https://doi.org/10.1161/01.STR.0000160873.32791.20
Patel MD, McKevitt C, Lawrence E, Rudd AG, Wolfe CDA (2007) Clinical determinants of long-term quality of life after stroke. Age Ageing 36(3):316–322 7p. http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=17374601&site=ehost-live&scope=site%5Cnhttp://search.ebscohost.com/login.aspx?direct=true&db=c8h&AN=105997982&site=ehost-live&scope=site
Moon Y-S, Kim S-J, Kim H-C, Won M-H, Kim D-H (2004) Correlates of quality of life after stroke. J Neurol Sci 224(1–2):37–41. https://doi.org/10.1016/j.jns.2004.05.018
Vrdoljak D, Rumboldt M (2008) Quality of life after stroke in Croatian patients. Coll Antropol 32(2):355–359
Nichols-Larsen DS, Clark PC, Zeringue A, Greenspan A, Blanton S (2005) Factors influencing stroke survivors’ quality of life during subacute recovery. Stroke 36(7):1480–1484. https://doi.org/10.1161/01.STR.0000170706.13595.4f
Kwon S, Hartzema AG, Duncan PW, Lai SM (2004) Disability measures in stroke: relationship among the Barthel index, the functional independence measure, and the modified Rankin scale. Stroke 35(4):918–923. https://doi.org/10.1161/01.STR.0000119385.56094.32
Quinn TJ, Dawson J, Walters MR, Lees KR (2008) Variability in modified rankin scoring across a large cohort of international observers. Stroke 39(11):2975–2979. https://doi.org/10.1161/STROKEAHA.108.515262
Rocco A, Ringleb PA, Grittner U, Nolte CH, Schneider A, Nagel S (2015) Follow-up C-reactive protein level is more strongly associated with outcome in stroke patients than admission levels. Neurol Sci 36(12):2235–2241. https://doi.org/10.1007/s10072-015-2342-7
Banks JL, Marotta CA (2007) Outcomes validity and reliability of the modified rankin scale: implications for stroke clinical trials—a literature review and synthesis. Stroke 38(3):1091–1096. https://doi.org/10.1161/01.STR.0000258355.23810.c6
Kasner SE (2006) Clinical interpretation and use of stroke scales. Lancet Neurol 5(7):603–612. https://doi.org/10.1016/S1474-4422(06)70495-1
Kim JS, Choi-Kwon S, Kwon SU, Lee HJ, Park KA, Seo YS (2005) Factors affecting the quality of life after ischemic stroke: young versus old patients. J Clin Neurol 1:59–68. https://doi.org/10.3988/jcn.2005.1.1.59
Wijeratne T, Gunaratne P, Gamage R et al (2011) Stroke care development in Sri Lanka: the urgent need for neurorehabilitation services. Neurol Asia 16(2):149–151
Chang T, Gajasinghe S, Arambepola C (2011) Epidemiology of stroke in the district of Colombo, Sri Lanka: A community-based study Cerebrovasc Dis 32:6. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed10&NEWS=N&AN=70610079
Chang T, Gajasinghe S, Arambepola C (2015) Prevalence of stroke and its risk factors in urban Sri Lanka: population-based study. Stroke 46(10):2965–2968. https://doi.org/10.1161/STROKEAHA.115.010203
Ranawaka U, Alexander F, Nawaratne D, Liyanage H, Kulatunga A, Tissera N, et al. (2012) Factors affecting early outcome in Sri Lankan patients with stroke. Neurology. 78(1 Meeting Abstract):no pagination-no pagination. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed10&NEWS=N&AN=70727749
Wasay M, Khatri I, Kaul S (2014) Stroke in South Asian countries. Nat Rev Neurol 10(3):135–143. https://doi.org/10.1038/nrneurol.2014.13
Sprigg N, Gray LJ, Bath PMW et al (2012) Quality of life after ischemic stroke varies in western countries: data from the Tinzaparin in acute ischaemic stroke trial (TAIST). J Stroke Cerebrovasc Dis 21(7):587–593. https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.01.007
Sacco RL, Kasner SE, Broderick JP et al (2013) An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American heart association/American stroke association. Stroke 44(7):2064–2089. https://doi.org/10.1161/STR.0b013e318296aeca
Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T (1980) Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 58(1):113–130 doi:D - NLM: PMC2395897 EDAT- 1980/01/01 MHDA- 1980/01/01 00:01 CRDT- 1980/01/01 00:00 PST - ppublish
Unalan D, Soyuer F, Ozturk A, Mistik S (2008) Comparison of SF-36 and WHOQOL-100 in patients with stroke. Neurol India 56(4):426–432. https://doi.org/10.4103/0028-3886.44573
Charan J, Biswas T (2013) How to calculate sample size for different study designs in medical research? Indian J Psychol Med 35(2):121–126. https://doi.org/10.4103/0253-7176.116232
Mahesh PKB, Gunathunga MW, Jayasinghe S et al (2017) Financial burden of survivors of medically-managed myocardial infarction and its association with selected social determinants and quality of life in a lower middle income country. BMC Cardiovasc Disord 17(1):251. https://doi.org/10.1186/s12872-017-0687-y
Mahesh P.K.B, Gunathunga M.W. JS. (2015) Influence of social determinants on the disease-outcome, financial burden and quality of life after a critical illness due to chronic non communicable diseases, among patients treated at government hospitals in the western province of Sri Lanka
Jayasekara RS, Schultz T (2007) Health status, trends, and issues in Sri Lanka. Nurs Health Sci 9(3):228–233. https://doi.org/10.1111/j.1442-2018.2007.00328.x
WHO. Closing the gap in a generation.health equity through action on the social determinants of health. 2008. doi:https://doi.org/10.1080/17441692.2010.514617
Author information
Authors and Affiliations
Contributions
All authors were involved in the planning of the research study. PKB was the principal investigator and was involved in getting ethics permissions, data collection, data analysis, and writing of the manuscript. MW, S, and SM were involved in data analysis, data interpretation, and writing of the manuscript. SN was involved in data collection, data entering, interpretation of data, and writing the manuscript. All authors went through the final manuscript.
Corresponding author
Ethics declarations
Ethics approval was obtained from the Ethics Review Committee of Sri Lanka Medical Association prior to the data collection (reference number ERC/119 approval was given on 27 August 2014). Informed written consent was obtained from the participants. Therefore, the study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Specific national laws have been observed.
Conflict of interest
The authors declare that they no conflict of interest.
Consent for publication
The manuscript does not contain any personal details at the individual level.
Availability of data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The dataset has been included as a supplementary file.
Electronic supplementary material
ESM 1
(SAV 245 kb)
Rights and permissions
About this article
Cite this article
Mahesh, P.K.B., Gunathunga, M.W., Jayasinghe, S. et al. Factors influencing pre-stroke and post-stroke quality of life among stroke survivors in a lower middle-income country. Neurol Sci 39, 287–295 (2018). https://doi.org/10.1007/s10072-017-3172-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3172-6