Abstract
This document presents the guidelines for testing antibodies against neuronal surface antigens that have been developed following a consensus process built on questionnaire-based surveys, internet contacts, and discussions at workshops of the sponsoring Italian Association of Neuroimmunology (AINI) congresses. Essential clinical information on autoimmune encephalitis associated with antibodies against neuronal surface antigens, indications and limits of testing for such antibodies, instructions for result interpretation, and an agreed laboratory protocol (Appendix A) are reported for the communicative community of neurologists and clinical pathologists.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diagnostics for autoimmune encephalitis associated with antibodies against neuronal surface antigens (NS-Abs) is performed by laboratories which usually conduct mono-specialist investigations requiring sophisticated technological and professional skills. These are designed to diagnose and monitor the course and treatment of autoimmune encephalitis. Notably, particularly at onset, these diseases are in differential diagnosis with other encephalitic manifestations [1,2,3,4,5]. The possibilities of NS-Ab-associated autoimmune encephalitis after the occurrence of Herpes simplex virus encephalitis [6] and of clinical phenotypes overlapping with acquired demyelinating syndromes of the CNS should be taken into consideration too [7].
The herein proposed procedures can also be used for research purposes, considering that many clinical pictures associated with these antibody reactivities have been only partially characterized. The type of studies that can be performed and the available equipment depend on the importance of the healthcare setting and thus on the type of diagnostic and observational questions to be answered.
Clinical and laboratory aspects
NS-Abs are directed against membrane proteins (synaptic receptors and ion channels). Identification of NS-Abs in patient serum and/or cerebrospinal fluid (CSF) is of key importance since the forms of encephalitis associated with these autoantibodies are potentially responsive to immunotherapy. A minority of cases (depending on antibody reactivity) are paraneoplastic forms (i.e., a tumor is the immunological trigger), and thus antibody positivity plays an essential role in planning adequate cancer screening.
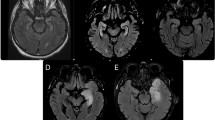
The NS-Ab spectrum is broad and continually expanding. The clinically most important antibodies, in relation to their frequency and number of reported cases, are the anti-NMDA-R (N-methyl-d-aspartate receptor) and the antibodies against proteins associated with the voltage-gated potassium channel-complex: anti-LGI1 (leucine-rich, glioma inactivated 1) and anti-CASPR2 (contactin-associated protein-like 2) (Fig. 1). Several other antibodies have been described, whose associated clinical picture has been only partially characterized. A list of these antibodies is as follows:
-
Anti-AMPA-R (α-amino-hydroxymethyl-isoxazoleproprionic acid receptor)
-
Anti-D2R (dopamine D2 receptor)
-
Anti-DPPX (dipeptidyl-peptidase-like protein 6)
-
Anti-GABA A -R (γ-aminobutyric acid-A-receptor)
-
Anti-GABA B -R (γ-aminobutyric acid-B-receptor)
-
Anti - Gly - R (glycine receptor)
-
Anti - IgLON5 (IgLON member 5)
-
Anti - mGluR5 (metabotropic glutamate receptor 5)
-
Anti-Neurixin-3α
Molecular organization of the voltage-gated potassium (Kv) channel-complex. Kv channels regulate cell-membrane potential and excitability in neurons and other cell types, with regulatory activity by interacting proteins (LGI1, leucine-rich, glioma inactivated 1) and accessory subunits (CASPR2, contactin-associated protein-like 2; contactin-2; ADAM22, disintegrin and metalloproteinase domain-containing protein 22); autoimmune antibody attacks can target extracellular or intracellular epitopes
NS-Abs target epitopes that are generally conformational, namely they depend on the tertiary structure of the target protein and are no longer recognizable by antibodies after denaturation. Accordingly, they are best identified by techniques preserving the native conformation of proteins/antigens (e.g., cell-based assays, CBAs).
Preliminary data from research laboratories suggest that in-house CBAs perform better than commercial fixed cell-based kits, but no studies have to date compared these techniques (as the one conducted for anti-aquaporin-4 antibodies) [8]. Particularly suspected cases testing negative with commercial CBAs should be assayed with in-house tests. There is also some debate as to whether to use vital or fixed (and possibly also permeabilized) transfected cells for in-house CBA [9, 10]. Vital cells should guarantee greater specificity since they minimize non-specific intracellular reactivity (due to antibody internalization after cell fixation or permeabilization).
The abovementioned considerations support a two-level approach for NS-Ab testing: first level diagnostics performed by laboratories that use certified commercial tests (most AINI laboratories fall into this category), and second level diagnostics performed by laboratories that conduct research work and use in-house tests with high levels of sensitivity and specificity (currently considered the gold standard) [11].
First level
Based on immunofluorescence tests using fixed cell lines (cell-based assay, CBA) transfected with the antigen of interest (Euroimmun, Lübeck, Germany), commercial kits for the following antibodies are available: NMDA-R, LGI1, CASPR2, GABAB-R, AMPA-R1/2, DPPX, IgLON5.
Mosaics designed for broad-spectrum approach including the most frequent antibody reactivities (i.e., anti-NMDA-R, anti-LGI1, anti-CASPR2) are recommended in routine diagnostics. Other tests with single antibody are designed to diagnose specific clinico-pathological pictures [10, 12, 13]. Diagnostic specificity and sensitivity data provided by the manufacturer are as follows: anti-NMDA-R (serum), 100 and 83.5%; anti-NMDA-R (CSF), 100 and 99.5%; anti-GABAB-R, 100 and 82.4%; anti-LGI1, 100 and 100%; anti-CASPR2, 100 and 99.7%; anti-DPPX, 100 and 100% [14]. While these data seem satisfactory, they require corroboration in independent clinical series.
Second level
Second-level diagnostics entail the search for known and unknown antibodies based on the following techniques:
-
Immunohistochemistry on fixed and/or frozen rat brain tissue (several fixation protocols differently impact on the conformational status of target epitopes);
-
Immunofluorescence on primary neuronal cultures;
-
Immunofluorescence on live or fixed in-house CBAs.
Discovery of the real antigen targets of voltage-gated potassium channel antibodies (VGKC Abs, historically identified with radioimmunoprecipitation assay, RIPA), i.e., the proteins LGI1 and CASPR2 (Fig. 1) [15, 16] has revealed that a non-negligible percentage of cases with positive results on RIPA are instead negative for the real reactivities assayed with CBA [15, 17]. However, it has been recently demonstrated that VGKC Ab-positive sera, but double negative for LGI1 and CASPR2 antibodies, mostly targeted intracellular cytosolic epitopes of Kv1 subunits (Fig. 1). These antibodies should no longer be classified as NS-Abs, and thus, lacking pathogenic potential, they should entail no immunotherapy [18].
In summary, a standardized autoantibody approach is recommended to appropriately screen patients with autoimmune encephalitis, based on the following pathway:
-
1.
A screening test with commercial broad-spectrum mosaic CBAs, except in the case of strong diagnostic suspicion of syndrome-specific forms (e.g., anti-NMDA-R antibody syndrome);
-
2.
A commercial CBA assay for less-common antibodies (e.g., anti-AMPA-R, anti-GABA-R, anti-DPPX) should be adopted when the results of screening tests with mosaics are negative and the clinical phenotypes are suggestive of autoimmune encephalitis, especially if they show atypical clinical features;
-
3.
If the patient continues to test negative despite strong clinical suspicion, samples should be sent to a center using the second-level tests within the AINI network.
NS-Abs usually belong to the IgG class; the significance of IgA or IgM reactivities is still uncertain, but they are probably non-specific [19]. However, clinical phenotypes characterized by mild cognitive impairment have been reported, but never confirmed so far, in patients with NMDA-R IgA [20].
Both serum and CSF samples should be tested in routine diagnostics, when NS-Ab-associated autoimmune encephalitis is suspected. In the most frequent anti-NMDA-R encephalitis, the disease-specific antibodies have been shown to be present in the CSF but not in the serum in 14% of cases [9]. Conversely, antibody positivity in serum and, at second opinions, negativity in the corresponding CSF have been reported in patients with degenerative or psychiatric pathologies [21, 22]. Accordingly, patients with serum positivity and CSF negativity, or with CSF sample unavailable, should be considered with high caution, taking into account the consistency of clinico-paraclinical data, and discussed with the reference laboratory experts. In patients with antibody positivity in both serum and CSF samples, antibody-specific intrathecal synthesis can be calculated [23]. Noteworthy, the recently proposed clinical diagnostic criteria for autoimmune encephalitis can help diagnose these syndromes in single patients [24].
The tests for NS-Ab detection yield qualitative (positive/negative/borderline positivity), or, in positive cases, semiquantitative results based on antibody titers. In accordance with current knowledge, antibody titers are not fundamental, and therefore testing for titers is optional. The limited and not confirmed data available, mainly obtained in anti-NMDA-R encephalitis, suggest an association between high antibody titers and poor prognosis, or presence of teratoma (CSF titers correlate better than serum titers) [9]. It is advisable to store serum and CSF samples for possible future titration.
References
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D et al (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 10:835–844
Ambrose HE, Granerod J, Clewley JP, Davies NWS, Keir G, Cunningham R et al (2011) Diagnostic strategy used to establish etiologies of encephalitis in a prospective cohort of patients in England. J Clin Microbiol 49:3576–3583
Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA (2012) The frequency of autoimmune N-methyl-d-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis 54:899–904
Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A et al (2013) Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis 57:1114–1128
Armangue T, Leypoldt F, Dalmau J (2014) Autoimmune encephalitis as differential diagnosis of infectious encephalitis. Curr Opin Neurol 27:361–368
Armangue T, Leypoldt F, Málaga I, Raspall-Chaure M, Marti I, Nichter C et al (2014) Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann Neurol 75:317–323
Titulaer MJ, Höftberger R, Iizuka T, Leypoldt F, McCracken L, Cellucci T et al (2014) Overlapping demyelinating syndromes and anti-N-methyl-D-aspartate receptor encephalitis. Ann Neurol 75:411–428
Waters P, Reindl M, Saiz A, Schanda K, Tuller F, Kral V et al (2016) Multicentre comparison of a diagnostic assay: aquaporin-4 antibodies in neuromyelitis optica. J Neurol Neurosurg Psychiatry 87:1005–1015
Gresa-Arribas N, Titulaer MJ, Torrents A, Aguilar E, McCracken L, Leypoldt F et al (2014) Antibody titers at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol 13:167–177
Irani SR, Gelfand JM, Al-Diwani A, Vincent A (2014) Cell-surface central nervous system autoantibodies: clinical relevance and emerging paradigms. Ann Neurol 76:168–184
Dalmau J, Geis C, Graus F (2017) Autoantibodies to synaptic receptors and neuronal cell surface proteins in autoimmune diseases of the central nervous system. Physiol Rev 97:839–887
Lancaster E, Dalmau J (2012) Neuronal autoantigens—pathogenesis, associated disorders and antibody testing. Nat Rev Neurol 8:380–390
Zuliani L, Graus F, Giometto B, Bien C, Vincent A (2012) Central nervous system neuronal surface antibody associated syndromes: review and guidelines for recognition. J Neurol Neurosurg Psychiatry 83:638–645
Euroimmun. IIFT: Neurology Mosaics. Instructions for the indirect immunofluorescence test. Version: 31/01/2017; www.euroimmun.com
Irani SR, Alexander S, Waters P, Kleopa KA, Pettingill P, Zuliani L et al (2010) Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan’s syndrome and acquired neuromyotonia. Brain 133:2734–2748
Lai M, Huijbers MGM, Lancaster E, Graus F, Bataller L, Balice-Gordon R et al (2010) Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol 9:776–785
Paterson RW, Zandi MS, Armstrong R, Vincent A, Schott JM (2013) Clinical relevance of positive voltage-gated potassium channel (VGKC)-complex antibodies: experience from a tertiary referral centre. J Neurol Neurosurg Psychiatry 85:625–630
Lang B, Makuch M, Moloney T, Dettmann I, Mindorf S, Probst C et al (2017) Intracellular and non-neuronal targets of voltage-gated potassium channel complex antibodies. J Neurol Neurosurg Psychiatry 88:353–361
Dahm L, Ott C, Steiner J, Stepniak B, Teegen B, Saschenbrecker S et al (2014) Seroprevalence of autoantibodies against brain antigens in health and disease. Ann Neurol 76:82–94
Prüss H, Höltje M, Maier N, Gomez A, Buchert R, Harms L et al (2012) IgA NMDA receptor antibodies are markers of synaptic immunity in slow cognitive impairment. Neurology 78:1743–1753
Zandi MS, Paterson RW, Ellul MA, Jacobson L, Al-Diwani A, Jones JL et al (2015) Clinical relevance of serum antibodies to extracellular N-methyl-d-aspartate receptor epitopes. J Neurol Neurosurg Psychiatry 86:708–713
Armangue T, Santamaria J, Dalmau J (2015) When a serum test overrides the clinical assessment. Neurology 84:1379–1381
Reiber H, Lange P (1991) Quantification of virus-specific antibodies in cerebrospinal fluid and serum: sensitive and specific detection of antibody synthesis in brain. Clin Chem 37:1153–1160
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404
Acknowledgements
The authors thank Joanne Fleming for the linguistic revision.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
-
1.0
Preanalytical procedures
-
1.1
Blood is collected in tubes without anticoagulant. Fasting samples are required. No necessity of food restrictions.
-
1.2
Blood sample is centrifuged, after clot formation, as soon as possible (3000 g for 10 min).
-
1.3
Serum samples are tested after centrifugation, or stored in aliquots at −20 °C until analysis (1 month, or preferably at −80 °C for longer periods).
-
1.4
Frozen serum samples should not be thawed and frozen again.
-
1.5
Grossly hemolyzed or lipemic samples should be discarded. Centrifuge the serum prior to assay to remove any particulate matter.
-
1.6
Plasma samples are allowed.
-
1.7
In the case of CSF testing, refer to the document on cerebrospinal fluid analysis and the determination of oligoclonal bands.
-
2.0
Analytical procedures
-
2.1
Cell-based assay. The commercial CBA provided by Euroimmun is currently the only available standardized test. Differently from in-house tests, for which the research purpose is specified in the report, standardized tests allow a formally valid use of diagnostic results.
-
2.1.1
Preparation of reagents
-
2.1.1.1
Slides on which transfected cells are attached are ready for use and sealed in a sachet that should be opened when it has reached room temperature (18–25 °C) to avoid condensation. If the sachet is damaged, slides are unusable.
-
2.1.1.2
Secondary antibody: shake before use and protect from direct light.
-
2.1.1.3
Washing solution: dissolve the buffer with distilled water, add Tween-20 and shake for at least 20 min (for assays performed after more than 1 week, a fresh washing solution must be prepared at each analytical session, in appropriate volumes).
-
2.1.2
Preparation of samples
-
2.1.2.1
Dilute 1:10 serum in PBS-Tween 20 (11 μL of sample in 100 μL of PBS-Tween-20). CSF should be tested undiluted. Shake the samples with vortex after thawing.
-
2.1.2.2
For sample titration, continue with dilutions of 1:10 (1:100 to 1:1000 to 1:10,000 and so on, until titration has been reached).
-
2.1.3
Analytical procedure
-
2.1.3.1
Method
-
i)
Dispense 30 μL of previously diluted serum or undiluted CSF in the well of the glass holder, avoiding bubble formation, using the polystyrene base as a reference.
-
ii)
Dispense all the samples of the series before starting the incubation.
-
iii)
Initiate the incubation by placing the biochips with transfected cells on the glass support, ensuring that the serum is in contact with the biochip and avoiding cross-contamination; incubate for 30 min at room temperature.
-
iv)
Washing: immerse the slides with biochips in a beaker containing PBS-Tween-20, and then immerse them in the appropriate PBS-Tween-20 containing cuvette for 5 min (if available, gently shake with a rotary stirrer).
-
v)
Dispense 30 μL of conjugated antibody (fluorescein anti-human IgG antiserum) in the wells.
-
vi)
Remove the biochip slides from the cuvettes one at a time and quickly dry the back and sides of the slide with absorbent paper, then immediately place it in the appropriate slots of the glass holder. Check that the biochip and conjugated antibody are in contact.
-
vii)
Incubate for 30 min at room temperature, in the dark.
-
viii)
Repeat the washing as in point iv, using fresh PBS-Tween-20.
-
ix)
Mount the slides with the biochip, placing the cover slides on the polystyrene support and place a drop (10 μL per well) of mounting liquid (glycerol/PBS) on each slide. Take out a slide at a time and dry the back and four sides with absorbent paper. The biochip slides must be delicately placed on the cover and slot in perfectly.
-
2.2
Observation and interpretation of results. Use fluorescence microscopes (excitation filter, 450–490 nm; color separator, 510 nm; blocking filter, 515 nm), with ×20 and ×40 magnifications. Results are interpreted blindly by two independent observers and defined as “positive” or “negative”; when interpretations differ, repeat the test. When interpreting results, keep in mind the general principle that the distribution of fluorescence across all the cells present on the biochip indicates a false positive since, by definition, transfection is always incomplete; therefore, fluorescence is distributed on only one part of the transfected cells in positive samples. Typically, the surface reactivity draws the outline of the cells, which is generally irregular, and extends along the cellular processes. Cell bodies are generally poorly fluorescent. Broadly homogeneous reactivity is likely non-specific and generated by apoptotic cells. Using biochips of non-transfected cells as controls help to rule out false positive results (in addition to using control samples from well-known healthy seronegative subjects). The AINI laboratory network is willing to evaluate doubtful results.
-
3.0
Quality control and sample storage
-
3.1
CBA
-
3.1.1
A positive internal control and a negative internal control should be included in each analytical session.
-
3.1.2
If the positive control does not produce the expected result, or if the negative control unexpectedly shows positive fluorescence, the entire analytical session must be repeated.
-
3.1.3
An external quality control scheme should be planned at least annually (e.g., AINI external quality control schemes).
-
3.2
Storage, see the document on cerebrospinal fluid analysis and the determination of oligoclonal bands.
-
4.0
Report
-
4.1
The following information should be reported:
-
i)
Type of sample (serum, CSF), with indication of the dilution.
-
ii)
Commercial CBA (first level): type of the test, and manufacturer (Euroimmun, Lübeck, Germany); in-house tests (second level): type of test (specify that the test is performed for research purpose).
-
iii)
Presence or absence of the detected NS-Ab, with the indication of the sample dilution (serum; CSF), and titer (if performed).
-
iv)
Comments: refer to the document on cerebrospinal fluid analysis and the determination of oligoclonal bands.
Rights and permissions
About this article
Cite this article
Zuliani, L., Zoccarato, M., Gastaldi, M. et al. Diagnostics of autoimmune encephalitis associated with antibodies against neuronal surface antigens. Neurol Sci 38 (Suppl 2), 225–229 (2017). https://doi.org/10.1007/s10072-017-3032-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3032-4