Abstract
Posture, gait and balance problems are very disabling symptoms in Parkinson’s disease (PD). An increased stride-to-stri de variability, reduction of automaticity and asymmetry of lower limbs function characterize parkinsonian gait. These features predispose to freezing of gait (FOG), which often leads to falls. The aim of this study was to evaluate how the modulation of asymmetry through physiotherapy might improve gait and reduce FOG, thus preventing falls. Twenty-eight PD patients entered a double-blind pilot feasibility controlled study and were evaluated at baseline and after 3 months of a rehabilitative program (performed twice a week) by means of the motor part of the Unified Parkinson’s Disease Rating Scale (UPDRS-III), Gait and Falls Questionnaire, Tinetti balance and gait scale, Short Physical Performance Battery (SPPB), European Quality of Life questionnaire. Patients were randomly assigned to three treatment arms: (1) worst side improvement; (2) best side improvement; (3) standard therapy. All study arms showed a significant improvement of the Tinetti and SPPB scores. BSI led to a greater improvement than ST in terms of UPDRS-III (p = 0.01); Tinetti total score (p = 0.05) and Tinetti gait subscore (p = 0.01). Our study confirms the efficacy of physical therapy in the treatment of PD and, more importantly, suggests that specific intervention tailored on individual feature (e.g., asymmetry of motor condition) might be even more effective than standard rehabilitative programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deficits in posture, gait and balance are disabling symptoms in Parkinson’s disease (PD) [1]. PD gait dysfunctions include a reduction of velocity and step length, decreased arm swing, and an increased cadence and stride-to-stride variability because of the reduction of stepping automaticity [2–8]. Another well-known feature, identifiable since the early stages [9], is an asymmetric motor function of lower limbs [10].
All these features are supposed to play a role in the pathogenesis of freezing of gait (FOG) [1], a gait disturbance characterized by “an episodic inability to generate effective stepping in the absence of any known cause other than parkinsonism or high-level gait disorders” [11]. Both instrumental [10, 12–14] and clinical evidences [8] support the pathogenic role of asymmetry in disrupting the rhythmic sequence of right–left antiphase activation of lower limbs during walking [15, 16].
Split-belt treadmill studies suggested a separate central pattern generators for each leg [17], which, although assuring a highly flexible gait control, are more susceptible to decompensate when their coupling is compromised [18]. Accordingly, in PD patients treated with bilateral deep brain stimulation of subthalamic nucleus, the asymmetric fine-tuning of stimulating parameters (i.e., the reduction of stimulation on the less affected side) might improve bilateral limb coordination and consequently FOG [14]. A study on patients with chronic hemiparesis found that those patients who naturally reduced the gait asymmetry by sacrificing the step length of the healthy (non-paretic) leg, displayed a more efficient gait pattern [19].
Assuming that gait asymmetry might predispose PD patients to gait impairment, FOG [10, 12] and falls [13, 20], we sought to evaluate whether specific rehabilitative programs modulating gait asymmetry might improve global walking performance in these patients.
Methods
Patients
Twenty-eight patients were enrolled. Inclusion criteria were: a diagnosis of PD according to UK Brain Bank criteria [21], Hoehn and Yahr stage II or III, medical treatment and clinical condition stable for at least 4 weeks. Exclusion criteria were: cognitive impairment (Mini Mental State Examination (MMSE) score <24) [22], orthopedic or major disease interfering with gait and balance, history of psychiatric or neurological illnesses (other than PD), depression [Hamilton Depression Rating Scale (HDRS) >17] [23].
Study protocol
This was a randomized controlled pilot study. Patients were blinded to the study protocol and aim; the neurologist assessing the patients was blinded to the group allocation. By means of random number generator, patients were randomly assigned to one of the three study groups: (1) physiotherapy aimed to potentiate the most affected body side (worst side improvement, WSI); (2) physiotherapy aimed to potentiate the least affected side (best side improvement, BSI); (3) physiotherapy aimed to potentiate both sides (standard treatment, ST) (Online Resource). Each group underwent physiotherapy twice a week for 3 months. Each session had duration of 1 h and included a first part of warming up, a final part of cooling down for all the groups. The active part of the session encompassed of the same type of exercises for all the three groups but the number of repetitions differed from group to group according to the study aim: the number of repetitions was the same for both body sides in the ST group; the number of repetition was doubled for the most affected side in the WSI group; the number was doubled for the least affected side in the BSI group (Supplementary Table for details). Medical treatment was kept stable throughout the study.
At baseline visit (T 0) demographic and clinical data were collected including Unified Parkinson Disease Rating Scale-motor score (UPDRS-III) [24] and Hoehn and Yahr stage and the sum of UPDRS-III items 27–30 defined the axial subscore was calculated; lateralized UPDRS items 20–26 were used for “UPDRS asymmetry” [10], defined as the ratio: (higher sum − lower sum)/(higher sum + lower sum). Cognitive abilities were tested by means of MMSE and Frontal Assessment Battery (FAB) [25]. Depression and anxiety were evaluated by means of HDRS [23] and Hamilton Anxiety Rating Scale (HARS) [26], respectively. Patients’ quality of life was assessed using the European Quality of Life questionnaire (EQ-5D). The clinical assessment of gait, balance and of falling risk was performed by means of: Gait and Falls Questionnaire (GFQ) [27]; the balance and gait subscores of Tinetti scale [28], and the gait, balance and sit and go time parts of the Short Physical Performance Battery (SPPB) [29]. One month after the beginning of the study (T 1), patients were evaluated by means of the Tinetti scale. At the end of the study (T 2), patients underwent the same assessment as at baseline. Finally, 1 month after the end of the program, patients were evaluated by means of Tinetti and SPPS scale (T 3). Patients and their next of kin were asked to keep a diary of falls during all the study period. Primary outcome were UPDRS-III, Tinetti scale, and SPPB; secondary outcomes were FOG-Q, number of falls and EQ-5. Medications were expressed as levodopa daily dose equivalent (LEDD) [30].
The local ethical committee approved the study protocol, all patients agreed to participate and signed an informed consent form.
Statistical analysis
Between groups analyses: groups were compared by means of Kruskal–Wallis ANOVA by Ranks at each study visit (T 0, T 1, T 2, and T 3) and in case of significant effect of the group factor, post hoc analysis was performed by means of Mann-Whitney U test.
Within-group analyses: Friedman ANOVA for repeated measures was used to compare changes in motor function parameters in each group of subjects across the study period and in case of significant effect, Wilcoxon matched pair test was used for post hoc analysis. To simplify data analysis, we only considered the comparisons with T 0 values. Categorical data were compared by means of chi2 test using Yates correction as needed. Values were expressed as mean ± standard deviation (range). Statistica 7.0 (StatSoft, Tulsa, OK) software was used for all statistical analyses. All tests were two-sided with a level of significance set at P < 0.05.
Results
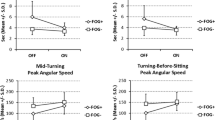
At baseline, groups did not differ in demographic and clinical variables (Table 1). The effects of the three treatment strategies are shown in Table 2 and Figs. 1 and 2. Evaluation of the within-group change over time revealed a significant effect for all the outcome measures in all the groups except for the variable SPPB balance in the WSI group (Friedman ANOVA P = 0.097). On post hoc analysis we found that all groups improved at UPDRS III–AXIAL and both WSI and BSI improved at UPDRS III–total score (see Table 2 for P values). UPDRS-III asymmetry resulted significantly improved only in ST group (Table 2). When comparing T 2 and T 3 to T 0, all groups significantly improved in the Tinetti scale total score (P values ranging from 0.005 to 0.01; Fig. 1a) and its subscores balance (P values ranging from 0.005 to 0.02; Fig. 1b) and gait (P values ranging from 0.01 to 0.03; Fig. 1c). With respect to the SPPB scale, BSI improved in all the comparisons for either total scores or subscores (P values ranging from 0.008 to 0.04, Fig. 2a–d), except for the comparison T 3 vs. T 0 at the balance subscore (Fig. 2c). WSI groups significantly improved with respect to T 0 when comparing the total scores and sit and go subscore at T 2 (P = 0.01 and 0.04) and T 3 (P = 0.01 and 0.03, Fig. 2a, c), and when comparing the gait subscore at T 2 vs. T 0 (P = 0.04; Fig. 2b). ST groups significantly improved with respect to T 0 when comparing the total score and the gait subscore at T 2 (P = 0.005 and P = 0.03) and T 3 (P = 0.005 and P = 0.04), when comparing the balance subscore at T 3 vs. T 0 (P = 0.03), and the sit and go subscore at T 2 vs. T 0 (P = 0.03; Fig. 1b).
Magnitude of change at Tinetti scale—total (a) and subscores balance (b) and gait (c). All groups significantly improved when comparing T 2 and T 3 with T 0 with respect the total score (P values ranging from 0.005 to 0.01; panel a), balance subscore (P values ranging from 0.005 to 0.02; panel b), and gait subscore (P values ranging from 0.01 to 0.03; panel c). Asterisk Tinetti scale–gait subscore, was higher in BSI than ST group at T 3 (P = 0.01)
Magnitude of change (scores at T 2 or T 3–scores at T 0) at SPPB scale, total (a) and subscores gait (b), balance (c) and sit and go (d). BSI improved in all the comparisons for either total scores or subscores (P values ranging from 0.008 to 0.04, panels a–d), except for the comparison T 3 vs. T 0 at the balance subscore (panel c). WSI groups significantly improved with respect to T 0 when comparing the total scores and sit and go subscore at T 2 (P = 0.01 and 0.04) and T 3 (P = 0.01 and 0.03, panels a and c), and when comparing the gait subscore at T 2 vs. T 0 (P = 0.04; panel b). ST groups significantly improved with respect to T 0 when comparing the total score and the gait subscore at T 2 (P = 0.005 and P = 0.03) and T 3 (P = 0.005 and P = 0.04), when comparing the balance subscore at T 3 vs. T 0 (P = 0.03), and the sit and go subscore at T 2 vs. T 0 (P = 0.03; panel b)
To evaluate an across-groups change over time, the comparison of the magnitudes of change with respect to baseline (T 0) revealed that the reduction of the UPDRS III and of Tinetti scale–gait subscore, were greater in BSI than ST group at T 3 (P = 0.01 for both comparisons; Table 2; Fig. 1c). They also differed as a trend at the Tinetti total score (at T 2 and T 3; p = 0.06 and p = 0.05, respectively), SPPB sit and go time (at T 3, p = 0.08).
No significant effect was found for VAS and GFQ; the number of falls registered during the study period did not differ among groups (2.2 ± 2.9, 3.4 ± 5.7, and 1.5 ± 3.8 for WSI, BSI and ST, respectively).Finally BSI also improved at HDRS (see Table 2 for P values).
Discussion
Our study confirms that physical therapy improves mobility and stability in PD patients [31–33] and, it suggests that new protocols, i.e., an asymmetric one, potentiating the body side which is less affected by PD symptoms, might be a successful practise, even more efficacious than conventional training.
PD is an asymmetric disorder [34] and great attention has been recently paid to the contribution of asymmetry in the pathophysiology of gait [10, 12, 14, 35] and balance disorders [13, 36]. Our pilot study suggests that an asymmetric training might be a useful rehabilitation strategy in PD. Our data propose that patients who underwent a training potentiating the less affected side improved in motor functions (UPDRS-III) and gait (Tinetti scale-gait subscore) more than patients who underwent a standard training. The improvement in the BSI group might be related to the fact that the less impaired side is more susceptible to training and more suitable for compensatory adaptive strategies. Accordingly, we recently demonstrated that the reduction of DBS amplitude for the hemisphere contralateral to the less affected leg improved lower limbs coordination and reduced FOG duration and frequency in PD patients [14]. This might be related to more residual brain plasticity in cortical–subcortical areas controlling the least affected side, which might better compensate for the impairment of locomotor generators. Several neurophysiological studies have disclosed an asymmetric plasticity when comparing the two hemispheres in PD patients; indeed, a recent study showed that clinically asymmetric patients with PD had a heightened response to a plasticity protocol (paired associative stimulation, PAS) using transcranial magnetic stimulation in the less affected hemisphere, in contrast to absent PAS response in the more affected hemisphere [37]. According to the authors, increased motor cortical plasticity might be consistent with a functional reorganization of sensorimotor cortex with compensatory aims [37].
A study on adaptive training in hemiparetic patients further confirmed how a compromised nervous system is still capable of normalizing gait when using split-belt treadmill paradigms [38, 39]. It has been showed that an important neural strategy to counter acta lag shift between legs in patients with limping gait is to shorten the step length of the leg with the longer stride [19], again supporting the compensative role of the less (or no) affected side.
Given the observation that the improvement in the depression scale was only detected in the BSI arm, another possible explanation is that training the most performing side lead to an improvement of its mobility more easily perceived by the patient. The sense of accomplishment and success may have led to a virtuous circle, impacting the outcome.
Notably, the UPDRS asymmetry score improved only in patients enrolled in the ST group, probably as a consequence of a standard balanced rehabilitative approach. However, such effect did not translate into a clinical improvement; in keeping with the established notion that asymmetry motor score is not related to gait asymmetry [10]. When considering the falls rate during the study period, no significant change emerged across groups. Although the short time period over which fall frequencies were monitored limits the relevance of this observation, it is worthy to report this since any improvement in mobility and gait could have increased the risk of falls [40].
The limitations of the present study are the small sample size and the lack of an objective assessment of gait parameters, although the double-blind design gives reliability to our results. We also acknowledge the limits of having used a short form of quality of life scale, which might have been not sensitive enough to detect changes; indeed, in spite of an improvement of stability and mobility, we did not detect any improvement in EQ-5. The short follow-up period is another limitation, especially because we cannot speculate on the duration of the beneficial effects of each training protocol.
Conclusions
Our pilot trial nicely suggests that rehabilitative intervention should be tailored on patients’ clinical features, such as motor asymmetry. To further support this concept, studies with larger sample and longer follow-up are encouraged.
Abbreviations
- BSI:
-
Best side improvement
- FAB:
-
Frontal Assessment Battery
- FOG:
-
Freezing of gait
- GFQ:
-
Gait and Falls Questionnaire
- HARS:
-
Hamilton Anxiety Rating Scale
- HDRS:
-
Hamilton Depression Rating Scale
- LEDD:
-
Levodopa daily dose equivalent
- MMSE:
-
Mini Mental State Examination
- PAS:
-
Paired associative stimulation
- PD:
-
Parkinson’s disease
- SPPB:
-
Short Physical Performance Battery
- ST:
-
Standard treatment
- UPDRS-III:
-
Unified Parkinson Disease Rating Scale-motor score
- VAS:
-
Visual analogic scale
- WSI:
-
Worst side improvement
References
Nutt JG, Horak FB, Bloem BR (2011) Milestones in gait, balance, and falling. Mov Disord 26(6):1166–1174
Blin O, Ferrandez AM, Serratrice G (1990) Quantitative analysis of gait in Parkinson patients: increased variability of stride length. J Neurol Sci 98(1):91–97
Blin O, Ferrandez AM, Pailhous J et al (1991) Dopa-sensitive and dopa-resistant gait parameters in Parkinson’s disease. J Neurol Sci 103(1):51–54
Morris ME, Iansek R, Matyas TA et al (1994) Ability to modulate walking cadence remains intact in Parkinson’s disease. J Neurol Neurosurg Psychiatry 57(12):1532–1534
Morris ME, Iansek R, Matyas TA et al (1994) The pathogenesis of gait hypokinesia in Parkinson’s disease. Brain 117:1169–1181
Hausdorff JM, Cudkowicz ME, Firtion R et al (1998) Gait variability and basal ganglia disorders: stride-to-stride variations of gait cycle timing in Parkinson’s disease and Huntington’s disease. Mov Disord 13(3):428–437
Hausdorff JM, Schaafsma JD, Balash Y et al (2003) Impaired regulation of stride variability in Parkinson’s disease subjects with freezing of gait. Exp Brain Res 149(2):187–194
Schaafsma JD, Giladi N, Balash Y et al (2003) Gait dynamics in Parkinson’s disease: relationship to Parkinsonian features, falls and response to levodopa. J Neurol Sci 212(1–2):47–53
Baltadjieva R, Giladi N, Gruendlinger L et al (2006) Marked alterations in the gait timing and rhythmicity of patients with de novo Parkinson’s disease. Eur J Neurosci 24(6):1815–1820
Plotnik M, Giladi N, Balash Y et al (2005) Is freezing of gait in Parkinson’s disease related to asymmetric motor function? Ann Neurol 57(5):656–663
Giladi N, Nieuwboer A (2008) Understanding and treating freezing of gait in parkinsonism, proposed working definition, and setting the stage. Mov Disord 23(Suppl 2):S423–S425
Plotnik M, Giladi N, Hausdorff JM (2008) Bilateral coordination of walking and freezing of gait in Parkinson’s disease. Eur J Neurosci 27(8):1999–2006
Yogev G, Plotnik M, Peretz C et al (2007) Gait asymmetry in patients with Parkinson’s disease and elderly fallers: when does the bilateral coordination of gait require attention? Exp Brain Res 177(3):336–346
Fasano A, Herzog J, Seifert E et al (2011) Modulation of gait coordination by subthalamic stimulation improves freezing of gait. Mov Disord 26(5):844–851
Prokop T, Berger W, Zijlstra W et al (1995) Adaptational and learning processes during human split-belt locomotion: interaction between central mechanisms and afferent input. Exp Brain Res 106(3):449–456
Sadeghi H, Allard P, Prince F et al (2000) Symmetry and limb dominance in able-bodied gait: a review. Gait Posture 12(1):34–45
Choi JT, Bastian AJ (2007) Adaptation reveals independent control networks for human walking. Nat Neurosci 10(8):1055–1062
Dietz V (2002) Do human bipeds use quadrupedal coordination? Trends Neurosci 25(9):462–467
Balasubramanian CK, Bowden MG, Neptune RR, Kautz SA (2007) Relationship between step length asymmetry and walking performance in subjects with chronic hemiparesis. Arch Phys Med Rehabil 88(1):43–49
Plotnik M, Giladi N, Dagan Y et al (2011) Postural instability and fall risk in Parkinson’s disease: impaired dual tasking, pacing, and bilateral coordination of gait during the “ON” medication state. Exp Brain Res 210(3–4):529–538
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56(1):33–39
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Hamilton M (1960) Arating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Fahn S, Elton R, Committee MotUD (1987) Recent developments in Parkinson’s disease. Macmillan Health Care Information, Folorham Park
Dubois B, Slachevsky A, Litvan I et al (2000) The FAB: a frontal assessment battery at bedside. Neurology 55(11):1621–1626
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32(1):50–55
Giladi N, Shabtai H, Simon ES et al (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6(3):165–170
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34(2):119–126
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49(2):M85–M94
Tomlinson CL, Stowe R, Patel S et al (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Morris ME, Martin CL, Schenkman ML (2010) Striding out with Parkinson disease: evidence-based physical therapy for gait disorders. Phys Ther 90(2):280–288
Fox SH, Katzenschlager R, Lim SY et al (2011) The Movement Disorder Society Evidence-Based Medicine Review Update: treatments for the motor symptoms of Parkinson’s disease. Mov Disord 26(Suppl 3):S2–S41
Tomlinson CL, Patel S, Meek C et al (2012) Physiotherapy versus placebo or no intervention in Parkinson’s disease. Cochrane Database Syst Rev 8:CD002817
Djaldetti R, Ziv I, Melamed E (2006) The mystery of motor asymmetry in Parkinson’s disease. Lancet Neurol 5(9):796–802
Plotnik M, Hausdorff JM (2008) The role of gait rhythmicity and bilateral coordination of stepping in the pathophysiology of freezing of gait in Parkinson’s disease. Mov Disord 23(Suppl 2):S444–S450
Skelton DA, Kennedy J, Rutherford OM (2002) Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing 31(2):119–125
Kojovic M, Bologna M, Kassavetis P et al (2012) Functional reorganization of sensorimotor cortex in early Parkinson disease. Neurology 78(18):1441–1448
Reisman DS, Wityk R, Silver K et al (2009) Split-belt treadmill adaptation transfers to overground walking in persons poststroke. Neurorehabil Neural Repair 23(7):735–744
Reisman DS, Wityk R, Silver K et al (2007) Locomotor adaptation on a split-belt treadmill can improve walking symmetry post-stroke. Brain 130(Pt 7):1861–1872
Nieuwboer A, Kwakkel G, Rochester L et al (2007) Cueing training in the home improves gait-related mobility in Parkinson’s disease: the RESCUE trial. J Neurol Neurosurg Psychiatry 78(2):134–140
Conflict of interest
Authors declare no conflict of interest in regard to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ricciardi, L., Ricciardi, D., Lena, F. et al. Working on asymmetry in Parkinson’s disease: randomized, controlled pilot study. Neurol Sci 36, 1337–1343 (2015). https://doi.org/10.1007/s10072-015-2082-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-015-2082-8