Abstract
Objectives
To evaluate specificity, level, and avidity of antineutrophil cytoplasmic antibodies (ANCA) in systemic lupus erythematosus (SLE). There are no studies of ANCA avidity in SLE.
Methods
Level (ELISA) and avidity (ELISA) of myeloperoxidase (MPO-), proteinase 3 (PR3-), lactoferrin (LF-), cathepsin G, elastase (EL-), and bactericidal/permeability increasing protein (BPI)-ANCA in 142 SLE patients were studied. SLE activity was measured by SLEDAI-2 K. 25/40 ANCA-positive patients were immunoserologically followed (12 ± 2 months).
Results
40/142 (28.2%) SLE patients were ANCA-positive: LF- (21/40), MPO- (19/40), EL- (6/40), PR3- (3/40), and BPI-ANCA (1/40). Only LF-ANCA were associated with renal manifestations (p < 0.05), and positive predictive value for renal involvement in ANCA-positive SLE was 76.2%. LF-ANCA-positive patients had higher SLEDAI-2 K (p < 0.05) and more frequently had anti-dsDNA (p < 0.05), low C3 (p < 0.001), and low C4 (p < 0.05) than LF-ANCA-negative patients. LF-ANCA level was in a positive correlation with SLEDAI-2 K, anti-dsDNA, and anti-C1q (p < 0.01) and in a negative correlation with C3 and C4 (p < 0.05). LF-ANCA avidity was higher than MPO-, EL-, PR3-, and BPI-ANCA avidity (p < 0.01). In LF-ANCA-positive patients, renal manifestations were associated with higher LF-ANCA level (p < 0.01) and avidity (p < 0.05). Based on LF-ANCA level and avidity, the receiver operating characteristic curves for discriminating patients with and without renal involvement had areas under the curves of 0.988 (95% CI: 0.949–1.00) and 0.813 (95% CI: 0.607–1.00), respectively. After the follow-up period, number of LF-ANCA-positive patients decreased (p < 0.01).
Conclusions
In contrast to other ANCAs, only LF-ANCA level correlated with activity and standard serological SLE markers. LF-ANCA level and avidity might be biomarkers of renal involvement in SLE. LF-ANCA are promising serological marker in SLE.
Key Points • LF- and MPO-ANCA were most frequently found, while EL-, PR3-, and BPI-ANCA were rarely detected in SLE. • In contrast to other ANCAs, only LF-ANCA were associated with renal involvement, and their level correlated with the activity and standard serological markers of SLE. • LF-ANCA avidity was higher than other ANCAs’ avidity; LF-ANCA level and avidity might be useful biomarkers of renal manifestations in SLE. • Detection of ANCA specificity, level, and avidity may help in the diagnosis of particular clinical SLE phenotypes. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inadequate clearance of dead cells in systemic lupus erythematosus (SLE) triggers autoimmunity, characterized by the production of antibodies specific to nuclear and cytoplasmic components [1]. It is well known that various SLE biomarkers are neutrophil-related, but the exact importance of antineutrophil cytoplasmic antibodies (ANCA) in SLE has not been defined.
In SLE, special population of proinflammatory neutrophils (low-density granulocytes) displays an increased capacity to form neutrophil extracellular traps (NETs) [1]. NETs are structures composed of neutrophil dsDNA, histones, and granular proteins which arise by “neutrophil explosion,” referred to as NETosis. NETosis, as a specific form of neutrophil death, is characterized by the release of nuclear and granular contents into the extracellular space [2]. NETs, triggered by microbial products, are important part of innate immune response, but NETs persistence contributes to the loss of autotolerance [1, 2]. In SLE, NETs are poorly cleared and stimulate plasmacytoid dendritic cells (pDCs) to produce type I interferon (IFN) through Toll-like receptor 9 stimulation [3]. NETs and IL-17 are abundant in discoid skin lesions and in kidneys of SLE patients [1]. Post-translational modification of nuclear and cytoplasmic proteins during NETosis induces the appearance neoepitopes that stimulate the acquired immune response and initiate autoimmunity [4]. In SLE, neutrophil activation, NETs production, and reduced clearance of NETs all together contribute to persistence of the inflammatory process [1, 3].
Histones, MPO, and elastase (EL) are the main NETs components involved in tissue inflammation and destruction [5]. On the other hand, lactoferrin (LF), a multifunctional, iron-binding protein, was shown to function as an endogenous inhibitor of NETs formation [6]. Aggregated NETs may degrade inflammatory cytokines, serine proteases, and chemokines [7]. Lactoferrin and aggregated NETs have important role in termination of the inflammatory response [6, 7].
It has been shown that ANCA enhance NETs formation and activate the complement system [1, 3]. Also, in new-onset SLE, there is a correlation between ANCA titers, disease activity, and the anti-dsDNA antibody levels [8]. ANCA was an independent risk factor for poor renal outcome in lupus nephritis (LN); a significant correlation between the presence of ANCA and crescent formation has been found [9].
Previous studies were focused on the association between ANCA and clinical manifestations of SLE [10], but few or no studies have investigated the target antigens and avidity of ANCA in SLE patients. The clinical relevance of the autoantibody avidity has been found in patients with anti-phospholipid syndrome (anti-beta2-glycoprotein I) and SLE (anti-dsDNA) [11, 12].
Although earlier studies have demonstrated that LF-ANCA-positive SLE patients had higher disease activity than LF-ANCA-negative patients [13,14,15], the exact prevalence, level, LF-ANCA avidity, and the clinical phenotype of LF-ANCA-positive SLE patients have not been investigated.
The primary objective of this study is to evaluate the clinical relevance of the presence, specificity, level, and avidity of ANCA in SLE. We studied the frequency and the profile of ANCA: myeloperoxidase (MPO), proteinase-3 (PR3), LF, EL, cathepsin-G (CAT-G), and bactericidal/permeability-increasing protein (BPI) and the association of ANCA with clinical and serological parameters of SLE activity.
To the best of our knowledge, this is the first study of ANCA avidity in SLE. Our study demonstrated that the LF-ANCA level and avidity might be biomarkers of renal involvement and disease activity of SLE.
Patients and methods
Patients
Serum samples from 142 consecutive adult patients (118 F, 24 M, aged 40.7 ± 15.9 years, range 18–78) with idiopathic SLE and 20 healthy individuals (15 F, 5 M, aged 43.5 ± 13.1 years) were collected between 2014 and 2018, at the Clinical Center of Serbia (CCS). SLE was diagnosed according to the ACR criteria [16]. Patients had met the following inclusion criteria: (1) newly diagnosed disease 44/142 (31%) or (2) SLE relapse 98/142 (69%), not treated with cyclophosphamide or methylprednisolone pulses for at least 3 months before the inclusion in the study. At the point of blood sampling, maximal prednisone doses were 20 mg/48 h. Lupus flare was defined as any increase in SLEDAI-2 K score by at least 3 points compared to the previous control [17]. None of our patients had ulcerative colitis (UC), autoimmune hepatitis (AIH), primary sclerosing cholangitis (PSC), and a history of propylthiouracil, isoniazid, or hydralazine use (drugs that might induce ANCA positivity). The study was approved by the Ethics Committee of the CCS.
The patients’ demographic, clinical, and serological data, as well SLE duration and current therapy, were reviewed retrospectively (Table 1). Disease activity index (SLEDAI-2 K) was determined based on the presence of symptoms and signs and laboratory parameters [18]. The value of SLEDAI-2 K ≥ 7 indicated moderately to highly active disease, whereas SLEDAI-2 K < 7 indicated a low SLE activity [19]. 25/40 ANCA-positive patients were immunoserologically followed for 12 ± 2 months.
Serological parameters
ANCA level
IgG ANCA to six different antigens, MPO, PR3, LF, EL, BPI, and CAT-G, were detected in patients’ sera using a semi-quantitative commercial enzyme-linked immunosorbent assay (ELISA) (ANCA Profile, Euroimmun, Lübeck, Germany). ANCA index was calculated as the ratio of the patient sample optical extinction/calibrator extinction × 0.2 (ratio for PR3-ANCA index, multiplied by 1.4). Based on the value of obtained indices for each antigen, ANCA levels were interpreted as negative (< 1.0), weakly positive (≥ 1.0 to < 2.0), moderately positive (≥ 2.0 to < 5.0), and strongly positive (≥ 5.0). Twenty healthy controls were ANCA-negative for all six antigens (index < 1.0).
ANCA avidity
Avidity was tested using the ANCA Profile immunosorbent assay (ELISA) (Euroimmun, Lübeck, Germany), as previously described [20]. Briefly, 100 μL of serum diluted 1:100 in sample buffer was added in duplicate to each well coated with PR3, MPO, LF, EL, Cat G, and BPI. After an incubation of 30 min at room temperature and washing, wells were exposed to 200 μL of 5M urea solution, or phosphate-buffered saline (PBS) for 10 min. After washing three times, wells were incubated with 100 μL peroxidase-labelled anti-human IgG for 30 min at room temperature, followed again by three washing cycles. One hundred microliters of a chromogenic substrate solution was added, and the reactions were stopped after 15 min by addition of 100 μL stop solution per well. The reactions were read immediately at a wavelength of 450 nm, using a reference wavelength of 650 nm. ANCA avidity was expressed as a relative avidity index (RAI) that was calculated for each specimen. RAI was calculated as the percentage of reactivity remaining in the urea-treated wells according to formula: extinction of the patient sample with 5 M urea/extinction of sample with PBS × 100. To calculate RAI, the optical extinction of sample with PBS must be higher than 0.150. ANCA avidity was not calculated in sera of healthy controls because extinctions with PBS to six ANCA antigens were below 0.150.
Other autoantibodies
Presence and titer of antinuclear antibodies (ANA) were measured by indirect immunofluorescence (IIF) using HEp-2 cells (Euroimmun, Lübeck, Germany). Anti-dsDNA IgG antibodies were detected by IIF using the Crithidia luciliae test (Euroimmun, Lübeck, Germany). Anti-histone, anti-nucleosomal, anti-C1q, anticardiolipin G/M, and anti-β2-glycoprotein I G/M antibodies were measured by quantitative ELISA, according to the protocols provided by the manufacturer (Euroimmun, Lübeck, Germany). Normal value for all ELISA tests was < 20 U/mL.
Complement components
C3 and C4 levels of complement were measured by nephelometry. Reference values for C3 were 0.8–2.1 g/L and for C4 0.1–0.4 g/L.
Statistical analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS), version 21.0 for Windows. The methods of measurement of central tendency (arithmetic mean and median), variability (variation interval, standard deviation and interquartile rank, and relative numbers), and methods of inferential statistics were used. Statistical methods used for related and independent samples included χ2 test, Fisher’s exact probability test, McNemar’s test, Mann–Whitney U test, Wilcoxon test of equivalent pairs, Kruskal–Wallis test, and t-test. Receiver operating characteristic (ROC) curve and the area under the curve (AUC) were used to assess the diagnostic value of LF-ANCA level and avidity in discriminating SLE patients with and without renal involvement. Spearman’s rank-order correlation coefficient was determined for the investigation of correlation between LF-ANCA levels with SLEDAI-2 K and immunoserological parameters (antibody and complement levels).
Distribution of values was verified using the Shapiro–Wilk test.
Results
Comparison of demographic, clinical, and immunoserological parameters between SLE patients with and without ANCA
40/142 (28.2%) SLE patients were ANCA-positive, while 102/142 (71.8%) were ANCA-negative (using ELISA ANCA Profile test: LF, MPO, PR3, EL, BPI, and CAT-G). Demographic and clinical data of these patients are shown in Table 1. We found that SLE patients in the ANCA-positive group were older, due to older male patients (Table 1). There was no statistically significant difference in frequency of newly diagnosed SLE between ANCA-positive (42.5%) and ANCA-negative (26.5%) SLE patients (p > 0.05). ANCA-negative SLE patients statistically significantly more frequently had mucocutaneous manifestations (p < 0.05); there was no difference in the frequency of other clinical manifestations. No statistical significance was observed in the presence of ANA, anti-dsDNA, and decreased complement levels between these two study groups (p > 0.05) (Table 1). Only the concentrations of anti-nucleosome antibodies were statistically significantly higher in ANCA-positive SLE patients (p < 0.05), while there was no difference in the frequency of anti-histone and anti-nucleosome antibodies in the study groups (p > 0.05). There was no difference in the presence and median of anti-C1q, aCL G/M, and anti-beta2-GPI G/M antibodies in ANCA-positive and ANCA-negative SLE patients (p > 0.05).
ANCA level and ANCA avidity in SLE patients
31/40 (77.5%) ANCA-positive SLE patients had monospecific ANCA, while 8/40 (20%) had ANCA specific to two target antigens, and only one patient (2.5%) had ANCA specific to three target antigens.
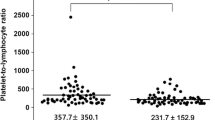
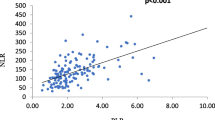
In 40 ANCA-positive SLE patients, LF-ANCA had 21/40 (52.5%), MPO-ANCA had 19/40 (47.5%), EL-ANCA had 6/40 (15%), and PR3-ANCA had 3/40 (7.5%) patients. Only one patient (2.5%) had BPI-ANCA, and no patients had CAT-G-ANCA (Fig. 1a). 17/21 (80.9%) had monospecific LF-ANCA, while 2/21 (9.5%) patients simultaneously had MPO- and LF-ANCA, 1/21 (4.7%) had polyspecific MPO-, EL-, and LF-ANCA, and 1/21 (4.7%) had BPI- and LF-ANCA. However, there was no statistically significant difference between ANCA levels (expressed as index) specific to MPO and LF (p > 0.05). LF-ANCA levels in SLE patients (n = 21) were significantly higher (median 1.8, range 1.02–7.39) than LF-ANCA level (median 0.06, range 0.02–0.29) in healthy controls (n = 20) (p < 0.001). Furthermore, LF-ANCA avidity (expressed as RAI) (median 42.12, range 16.67–90.0%) was statistically significantly higher than MPO-ANCA (median 10.15, range 4.0–14.61%), EL-ANCA (median 8.4, range 4.6–12.5%), PR3-ANCA (median 6.8, range 5.5–8.5%), and BPI-ANCA (6.4%) avidity (p < 0.01) (Fig. 1b).
a ANCA Profile in 40 ANCA-positive SLE patients (ANCA levels expressed semi-quantitatively by ANCA index values: slightly positive (≥ 1.0–2), positive (≥ 2.0–5.0), and strongly positive (≥ 5.0)). b The median of the relative avidity index (RAI) of different ANCA specificities in 40 ANCA-positive SLE patients. c The median of LF-ANCA RAI in SLE patients with and without renal involvement. d ROC curve with AUC values for discriminating SLE patients with and without renal involvement based on LF-ANCA avidity. e Positive correlation between LF-ANCA index and anti-dsDNA titers in 40 ANCA-positive patients. f Positive correlation between LF-ANCA index and anti-dsDNA titers in 21 LF-ANCA-positive patients
Comparison of clinical and immunoserological parameters between SLE patients with and without LF-ANCA
There was no statistically significant difference in frequency of newly diagnosed SLE between LF-ANCA-positive (38%) and LF-ANCA-negative (47%) SLE patients (Table 2). SLEDAI-2 K in LF-ANCA-positive persons was statistically significantly higher than SLEDAI-2 K in LF-ANCA-negative patients (p < 0.05). LF-ANCA-positive SLE patients statistically significantly more frequently had renal involvement (proteinuria > 0.5 g/24 h and/or urinary casts and/or hematuria and/or leukocyturia) (p < 0.05). For ANCA-positive SLE patients, positive predictive value (PPV) of LF-ANCA for renal involvement was 76.2%. LF-ANCA-positive patients with renal manifestations (n = 16) had a statistically significantly higher LF-ANCA index (median 1.57, range 1.21–7.39) than LF-ANCA-positive patients (n = 5) without renal manifestations (median 1.12, range 1.02–1.25) (p < 0.01). LF-ANCA index at the cutoff value of 1.23 has sensitivity of 93.8% and specificity of 80% for renal involvement; AUC was 0.988 (95% CI: 0.949–1.00). Furthermore, LF-ANCA-positive patients with renal manifestations (n = 16) had higher LF-ANCA avidity (median 45.37, range 21.0–90.0%) than LF-ANCA-positive patients (n = 5) without renal manifestations (median 23.5, range 16.67–45.0%) (p < 0.05) (Fig. 1c). LF-ANCA avidity at the cutoff value of 31.35% has sensitivity of 81.3% and specificity of 80% for renal involvement. Based on LF-ANCA avidity, the ROC curve for discriminating patients with renal involvement showed that the AUC is 0.813 (95% CI: 0.607–1.00) (Fig. 1d).
LF-ANCA-negative patients more frequently had arthralgia and synovitis (p < 0.05). LF-ANCA-positive patients significantly more frequently had anti-dsDNA antibodies (p < 0.05) and decreased C3 (p < 0.001) and C4 complement components (p < 0.05) and lower concentration of C3 (p < 0.05) (Table 2). The presence of MPO-ANCA and EL-ANCA, unlike LF-ANCA, were not associated with renal lesions, decreased C3 and C4 complement levels, or a positive anti-dsDNA.
Correlation between LF-ANCA levels and studied parameters in 40 ANCA-positive SLE patients
The correlations between specific immunoserological parameters in 40 ANCA-positive SLE patients are shown in Table 3. In ANCA-positive patients, a highly significant positive correlation was found between LF-ANCA index and anti-dsDNA titers (p < 0.001, Spearman’s coefficient 0.526) (Fig. 1e) and SLEDAI-2 K score (p < 0.01). Also, a statistically significant, moderately positive correlation between LF-ANCA level and anti-histone antibody concentration (p < 0.05) and a highly statistically significant moderately positive correlation between LF-ANCA levels and anti-C1q concentration (p < 0.01) have been found. In addition, a statistically significant moderately negative association was found between LF-ANCA and C3 (p < 0.05) and C4 concentrations (p < 0.05) and MPO-ANCA level (p < 0.05). Furthermore, in 21 LF-ANCA-positive patients, a significantly positive correlation was found between LF-ANCA index and anti-dsDNA titers (p < 0.01, Spearman’s coefficient 0.656) (Fig. 1f). We did not find correlation between LF-ANCA avidity and anti-dsDNA, anti-nucleosomal, anti-histone, C3, and C4 concentrations, respectively (p > 0.05).
Immunoserological parameters after the follow-up period
In 25/40 ANCA-positive SLE patients, after the follow-up period of 12 ± 2 months, immunoserological parameters were re-assessed. There was a highly statistically significant decrease in the number of LF-ANCA-positive patients (p < 0.01) (Table 4). 8/11 patients with LF-ANCA became negative, while no patients with strong positivity were noted after the follow-up period. The number of patients with anti-dsDNA and low C3 significantly decreased (p < 0.05). A highly statistically significant decrease in anti-dsDNA antibody titers (p < 0.01) was observed, as well as a highly statistically significant increase in C3 concentration (p < 0.01) (Table 4).
Discussion
PR3-ANCA and MPO-ANCA are standard serological markers of the subset of small vessel vasculitides, known as ANCA-associated vasculitides (AAV) [21]. Furthermore, ANCA are also present in patients with drug-induced vasculitis and in lupus-like syndrome [22] and may be found in idiopathic connective tissue diseases, such as rheumatoid arthritis and SLE [8, 10]. Atypical pANCA are commonly detected in patients with inflammatory bowel diseases, mainly in UC, and some autoimmune liver diseases such as AIH and PSC [23]. In our previous study, we demonstrated higher concentrations of multi-specific ANCA in long-lasting (p < 0.05), left-sided UC (p < 0.001), and we found association of multi-specific ANCA with ANA and anti-smooth muscle antibodies (ASMA) in PSC [24]. Although the main target antigen of pANCA still remains to be identified, LF-ANCA were found in 3–50% of patients with UC and in 22–50% of patients with PSC [23].
Previous studies were focused on clinical manifestations in ANCA-positive SLE patients, but only a few have investigated the clinical importance of ANCA specificity and the potential role of “esoteric” or “minor” target ANCA antigens. According to the literature, the prevalence of ANCA in SLE patients ranges between 16.4 and 42% [8, 10, 25,26,27,28,29,30,31]. Table 5 shows the literature overview, together with our results in 142 SLE patients.
In our ANCA-positive group, SLE patients were older, due to older male patients (Table 1). It is well known that AAV are characterized by a slight male predominance and that the incidence of AAV increases with age [21].
Some studies have demonstrated that ANCA-positive patients had a higher incidence of certain clinical manifestations (serositis, renal and CNS involvement, myocarditis, pulmonary hemorrhage, livedo reticularis, venous thrombosis, and arthritis) [8, 10, 14, 32].
Kidney lesions were found in more than half of SLE patients with ANCA and contribute significantly to morbidity [8, 9]. Pan et al. and Pradhan et al. found that ANCA positivity was higher in patients with LN compared to patients without nephritis (p < 0.01, p < 0.05, respectively) [8, 31]. Yu et al. established that most of ANCA-positive patients (67.9%) had type IV LN, with a higher mortality rate compared to ANCA-negative patients; also, ANCA-positive patients more frequently had anti-dsDNA antibodies [33]. The rare presentation of SLE/AAV overlap syndrome has been recently described, in patients who fulfill both SLE and AAV classification criteria. AAV may occur before, after, or concomitantly with SLE. Most patients are women; rapidly progressive glomerulonephritis (with or without alveolar hemorrhage) is the most frequent presentation [34].
Additionally, positive anti-dsDNA, along with decreased C3 and C4 levels, were significantly more frequently detected in ANCA-positive than in ANCA-negative SLE patients, which is explained by the fact that the production of anti-chromatin and ANCA antibodies simultaneously occur following NETosis [1, 2, 35].
In our study, mucocutaneous lesions were more frequent in ANCA-negative patients (Table 1). Affection of joints, serous membranes, and hematological disorders were equally present in ANCA-positive and ANCA-negative SLE patients. Also, considering renal involvement, there was no statistically significant difference between ANCA-positive and ANCA-negative patients (Table 1), but further analysis revealed that the LF-ANCA-positive patients more frequently had renal lesions than LF-ANCA-negative patients (Table 2).
In the literature, the prevalence of LF-ANCA was 10 to 59%, while MPO-ANCA were reported in 0 to 54.5% of SLE patients (Table 5). As in the literature [10, 14, 15, 36], in our study, the most frequently detected antibodies were LF-ANCA (in 14.8% of all SLE patients and in 52.5% of ANCA-positive patients), MPO-ANCA (in 13.4% and 47.5%, respectively), and EL-ANCA (in 4.2% and 15%, respectively) (Fig. 1a). In contrast to our study, Manolova et al. found the predominance of PR3-ANCA (12.7%) and BPI-ANCA (23.6%) [37]. Turner-Stokes et al. demonstrated the predominance of MPO-ANCA (82%) and PR3-ANCA (7%) [38]. In other studies, as well as in ours, PR3-ANCA and BPI-ANCA were found only in a minority of SLE patients (2.1% and 0.7%, respectively). In our study, no patients were positive for CAT-G-ANCA (Fig. 1a). Significant differences in prevalence and specificity of ANCA in SLE published in the literature (Table 5) imply that more accurate characterization of target antigens and more sensitive and specific ELISA assays regarding ANCA classes and IgG subclasses distribution are necessary.
According to the results of numerous studies, there is no consensus regarding the association between the LF-ANCA and the disease activity. Chikazawa et al. showed that the presence of IgG LF-ANCA was associated with higher SLEDAI [15]. Spronk et al. found that levels of LF-ANCA, PR3-ANCA, and BPI-ANCA did not correlate with SLEDAI [27]. Caccavo et al. found that IgG LF-ANCA in medium/high concentrations were associated with higher disease activity, assessed by Systemic Lupus Activity Measure (SLAM) [14]. Similar to these results, we found a positive correlation between LF-ANCA level and SLEDAI-2 K (Table 3). Lee et al. showed a correlation between LF-ANCA positivity and both the disease duration and clinical flare-ups. After the follow-up period, we also demonstrated that LF-ANCA, but not MPO-ANCA, was associated with active SLE [13].
Spronk et al. found that ANCA prevalence was higher in patients who developed relapse than in those who did not (p < 0.01) [27].
IgG LF-ANCA in medium and high concentrations correlated with anti-dsDNA antibodies and anticardiolipin antibodies [14]. Furthermore, these antibodies were associated with specific clinical manifestations, such as skin involvement and serositis, and in medium/high concentrations, with Raynaud’s phenomenon, renal involvement, serositis, and a history of thrombosis [1]. On the other hand, Chikazawa et al. found no association of LF-ANCA and MPO-ANCA with any specific clinical manifestations [15]. Other authors demonstrated that ANCA-positive patients had significantly higher incidence of renal involvement. Anti-dsDNA and anti-Sm antibodies were significantly higher, while C3 and C4 were significantly decreased in ANCA-positive patients [8, 31]. In the study of Turner-Stokes et al., the ANCA-positive group had significantly higher anti-dsDNA and significantly lower serum C4 concentrations [38]. ANCAs influence the histological pattern of LN, and ANCA positivity has been associated with worse baseline renal function and more severe disease [38]. We demonstrated that LF-ANCA-positive patients more frequently had renal involvement, while LF-ANCA-negative patients more frequently had arthralgia and synovitis (Table 2). Chin et al. found that LF-ANCA were positive in 12/51 (23%) LN patients, and MPO-ANCA were positive only in 1/51 (1.9%) LN patients, suggesting that LF-ANCA is the most important antigen for renal involvement [39], similar to our findings (Table 2). In our study, in the group of ANCA-positive SLE patients, PPV of LF-ANCA for renal involvement was 76.2%. In 40 ANCA-positive SLE patients, we demonstrated a significantly positive correlation between LF-ANCA levels and anti-dsDNA titers (Fig. 1e), anti-histone, and anti-C1q antibodies, while a significantly negative correlation between LF-ANCA levels and C3 and C4 levels was found (Table 3). In addition, in 21 LF-ANCA-positive SLE patients, we found a significantly positive correlation between LF-ANCA levels and anti-dsDNA titers (Fig. 1f). In our study, contrary to LF-ANCA, MPO-ANCA and EL-ANCA were not associated with renal lesions, decreased C3 and C4 levels, or anti-dsDNA.
Furthermore, LF-ANCA level was higher in LF-ANCA-positive patients with renal manifestations in comparison with LF-ANCA-positive patients without renal manifestations (p < 0.01). In contrast to other ANCA specificities, only LF-ANCA had high avidity (Fig. 1b); patients with renal involvement had higher LF-ANCA avidity than LF-ANCA-positive patients without renal involvement (p < 0.05) (Fig. 1c), which imply a pathogenic potential of high-avidity LF-ANCA. To detect ANCA avidity in sera of our patients, 5 M urea treatment was used, allowing low-affinity antibodies to dissociate from their cognate antigen, while higher-affinity antibodies remained bound. RAI was calculated as the percentage of reactivity remaining in the urea-treated wells. This method has already been published [20, 40]. The importance of ANCA avidity has been already demonstrated in AAV. High avidity MPO-ANCA were associated with high AAV activity [41]. In granulomatosis with polyangiitis, PR3-ANCA avidity is increased only in patients with relapsing renal disease [20]. Zeng et al. [40] used 40% as the cut-off level for RAI of ANA; on the other hand, we used the ROC curve to calculate the cut-off RAI value of LF-ANCA in order to discriminate SLE patients with or without renal involvement.
The ROC curve analysis demonstrated that quantification of LF-ANCA level and avidity (Fig. 1d) could be used to predict renal involvement in SLE. It has been shown that LN patients with ANCA have a higher chronicity index than those without ANCA [42]. After the follow-up period, most of our LF-ANCA-positive patients became LF-ANCA-negative; also, anti-dsDNA significantly decreased, while C3 and C4 increased (Table 4).
It is known that LF has a physiological role in binding iron ions (as antioxidant), reducing the production of proinflammatory OH− ions. Therefore, LF-ANCA in SLE patients may inhibit these important protective functions of LF and lead to an increase in OH− ion production and, consequently, to inflammation. LF inhibits the release of proinflammatory cytokines such as IL-6 and TNF-alpha. In addition, LF inhibits IL-8 production and modifies the complement cascade by preventing C3 deposition in the immune complexes [1, 2]. On the other hand, since LF is a cationic glycoprotein, it is quite likely that LF-anti-LF immune complexes might be pathogenic by itself [1, 6].
Additionally, LF-ANCA may induce, like other ANCAs, oxidative stress and PMN degradation, with the release of reactive oxygen intermediates and the consecutive tissue damage. It has not been shown that heterogeneous epitopes of LF are responsible for the broad spectrum of clinical manifestations associated with LF-ANCA [43].
Our study has some limitations. The number of our healthy controls is relatively small. Also, a higher number of patients might be necessary to confirm our results. Nevertheless, to the best of our knowledge, this is the first study of ANCA avidity in SLE; the exact clinical significance of LF-ANCA avidity needs to be further elucidated in long-term follow-up studies, in large number of patients. The methods we used for determination of RAI have been already published [20, 40], are reproducible, and relatively easy to perform in laboratory practice.
In conclusion, detection of ANCA specificity, level, and avidity may help in the diagnosis of particular clinical phenotypes of SLE. In contrast to other ANCAs, only LF-ANCA level correlated with disease activity and standard serological SLE markers. We are the first to report the positive correlation between LF-ANCA levels with both anti-histone and anti-C1q antibodies. In addition, we are the first to demonstrate that LF-ANCA avidity was higher than avidity of other ANCAs. LF-ANCA level and avidity might be used as valuable serological biomarkers for renal involvement in SLE.
References
Tsokos GC (2020) Autoimmunity and organ damage in systemic lupus erythematosus. Nat Immunol 21(6):605–614. https://doi.org/10.1038/s41590-020-0677-6
Sangaletti S, Tripodo C, Chiodoni C, Guarnotta C, Cappetti B, Casalini P, Piconese S, Parenza M, Guiducci C, Vitali C, Colombo MP (2012) Neutrophil extracellular traps mediate transfer of cytoplasmic neutrophil antigens to myeloid dendritic cells toward ANCA induction and associated autoimmunity. Blood 120(15):3007–3018. https://doi.org/10.1182/blood-2012-03-416156
Garcia-Romo GS, Caielli S, Vega B, Connolly J, Allantaz F, Xu Z, Punaro M, Baisch J, Guiducci C, Coffman RL, Barrat FJ, Banchereau J, Pascual V (2011) Netting neutrophils are major inducers of type I IFN production in pediatric systemic lupus erythematosus. Sci Transl Med 3(73):73ra20. https://doi.org/10.1126/scitranslmed.3001201
Nakazawa D, Tomaru U, Suzuki A, Masuda S, Hasegawa R, Kobayashi T, Nishio S, Kasahara M, Ishizu A (2012) Abnormal conformation and impaired degradation of propylthiouracil-induced neutrophil extracellular traps: implications of disordered neutrophil extracellular traps in a rat model of myeloperoxidase antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 64(11):3779–3787. https://doi.org/10.1002/art.34619
Podolska MJ, Biermann MH, Maueröder C, Hahn J, Herrmann M (2015) Inflammatory etiopathogenesis of systemic lupus erythematosus: an update. J Inflamm Res 8:161–171. https://doi.org/10.2147/jir.s70325
Okubo K, Kamiya M, Urano Y, Nishi H, Herter JM, Mayadas T, Hirohama D, Suzuki K, Kawakami H, Tanaka M, Kurosawa M, Kagaya S, Hishikawa K, Nangaku M, Fujita T, Hayashi M, Hirahashi J (2016) Lactoferrin suppresses neutrophil extracellular traps release in inflammation. EBioMedicine 10:204–215. https://doi.org/10.1016/j.ebiom.2016.07.012
Schauer C, Janko C, Munoz LE, Zhao Y, Kienhöfer D, Frey B, Lell M, Manger B, Rech J, Naschberger E, Holmdahl R, Krenn V, Harrer T, Jeremic I, Bilyy R, Schett G, Hoffmann M, Herrmann M (2014) Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat Med 20(5):511–517. https://doi.org/10.1038/nm.3547
Pan HF, Fang XH, Wu GC, Li WX, Zhao XF, Li XP, Xu JH, Ye DQ (2008) Anti-neutrophil cytoplasmic antibodies in new-onset systemic lupus erythematosus and lupus nephritis. Inflammation 31(4):260–265. https://doi.org/10.1007/s10753-008-9073-3
Wang Y, Huang X, Cai J, Xie L, Wang W, Tang S, Yin S, Gao X, Zhang J, Zhao J, Huang Y, Li Y, Zhang Y, Zhang J (2016) Clinicopathologic characteristics and outcomes of lupus nephritis with antineutrophil cytoplasmic antibody: a retrospective study. Medicine 95(4):e2580. https://doi.org/10.1097/md.0000000000002580
Galeazzi M, Morozzi G, Sebastiani GD, Bellisai F, Marcolongo R, Cervera R, De Ramòn Garrido E, Fernandez-Nebro A, Houssiau F, Jedryka-Goral A, Mathieu A, Papasteriades C, Piette JC, Scorza R, Smolen J (1998) Anti-neutrophil cytoplasmic antibodies in European patients with systemic lupus erythematosus: prevalence, clinical associations and correlation with other autoantibodies. European Concerted Action on the Immunogenetics of SLE. Clin Exp Rheumatol. 16(5):541–546
Čučnik S, Kveder T, Artenjak A, Ulcova Gallova Z, Swadzba J, Musial J, Iwaniec T, Stojanovich L, Alessandri C, Valesini G, Avčin T, Cohen Tervaert JW, Rozman B, Božič B (2012) Avidity of anti-β2-glycoprotein I antibodies in patients with antiphospholipid syndrome. Lupus 21(7):764–765. https://doi.org/10.1177/0961203312440057
Andrejevic S, Jeremic I, Sefik-Bukilica M, Nikolic M, Stojimirovic B, Bonaci-Nikolic B (2013) Immunoserological parameters in SLE: high-avidity anti-dsDNA detected by ELISA are the most closely associated with the disease activity. Clin Rheumatol 32(11):1619–1626. https://doi.org/10.1007/s10067-013-2330-3
Lee SS, Lawton JW, Chan CE, Li CS, Kwan TH, Chau KF (1992) Antilactoferrin antibody in systemic lupus erythematosus. Br J Rheumatol 31(10):669–673. https://doi.org/10.1093/rheumatology/31.10.669
Caccavo D, Rigon A, Picardi A, Galluzzo S, Vadacca M, Ferri GM, Amoroso A, Afeltra A (2005) Anti-lactoferrin antibodies in systemic lupus erythematosus: isotypes and clinical correlates. Clin Rheumatol 24(4):381–387. https://doi.org/10.1007/s10067-004-1040-2
Chikazawa H, Nishiya K, Matsumori A (2000) Hashimoto K (2000) Immunoglobulin isotypes of anti-myeloperoxidase and anti-lactoferrin antibodies in patients with collagen diseases. J Clin Immunol 4:279–286. https://doi.org/10.1023/a:1006667703202
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Petri M, Buyon J, Kim M (1999) Classification and definition of major flares in SLE clinical trials. Lupus 8(8):685–691. https://doi.org/10.1191/096120399680411281
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Romero-Díaz J, Vargas-Vóracková F, Kimura-Hayama E, Cortázar-Benítez LF, Gijón-Mitre R, Criales S, Cabiedes-Contreras J, Iñiguez-Rodríguez Mdel R, Lara-García EA, Núñez-Alvarez C, Llorente L, Aguilar-Salinas C, Sánchez-Guerrero J (2012) Systemic lupus erythematosus risk factors for coronary artery calcifications. Rheumatology (Oxford) 51(1):110–119. https://doi.org/10.1093/rheumatology/ker307
Kemna MJ, Schlumberger W, van Paassen P, Dähnrich C, Damoiseaux JG, Cohen Tervaert JW (2016) The avidity of PR3-ANCA in patients with granulomatosis with polyangiitis during follow-up. Clin Exp Immunol 185(2):141–147. https://doi.org/10.1111/cei.12796
Bosch X, Guilabert A, Font J (2006) Antineutrophil cytoplasmic antibodies. Lancet (London, England) 368(9533):404–418. https://doi.org/10.1016/s0140-6736(06)69114-9
Gajic-Veljic M, Bonaci-Nikolic B, Lekic B, Skiljevic D, Ciric J, Zoric S, Stojimirovic B, Nikolic M (2015) Importance of low serum DNase I activity and polyspecific anti-neutrophil cytoplasmic antibodies in propylthiouracil-induced lupus-like syndrome. Rheumatology (Oxford) 54(11):2061–2070. https://doi.org/10.1093/rheumatology/kev243
Kyriakidi KS, Tsianos VE, Karvounis E, Christodoulou DK, Katsanos KH, Tsianos EV (2016) Neutrophil anti-neutrophil cytoplasmic autoantibody proteins: bactericidal increasing protein lactoferrin cathepsin and elastase as serological markers of inflammatory bowel and other diseases. Ann Gastroenterol 29(3):258–267. https://doi.org/10.20524/aog.2016.0028
Dobric S, Popovic D, Nikolic M, Andrejevic S, Spuran M, Bonaci-Nikolic B (2011) Anti-neutrophil cytoplasmic antibodies (ANCA) specific for one or several antigens: useful markers for subtypes of ulcerative colitis and associated primary sclerosing cholangitis. Clin Chem Lab Med 50(3):503–509. https://doi.org/10.1515/CCLM.2011.797
Schnabel A, Csernok E, Isenberg DA, Mrowka C, Gross WL (1995) Antineutrophil cytoplasmic antibodies in systemic lupus erythematosus Prevalence specificities and clinical significance. Arthritis Rheum 38(5):633–637. https://doi.org/10.1002/art.1780380509
Nishiya K, Chikazawa H, Nishimura S, Hisakawa N, Hashimoto K (1997) Anti-neutrophil cytoplasmic antibody in patients with systemic lupus erythematosus is unrelated to clinical features. Clin Rheumatol 16(1):70–75. https://doi.org/10.1007/bf02238766
Spronk PE, Bootsma H, Horst G, Huitema MG, Limburg PC, Tervaert JW, Kallenberg CG (1996) Antineutrophil cytoplasmic antibodies in systemic lupus erythematosus. Br J Rheumatol 35(7):625–631. https://doi.org/10.1093/rheumatology/35.7.625
Zhao MH, Liu N, Zhang YK, Wang HY (1998) Antineutrophil cytoplasmic autoantibodies (ANCA) and their target antigens in Chinese patients with lupus nephritis. Nephrol Dial Transplant 13(11):2821–2824. https://doi.org/10.1093/ndt/13.11.2821
Molnár K, Kovács L, Kiss M, Husz S, Dobozy A, Pokorny G (2002) Antineutrophil cytoplasmic antibodies in patients with systemic lupus erythematosus. Clin Exp Dermatol 27(1):59–61. https://doi.org/10.1046/j.0307-6938.2001.00964.x
Sinico RA, Pozzi C, Radice A, Tincani A, Li Vecchi M, Rota S, Comotti C, Ferrario F, D’Amico G (1993) Clinical significance of antineutrophil cytoplasmic autoantibodies with specificity for lactoferrin in renal diseases. Am J Kidney Dis 22(2):253–260. https://doi.org/10.1016/s0272-6386(12)70314-1
Pradhan VD, Badakere SS, Bichile LS, Almeida AF (2004) Anti-neutrophil cytoplasmic antibodies (ANCA) in systemic lupus erythematosus: prevalence, clinical associations and correlation with other autoantibodies. J Assoc Physicians India 52:533–537
Su F, Xiao W, Yang P, Chen Q, Sun X, Li T (2017) Anti-neutrophil cytoplasmic antibodies in new-onset systemic lupus erythematosus. An Bras Dermatol 92(4):466–469. https://doi.org/10.1590/abd1806-4841.20175476
Yu YW, Liu ZR, Xie D, Chen SX, Li HY (2006) Clinical significance of antineutrophil cytoplasmic antibodies in patients with lupus nephritis. Nan Fang Yi Ke Da Xue Xue Bao 26(6):833–836
Jarrot PA, Chiche L, Hervier B, Daniel L, Vuiblet V, Bardin N, Bertin D, Terrier B, Amoura Z, Andrés E, Rondeau E, Hamidou M, Pennaforte JL, Halfon P, Daugas E, Dussol B, Puéchal X, Kaplanski G, Jourde-Chiche N (2016) Systemic lupus erythematosus and antineutrophil cytoplasmic antibody-associated vasculitis overlap syndrome in patients with biopsy-proven glomerulonephritis. Medicine (Baltimore) 95(22):e3748. https://doi.org/10.1097/MD.0000000000003748
Flores-Mendoza G, Sansón SP, Rodríguez-Castro S, Crispín JC, Rosetti F (2018) Mechanisms of tissue injury in lupus nephritis. Trends Mol Med 24(4):364–378. https://doi.org/10.1016/j.molmed.2018.02.003
Fu HL, Hsu TC, Chang CC, Tsay GJ (2001) Antigenic specificity of anti-neutrophil cytoplasmic antibody. J Formos Med Assoc 100(1):35–39
Manolova I, Dancheva M, Halacheva K (2001) Antineutrophil cytoplasmic antibodies in patients with systemic lupus erythematosus: prevalence, antigen specificity, and clinical associations. Rheumatol Int 20(5):197–204. https://doi.org/10.1007/s002960100108
Turner-Stokes T, Wilson HR, Morreale M, Nunes A, Cairns T, Cook HT, Pusey CD, Tarzi RM, Lightstone L (2017) Positive antineutrophil cytoplasmic antibody serology in patients with lupus nephritis is associated with distinct histopathologic features on renal biopsy. Kidney Int 92(5):1223–1231. https://doi.org/10.1016/j.kint.2017.04.029
Chin HJ, Ahn C, Lim CS, Chung HK, Lee JG, Song YW, Lee HS, Han JS, Kim S, Lee JS (2000) Clinical implications of antineutrophil cytoplasmic antibody test in lupus nephritis. Am J Nephrol 20(1):57–63. https://doi.org/10.1159/000013557
Zeng Y, Lin Y, Wang X, Zhang Y, Peng F, Wang J, Jiang L, Liang S, Xiao Y (2020) Assessment of a high-avidity IgG ANAs for the diagnosis and activity prediction of systemic lupus erythematosus. Clin Rheumatol 39(9):2619–2629. https://doi.org/10.1007/s10067-020-05040-4
Yoshida M, Sasaki M, Nakabayashi I, Akashi M, Tomiyasu T, Yoshikawa N, Kojima T, Ohno N, Yamada M (2009) Two types of myeloperoxidase-antineutrophil cytoplasmic autoantibodies with a high affinity and a low affinity in small vessel vasculitis. Clin Exp Rheumatol 27(Suppl 52):S28–S32
Pyo JY, Jung SM, Song JJ, Park YB, Lee SW (2019) ANCA positivity at the time of renal biopsy is associated with chronicity index of lupus nephritis. Rheumatol Int 39(5):879–884. https://doi.org/10.1007/s00296-019-04263-2
Audrain MA, Gourbil A, Muller JY, Esnault LM (1996) Anti-lactoferrin autoantibodies: relation between epitopes and iron-binding domain. J Autoimmun 9(4):569–574. https://doi.org/10.1006/jaut.1996.0076
Funding
This study was supported by the Ministry of Education and Science of the Republic of Serbia, Grant No. 175065 (M Nikolic, B Bonaci-Nikolic, and M Gajic-Veljic). The Ministry of Education and Science of the Republic of Serbia had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
MGV, BL, and BBN contributed to the design and implementation of the research, to the analysis of the results, and to the writing of the manuscript. MN was involved in planning and supervised the work. BS interpreted renal function tests. BL and JL performed the statistical analyses and participated in the interpretation of the results. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mirjana Gajic-Veljic and Branislav Lekic contributed equally to this work.
Rights and permissions
About this article
Cite this article
Gajic-Veljic, M., Lekic, B., Nikolic, M. et al. Level and avidity of antineutrophil cytoplasmic antibodies specific to lactoferrin are useful biomarkers in systemic lupus erythematosus. Clin Rheumatol 41, 709–720 (2022). https://doi.org/10.1007/s10067-021-05926-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05926-x