Abstract
Rheumatoid arthritis is a systemic inflammatory disease which causes symmetric polyarthritis. Lungs are common site for extra-articular involvement. Rheumatoid lung nodules occur in about 32% of patients with rheumatoid arthritis. The appearance of a lung nodule, along with the blood vessel supplying it, is called “feeding-vessel” sign on computed tomography. It is most commonly seen in infections. However, it can also be present in metastases and pulmonary vasculitis. We describe a woman with long-standing rheumatoid arthritis with subcutaneous and pulmonary nodules. Computed tomography of the chest showed “feeding-vessel” sign. There was no evidence of infection, malignancy, or vasculitis. She was treated for rheumatoid lung nodulosis with rituximab with which she improved remarkably. To the best of our knowledge, “feeding-vessel” sign in rheumatoid lung nodules has never been reported before. This case highlights the fact that “feeding-vessel” sign is not specific for pulmonary infections. It can rarely be seen in rheumatoid lung nodulosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a systemic inflammatory disease, which causes symmetric polyarthritis. A common site for extra-articular involvement is lungs. Pulmonary parenchyma is mostly affected by interstitial lung disease. Rheumatoid lung nodules occur infrequently. The nodules mimic infections, metastases, and vasculitis on imaging. Biopsy from the nodule is often required for making the correct diagnosis and ruling-out other causes. “Feeding-vessel” sign on computed tomography (discussed further) is commonly seen in pulmonary infections and metastasis. We report a woman with RA with “feeding-vessel” sign associated with rheumatoid lung nodules, which, to our knowledge, has not been reported before.
Case presentation
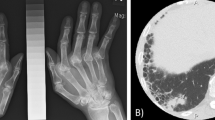
A 45-year-old woman presented with cough and breathlessness for 3 months. She had been diagnosed with seropositive RA 8 years back, being treated with methotrexate. Examination showed crepitations in both infrascapular lung fields, synovitis in proximal interphalangeal, metacarpophalangeal, and wrist joints along with deformities suggestive of RA. Rheumatoid nodules were present over the elbows. Disease activity of RA was high (Clinical Disease Activity Index (CDAI) 41) and dyspnea was significant (Medical Research Council (MRC) grade 3). Blood investigations showed elevated erythrocyte sedimentation rate (54 mm/hour) and C-reactive protein (15.6 mg/L). Hemogram, transaminases, and creatinine were normal. High-resolution computed tomogram (CT) of the chest revealed multiple nodules in both lungs. Blood vessels perfusing the nodules were seen along with some of them (Fig. 1a and b), which is called “feeding-vessel” sign. Further investigations were obtained to rule out infection, malignancy, and vasculitides, which were the differential diagnoses. The results showed normal serum calcium, alkaline phosphatase, procalcitonin, serum galactomannan, and sterile blood culture. Antinuclear antibody, perinuclear and cytoplasmic anti-neutrophil cytoplasmic antibody (p-ANCA and c-ANCA, respectively), anti-proteinase-3, anti-myeloperoxidase, serology for human immunodeficiency virus, Mantoux test, and interferon-gamma release assay were negative; transthoracic echocardiogram was normal. Bronchoscopy was negative for infections (tubercular, bacterial, fungal, and Nocardia) and malignancy. Contrast-enhanced CT of the chest and abdomen did not reveal any evidence of malignancy. The nodules were away from the pleural surface due to which a CT-guided tissue sampling was difficult. In addition, none of the nodules were amenable to bronchoscopic biopsy. The patient denied consent for thoracoscopic biopsy.
Results of blood investigations, broncho-alveolar lavage, and imaging did not reveal any evidence of infection, malignancy, or vasculitis. Patient was diagnosed with RA with probable rheumatoid lung nodules with “feeding-vessel” sign. She was treated with prednisolone (0.5 mg/kg body weight in tapering doses) and rituximab (two doses of 1 g, 2 weeks apart); methotrexate was discontinued (discussed further). Three months after treatment, marked improvement was observed in synovitis (CDAI 2) and dyspnea (MRC grade 1); acute phase reactants became normal. Repeat CT of the chest after 6 months revealed significant reduction in the lung nodules and disappearance of the “feeding-vessel” sign (Fig. 2).
Discussion
Rheumatoid lung nodules occur in about 32% of patients with RA [1]. They are mostly asymptomatic and resolve spontaneously. Male gender, smoking, and rheumatoid factor positivity are known risk factors [2]. Certain drugs used in the treatment of RA have also been implicated including methotrexate, leflunomide, and TNF inhibitors (therefore, methotrexate was discontinued in our patient) [3]. They seldom occur in the absence of rheumatoid nodules elsewhere in the body. Epithelioid cells along with chronic inflammatory infiltrates are visualized on histopathological examination. Fibrinoid necrosis can be seen, leading to radiologically visible cavitation [2]. Necrotizing nodules can give rise to hemoptysis and pneumothorax secondary to rupture into the pleural cavity. Therefore, aggressive treatment is warranted in patients with cavitating lung nodules. In addition, those with respiratory symptoms, which occur frequently when there are multiple nodules, should also be treated.
Blood vessel supplying a lung nodule or an area of consolidation may be visible on CT along with the lung lesion. This appearance is called “feeding-vessel” sign [4]. It is strongly suggestive of lung infection spreading hematogenously from a distant site, most commonly the heart valves [4]. However, it is also seen in metastasis, arterio-venous malformations, and pulmonary vasculitis. Air bronchogram and cavitation within the nodules along with “tree-in-bud” opacities are additional features seen in infection, whereas spiculation of the margins of the nodules suggests metastasis [5]. These features were not present in our patient and investigations other than histopathological examination did not reveal any other alternative diagnosis. The patient was treated for probable rheumatoid lung nodulosis, with which she improved remarkably.
Disease processes, which occur in the vicinity of the blood vessels, can also give rise to “feeding-vessel” sign [6]. Angiitis may be seen in rheumatoid lung nodules [1]. This could be the mechanism, which resulted in “feeding-vessel” sign in our patient. Angiitis may co-exist with granulomatous inflammation which may result in necrosis and cavitation [1]. Perhaps “feeding-vessel” sign in rheumatoid lung nodulosis increases the risk of such fatal complications and therefore, we propose that such patients should be treated aggressively. This case report highlights the fact that “feeding-vessel” sign is not specific for infections. It can rarely be seen in rheumatoid lung nodules. Treatment with rituximab leads to marked improvement, as in our patient and previous reports [7]. To the best of our knowledge, this is the first report of “feeding-vessel” sign in rheumatoid lung nodulosis.
Data availability
Data presented in the manuscript was obtained during the routine care of the patient after obtaining informed consent.
References
Yousem SA, Colby TV, Carrington CB (1985) Lung biopsy in rheumatoid arthritis. Am Rev Respir Dis 131:770–777
Ziff M (1990) The rheumatoid nodule. Arthritis Rheum 33:761–767
Akiyama N, Toyoshima M, Kono M, Nakamura Y, Funai K, Suda T (2015) Methotrexate-induced accelerated pulmonary nodulosis. Am J Respir Crit Care Med 192:252–253
Huang RM, Naidich DP, Lubat E, Schinella R, Garay SM, McCauley DI (1989) Septic pulmonary emboli: CT-radiographic correlation. Am J Roentgenol 153:41–45
Zwirewich CV, Vedal S, Miller RR, Müller NL (1991) Solitary pulmonary nodule: high-resolution CT and radiologic-pathologic correlation. Radiology 179:469–476
Ussavarungsi K, Khoor A, Jolles HI, Mira-Avendano I (2014) A 40-year-old woman with multiple pulmonary nodules. Pulmonary hyalinizing granuloma. Chest 146:e198–e203
Braun MG, Wagener P (2013) Regression of peripheral and pulmonary rheumatoid nodules under therapy with rituximab. Z Rheumatol 72:166–171
Author information
Authors and Affiliations
Contributions
All the authors have contributed equally in the preparation of the manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval
Not applicable as the data presented in the manuscript was obtained during the routine care of the patient.
Consent to participate
Written consent obtained.
Consent for publication
Written consent obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharma, A., Kasetty, A. & Kumar, A. Rheumatoid lung nodules with “feeding-vessel” sign. Clin Rheumatol 40, 1645–1647 (2021). https://doi.org/10.1007/s10067-020-05351-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05351-6