Abstract
Objective
The objectives of our study were to compare the efficacy of febuxostat with allopurinol in Thai subjects with gout, as well as to determine the predictive factors of responsiveness to urate-lowering agents and to evaluate the safety of febuxostat in a real-world setting.
Methods
The study was a retrospective cohort study; a total of 354 gout patients were recruited from February 2015 to November 2018. The patients were categorized according to prescription of allopurinol or febuxostat. Demographic data, comorbidities, concomitant medications, gout-related clinical parameters, and the laboratory results were collected. The serial serum urate (sUA) levels were recorded at the beginning of the treatment (baseline), and after treatment at 12 weeks, 18 weeks, and 27 weeks. The primary efficacy endpoint was the achievement of target urate of < 6 mg/dl in people taking febuxostat, compared with those taking allopurinol. The secondary endpoints were the predictive factors of achieving target urate level and adverse drug reactions in patients taking febuxostat. Multivariable regression analysis was used to determine factors associated with achieving target serum urate.
Results
After the treatment, the febuxostat groups had significantly lower mean sUA compared with the allopurinol groups across all follow-up periods. The proportion of people who achieved target serum urate was also higher in the febuxostat groups compared with the allopurinol groups throughout the follow-up periods. The multivariable regression analysis showed that febuxostat 40 mg (OR = 10.96 (95% CI 4.32–27.80); p value < 0.001), febuxostat 80 mg (OR = 9.54 (95% CI 3.91–23.28), smoking (OR = 2.35 (95% CI 1.13–4.91); p value = 0.023), and low baseline serum urate (OR = 0.62 (95% CI 0.52–0.74); p value < 0.001) were associated with the achievement of target serum urate. No adverse drug reaction from febuxostat was observed even among people with renal insufficiency.
Conclusion
In a Thai cohort, people receiving febuxostat are more likely to achieve target serum urate level, compared with people receiving allopurinol. Febuxostat (40 or 80 mg), smoking, and low baseline serum urate were associated with the achievement of target serum urate.
Key points: • Febuxostat showed superior urate-lowering efficacy compared with allopurinol in an Asian population. • In addition to febuxostat, lower baseline serum urate level and history of smoking were associated with achieving target serum urate in gout patients. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gouty arthritis is an inflammatory joint disease, caused by monosodium urate monohydrate crystal, which leads to local and systemic inflammation [1]. The prevalence of gout is 1.4–3.9% in most developed countries. It is more prevalent in men and postmenopausal women, and is on the rise [2]. Hyperuricemia, defined as a serum urate level exceeding the limit of solubility (6.8 mg/dl), also predisposes affected subjects to gouty arthritis and its spectrum [3]. Elevated serum urate is associated with cardiovascular disease, hypertension, insulin resistance, metabolic syndrome, chronic kidney disease, and increased mortality [4].
Recent guidelines, ACR and EULAR, recommend treatment to reach the target serum urate level of <6 mg/dl. [5,6,7] Urate-lowering therapy is the mainstay of the treatment to achieve the target serum urate. The ACR guideline recommends allopurinol and febuxostat as the first-line therapy [5]. However, the EULAR and British guidelines both recommend allopurinol as the first-line drug and febuxostat only for refractory cases [6, 7].
Due to the high mortality rate of allopurinol hypersensitivity syndrome (AHS), ACR recommends screening for HLA-B*5801 in high-risk population [5, 8]. People of Thai descent are considered a high-risk group for AHS [5].
Febuxostat, a non-purine selective xanthine oxidase inhibitor, exhibited potent and dose-dependent urate-lowering effect. In terms of urate-lowering efficacy, febuxostat is superior to 300 mg of allopurinol and displays good safety profile in cohorts dominated by people of European descent [9, 10]. However, the data regarding febuxostat in Asian people is still limited, as well as the factors associated with successful urate control. There are few Asian studies that showed febuxostat could be safely prescribed in patients with renal insufficiency [11, 12]. Furthermore, febuxostat may also delay the progression of renal dysfunction in people with coexisting chronic kidney disease [13].
The objective of this retrospective study was to compare the efficacy of febuxostat (40 mg/day and 80 mg/day) with allopurinol (100 mg/day and 300 mg/day) in Thai people with gout. We also compared the proportion of target urate achievement in febuxostat to allopurinol. Furthermore, this study sought to determine the predictive factors for target urate achievement and to describe the safety profile of febuxostat in a real-world, resource-limited clinical setting.
Material and methods
Study design and population
The study was conducted as a retrospective cohort study of people with gout who were initiated on febuxostat or allopurinol during their follow-ups at the rheumatology service, Thammasat University Hospital, between February 2015 and November 2018. Data of people with gout who were 18 years or older were collected from physical and electronic medical records. All patients were diagnosed with gout according to the 2015 ACR/EULAR classification criteria for gout [14]. The exclusion criteria were the following: (1) chronic kidney disease (CKD) stage 4 and 5 or renal replacement therapy, (2) pregnancy or breast feeding, (3) active liver disease or liver enzymes > 1.5 times the upper limit of normal, (4) alcoholism (alcohol > 14 units/week), (5) people with missing laboratory results, and (6) any modification to medications that could affect serum urate level. These medications included allopurinol, febuxostat, probenecid, benzbromarone, sulfinpyrazone, aspirin, diuretics, losartan, fenofibrate, pyrazinamide, ethambutol, cyclosporine, and estrogen. For those started on allopurinol and febuxostat, no dose titration was applied. The patients were initiated on the dose according to their subgroup and had their medications maintained at the same dosage throughout the study.
Variables
The variables included demographics, comorbidities (impaired fasting blood glucose, diabetes, hypertension, chronic kidney disease, hyperlipidemia, fatty liver, ischemic heart, and metabolic syndrome), and history of alcohol intake and smoking. The concomitant medications, including beta-blocker, calcium channel blocker, aspirin, angiotensin-converting enzyme inhibitor (ACEI), losartan, irbesartan, statin, fenofibrate, diuretics, and anti-tuberculosis drugs, were recorded. Gout-related variables included the presence of crystal, tophus, renal stone, radiographic joint destruction, the prophylaxis of flare, the usage of uricosuric agents, and flare during the first 3 months after medication. Laboratory investigation included serum urate, creatinine, aspartate transaminase (AST), alanine transaminase (ALT), and alkaline phosphatase. The serial serum urate (sUA) levels were recorded at the beginning of the treatment (baseline) and then at 12 weeks, 18 weeks, and 27 weeks after treatment initiation. The creatinine, AST, and ALT were recorded at baseline and 12 weeks after treatment to monitor for potential adverse drug reaction. As febuxostat is the second-line agent in our hospital, we also recorded the reason for using or switching to febuxostat. Patients were divided into four groups according to the urate-lowering agent used: allopurinol 100 mg/day, allopurinol 300 mg/day, febuxostat 40 mg/day, and febuxostat 80 mg/day. A study time table is shown in supplementary Table 1.
Efficacy endpoints
The primary efficacy endpoint was the proportion of patients who achieved sUA < 6.0 mg/dl at 12 weeks, 18 weeks, and 27 weeks after treatment in each study group [5, 6].
The secondary endpoints were the factors associated with achieving target serum urate level.
Statistical analysis
The categorical data were described as frequency and percentage, while continuous data were presented as mean and standard deviation. The comparison was analyzed using Mann-Whitney U test for continuous variables and Chi-square or Fisher’s exact test for categorical variables. A univariate binary logistic regression was used to screen for potential factor associated with achieving target serum urate. Variables with the p value less than 0.05 were included in the multivariable regression model. We reported the regression coefficients, odds ratios, 95% confidence interval, and p value for the final regression analysis. Statistical analysis was carried out using IBM SPSS Statistics version 25.
Ethical approval
The study protocol was reviewed and approved by the Human Research Ethics Committee, Faculty of Medicine, Thammasat University (reference number MTU-EC-IM-6-141/60). Informed consent is not required for this type of study.
Results
Cohort characteristics
In total, there were 354 people with gout in the cohort: The characteristics of the patients as well as comparison between study groups are listed in Table 1.
Compared with the allopurinol 100 group, the other groups (allopurinol 300, febuxostat 40, and febuxostat 80) had more severe disease: higher prevalence of flare per year, tophi, renal stone, and erosion or deposition by imaging study. Combination with uricosuric agent was more common in patients taking febuxostat, compared with those taking allopurinol. Statin, diuretics, and aspirin were more common in the allopurinol 100 group, compared with other groups.
One hundred and fourteen patients were prescribed with febuxostat. Inefficacy of the first-line therapy (allopurinol) accounted for 45.6% of patients, whereas adverse reactions from allopurinol were the indication in 38.6% (Table 2). Metabolic syndrome was higher in febuxostat groups than allopurinol groups (62% versus 64%). Also, CKD was found with higher percentage in febuxostat groups (57% versus 46%). From our study, we did not find adverse drug reaction in febuxostat-prescribed patients even in those with CKD.
Achievement of target serum urate level
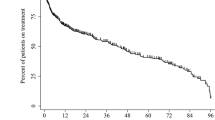
Mean serum urate levels at baseline were similar in all study groups. In all study groups, serum urate level continued to decrease after treatment initiation. Similarly, the proportion of people who achieved target serum urate level continuously rose. However, a significantly greater proportion of people who took febuxostat achieved target serum urate at every follow-up visit, compared with those taking allopurinol (Table 3 and Fig. 1).
Logistic regression analysis
The univariate analysis revealed that six variables were associated with achieving target serum urate level: febuxostat (both 40 mg/day and 80 mg/day), baseline urate level, number of flare per year, smoking, and hyperlipidemia (Table 4). In the multivariate analysis, 40 mg febuxostat (OR = 10.96 (95% CI 4.32–27.80); p value < 0.001), 80 mg febuxostat (OR = 9.54 (95% CI 3.91–23.28); p value < 0.001), low baseline urate level (OR = 0.62 (95% CI 0.52–0.74); p value < 0.001), and smoking (OR = 2.35 (95% CI 1.13–4.91); p value = 0.23) were associated with the achievement of target serum urate (Table 5).
Discussion
Our study showed that, in a real-world setting, febuxostat had higher urate-lowering efficacy at 12, 18, and 27 weeks compared with allopurinol. Factors associated with achieving the target serum urate at 27 weeks were the use of either 40 mg or 80 mg of febuxostat, lower baseline serum urate level, and smoking. No serious adverse event was observed. Febuxostat is a non-purine, selective xanthine oxidase inhibitor that can be prescribed as a second-line drug according to EULAR, BSR, and our Thai guideline.
Long-term studies have confirmed the efficacy and tolerability of febuxostat. [15,16,17,18] Current guidelines recommend to start with a dose of 80 mg/day and the dose could be increased for up to a maximum of 120 mg/day if necessary [19, 20]. Our study regarding the efficacy of febuxostat was in agreement with previous studies. A 28-week study to compare the urate-lowering efficacy and safety of febuxostat, allopurinol, and placebo demonstrated that febuxostat was more effective than allopurinol (100 mg/day and 300 mg/day), including for those with mild to moderately impaired renal function [21]. After 1 month of treatment initiation, more than 80% of patients receiving febuxostat 80 mg/day or 120 mg/day achieved sUA < 6.0 mg/dl, whereas only 46% of the allopurinol group did. Febuxostat also led to progressive reduction of tophi and elimination of gout flare [15]. Another study of elderly (> 65 years old) patients also showed that febuxostat was superior to allopurinol and well tolerated in the elderly with renal impairment [17]. A study from Japan found that the serum urate-lowering efficacy of febuxostat may decrease in patients with a higher previous dose of allopurinol, renal impairment, or in male patients [22]. The previous high allopurinol dose may reflect the therapeutic resistance of patients to xanthine oxidase inhibitors. Febuxostat had lower efficacy in male patients compared with female. The lower plasma concentration explained by higher body weight is presumed to contribute to the lower response in male patients [22]. Data from China, regarding predictors of poor response to ULT, found that younger age, higher BMI, and higher baseline sUA are predictors of poor response to ULT [23]. Overweight and obesity are associated with metabolic syndrome and hyperuricemia, and weight reduction is associated with better control of sUA [24]. There was data suggesting that a medical history of treatment with hyperlipidemia was a protective factor against therapeutic failure to achieve sUA. The rationale for this association might be from the relation between hyperlipidemia and hyperuricemia or only a selective bias in health-concerned patients [24]. There were many researches confirming the association between higher baseline sUA and lower achievement of sUA goal < 6.0 mg/dl [23, 25, 26]. Predictive factors of achieving the target urate in our study were febuxostat, smoking, and the low baseline serum urate. The association between initial serum urate and the achievement in our study was concordant with the previous studies. The higher response in febuxostat groups can be explained by the higher efficacy of the drug. Another possibility is the previous high allopurinol dose might reflect the resistance to xanthine oxidase inhibitors. Our cohort agrees with previous studies, which found that the resistant groups were the patients with high serum uric acid, higher allopurinol dosage, renal insufficiency, and metabolic syndrome [13, 22,23,24,25]. Additionally, data showed that patients who switched to febuxostat from allopurinol had a significantly higher likelihood of attaining sUA goal of lower than 6.0 mg/dl compared with patients who maintained on allopurinol [23, 25]. We could not find plausible mechanism to explain how smoking could be an indicator of a better sUA outcome.
The result from our study demonstrated a good safety profile of febuxostat, despite a proportion of people having coexisting renal insufficiency. Febuxostat, which is metabolized mainly in the liver, had shown efficacy and tolerability in patients with renal impairment in large studies [16,17,18, 27,28,29]. In Asian people specifically, febuxostat also showed a generally good safety profile [11,12,13], even in hemodialysis patients. [30, 31]
There were some limitations in our study. First, the study was a retrospective study which might be subjected to selection bias. Second, the number of patients was relatively small and the patients were all from a referral center which might not reflect a primary care setting, where a large proportion of gout patients are treated. On the other hand, a study based on participants from a resource-limited, real-world setting is currently lacking. Our study provides an additional insight into this little-studied population.
In conclusion, febuxostat has higher urate-lowering efficacy and generally good safety profile compared with allopurinol in an Asian cohort of gout patients. Febuxostat, smoking, and the low baseline serum urate were associated with the achievement of the target serum urate level of < 6 mg/dl at 12, 18, and 27 weeks of treatment. In patients with inadequate response to allopurinol or allopurinol hypersensitivity, febuxostat may be considered an effective and safe alternative option.
References
Singh JA, Cleveland JD (2019) Gout is associated with a higher risk of chronic renal disease in older adults: a retrospective cohort study of U.S. Medicare population. BMC Nephrol 20(1):93. https://doi.org/10.1186/s12882-019-1274-5
Elfishawi MM, Zleik N, Kvrgic Z, Michet CJ Jr, Crowson CS, Matteson EL, Bongartz T (2019) Changes in the presentation of incident gout and the risk of subsequent flares: a population-based study over 20 years. J Rheumatol 47:613–618. https://doi.org/10.3899/jrheum.190346
Towiwat P, Chhana A, Dalbeth N (2019) The anatomical pathology of gout: a systematic literature review. BMC Musculoskelet Disord 20(1):140. https://doi.org/10.1186/s12891-019-2519-y
Foody J, Turpin RS, Tidwell BA, Lawrence D, Schulman KL (2017) Major cardiovascular events in patients with gout and associated cardiovascular disease or heart failure and chronic kidney disease initiating a xanthine oxidase inhibitor. Am Health Drug Benefits 10(8):393–401
Khanna D, Fitzgerald JD, Khanna PP et al (2012) American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken) 64(10):1431–1446. https://doi.org/10.1002/acr.21772
Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castañeda-Sanabria J, Coyfish M, Guillo S, Jansen TL, Janssens H, Lioté F, Mallen C, Nuki G, Perez-Ruiz F, Pimentao J, Punzi L, Pywell T, So A, Tausche AK, Uhlig T, Zavada J, Zhang W, Tubach F, Bardin T (2017) 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis 76(1):29–42. https://doi.org/10.1136/annrheumdis-2016-209707
Hui M, Carr A, Cameron S, Davenport G, Doherty M, Forrester H, Jenkins W, Jordan KM, Mallen CD, McDonald TM, Nuki G, Pywell A, Zhang W, Roddy E, for the British Society for Rheumatology Standards, Audit and Guidelines Working Group (2017) The British Society for Rheumatology guideline for the management of gout. Rheumatology (Oxford) 56(7):1246. https://doi.org/10.1093/rheumatology/kex250
Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T (2018) Current perspectives on Stevens-Johnson syndrome and toxic epidermal necrolysis. Clin Rev Allergy Immunol 54(1):147–176. https://doi.org/10.1007/s12016-017-8654-z
Becker MA, Schumacher HR, Espinoza LR et al (2010) The urate-lowering efficacy and safety of febuxostat in the treatment of the hyperuricemia of gout: the CONFIRMS trial. Arthritis Res Ther 12(2):R63. https://doi.org/10.1186/ar2978
Singh JA, Akhras KS, Shiozawa A (2015) Comparative effectiveness of urate lowering with febuxostat versus allopurinol in gout: analyses from large U.S. managed care cohort. Arthritis Res Ther 17:120. https://doi.org/10.1186/s13075-015-0624-3
Kimura K, Hosoya T, Uchida S, Inaba M, Makino H, Maruyama S, Ito S, Yamamoto T, Tomino Y, Ohno I, Shibagaki Y, Iimuro S, Imai N, Kuwabara M, Hayakawa H, Ohtsu H, Ohashi Y, Kimura K, Hosoya T, Ito S, Inaba M, Tomino Y, Uchida S, Makino H, Matsuo S, Yamanaka H, Yamamoto T, Ohno I, Shibagaki Y, Iimuro S, Imai N, Kuwabara M, Hayakawa H, Akizawa T, Teramoto T, Kasanuki H, Yoshimura K, Kimura K, Hosoya T, Shibagaki Y, Ohno I, Sato H, Uchida S, Horikoshi S, Maruyama S, Inaba M, Moriwaki Y, Uchida H, Kaneshiro N, Imai N, Moriya H, Komatsu Y, Kaname S, Hanaoka K, Ogura M, Ikeda M, Kasai K, Sugiura A, Takahashi K, Kojima K, Nitta K, Tamai H, Nagaya H, Okuno S, Kakiya R, Takeoka H, Hirata K, Asano K, Fukaya Y, Iwaida Y, Tsuneda Y, Nishimura S, Hiramatsu T, Isaka Y, Ito T, Yuzawa Y, Yamagata K, Sofue T, Jinguji Y, Hirano K, Matsuyama K, Mizumoto T, Shibuya Y, Sugawara M, Kadomura M, Teshima Y, Ohtani H, Kamata H, Okawara S, Fukushima M, Takemura K, Kinugasa E, Kogure M, Ehara Y (2018) Febuxostat therapy for patients with stage 3 CKD and asymptomatic hyperuricemia: a randomized trial. Am J Kidney Dis 72(6):798–810. https://doi.org/10.1053/j.ajkd.2018.06.028
Tanaka A, Taguchi I, Teragawa H, Ishizaka N, Kanzaki Y, Tomiyama H, Sata M, Sezai A, Eguchi K, Kato T, Toyoda S, Ishibashi R, Kario K, Ishizu T, Ueda S, Maemura K, Higashi Y, Yamada H, Ohishi M, Yokote K, Murohara T, Oyama JI, Node K, on behalf of the PRIZE study investigators (2020) Febuxostat does not delay progression of carotid atherosclerosis in patients with asymptomatic hyperuricemia: a randomized, controlled trial. PLoS Med 17(4):e1003095. https://doi.org/10.1371/journal.pmed.1003095
Kojima S, Matsui K, Hiramitsu S, Hisatome I, Waki M, Uchiyama K, Yokota N, Tokutake E, Wakasa Y, Jinnouchi H, Kakuda H, Hayashi T, Kawai N, Mori H, Sugawara M, Ohya Y, Kimura K, Saito Y, Ogawa H (2019) Febuxostat for cerebral and cardiorenovascular events prevention study. Eur Heart J 40(22):1778–1786. https://doi.org/10.1093/eurheartj/ehz119
Neogi T, Jansen TL, Dalbeth N et al (2015) 2015 gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 74(10):1789–1798. https://doi.org/10.1136/annrheumdis-2015-208237
Becker MA, Schumacher HR, MacDonald PA et al (2009) Clinical efficacy and safety of successful longterm urate lowering with febuxostat or allopurinol in subjects with gout. J Rheumatol 36(6):1273–1282. https://doi.org/10.3899/jrheum.080814
Edwards NL (2008) Febuxostat : a viewpoint by N. Lawrence Edwards. Drugs 68(13):1875–1876. https://doi.org/10.2165/00003495-200868130-00007
Jackson RL, Hunt B, MacDonald PA (2012) The efficacy and safety of febuxostat for urate lowering in gout patients ≥65 years of age. BMC Geriatr 12:11. https://doi.org/10.1186/1471-2318-12-11
Huang X, Du H, Gu J et al (2014) An allopurinol-controlled, multicenter, randomized, double-blind, parallel between-group, comparative study of febuxostat in Chinese patients with gout and hyperuricemia. Int J Rheum Dis 17(6):679–686. https://doi.org/10.1111/1756-185X.12266
Nuki G, Doherty M, Richette P (2017) Current management of gout: practical messages from 2016 EULAR guidelines. Pol Arch Intern Med 127(4):267–277. https://doi.org/10.20452/pamw.4001
Waller A, Jordan KM (2017) Use of febuxostat in the management of gout in the United Kingdom. Ther Adv Musculoskelet Dis 9(2):55–64. https://doi.org/10.1177/1759720X16682010
Schumacher HR Jr, Becker MA, Wortmann RL et al (2008) Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricemia and gout: a 28-week, phase III, randomized, double-blind, parallel-group trial. Arthritis Rheum 59(11):1540–1548. https://doi.org/10.1002/art.24209
Koide H, Hira D, Tsujimoto M, Katsube Y, Minegaki T, Uzu T, Ikeda Y, Morita SY, Nishiguchi K, Terada T (2017) Previous dosage of allopurinol is a strong determinant of febuxostat efficacy. Biol Pharm Bull 40(5):681–686. https://doi.org/10.1248/bpb.b16-00972
Mu Z, Wang W, Wang J, Lv W, Chen Y, Wang F, Yu X, Wang Y, Cheng B, Wang Z (2019) Predictors of poor response to urate-lowering therapy in patients with gout and hyperuricemia: a post-hoc analysis of a multicenter randomized trial. Clin Rheumatol 38:3511–3519. https://doi.org/10.1007/s10067-019-04737-5
Katayama A, Yokokawa H, Fukuda H, Ono Y, Isonuma H, Hisaoka T, Naito T (2019) Achievement of target serum uric acid levels and factors associated with therapeutic failure among Japanese men treated for hyperuricemia/gout. Intern Med 58(9):1225–1231. https://doi.org/10.2169/internalmedicine.1899-18
Hatoum H, Khanna D, Lin SJ et al (2014) Achieving serum urate goal: a comparative effectiveness study between allopurinol and febuxostat. Postgrad Med 126(2):65–75. https://doi.org/10.3810/pgm.2014.03.2741
Sheer R, Null KD, Szymanski KA, Sudharshan L, Banovic J, Pasquale M (2017) Predictors of reaching a serum uric acid goal in patients with gout and treated with febuxostat. Clinicoecon Outcomes Res 9:629–639. https://doi.org/10.2147/CEOR.S139939
Kojima S, Matsui K, Ogawa H, Jinnouchi H, Hiramitsu S, Hayashi T, Yokota N, Kawai N, Tokutake E, Uchiyama K, Sugawara M, Kakuda H, Wakasa Y, Mori H, Hisatome I, Waki M, Ohya Y, Kimura K, Saito Y, Febuxostat for Cerebral and Cardiorenovascular Events Prevention Study (FREED) investigators (2017) Rationale, design, and baseline characteristics of a study to evaluate the effect of febuxostat in preventing cerebral, cardiovascular, and renal events in patients with hyperuricemia. J Cardiol 69(1):169–175. https://doi.org/10.1016/j.jjcc.2016.02.015
Saag KG, Whelton A, Becker MA, MacDonald P, Hunt B, Gunawardhana L (2016) Impact of febuxostat on renal function in gout patients with moderate-to-severe renal impairment. Arthritis Rheumatol 68(8):2035–2043. https://doi.org/10.1002/art.39654
Sircar D, Chatterjee S, Waikhom R, Golay V, Raychaudhury A, Chatterjee S, Pandey R (2015) Efficacy of febuxostat for slowing the GFR decline in patients with CKD and asymptomatic hyperuricemia: a 6-month, double-blind, randomized, Placebo-Controlled Trial. Am J Kidney Dis 66(6):945–950. https://doi.org/10.1053/j.ajkd.2015.05.017
Tsuruta Y, Kikuchi K, Tsuruta Y, Sasaki Y, Moriyama T, Itabashi M, Takei T, Uchida K, Akiba T, Tsuchiya K, Nitta K (2015) Febuxostat improves endothelial function in hemodialysis patients with hyperuricemia: a randomized controlled study. Hemodial Int 19(4):514–520. https://doi.org/10.1111/hdi.12313
Mitsuboshi S, Yamada H, Nagai K, Okajima H (2015) Switching from allopurinol to febuxostat: efficacy and tolerability in hemodialysis patients. J Pharm Health Care Sci 1:28. https://doi.org/10.1186/s40780-015-0028-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 530 kb)
Rights and permissions
About this article
Cite this article
Lertnawapan, R., Jatuworapruk, K. Efficacy of febuxostat versus allopurinol and the predictors of achieving target serum urate in a cohort of Thai people with gout. Clin Rheumatol 40, 255–262 (2021). https://doi.org/10.1007/s10067-020-05262-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05262-6