Abstract
Introduction
Ramadan intermittent fasting is observed by Muslims from sunrise to sunset and alternated with moments of re-feeding. The aims of this study were to assess the impact of Ramadan fasting on rheumatoid arthritis (RA) and spondyloarthritis (SpA) activity and to assess its impact on chronic medications intake in patients with rheumatic diseases.
Methods
This prospective monocentric study included patients with RA or SpA who fasted during Ramadan of 2019. The disease activity and the managing of chronic medications were assessed and compared between two visits: the first one 6 months before starting Ramadan fasting and the second after fasting at least 7 days.
Results
Fifty-six patients were included: 36 with RA (average age 57.5 ± 10.9 years) and 20 with SpA (average age 47 ± 12.6 years). In the RA group, the Disease Activity Scores (DAS) 28 ESR, and DAS 28 CRP decreased after fasting respectively from 4.3 ± 1.3 to 3.5 ± 1.4 (p < 0.001) and from 3.4 ± 1.2 to 2.9 ± 1.3 (p = 0.001). In the SpA group, Ankylosing Spondylitis Disease Activity Scores (ASDAS) ESR and ASDAS CRP decreased respectively from 2.3 ± 0.5 to 1.9 ± 0.7 (p = 0.039) and from 1.9 ± 0.5 to 1.8 ± 0.8 (p = 0.388). Fasting did not affect significantly either compliance with chronic medications or tolerance.
Conclusions
Fasting can be a possible way to induce rapid improvement of rheumatic diseases activity. In addition, patients with a specific fear of drug intake during this period can be reassured, which will enhance the adherence to treatment.
Key Points • Fasting during Ramadan, the ninth month of the Islamic calendar, consists of intermittent fasting observed from sunrise to sunset. • In this set of patients, beneficial effects of intermittent fasting were demonstrated on RA activity, but were less evident in patients with SpA despite a general trend towards improvement. • Fasting did not affect significantly either compliance with chronic medications or tolerance. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fasting during Ramadan, the ninth month of the Islamic calendar, is one of the 5 fundamental pillars of Islam. It consists of intermittent fasting that is observed from sunrise to sunset and is alternated with moments of re-feeding [1]. Muslims consume two main meals, one shortly before dawn (Suhoor) and the other immediately after sunset (Iftar). During daylight hours, they abstain from eating, drinking, smoking, and sexual intercourses.
Although several studies have evaluated the effects of Ramadan fasting on the immune system [2, 3], very few investigations have dealt with the possible impact of intermittent fasting on rheumatic diseases [1, 4].
Two major issues are often raised by patients during this period: the fasting impact on disease activity and the managing of drug intake. Considering the globalization, any physician, even in non-Muslim countries, could face the issue of managing patients who choose to fast Ramadan and monitoring their immune status [2]. However, there are very few guidelines or standardized protocols that can help physicians properly advise patients willing to fast during this month [5].
Being aware of the lack of physicians’ knowledge in this field, and the difficulties encountered in addressing patient concerns, the purpose of this study was to fill this gap in knowledge. Our objectives were to assess the impact of intermittent fasting on rheumatoid arthritis (RA) and spondyloarthritis (SpA) activity and to assess its impact on chronic medications intake in patients with rheumatic diseases.
Methods
Study design
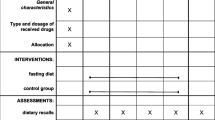
This is a prospective study conducted over 2 periods in 2019. Patients with RA (according to 2010 ACR/EULAR classification criteria for RA) or SpA (according to ASAS classification criteria for SpA) who fasted Ramadan 2019 (5 May–3 June 2019) were enrolled in the study. The elapsed time from dawn to sunset was 15.5 h at the beginning and 16.5 h at the end of Ramadan. For each patient, the study period took 6–7 months and included 2 visits:
-
a first inclusion visit, 6 months before starting Ramadan fasting
-
a follow-up visit, during the month between the 7th day of fasting and the 7th day after the end of Ramadan
Study population
Fifty-six patients were recruited from the department of the rheumatology of Kassab Institute in Tunisia. Patients older than 18 years, with a confirmed diagnosis of RA or SpA, and planning to fast the whole month of Ramadan were included.
The non-inclusion criteria were as follows: patients who changed dose or started or stopped any medication that may affect the disease activity during the last consultation before Ramadan fast and medical conditions preventing the patient from following fasting, pregnancy, or breastfeeding.
Measures and outcomes
Data regarding age, gender, comorbidities, disease duration, and treatments were documented.
The following parameters were collected and compared between the 2 consecutive visits: visual analogue scale (VAS) pain score, morning stiffness duration, awakening because of pain during the night, tender and swollen joint counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). RA activity was evaluated according to the Disease Activity Score 28 (DAS 28) ESR and CRP and SpA activity according to Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and Ankylosing Spondylitis Disease Activity Score (ASDAS) ESR and CRP. Concerning drug intake, patients were asked for each treatment about compliance (enhanced, impaired, or unchanged during Ramadan), tolerability (enhanced, impaired, or unchanged during Ramadan), and timing of intake (Iftar meal, evening, Suhoor meal).
The present study received ethical approval from the Ethical Committee of the Kassab Institute and informed consent was obtained from each participant.
Statistical analysis
The study data were collected, recorded, and analyzed by the SPSS statistical software (version 18.0). The quantitative variables were expressed by their means with the estimation of their standard deviations. The normal distribution of variables was examined with the Kolmogorov–Smirnov normality test. The following tests were applied to assess the differences before and during the Ramadan fasting: Student’s t test for paired samples (for quantitative variables with normal distribution and with a sample size > 30), Wilcoxon test (the nonparametric equivalent of the paired t test), and McNemar’s test (for qualitative variables).
Results
Study population: general data
Fifty-six patients were included: 36 with RA and 20 with SpA. The main demographic, clinical, and therapeutic characteristics are shown in Table 1.
Fasting impact on disease activity (Table 2)
Fasting impact on subjective parameters
-
VAS pain score
RA group: After fasting at least one week, the average VAS pain score was shown to be significantly decreased (p = 0.002). Twenty-one patients (58.3%) reported relief of pain during fasting, 11 patients (30.5%) did not report any change, whereas an exacerbation of pain was noted by 4 patients (11.1%).
SpA group: The reduction of the average VAS pain score was not significant in this group (p = 0.204). While VAS pain score decreased during Ramadan fasting in 9 patients (45%), it did not change in 8 patients (40%), and it increased in 3 patients (15%).
-
Morning stiffness
RA group: The average of morning stiffness duration after fasting was not significantly lower than the one observed before fasting (p = 0.372). This duration decreased in 5 patients (13.8%), did not change in 27 patients (75%), and increased in 4 patients (11.1%).
SpA group: The noted average decrease of morning stiffness duration was not shown to be statistically significant (p = 0.181). This duration was reported to be reduced by 9 patients (45%), unchanged by 9 patients (45%), and prolonged by 2 patients (10%).
-
Awakening because of pain during the night
RA group: Awakening because of pain during the night was reported by 11 patients (30.5%) before fasting and by 6 patients (16.7%) during fasting (p = 0.125).
SpA group: It was reported by 8 patients (40%) before fasting and by 1 patient (5%) after fasting. This improvement was statistically significant in this group of patients (p = 0.039).
Fasting impact on clinical parameters
The improvement of tender and swollen joint count (TJC and SJC) after fasting was significant in patients with RA (TJC p = 0.029, SJC p = 0.05) but not in patients with SpA (TJC p = 0.356, SJC p = 1.000).
Fasting impact on biological parameters
RA group: The average levels of the inflammatory markers decreased after fasting. This improvement was statistically significant for ESR (p < 0.001) but not for CRP (p = 0.06). Indeed, ESR and CRP respectively` decreased in 84.3% and 48.5% of patients, did not vary in 9.4% and 27.3% of patients, and increased in 6.3% and 24.2% of patients.
SpA group: ESR and CRP respectively decreased in 70% and 60% of patients, did not vary in 5% and 25% of patients, and increased in 25% and 15% of patients. This improvement seen in the majority of patients was not significant (ESR p = 0.083, CRP p = 0.303).
Fasting impact on disease activity scores
RA group: There was a statistically significant change in the DAS28 scores before and after fasting (DAS28 ESR p < 0.001, DAS28 CRP p = 0.001). The distribution of patients according to the variation of disease activity is detailed in Fig. 1.
SpA group: The disease activity did not differ significantly according to BASDAI (p = 0.944) and ASDAS CRP (p = 0.388). Nevertheless, it was significantly lower according to ASDAS ESR after fasting (p = 0.039) (Fig. 2).
At the univariate analysis (Table 3), we did not find significant confounding factors influencing the change in disease activity scores before and after fasting. Therefore, a multivariate analysis was not carried out.
Managing medications during Ramadan
bDMARDs
Among the 11 patients under biological agents, Ramadan fasting did not affect either compliance with treatment or tolerance. No additional side effects have been reported during this period.
csDMARDs
-
Adherence to treatment
Patients’ compliance to MTX was adequate and comparable before and during fasting in 71.4% of cases. It was impaired by fasting in the rest with a full stop in 23.8% of patients. MTX was taken away from meals by 46.6% of patients. The timing of drug intake was the Iftar meal in 13% of patients, the Suhoor meal in 67% of patients, and the evening in 20% of patients.
Except for 1 patient, adherence to SLZ was not affected during Ramadan fasting. It was taken with the 2 major meals in 70% of cases and during the evening in 30% of cases.
Patients under LFN did not report any discontinuation.
Discontinuation of csDMARD therapy was due to objective adverse effects in 20% of patients, apprehension of gastrointestinal adverse effects in 20% of patients, and lack of time between the two major meals in 60% of patients (since they were advised to take MTX away from meals).
-
Tolerance of treatment
Additional gastrointestinal side effects of MTX were observed during Ramadan in 17.6% of patients. These side effects were reported to be fewer during this period by 11.8% of patients. No significant changes were noted by the rest of the patients.
Regarding the gastrointestinal tolerance of SLZ and LFN, it was similar before and during Ramadan fasting.
Non-steroidal anti-inflammatory drugs (NSAIDs)
In a quarter of patients, the consumption of NSAIDs was reduced during Ramadan. This reduction was explained by pain relief (75%) or by an apprehension of gastrointestinal adverse effects (25%). No objective adverse effects were detected. In 60% of cases, NSAIDs were taken during the major meals.
Corticosteroids
Fasting had no impact on either compliance or tolerance of corticosteroids, taken by 50% of patients during the Suhoor meal.
Analgesics
Analgesic consumption was reduced in 50% of patients, mainly due to pain relief (except 1 patient who reported additional gastrointestinal adverse effects).
Discussion
This is the first investigation to demonstrate that intermittent fasting has beneficial effects on RA activity. This improvement included pain assessment, clinical examination, and biological inflammatory markers. This result was less evident in patients with SpA despite a general trend toward improvement. The decrease in the levels of VAS pain score, morning stiffness duration, tender and swollen joint count, ESR, and CRP were not statistically significant. While the improvement of ASDAS ESR was statistically significant, there was no significant change in the level of BASDAI and ASDAS CRP.
The noted differences between the 2 groups (RA and SpA) may be explained by two reasons. First, the number of patients with SpA included in the study was relatively limited (n = 20), which reduces the power of the statistical findings. Second, the disease activity scores of SpA, especially the BASDAI, are mostly based on subjective parameters such as fatigue and discomfort. As Ramadan fast can represent by itself a risk factor of tiredness, these scores may be falsely elevated. In fact, additional tiredness during fasting may be explained by dehydration, lack of some substances like caffeine, extra physical effort involved in family commitments, and lack of proper sleep [6].
The noted decrease in disease activity has been described earlier in RA patients during fasting [3, 7,8,9,10]. The main difference between our study and previous ones is the type of fasting. To our knowledge, this is the first investigation assessing the impact of intermittent diurnal fasting on RA activity. Previous reports evaluated continuous therapeutic fasting (Table 4). The duration differed from one study to another (7 to 23 days), and the fasting was usually partial (liquids allowed) and followed by a specific diet (vegetarian, lacto-vegetarian, and low-calorie diet).
A systematic review conducted by Müller et al. included 31 original reports assessing the impact of fasting followed by a vegetarian diet on patients with RA [11]. This review supported the hypothesis that a short period of fasting followed by a vegetarian diet can cause clinically relevant improvement in patients with RA. The fasting patients showed reduced pain, stiffness, consumption of analgesics, several clinical and biological variables, and disease activity scores [7,8,9]. However, this improvement was not always shown to be sustainable [9]. Consequently, fasting was considered to produce subjective and objective improvements in RA, though of short duration.
Even though only partly understood, some mechanisms for the decrease of inflammatory symptoms in patients with RA were suggested and confirmed by several studies during fasting. The main suggested hypotheses were the decrease of several proinflammatory cytokines levels such as IL-1, TNF, IL-6, and CRP and the decrease in the proportion of agalactosyl IgG that is known to be higher in patients with RA than healthy individuals [12]. The decrease of inflammatory markers after Ramadan fasting, demonstrated by several studies [1, 13,14,15,16], could be explained by a weight loss and reduced body fat percentage during fasting [13, 15]. Since the inflammatory status is associated with the features of metabolic syndrome (hyperglycemia, insulin resistance, and type II diabetes), it could be concluded that fasting decreases inflammatory markers through the down-regulation of metabolic syndrome [17]. Further plausible explanations for the improvement during Ramadan such as reduced ability to generate cytotoxins, reduced release of enzymes, reduced leukotriene formation from RA neutrophils, diminished gastrointestinal permeability [3], and changes of short-chain fatty acid profiles from intestinal microflora [7] were also provided. Another hypothesis for explaining clinical improvement is that, during Ramadan, patients tend to administer their drugs during the night. This may have beneficial effects, as some studies have suggested that bedtime or night doses compared with morning administration can lead to a better effect of the drug [1]. In our study, the improvement after fasting was independent from the timing of drug intake (Table 3).
Regarding the impact of fasting on SpA activity, it remains vastly understudied. A recent study reported that intermittent fasting in Ramadan has beneficial effects on psoriatic arthritis (PsA) disease expressed by the Disease Activity index for Psoriatic Arthritis (DAPSA), BASDAI, enthesitis, and dactylitis [1]. However, it seems too early to generalize these results to patients with SpA, especially that fasting has an established benefit on psoriasis [18], which may influence positively its impact on PsA. Further studies are consequently needed, hopefully with a larger number of patients, to confirm or refute this hypothesis in patients with SpA.
Another strength of this study is the evaluation of drug intake during the period of fasting. In fact, there are no data in the literature regarding the impact of Ramadan fast in terms of adherence to treatment or tolerability. So, our study is the first one in this sense, by confirming the safety of drug intake in patients with rheumatic diseases during Ramadan. No significant additional gastrointestinal side effects were noted. However, it should be noted that patient’s compliance to MTX was impaired in more than a quarter of patients (28.6%), mainly because of a lack of time between the two major meals (60%).
However, several limitations should be acknowledged. Firstly, the sample size was relatively limited which can be explained by the limited study duration. Furthermore, patients who changed dose or started or stopped any medication during the last consultation before Ramadan fast were not included, which reduced the sample size. But, in the face of the lack of data in the literature on this topic, this study may serve as a reference for physicians when asked by patients with rheumatic diseases about the consequences of fasting Ramadan. Secondly, the limited duration of our study may be short to confirm the sustainability of the observed benefits. Further investigations are needed to verify the long-term efficacy of fasting. Finally, a control group of non-fasting subjects would have strengthened our results. Actually, obtaining a control group comparable to the patient group was almost impossible, since the groups exempted from observing this religious duty include children, pregnant and breastfeeding women, and frail people with serious medical problems.
Conclusions
In conclusion, this study carries two messages we believe to be important. Fasting can be a possible way to induce rapid improvement of rheumatic diseases activity. In addition, patients with a specific fear of drug intake during this period can be reassured, which will enhance the adherence to treatment.
References
Adawi M, Damiani G, Bragazzi NL et al (2019) The impact of intermittent fasting (Ramadan fasting) on psoriatic arthritis disease activity, enthesitis, and dactylitis: a multicentre study. Nutrients 11. https://doi.org/10.3390/nu11030601
Adawi M, Watad A, Brown S, Aazza K, Aazza H, Zouhir M, Sharif K, Ghanayem K, Farah R, Mahagna H, Fiordoro S, Sukkar SG, Bragazzi NL, Mahroum N (2017) Ramadan fasting exerts immunomodulatory effects: insights from a systematic review. Front Immunol 8:1144. https://doi.org/10.3389/fimmu.2017.01144
Hafström I, Ringertz B, Gyllenhammar H et al (1988) Effects of fasting on disease activity, neutrophil function, fatty acid composition, and leukotriene biosynthesis in patients with rheumatoid arthritis. Arthritis Rheum 31:585–592. https://doi.org/10.1002/art.1780310502
Bragazzi NL, Watad A (2017) The impact of fasting on rheumatic diseases. Isr Med Assoc J IMAJ 19:378–379
Rouhani MH, Azadbakht L (2014) Is Ramadan fasting related to health outcomes? A review on the related evidence. J Res Med Sci Off J Isfahan Univ Med Sci 19:987–992
Boukhris O, Trabelsi K, Shephard RJ et al (2019) Sleep patterns, alertness, dietary intake, muscle soreness, fatigue, and mental stress recorded before, during and after Ramadan observance. Sports Basel Switz 7. https://doi.org/10.3390/sports7050118
Abendroth A, Michalsen A, Lüdtke R et al (2010) Changes of intestinal microflora in patients with rheumatoid arthritis during fasting or a Mediterranean diet. Forsch Komplementmed 2006 17:307–313. https://doi.org/10.1159/000322313
Kjeldsen-Kragh J, Haugen M, Borchgrevink CF et al (1991) Controlled trial of fasting and one-year vegetarian diet in rheumatoid arthritis. Lancet Lond Engl 338:899–902. https://doi.org/10.1016/0140-6736(91)91770-u
Sköldstam L, Larsson L, Lindström FD (1979) Effect of fasting and lactovegetarian diet on rheumatoid arthritis. Scand J Rheumatol 8:249–255. https://doi.org/10.3109/03009747909114631
Sköldstam L (1986) Fasting and vegan diet in rheumatoid arthritis. Scand J Rheumatol 15:219–221. https://doi.org/10.3109/03009748609102091
Müller H, de Toledo FW, Resch KL (2001) Fasting followed by vegetarian diet in patients with rheumatoid arthritis: a systematic review. Scand J Rheumatol 30:1–10
Kjeldsen-Kragh J, Sumar N, Bodman-Smith K, Brostoff J (1996) Changes in glycosylation of IgG during fasting in patients with rheumatoid arthritis. Br J Rheumatol 35:117–119. https://doi.org/10.1093/rheumatology/35.2.117
The effects of Ramadan fasting on body composition, blood pressure, glucose metabolism, and markers of inflammation in NAFLD patients: an observati... - PubMed - NCBI. https://www.ncbi.nlm.nih.gov/pubmed/28922096. Accessed 6 Feb 2020
Meo SA, Hassan A (2015) Physiological changes during fasting in Ramadan. JPMA J Pak Med Assoc 65:S6–S14
Effect of fasting with two meals on BMI and inflammatory markers of metabolic syndrome. - PubMed - NCBI. https://www.ncbi.nlm.nih.gov/pubmed/24199461. Accessed 6 Feb 2020
Aksungar FB, Topkaya AE, Akyildiz M (2007) Interleukin-6, C-reactive protein and biochemical parameters during prolonged intermittent fasting. Ann Nutr Metab 51:88–95. https://doi.org/10.1159/000100954
Ebrahimi S, Rahmani F, Avan A et al (2016) Effects of Ramadan fasting on the regulation of inflammation. J Fasting Health 4:32–37
Damiani G, Watad A, Bridgewood C et al (2019) The impact of Ramadan fasting on the reduction of PASI score, in moderate-to-severe psoriatic patients: a real-life multicenter study. Nutrients 11. https://doi.org/10.3390/nu11020277
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Informed consent was obtained from the patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben Nessib, D., Maatallah, K., Ferjani, H. et al. Impact of Ramadan diurnal intermittent fasting on rheumatic diseases. Clin Rheumatol 39, 2433–2440 (2020). https://doi.org/10.1007/s10067-020-05007-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05007-5