Abstract
Objectives
To evaluate the efficacy and safety of interleukin 17 (IL-17) inhibitors in two rheumatoid arthritis (RA) populations: biologic-naïve or tumor necrosis factor inhibitor inadequate responders (TNF-IR).
Method
A systematic search was performed in major electronic databases to identify relevant randomized controlled trials (RCTs) reporting the American College of Rheumatology 20% (ACR20), ACR50, ACR70 responses and adverse events (AEs) of IL-17 inhibitors versus placebo in patients with RA. We divided these patients into two subgroups: biologic-naïve or TNF-IR. The meta-analysis was performed using Review Manager 5.3 software. Results were expressed as risk ratio (RR) with pertinent 95% confidence interval (95% CI).
Results
Ten studies with a total of 2499 patients were included. For biologic-naïve patients, ACR50 and ACR70 responses were significantly better with IL-17 inhibitors than placebo (RR = 1.71, 95% CI 1.23–2.38, P = 0.001 and RR = 2.63, 95% CI 1.10–6.25, P = 0.03, respectively), but ACR20 responses for IL-17 inhibitors were not statistically superior to placebo (RR = 1.34, 95% CI 0.94–1.91, P = 0.11). For TNF-IR, IL-17 inhibitors were effective in achieving ACR20 (RR = 1.67, 95% CI 1.40–2.00, P < 0.00001), ACR50 (RR = 1.94, 95% CI 1.43–2.63, P < 0.0001), and ACR70 (RR = 2.11, 95% CI 1.26–3.55, P = 0.005) compared to placebo. In the safety analysis, IL-17 inhibitors did not show increased risk of any AEs by comparing to placebo in both biologic-naïve patients and TNF-IR.
Conclusion
IL-17 inhibitors were effective in the treatment of RA without increased risk of AEs, whether for biologic-naïve patients or TNF-IR.
Key Points • In this meta-analysis comparing IL-17 inhibitors with placebo in 2499 rheumatoid arthritis patients, IL-17 inhibitors improved ACR50 and ACR70, but not ACR20, responses in biologic-naïve patients. • IL-17 inhibitors improved ACR20, ACR50, and ACR70 responses in tumor necrosis factor inhibitor inadequate responders. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is an inflammatory and systemic autoimmune disease affecting approximately 1% of the adults worldwide [1]. It is characterized by chronic, symmetrical, multiple joints, and invasive synovitis that mainly involves the peripheral joints [2]. It is usually a progressive disease with cartilage damage, joint destruction, and complications of numerous extra-articular manifestations, which is associated with deformed joint, decline in functional status, decreased quality of life, and premature mortality [3, 4].
Conventional disease-modifying anti-rheumatic drugs (DMARDs) are used as a first-line therapy for the patients newly diagnosed with RA [5]. However, these DMARDs only work for a small percentage of patients. Novel biological agents have increasingly become the focus in RA therapeutic regimens.
Tumor necrosis factor (TNF)-α inhibitors gradually replace conventional medicine and are initial choices for RA patients who fail to respond to DMARDs and/or could not tolerate their toxicities [6]. However, in clinical practice, a proportion of patients treated with anti-TNF-α agents presented with inadequate treatment response [7] or intolerable side effects [8]. Hence, novel biological agents represent a promising therapeutic avenue for these patients.
Current scientific evidence shows that interleukin 17 (IL-17) and IL-17-producing-T helper cells (Th17) play an important role in the progression of RA [9, 10]. IL-17 induces negative feedback regulation through the induction of prostaglandin E2 (PGE2) while it stimulates proinflammatory pathways such as inflammatory cytokine production, pannus growth, and synovial neoangiogenesis, resulting in structural destruction of rheumatoid joints [11,12,13]. Current research shows that there is a significantly elevated level of IL-17 in synovium, serum, and synovial fluid from treatment-naïve early RA patients [14]. Therefore, it is indicated that blockade of IL-17 may reduce inflammation and bone erosions [15]. Moreover, it could be a most concerned therapeutic method for patients with RA.
In recent years, randomized controlled trials (RCTs) of IL-17 inhibitors for the treatment of RA have been reported and the conclusions are different. In addition, it is not known whether IL-17 inhibitors would be effective in patients who have an inadequate response to TNF inhibitors (TNF-IR) or biologic-naïve. Some researches [16, 17] showed other biologic treatments can produce significant benefits in patients who had TNF-IR, but an independent study [18] got an opposite conclusion. The aim of our meta-analysis was to review systematically available evidence on efficacy and safety of IL-17 inhibitors in the two RA populations.
Methods
Eligibility criteria
All eligible studies in this meta-analysis met the following criteria: (i) they were RCTs that enrolled patients with rheumatoid arthritis; (ii) duration of treatment as the main limitation was ≥ 10 weeks; (iii) they used a parallel design or crossover design of IL-17 inhibitors versus placebo; (iv) the reported data on American College of Rheumatology 20% (ACR20), ACR50, ACR70 response and adverse events (AEs) were investigated; and (v) eligible patients are biologic-naïve or TNF-IR.
Search strategy
A systematic review of the literature was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement protocol [19]. We searched electronic database of Pubmed, Embase, and Cochrane Library for publications from inception through April 2018 using the keywords “rheumatoid arthritis,” “secukinumab,” “brodalumab,” “ixekizumab,” “AIN457,” “AMG827,” “LY2439821” “anti-IL-17,” “IL-17 inhibitor” or “IL-17 antagonists.”
Data extraction
Articles screening was performed by two independent researchers. Firstly, they evaluated titles and abstracts of cited articles to determine their relevance. Then, they reviewed full papers to confirm all trials meeting the eligibility criteria. Discrepancies were further resolved through discussion or agreement of a third researcher. When there were multiple studies from the same trial, the most completely or recently reported data were eligible.
Methodological quality
Methodological quality of included trials was further assessed using modified Jadad score [20]. Scores ranged from 0 to 8 (a high score indicating high quality) with a score of ≥ 4 indicating high quality.
Meta-analysis
The analysis of efficacy was dependent on the increasing number of patients achieving ACR20, ACR50, and ACR70 responses from baseline. We assess safety by reviewing AEs, including any AEs, serious adverse events (SAEs), infection, hypertension, and neutropenia. Subgroup analyses for two different RA populations were performed.
The statistical analysis was assessed by using Review Manager 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark) from the Cochrane Collaboration. The dichotomous variables were assessed using risk ratio (RR), and continuous variables were assessed using mean differences (MD). P < 0.05 was considered statistically significant, and 95% confidence interval (CI) were reported.
Homogeneity was tested by using the Q statistic the I2 statistic [21]. When I2 was higher than 50%, random-effects model was used and which indicates a statistical heterogeneity. Otherwise, when I2 was lower than 50%, a fixed-effects model was used. We performed a subgroup analysis to assess the potential confounding effect of heterogeneity and comparing the efficacy and safety of different subgroups.
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Results
Literature search and study characteristics
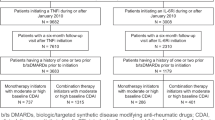
A total of 293 potential relevant articles were retrieved initially from various electronic databases. We retrieved 247 studies after removing duplicates. After reviewing the titles and abstracts, 38 articles were assessed for eligibility. However, 28 articles were excluded due to various reasons (not RCT, no required data or mixed biologic-naïve, and TNF-IR). Finally, ten studies [22,23,24,25,26,27,28,29,30,31] including eleven RCTs met eligibility criteria in the final analysis (Fig. 1). Seven articles [22,23,24,25,26,27,28] compared the efficacy and safety of IL-17 inhibitor with placebo in biologics-naïve patients. Four articles [24, 29,30,31] evaluated the efficacy and safety of IL-17 inhibitor in TNF-IR. The article published by Genovese MC et al. in 2014 [24] contains an analysis of IL-17 inhibitor versus placebo in both two RA populations. Although the article published by Genovese MC et al. in 2013 [32] reported the efficacy and safety of different doses of secukinumab in patients with active RA, they mixed the biologic-naïve patients and TNF-IR, so we excluded this article. The pooled analysis included 2499 patients with RA (1022 patients in biologics-naïve subgroup and 1477 patients in TNF-IR subgroup). The majority of studies included were allocated high-quality scores (all of the eleven RCTs had a score ≥ 6). Included studies, basic characteristics of enrolled patients, details about drug therapy, study duration, and modified Jadad scores are briefly presented in Table 1.
Efficacy
ACR20 response
Nine studies including ten RCTs with 2481 patients reported the proportion of patients meeting ACR20 improvement criteria. Compared to placebo, IL-17 inhibitors showed a trend toward efficacy but did not have statistical significance in achieving ACR20 response [53.4% vs. 43.9%; RR = 1.34, 95% CI 0.94–1.91, P = 0.11, I2 = 77%; Fig. 2] for biologics-naïve patients. The proportion of ACR20 responders was statistically higher with IL-17 inhibitors compared to placebo in TNF-IR [37.6% vs. 22.5%; RR = 1.67, 95% CI 1.40–2.00, P < 0.00001, I2 = 0%; Fig. 2].
ACR50 response
Eight studies including nine RCTs with 2403 patients reported the proportion of patients meeting ACR50 improvement criteria. Compared to placebo, IL-17 inhibitors were more effective in achieving ACR50 response for both biologics-naïve (25.1% vs. 16.5%; RR = 1.71, 95% CI 1.23–2.38, P = 0.001, I2 = 60%; Fig. 3) and TNF-IR (17.9% vs. 9.3%; RR = 1.94, 95% CI 1.43–2.63, P < 0.0001, I2 = 11%; Fig. 3).
ACR70 response
Eight studies including nine RCTs with 2329 patients reported the proportion of patients meeting ACR70 improvement criteria. Compared to placebo, IL-17 inhibitors were more effective in achieving ACR70 response for both biologics-naïve (7.7% vs. 2.7%; RR = 2.63, 95% CI 1.10–6.25, P = 0.03, I2 = 6%; Fig. 4) and TNF-IR (7.2% vs. 3.4%; RR = 2.11, 95% CI 1.26–3.55, P = 0.005, I2 = 0%; Fig. 4).
Safety
The focus in safety that accompanies IL-17 inhibitor therapy for patients with RA was on infection, hypertension, and neutropenia. The most commonly reported infection events were upper respiratory tract infections, urinary tract infections, and diarrhea.
For biologics-naïve patients, results for safety indicated that the IL-17 inhibitor did not increase the risks of any AEs (53.0% vs. 47.6%; RR = 1.14, 95% CI 0.98–1.32, P = 0.09, I2 = 0%) or SAEs (18.3% vs. 13.0%; RR = 1.16, 95% CI 0.86–1.55, P = 0.33, I2 = 0%). In the analysis of individual adverse events, IL-17 inhibitors also had not significant increase in the risk of upper respiratory tract infections (4.2% vs. 1.0%; RR = 2.72, 95% CI 0.91–8.13, P = 0.07, I2 = 0%), urinary tract infection (5.3% vs. 4.4%; RR = 1.18, 95% CI 0.50–2.80, P = 0.71, I2 = 13%), diarrhea (8.8% vs. 2.2%; RR = 1.98, 95% CI 0.45–8.68, P = 0.37, I2 = 0%), hypertension (4.2% vs. 4.5%; RR = 0.92, 95% CI 0.33–2.58, P = 0.88, I2 = 44%), or neutropenia (2.3% vs. 0%; RR = 2.00, 95% CI 0.25–16.02, P = 0.52, I2 = 0%). Nineteen of 771 biologics-naïve patients in IL-17 inhibitors group and 6 of 251 patients in placebo group leaded to discontinuations due to adverse events; however, no significant difference between the two groups (2.5% vs. 2.4%; RR = 0.88, 95% CI 0.39–1.96, P = 0.75, I2 = 8%).
For TNF-IR, we found that the IL-17 inhibitor also did not increase the risks of any AEs (58.4% vs. 53.4%; RR = 1.09, 95% CI 0.99–1.21, P = 0.07, I2 = 44%) or SAEs (4.6% vs. 2.8%; RR = 1.59, 95% CI 0.89–2.85, P = 0.12, I2 = 34%). In the analysis of individual AEs, IL-17 inhibitors had not significant increase in the risk of upper respiratory tract infections (3.7% vs. 4.8%; RR = 0.76, 95% CI 0.44–1.33, P = 0.34, I2 = 0%), urinary tract infection (3.1% vs. 3.2%; RR = 0.96, 95% CI 0.44–2.13, P = 0.93, I2 = 37%), diarrhea (3.0% vs. 1.4%; RR = 1.99, 95% CI 0.78–5.03, P = 0.15, I2 = 73%), hypertension (3.0% vs. 2.1%; RR = 1.41, 95% CI 0.68–2.93, P = 0.36, I2 = 0%), or neutropenia (1.3% vs. 0.8%; RR = 1.52, 95% CI 0.52–4.38, P = 0.44, I2 = 0%). Twenty-four of 981 TNF-IR in IL-17 inhibitors group and 14 of 496 patients in placebo group leaded to discontinuations due to adverse events, also no significant difference between two groups (2.4% vs. 2.8%; RR = 0.87, 95% CI 0.45–1.66, P = 0.67, I2 = 38%). The results of safety outcomes for two rheumatoid arthritis populations were shown in Table 2 respectively.
In addition, brodalumab should be more concerned. Some of the patients receiving brodalumab have serious adverse events, including suicide. An article reported that four patients died of suicide after receiving brodalumab [33]. One of the included articles [26] reported a suicide attempter in the 210-mg brodalumab group, although there was no clear evidence in the current study that suicidal tendencies were related to the use of brodalumab.
Discussion
The meta-analysis results show that IL-17 inhibitors are effective in achieving target of ACR20, ACR50, and ACR70 without increasing risks of any AEs, serious AEs, or individual AEs in both biologic-naïve and TNF-IR patients with RA. In Kunwar’ s meta-analysis [34] of seven RCTs with 1226 patients, IL-17 inhibitors were effective in the treatment of RA without increased risk of any or serious AEs, consistent with our observations in this study with higher number of RCTs (n = 11) and patients (n = 2499).
Many previous RCTs showed that some other biological agents such as abatacept [17], rituximab [18], tocilizumab [35], and golimumab [36] could improve therapeutic outcomes in TNF-IR patients with RA. Similar results appeared on IL-17 inhibitors in our meta-analysis. Alzabin S’s study showed that patients with lack of response to anti-TNF-α agents had a relatively high baseline Th17 cell level [37], which may be a possible mechanism for this result.
Safety analysis showed IL-17 inhibitors did not increase in the incidence of any AEs, SAEs, infections, hypertension, neutropenia, or treatment discontinuations compared with placebo. The infections mentioned in this article mainly referred to upper respiratory tract infection, urinary tract infection, and diarrhea. IL-17A plays an important role in host defense against microorganisms and in the development of chronic inflammation [38, 39]. Therefore, IL-17 inhibitors can increase the incidence of infection. However, our study showed that IL-17 inhibitors were relatively safe for patients with upper respiratory tract infections, urinary tract infections, and diarrhea.
The risk of hypertension in RA patients is increased compared with normal people, which may be related to inflammatory activity [40]. While some DMARDs [41] for the treatment of RA can also lead to elevated blood pressure, IL-17 inhibitors do not increase the incidence of hypertension, showing its safety in cardiovascular events.
Some patients included in this article were taking concomitant methotrexate, which has also been associated with neutropenia [42]. However, the use of Il-17 inhibitors did not increase the risk of neutropenia in either biologics-naïve or TNF-IR subgroup. Therefore, IL-17 inhibitors are more suitable for patients who have had adverse reactions to previous drug us.
A 64-week study [43] of safety and efficacy of subcutaneous ixekizumab treatment in biologic-naïve and TNF-IR patients with RA showed that most AEs were mild to moderate in severity and did not lead to research discontinuation. Clinical responses observed at week 16 (improving RA signs and symptoms) were maintained or improved through the whole 64 weeks.
There are several limitations to our meta-analysis: relatively small number of included studies, variable forms and doses of IL-17 inhibitors, and short study duration. We combined data on three IL-17 inhibitors: secukinumab, ixekizumab, and brodalumab, respectively. Some of the patients were injected subcutaneously and some were injected intravenously; besides, the dosage of the same drug is different in these studies. For example, patients were all given secukinumab; some were assigned to receive intravenous at a dose of 10 mg/kg, while others were assigned to receive subcutaneous 75 mg or 150 mg. The durations of included studies are ranging from 10 to 24 weeks. The short time of follow-up of the studies is the biggest limitation. In order to acquire more accurate results, more high-quality, large-scale, long following-up clinical trials are needed.
In summary, IL-17 inhibitors are clearly effective and well tolerated in patients with RA who are either naive to biologic agents or have a TNF-IR.
References
McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365:2205–2219
Andersson AK, Li C, Brennan FM (2008) Recent developments in the immunobiology of rheumatoid arthritis. Arthritis Res Ther 10:204
Gabriel SE, Michaud K (2009) Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther 11:229
Uhlig T, Moe RH, Kvien TK (2014) The burden of disease in rheumatoid arthritis. Pharmacoeconomics 32:841–851
Singh JA, Saag KG, Bridges SL Jr et al (2016) 2015 American College of Rheumatology Guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 68:1–25
Smolen JS, Landewé R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, Nam J, Ramiro S, Voshaar M, van Vollenhoven R, Aletaha D, Aringer M, Boers M, Buckley CD, Buttgereit F, Bykerk V, Cardiel M, Combe B, Cutolo M, van Eijk-Hustings Y, Emery P, Finckh A, Gabay C, Gomez-Reino J, Gossec L, Gottenberg JE, Hazes JMW, Huizinga T, Jani M, Karateev D, Kouloumas M, Kvien T, Li Z, Mariette X, McInnes I, Mysler E, Nash P, Pavelka K, Poór G, Richez C, van Riel P, Rubbert-Roth A, Saag K, da Silva J, Stamm T, Takeuchi T, Westhovens R, de Wit M, van der Heijde D (2017) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 76:960–977
Jamnitski A, Krieckaert CL, Nurmohamed MT, Hart MH, Dijkmans BA, Aarden L, Voskuyl AE, Wolbink GJ (2012) Patients non-responding to etanercept obtain lower etanercept concentrations compared with responding patients. Ann Rheum Dis 71:88–91
Kroesen S, Widmer AF, Tyndall A, Hasler P (2003) Serious bacterial infections in patients with rheumatoid arthritis under anti-TNF-alpha therapy. Rheumatology (Oxford) 42:617–621
Chabaud M, Durand JM, Buchs N, Fossiez F, Page G, Frappart L, Miossec P (1999) Human interleukin-17: a T cell-derived proinflammatory cytokine produced by the rheumatoid synovium. Arthritis Rheum 42:963–970
Shen H, Goodall JC, Hill Gaston JS (2009) Frequency and phenotype of peripheral blood Th17 cells in ankylosing spondylitis and rheumatoid arthritis. Arthritis Rheum 60:1647–1656
Ito H, Yamada H, Shibata TN, Mitomi H, Nomoto S, Ozaki S (2011) Dual role of interleukin-17 in pannus growth and osteoclastogenesis in rheumatoid arthritis. Arthritis Res Ther 13:R14
Sato K, Suematsu A, Okamoto K, Yamaguchi A, Morishita Y, Kadono Y, Tanaka S, Kodama T, Akira S, Iwakura Y, Cua DJ, Takayanagi H (2006) Th17 functions as an osteoclastogenic helper T cell subset that links T cell activation and bone destruction. J Exp Me 203:2673–2682
Pickens SR, Volin MV, Mandelin AM 2nd, Kolls JK, Pope RM, Shahrara S (2010) IL-17 contributes to angiogenesis in rheumatoid arthritis. J Immunol 184:3233–3241
Roşu A, Mărgăritescu C, Stepan A, Muşetescu A, Ene M (2012) IL-17 patterns in synovium, serum and synovial fluid from treatment-naïve, early rheumatoid arthritis patients. Romanian J Morphol Embryol 53:73–80
Lubberts E (2008) IL-17/Th17 targeting: on the road to prevent chronic destructive arthritis? Cytokine 41:84–91
Cohen SB, Emery P, Greenwald MW, Dougados M, Furie RA, Genovese MC, Keystone EC, Loveless JE, Burmester GR, Cravets MW, Hessey EW, Shaw T, Totoritis MC, REFLEX Trial Group (2006) Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum 54:2793–2806
Genovese MC, Becker J, Schiff M, Luggen M, Sherrer Y, Kremer J et al (2005) Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med 353:1114–1123
Torrente-Segarra V, Acosta Pereira A, Morla R, Ruiz JM, Clavaguera T, Figuls R, Corominas H, Geli C, Roselló R, de Agustín JJ, Alegre C, Pérez C, García A, Rodríguez de la Serna A (2016) VARIAR study: assessment of short-term efficacy and safety of rituximab compared to an tumor necrosis factor alpha antagonists as second-line drug therapy in patients with rheumatoid arthritis refractory to a first tumor necrosis factor alpha antagonist. Reumatol Clin 12:319–322
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:1–34
Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord 12:232–236
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Tlustochowicz W, Rahman P, Seriolo B, Krammer G, Porter B, Widmer A, Richards HB (2016) Efficacy and safety of subcutaneous and intravenous loading dose regimens of secukinumab in patients with active rheumatoid arthritis: results from a randomized phase II study. J Rheumatol 43:495–503
Burmester GR, Durez P, Shestakova G, Genovese MC, Schulze-Koops H, Li Y, Wang YA, Lewitzky S, Koroleva I, Berneis AA, Lee DM, Hueber W (2016) Association of HLA-DRB1 alleles with clinical responses to the anti-interleukin-17A monoclonal antibody secukinumab in active rheumatoid arthritis. Rheumatology (Oxford) 55:49–55
Genovese MC, Greenwald M, Cho CS, Berman A, Jin L, Cameron GS, Benichou O, Xie L, Braun D, Berclaz PY, Banerjee S (2014) A phase II randomized study of subcutaneous ixekizumab, an anti-interleukin-17 monoclonal antibody, in rheumatoid arthritis patients who were naive to biologic agents or had an inadequate response to tumor necrosis factor inhibitors. Arthritis Rheum 66:1693–1704
Genovese MC, Van den Bosch F, Roberson SA, Bojin S, Biagini IM, Ryan P, Sloan-Lancaster J (2010) LY2439821, a humanized anti-interleukin-17 monoclonal antibody, in the treatment of patients with rheumatoid arthritis: a phase I randomized, double-blind, placebo-controlled, proof-of-concept study. Arthritis Rheum 62:929–939
Pavelka K, Chon Y, Newmark R, Lin SL, Baumgartner S, Erondu N (2015) A study to evaluate the safety, tolerability, and efficacy of brodalumab in subjects with rheumatoid arthritis and an inadequate response to methotrexate. J Rheumatol 42:912–919
Martin DA, Churchill M, Flores-Suarez L, Cardiel MH, Wallace D, Martin R, Phillips K, Kaine JL, Dong H, Salinger D, Stevens E, Russell CB, Chung JB (2013) A phase Ib multiple ascending dose study evaluating safety, pharmacokinetics, and early clinical response of brodalumab, a human anti-IL-17R antibody, in methotrexate-resistant rheumatoid arthritis. Arthritis Res Ther 15:R164
Hueber W, Patel DD, Dryja T et al (2010) Effects of AIN457, a fully human antibody to interleukin-17A, on psoriasis, rheumatoid arthritis, and uveitis. Sci Transl Med 2:52ra72
Blanco FJ, Möricke R, Dokoupilova E, Codding C, Neal J, Andersson M, Rohrer S, Richards H (2017) Secukinumab in active rheumatoid arthritis: a phase III randomized, double-blind, active comparator-and placebo-controlled study. Arthritis Rheum 69:1144–1153
Dokoupilová E, Aelion J, Takeuchi T, Malavolta N, Sfikakis PP, Wang Y, Rohrer S, Richards HB (2018) Secukinumab after anti-tumour necrosis factor-α therapy: a phase III study in active rheumatoid arthritis. Scand J Rheumatol 47:276–281
Tahir H, Deodhar A, Genovese M, Takeuchi T, Aelion J, van den Bosch F, Haemmerle S, Richards HB (2017) Secukinumab in active rheumatoid arthritis after anti-TNFα therapy: a randomized, double-blind placebo-controlled phase 3 study. Rheumatol Ther 4:475–488
Genovese MC, Durez P, Richards HB, Supronik J, Dokoupilova E, Mazurov V, Aelion JA, Lee SH, Codding CE, Kellner H, Ikawa T, Hugot S, Mpofu S (2013) Efficacy and safety of secukinumab in patients with rheumatoid arthritis: a phase II, dose-finding, double-blind, randomised, placebo controlled study. Ann Rheum Dis 72:863–869
Papp KA, Reich K, Paul C, Blauvelt A, Baran W, Bolduc C, Toth D, Langley RG, Cather J, Gottlieb AB, Thaçi D, Krueger JG, Russell CB, Milmont CE, Li J, Klekotka PA, Kricorian G, Nirula A (2016) A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br J Dermatol 175:273–286
Kunwar S, Dahal K, Sharma S (2016) Anti-IL-17 therapy in treatment of rheumatoid arthritis: a systematic literature review and meta-analysis of randomized controlled trials. Rheumatol Int 36:1065–1075
Emery P, Keystone E, Tony HP, Cantagrel A, van Vollenhoven R, Sanchez A, Alecock E, Lee J, Kremer J (2008) IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomised placebo-controlled trial. Ann Rheum Dis 67:1516–1523
Smolen JS, Kay J, Doyle MK, Landewé R, Matteson EL, Wollenhaupt J, Gaylis N, Murphy FT, Neal JS, Zhou Y, Visvanathan S, Hsia EC, Rahman MU (2009) GO-AFTER study investigators. Golimumab in patients with active rheumatoid arthritis after treatment with tumour necrosis factor alpha inhibitors (GO-AFTER study): a multicentre, randomised, double-blind, placebo-controlled, phase III trial. Lancet 374:210–221
Alzabin S, Abraham SM, Taher TE, Palfreeman A, Hull D, McNamee K, Jawad A, Pathan E, Kinderlerer A, Taylor PC, Williams R, Mageed R (2012) Incomplete response of inflammatory arthritis to TNFα blockade is associated with the Th17 pathway. Ann Rheum Dis 71:1741–1748
Puel A, Cypowyj S, Bustamante J, Wright JF, Liu L, Lim HK, Migaud M, Israel L, Chrabieh M, Audry M, Gumbleton M, Toulon A, Bodemer C, el-Baghdadi J, Whitters M, Paradis T, Brooks J, Collins M, Wolfman NM, al-Muhsen S, Galicchio M, Abel L, Picard C, Casanova JL (2011) Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science 332:65–68
Valeri M, Raffatellu M (2016) Cytokines IL-17 and IL-22 in the host response to infection. Pathog Dis 74:ftw111
Midtbø H, Gerdts E, Kvien TK, Olsen IC, Lønnebakken MT, Davidsen ES, Rollefstad S, Semb AG (2016) The association of hypertension with asymptomatic cardiovascular organ damage in rheumatoid arthritis. Blood Press 25:298–304
Ishaq M, Razzaque S, Shohail F, Kumar A, Muhammad JS (2017) Onset of hypertension in leflunamide treated low socioeconomic rheumatoid arthritis patients: an unseen iceberg. Curr Rheumatol Rev (Epub ahead of print). https://doi.org/10.2174/1573397114666171227211048
Kinder AJ, Hassell AB, Brand J, Brownfield A, Grove M, Shadforth MF (2005) The treatment ofinflammatory arthritis with methotrexate in clinical practice: treatment duration and incidence of adverse drug reactions. Rheumatology 44:61–66
Genovese MC, Braun DK, Erickson JS, Berclaz PY, Banerjee S, Heffernan MP, Carlier H (2016) Safety and efficacy of open-label subcutaneous ixekizumab treatment for 48 weeks in a phase II study in biologic-naive and TNF-IR patients with rheumatoid arthritis. J Rheumatol 43:289–297
Acknowledgments
The authors wish to thank all researchers of the included studies who provided additional data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, D., Hou, SY., Zhao, S. et al. Meta-analysis of IL-17 inhibitors in two populations of rheumatoid arthritis patients: biologic-naïve or tumor necrosis factor inhibitor inadequate responders. Clin Rheumatol 38, 2747–2756 (2019). https://doi.org/10.1007/s10067-019-04608-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04608-z