Abstract
Previous in vitro studies have shown that oxidized low-density lipoprotein (ox-LDL) plays a role in the pathogenesis of osteoarthritis (OA). Paraoxonase-1 (PON1) protects both low-density lipoproteins (LDLs) and high-density lipoprotein (HDLs) against oxidative damage from circulating cells. In addition, PON1 is inactivated by ox-LDL and preserved by antioxidants. However, the relationship between serum ox-LDL, oxidative stress, and PON1 in knee OA remains unclear. Therefore, we investigated ox-LDL association with oxidative stress and PON1 in knee OA, and evaluated their relationships using radiological and clinical parameters. This study included 203 patients and 194 controls. The severity of OA was classified based on the Kellgren–Lawrence scoring system. In addition, each patient was clinically evaluated using the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) score. Plasma concentrations of ox-LDL, oxidative stress markers, and PON1 were measured. Serum ox-LDL and oxidant parameters were significantly higher in patients compared to controls (p < 0.001 for all), whereas PON1 was significantly lower (p < 0.001). ox-LDL was inversely correlated with PON1, whereas it was positively correlated with radiographic severity, WOMAC score, and oxidant parameters. We found an association between the levels of various serum markers of oxidative injury, especially ox-LDL, and increasing severity of knee OA, as well as indirect evidence for their regulation by PON1. oxLDL seems to play a critical role in OA, both in the beginning, and during progression of, the disease. Therefore, serum oxLDL levels may be a helpful biomarker to evaluate the severity of knee OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous in vitro studies have reported that oxidized low-density lipoprotein (ox-LDL) plays a role in the pathogenesis of articular cartilage degeneration [1,2,3]. ox-LDL is a lipid peroxidation product induced by oxidative stress that contributes to inflammation through specific gene expression [4, 5]. It has been shown that ox-LDL plays a critical role in the development of atherosclerosis [6, 7]. It has also been reported that ox-LDL may be involved in the pathogenesis of osteoarthritis (OA) [8, 9]. Indeed, this molecule stimulates reactive oxygen species (ROS) production and promotes cartilage degradation due to collagen breakdown [1, 4, 5, 10].
Previously, we examined Paraoxonase-1 (PON1) and oxidative stress in knee OA [11]. PON-1 is a hydrolytic enzyme associated with high-density lipoprotein (HDL). It protects both low-density lipoproteins (LDLs) and HDLs against oxidative damage from circulating cells [12,13,14]. In addition, PON1 is inactivated by ox-LDL and preserved by antioxidants [15, 16]. To the best of our knowledge, there is no report on the relationship between serum ox-LDL, oxidative stress, and PON1 in knee OA in the English literature.
Therefore, we sought to address the following questions: (1) Is there a relationship between ox-LDL and oxidative stress markers in knee OA?; (2) Is there a relationship between ox-LDL and PON1 in knee OA?; and (3) Is there a relationship between ox-LDL, radiographic severity, and clinical parameters?
Materials and methods
Study population
This cross-sectional study included 203 patients with OA (161 females and 42 males) and 194 healthy controls (147 females and 47 males). The diagnosis of OA was confirmed based on American College of Rheumatology criteria [17]. Exclusion criteria were consistent with those previously described [11]. Controls were selected on the basis of having a similar distribution to the cases in terms of age, body mass index (BMI), and gender. For inclusion in the control group, subjects had to have no known knee OA symptoms. This study was approved by the local Ethics Committee and written informed consent was obtained from all patients.
Radiologic and clinical assessment
Conventional knee radiographs were taken for radiologic assessment as previously described [18]. Radiographic grading of the knee OA was evaluated utilizing the Kellgren-Lawrence (KL) scoring system [19].The Western Ontario and McMaster University Osteoarthritis Index (WOMAC) was used clinical evaluation [20].
Biochemical analysis
The serum was prepared by centrifugation at 3000 rpm for 10 min. All samples were stored at −80 °C until these were analysed. The levels of triglycerides (TG), total cholesterol (TC), HDL cholesterol (HDL-C), and LDL-cholesterol (LDL-C) were measured using enzymatic methods (Abbott, Wiesbaden-Delkenheim, Germany) with an autoanalyser (Aeroset®; Abbott). ox-LDL concentrations were measured by a sandwich enzyme-linked immunosorbent assay (ELISA) method (Immundiagnostik, Cat no: 201–12-1543) [21]. ELISAs were carried out according to the manufacturer’s instructions. Serum PON1 and plasma concentration were measured together with other enzymes of oxidative status [lipid hydroperoxide (LOOH), total oxidative status (TOS), and the oxidative stress index (OSI)] and antioxidative status [(free sulfhydryl groups, −SH = total thiol), and total antioxidative capacity (TAC)].The methods were determined as previously described [11, 22, 23].
Statistical methods
All statistical analyses were conducted using the SPSS 16 computer program. Chi-square test and Student’s t-test and one-way ANOVA were used for group comparisons. For correlation analysis, a Pearson’s correlation test was used. Standardized β-values in multiple linear regressions were described. Values of P < 0.05 were significant.
Results
The demographic characteristics of the study participants are shown in Table 1. There was no statistical difference between patients and control subjects in age, BMI, female/male ratio and in terms of fasting blood triglyceride, total cholesterol, or LDL and HDL levels (p > 0.05). The ox-LDL and oxidative stress were significantly higher in OA, whereas PON1 was significantly lower in OA (p < 0.001). Furthermore, there was no significant difference between the two groups (p > 0.05) according to antioxidative capacity.
We divided our patients into four subgroups according to the KL scoring system: Grade 1 (n = 50), grade 2 (n = 54), grade 3 (n = 49), and grade 4 (n = 50). The lowest and highest mean ox-LDL levels were observed in patients with grades 1 and 4, respectively (ANOVA, P < 0.001, Fig. 1). The relationships between ox-LDL and clinical and laboratory characteristics are demonstrated in Table 2. A correlation was established between the ox-LDL and radiographic grading and PON1 (p < 0.001 for all). In addition, there was an association between the ox-LDL and oxidative stress, age, and WOMAC score (p < 0.05 for all; Table 2). The inverse correlation between serum ox-LDL and PON1 is shown in Fig. 2. Also, the ox-LDL was independently associated with OA grade (β = 0.440, p < 0.001) and age (β = 0.211, p = 0.002) according to a multiple regression analysis (Table 2).
Discussion
In previous studies, it has been shown that ox-LDL may be associated with the pathogenesis of OA in vitro. However, the association between serum ox-LDL, oxidative stress, and PON1 in OA is unknown, and we believe that, if there is an association between serum ox-LDL, oxidative stress and PON1, ox-LDL may be a biomarker for follow-up in patients with knee OA. The present study showed that ox-LDL and oxidative stress parameters were significantly higher in an OA versus control group, whereas PON1 was significantly lower in the OA group. In addition, serum ox-LDL was positively correlated with oxidant parameters, knee OA grade, and WOMAC score, but inversely correlated with serum PON1. Finally, ox-LDL was positively correlated with radiographic severity and WOMAC score.
We found that serum ox-LDL was significantly higher in patients with OA. The increased serum ox-LDL in patients with knee OA could be due to oxidative stress. This hypothesis is supported by a previous study by Nishimura et al. [4], who showed that ox-LDL increases the production of intracellular ROS via activation of NF-kappaB in cultured bovine articular chondrocytes . [4]. It is known that a higher plasma level of ox-LDL is a risk factor for atherosclerosis, which is important in the development and progression of cardiovascular disease and its complications [6, 7, 24]. ox-LDL was also produced by generation of ROS from different cell types such as endothelial cells, vascular smooth muscle cells, leukocytes, and platelets [25,26,27]. On the other hand, there are similarities between OA and atherosclerosis [9, 28]. OA, similar to atherosclerosis, is an age-related inflammatory disease caused by inflammatory mediators released by cartilage, bone, and the synovium [29]. In addition, as in atherosclerosis, altered lipid metabolism has been implicated as playing a critical role in OA development [9, 28, 30, 31]. Increased lipid content in the superficial layer of articular cartilage has been reported [32]. Furthermore, synovial tissue in joints with OA is often inflamed, and inflammatory cytokines, including ox-LDL – which is oxidatively modified extra-articularly – contribute to cartilage damage [33]. Therefore, inflammatory cells in articular joints secrete ROS, which could promote the oxidation of natural LDL to ox-LDL [4, 5].
In the current study, levels of oxidative stress markers were significantly higher in OA. These results confirm that OA is associated with oxidative damage, in agreement with previous studies [11, 23]. We believe that LOOH can be used as a predictor of oxidative stress. LOOH is the first comparatively stable product of the lipid peroxidation reaction and is an important tool in oxidative stress research [22, 34, 35]. In addition, ox-LDL, as the basic structure of LOOH, is closely associated with the atherosclerotic process [34]. Likewise, lipid peroxidation to cartilage matrix protein degradation has been clearly demonstrated in the etiopathogenesis of OA [1]. Furthermore, in the current study, serum ox-LDL was positively correlated with oxidative stress markers. Collectively, these results suggest that the cause of elevated serum ox-LDL levels may be increased lipid oxidation.
In our previous study [11], we showed important relationships between decreased serum PON1 and increased oxidative stress parameters and knee OA. Therefore, we explored the correlation between serum PON1 and ox-LDL in knee OA. Our study showed that the ox-LDL level was inversely correlated with PON1 in knee OA. These results confirm the relationship between PON1 and its protective role against LDL oxidation [15, 16]. PON1 is an important component of the antioxidant mechanism. Indeed, it is known to protect LDL against oxidation stimulated either by copper ion or by a free radical generator system [15, 36].
A correlation was established between the ox-LDL level and radiographic severity. The highest ox-LDL levels were observed in grade 4 OA, with the lowest levels seen in grade 1 OA. The cause of the increase in ox-LDL with advancing OA stage is unknown, but structural changes are advanced in an ‘end-stage’ knee joint. Similarly, Akagi et al. [37] reported that the immunoreactivity of ox-LDL was correlated with the grade of cartilage degradation in OA. Therefore, ox-LDL can lead to local inflammation throughout the joint and accelerate the pathophysiology of cartilage degradation [9, 28]. Furthermore, there was an association between ox-LDL and WOMAC score, possibly due to oxidation of lipids under increased oxidative stress in OA. The symptoms in knee OA are well-described by the WOMAC score [20]. The altered histological structure of the articular cartilage, synovial tissue, joint capsule, and other soft tissues may be responsible for joint pain and symptoms [38].
In this study, we have established a relationship between PON-I and ox-LDL and other lipo-proteins in different grades of OA. However, establishing these as markers need further studies as both PON-I and ox-LDL show a similar trend in other inflammatory diseases as rheumatoid arthritis.
Clinical implications
Notably, there is an important interconnection between lipid metabolism (body fat mass) and knee OA [39, 40]. Therefore, in the elderly, to increase muscle mass, physical activity should be encouraged. In addition, statins – which are widely used for the treatment of hypercholesterolemia – may also limit the progression of OA [41]. Furthermore, antioxidant treatments with nutraceuticals may prevent or alleviate OA as adjuvants [39].
There were some limitations to this study. First, it used a cross-sectional design. Second, serological correlation studies could potentially provide greater insights into the mechanisms of knee OA. In addition, measurements in synovial fluid could support our results. However, we did not have the opportunity to perform synovial aspiration for ethical reasons.
Conclusions
In conclusion, we found an association between the levels of various serum markers of oxidative injury, especially ox-LDL, and increasing severity of knee OA, as well as indirect evidence for their regulation by PON1. It is possible that increased oxLDL levels are associated with oxidative stress, as observed in cardiovascular disease. oxLDL seems to play a critical role in OA, both in the beginning, and during progression of, the disease. Therefore, serum oxLDL levels may be a helpful biomarker to evaluate the severity of knee OA. The information presented here in represents an important contribution to the field.
References
Tiku ML, Shah R, Allison GT (2000) Evidence linking chondrocyte lipid peroxidation to cartilage matrix protein degradation. Possible role in cartilage aging and the pathogenesis of osteoarthritis. J Biol Chem 275(26):20069–20076
Kishimoto H, Akagi M, Zushi S et al (2010) Induction of hypertrophic chondrocyte-like phenotypes by oxidized LDL in cultured bovine articular chondrocytes through increase in oxidative stress. Osteoarthr Cartil 18(10):1284–1290
de Munter W, Blom AB, Helsen MM et a (2013). Cholesterol accumulation caused by low density lipoprotein receptor deficiency or a cholesterol-rich diet results in ectopic bone formation during experimental osteoarthritis. Arthritis Res Ther 15(6):R178. doi: 10.1186/ar4367.
Nishimura S, Akagi M, Yoshida K et al (2004) Oxidized low-density lipoprotein (ox-LDL) binding to lectin-like ox-LDL receptor-1 (LOX-1) in cultured bovine articular chondrocytes increases production of intracellular reactive oxygen species (ROS) resulting in the activation of NF-kappaB. Osteoarthr Cartil 12(7):568–576
Mazière C, Mazière JC (2009) Activation of transcription factors and gene expression by oxidized low-density lipoprotein. Free Radic Biol Med 46(2):127–137
Matsuura E, Hughes GR, Khamashta MA (2008) Oxidation of LDL and its clinical implication. Autoimmun Rev 7(7):558–566
Trpkovic A, Resanovic I, Stanimirovic J et al (2015) Oxidized low-density lipoprotein as a biomarker of cardiovascular diseases. Crit Rev Clin Lab Sci 52(2):70–85
Levitan I, Volkov S, Subbaiah PV (2010) Oxidized LDL: diversity, patterns of recognition, and pathophysiology. Antioxid Redox Signal 13(1):39–75
Gkretsi V, Simopoulou T, Tsezou A (2011) Lipid metabolism and osteoarthritis: lessons from atherosclerosis. Prog Lipid Res 50:133–140
Lepetsos P, Papavassiliou AG (2016) ROS/oxidative stress signaling in osteoarthritis. Biochim Biophys Acta 4:576–591
Ertürk C, Altay MA, Selek S et al (2012) Paraoxonase-1 activity and oxidative status in patients with knee osteoarthritis and their relationship with radiological and clinical parameters. Scand J Clin Lab Invest 72:433–439
Aviram M, Rosenblat M (2004) Paraoxonases 1, 2, and 3,oxidative stress, and macrophage foam cell formation during atherosclerosis development. Free Rad Bio Med 37(9): 1304–1316.
Loued S, Isabelle M, Berrougui H et al (2012) The anti-inflammatory effect of paraoxonase 1 against oxidized lipids depends on its association with high density lipoproteins. Life Sci 90(1–2):82–88
García-Heredia A, Marsillach J, Rull A et al (2013) Paraoxonase-1 inhibits oxidized low-density lipoprotein-induced metabolic alterations and apoptosis in endothelial cells: a nondirected metabolomic study. Mediators Inflamm :156053.
Aviram M, Rosenblat M, Billecke S et al (1999) Human serum paraoxonase (PON 1) is inactivated by oxidized low density lipoprotein and preserved by antioxidants. Free Radic Biol Med 26(7–8):892–904
Aviram M, Kaplan M, Rosenblat M (2005) Dietary antioxidants and paraoxonases against LDL oxidation and atherosclerosis development. Handb Exp Pharmacol 170:263–300
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Ertürk C, Altay MA, Altay N (2016) Will a single periarticular lidocaine-corticosteroid injection improve the clinical efficacy of intraarticular hyaluronic acid treatment of symptomatic knee osteoarthritis? Knee Surg Sports Traumatol Arthrosc 24(11):3653–3660
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–502
Bellamy N, Buchanan WW, Goldsmith CH et al (1957) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Kurban S, Mehmetoglu I (2010) Effects of acetylsalicylic acid on serum paraoxonase activity, ox-LDL, coenzyme Q10 and other oxidative stress markers in healthy volunteers. Clin Biochem 43(3):287–290
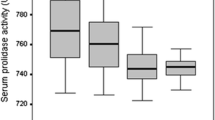
Altay MA, Ertürk C, Bilge A et al (2015) Evaluation of prolidase activity and oxidative status in patients with knee osteoarthritis: relationships with radiographic severity and clinical parameters. Rheumatol Int 35(10):1725–1731
Altay MA, Ertürk C, Levent A (2016) Çetin BV, Aksoy N. Serum prolidase activity and oxidative-antioxidative status in patients with developmental dysplasia of the hip and its relationship with radiographic severity. Redox Rep 20:1–8. doi:10.1080/13510002.2016.1196873
Meisinger C, Baumert J, Khuseyinova N et al (2005) Plasma oxidized low-density lipoprotein, a strong predictor for acute coronary heart disease events in apparently healthy, middle-aged men from the general population. Circulation 112(5):651–657
Roy Chowdhury SK, Sangle GV, Xie X (2010) Effects of extensively oxidized low-density lipoprotein on mitochondrial function and reactive oxygen species in porcine aortic endothelial cells. Am J Physiol Endocrinol Metab 298(1):E89–E98
Mitra S, Goyal T, Mehta JL (2011) Oxidized LDL, LOX-1 and atherosclerosis. Cardiovasc Drugs Ther 25(5):419–429
Hong D, Bai YP, Gao HC et al (2014) Ox-LDL induces endothelial cell apoptosis via the LOX-1-dependent endoplasmic reticulum stress pathway. Atherosclerosis 2:310–317
Villalvilla A, Gómez R, Largo R et al (2013) Lipid transport and metabolism in healthy and osteoarthritic cartilage. Int J Mol Sci 14(10):20793–20808
Berenbaum F (2013) Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr Cartil 21(1):16–21
Mehta JL, Chen J, Hermonat PL et al (2006) Lectin-like, oxidized low-density lipoprotein receptor-1 (LOX-1): a critical player in the development of atherosclerosis and related disorders. Cardiovasc Res 69(1):36–45
Simopoulou T, Malizos KN, Tsezou A (2007) Lectin-like oxidized low density lipoprotein receptor 1 (LOX-1) expression in human articular chondrocytes. Clin Exp Rheumatol 25(4):605–612
Cillero-Pastor B, Eijkel G, Kiss A et al (2012) Time-of-flight secondary ion mass spectrometry-based molecular distribution distinguishing healthy and osteoarthritic human cartilage. Anal Chem 84(21):8909–8916
Kosinska MK, Liebisch G, Lochnit G et al (2013) A lipidomic study of phospholipid classes and species in human synovial fluid. Arthritis Rheum 65(9):2323–2333
Girotti AW (1998) Lipid hydroperoxide generation, turnover, and effector action in biological systems. J Lipid Res 39:1529–1542
de Farias CC, Maes M, Bonifácio KL et al (2016) Highly specific changes in antioxidant levels and lipid peroxidation in Parkinson's disease and its progression: disease and staging biomarkers and new drug targets. Neurosci Lett 617:66–71
Mackness MI, Mackness B, Durrington PN (1996) Paraoxonase: biochemistry, genetics and relationship to plasma lipoproteins. Curr Opin Lipidol 7(2):69–76
Akagi M, Kanata S, Mori S et al (2007) Possible involvement of the oxidized low-density lipoprotein/lectin-like oxidized low-density lipoprotein receptor-1 system in pathogenesis and progression of human osteoarthritis. Osteoarthr Cartil 15(3):281–290
Ishijima M, Watari T, Naito K et al (2011) Relationships between biomarkers of cartilage, bone, synovial metabolism and knee pain provide insights into the origins of pain in early knee osteoarthritis. Arthritis Res Ther 13:R22
Henrotin Y, Lambert C, Couchourel D et al (2011) Nutraceuticals: do they represent a new era in the management of osteoarthritis? - a narrative review from the lessons taken with five products. Osteoarthr Cartil 19(1):1–21
Ertürk C, Altay MA, Sert C et al (2015) The body composition of patients with knee osteoarthritis: relationship with clinical parameters and radiographic severity. Aging Clin Exp Res 27(5):673–679
Kadam UT, Blagojevic M, Belcher J (2013) Statin use and clinical osteoarthritis in the general population: a longitudinal study. J Gen Intern Med 28(7):943–949
Acknowledgements
This project was funded by the Harran University Scientific Research Coordination Committee (2014/2/14075). The authors did not receive any outside funding or grants in support of their research, or during the preparation of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None
Rights and permissions
About this article
Cite this article
Ertürk, C., Altay, M.A., Bilge, A. et al. Is there a relationship between serum ox-LDL, oxidative stress, and PON1 in knee osteoarthritis?. Clin Rheumatol 36, 2775–2780 (2017). https://doi.org/10.1007/s10067-017-3732-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3732-4