Abstract
Patients with osteoporosis have a low bone mass resulting in an increased risk for bone fractures, morbidity and mortality. One hundred thirty-one female pre-menopausal participants (98 Turkish immigrants living in Germany in comparison with 33 age-matched healthy Germans) were recruited for this study which explored vitamin D deficiency and specific genetic modifications of bone metabolism. The subjects were investigated for their femoral and lumbar bone mineral density (BMD) by dual-energy X-ray absorptiometry (DEXA) of the right total femur and the lumbar spine. Serum levels of osteologic parameters were determined: parathormone (PTH), calcium (Ca), osteocalcin (OC), phosphate (P), alkaline phosphatase (AP), beta-crossLaps (CL), tartrate-resistant acid phosphatase isoform 5b (TRAP5b), and 25-vitamin D3 (25-OH D3). The Bsml- and Fokl-polymorphisms of the vitamin D receptor (VDR) gene and the collagen type I alpha 1 (COLIA1)-gene polymorphism were also genotyped. An extremely high prevalence of vitamin D deficiency could be found in the immigrant cohort (87.8 %). Osteoporosis but not osteopenia was more prevalent in this group. Among immigrants with osteoporosis, TRAP5b was elevated in 42.9 % and beta-CL in 28.6 %. Only the Fokl FF-genotype of the VDR polymorphism was significantly more prevalent among the Turkish women, Ff-genotyped immigrants showed significantly decreased BMD. A significant correlation between the COLIA1-gene polymorphism and BMD could not be identified in the two groups. Vitamin D deficiency and osteoporosis appear to be dominant and unrecognized problem among female Turkish immigrants in Germany. Therefore, in this population, osteologic parameters and BMD should be routinely analyzed and deficiencies be treated immediately.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D is a steroid hormone which regulates several endocrine functions, bone metabolism, cell proliferation and differentiation. Its major function is to maintain calcium homeostasis [1]. Many common diseases such as rickets (defect of mineralization affecting the growth skeleton), osteomalacia (abnormal mineralization of the nature skeleton), bone loss (osteopenia/osteoporosis), autoimmune and cardiovascular diseases, diabetes, and cancer have been associated with vitamin D deficiency [2–4]. Less severe 25-OH D3-hypovitaminosis causes an increase of serum parathyreoid hormone (PTH) leading to bone resorption, low BMD, and even fractures [4, 5].
The nuclear functions of vitamin D require binding to the vitamin D receptor (VDR). The gene encoding VDR is located on the chromosome 12q12-13 [6, 7]. There are more than 470 single nucleotide polymorphisms (SNPs) identified in the VDR-gene, and locations of the polymorpisms determine their functional roles [3, 8]. One of the most extensively analyzed VDR polymorphisms are Fokl in exon 2 and Bsml in intron 8 [9–11].
The status of vitamin D shows a high variation within different countries of Europe. Especially in the Middle East and Asia, there is a general problem with hypovitaminosis D during the winter time. Moreover, there is a north-south gradient for 25-OH D3 with higher levels in Scandinavia and lower levels in Italy, Spain, and some eastern European countries. This fact points to other determinants than sunshine, e.g., nutrition, food fortification, and supplement use. Specifically very low levels of 25-OH D3 have been observed in the Middle East, e.g., in Turkey, Lebanon, Jordan, and Iran. Especially the women living in these countries had lower levels due to their clothing habits [12, 13].
Vitamin D deficiency is usually caused by a reduced cutaneous production of vitamin D in institutionalized or housebound elderly people, immigrants to Northern countries and women, who obey strict religious dress codes with banned exposure of uncovered skin [14, 15].
Collagen type I is a common structural component of bone, blood vessels, ligaments, tendons, and skin. It also represents the most abundant extracellular matrix potein in subcutaneous tissue. Polymorphic variants of the COLIA1-gene, which is located on the chromosome 17q21-22 [16], are also considered to be a risk factor for altered bone metabolism and decreased BMD [17, 18].
Osteoporosis is the most common skeletal disease characterized by reduced bone mass and increased risk of fragility fractures [19]. It has a complex etiology and is considered as a multi-factorial and polygenic disorder, in which genetic determinants are modulated by hormonal, environmental, and nutritional factors [20]. Evidence from family and twin studies have shown that genetic factors have a major role in the pathogenesis of osteoporosis [21–23]. Therefore, a series of polymorphisms have been described in several genetic loci. Of these the VDR-gene polymorphisms Fokl and Bsml such as the COLIA-Sp1-binding site polymorphism are one of the most extensively studied candidate genes for osteoporosis [24–26].
A recent study described a high prevalence of vitamin D deficiency, secondary hyperparathyreoidism, and generalized bone pain in gender-mixed Turkish immigrants living in Germany [14].
To elucidate potential causative factors for alteration of bone metabolism, we performed a cross-sectional study that investigated female Turkish immigrants living in Germany compared to a group of healthy age-matched female Germans.
To our knowledge, this is the first study investigating the prevalence of vitamin D deficiency, loss of BMD, markers of bone metabolism and polymorphisms of the VDR-gene, and the COLIA1-gene in Middle East female immigrants to a central European country.
Materials and methods
Study population
The study population comprised 98 female Turkish immigrants living in Germany for more than 5 years and 33 age-matched female Germans. All women were premenopausal with physiological hormone status. Criteria for exclusion were diseases with an influence on bone metabolism like inflammatory bowel disease, malabsorption, liver disease, hypophosphataemia, tubular dysfunction, and anticonvulsive therapy. None of the patients had a history for cardiovascular incidents or tumors. The study period was limited to March to April 2008 to minimize short-term effects of nutrition and sunlight exposure could be minimized.
Laboratory parameters
After overnight fasting, blood samples were collected by phlebotomy for plasma separation in EDTA-containing tubes. The samples were centrifugated at once (less than 30 min after phlebotomy). Serum tubes were centrifugated after clotting and total serum calcium (sCa2+, referance range 2.15–2.55 mmol/l), phosphate concentration (P, reference range 0.87–1.45 mmol/l), alkaline phosphatase (AP, reference range 35–129 U/l), 25-OH-vitamin D3 (25-OH D3, reference range 30–60 ng/ml; Incstar Corporation, Stillwater, MN, USA), parathyroid hormone (PTH, reference range 8.3–68 pg/ml; PTH intact ELISA, DRG Instruments GmbH, Marburg, Germany), osteocalcin (OC, reference range females 6.5–42.3 ng/ml; LIAISON Osteocalcin, DiaSorin Ins, Stillwater, MN, USA), beta-crosslaps (CL, reference range premenopausal female <0.573 ng/ml, b-crosslaps/serum, Roche Diagnostics, Indianapolis, IN, USA), and tartrate-resistant acid phosphatase isoform 5b (TRAP5b, reference range females 2.9 ± 1.4 U/l; Metra TRAP5b EIA Kit, Quidel Corporation, San Diego, CA, USA) were analyzed in serum samples.
Genotyping
The genomic DNA was isolated from peripheral venous blood using QiaAmp-Blood-Kit (Qiagen, Hilden, Germany).
Single nucleotide polymorphism (SNP) genotyping was performed by using a microplate fluorometer (Fluoroskan Ascent, Thermo Fisher Scientific, Waltham, MA, USA).
Genotyping of the VDR-gene polymorphisms Fokl and Bsml was performed as outlined before [9, 11, 17]. Alleles were genotyped for the presence (f, b) or the absence (F, B) of the Fokl- or Bsml-restriction sites.
The guanine (G) to thymidine (T) polymorphism in the Sp1-binding site in the first intron of the COLIA1-gene was determined by a PCR-based method as described previously [17, 27]. The alleles were denominated as G or T, according to the absence or the presence of the restriction site.
Osteodensitometry
Bone mineral density (BMD; g/cm2) at the total right femur and the lumbar spine (first to fourth vertebrae, antero-posterior view) was measured by the most widely technique, the dual-energy X-ray absoptiometry (DXA; ProdigyLunar. Milwaukee, WI, USA). DXA is a non-invasive, painless method and involves low radiation exposure. It is commonly used to screen people for osteoporosis risk. The coefficient of variation of repeated measurements in vivo was 0.9 % for the lumbar spine and 1.6 % for the femur T-score (number of standard deviations (SD) from the normal mean obtained from young healthy adults) and Z-score (number of SD above or below the mean of age- and sex-matched controls) were also calculated. A poor BMD was defined according to the criteria of the World Health Organization (WHO) guidelines: Osteopenia is explained as a T-score between −1 and −2.5 SD and osteoporosis as a T-score −2.5 SD or lower. The respective reference values have been published previously for women and men. For the purpose of this study, the reference values of the producer were used.
Statistical analysis
All data were statistically evaluated using SPSS Release 12.0.1 (SPSS Inc., Chicago, IL, USA) and are presented as mean ± SD. Data were tested for normality by the Kolmogorov-Smirnov test. For comparison of the groups, numeric values were analyzed by Student’s t test. Data that demonstrated unequal statistical spread or variant distribution were analyzed by the Mann-Whitney rank sum test. Proportions of the group were matched by chi-square analysis and Fisher’s exact test. A p value of <0.05 was regarded as significant for all analyses.
Results
Vitamin D metabolism and other laboratory parameters
Basic demographic and osteologic data of the participant groups are demonstrated in Table 1. Both groups, Turkish and German women, did not show a difference in age, lumbar and femoral BMD (including T- and Z-scores). There was also no serious difference in serum levels of PTH and AP between the two groups.
The Turkish immigrants showed significantly higher values of their body mass index (BMI). In contrast, their serum levels of 25-OH D3, P, sCa2+, CL, OC, and TRAP5b were significantly reduced.
The strong differences in the vitamin D levels have to be underlined: the majority of Turkish participants showed reduced vitamin D levels. A severe vitamin D deficiency (25-OH D3 < 10 ng/ml) was observed in 87.8 vs. 45.4 % of the Germans, a moderate vitamin D deficiency (25-OH D3 10–19.9 ng/ml) in 5.1 vs. 18.2 % of the Germans and a mild vitamin D deficiency (25-OH D3 20–29.9 ng/ml) in 5.1 vs. 9.1 % of the Germans. Sufficient levels of vitamin D (25-OH D3 ≥ 30 ng/ml) were only demonstrated in 2 % of the Turkish immigrants vs. 27.3 % of the Germans.
Moreover, Turkish immigrants had elevated levels of PTH in 81.6 %, of TRAP5b in 18.4 % and of CL in 7.1 % (Table 2).
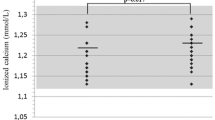
Although there was a significant vitamin D deficiency in the Turkish group, the typical laboratory constellation of secondary hyperparathyreoidism (increased PTH, decreased sCa2+) was only seen in 10 cases. This prevalence of secondary hyperparathyreodism (10.2 %) did not show a significant difference to the German group (9.1 %, Fisher’s exact test, p = 1.000) (Table 3).
BMD, bone metabolism parameters, and genetic pattern
Turkish female immigrants showed in 36.7 % an alteration of BMD. Osteoporosis was observed in seven cases (7.1 %) and osteopenia in 29 cases (29.6 %) [Table 4], whereas German participants showed no osteoporosis, osteopenia was observed only in 10 cases (30.3 %) [Table 5]. The incidence of severe vitamin D deficiency (25-OH D3 < 10 mg/ml) was approximately similar (more than 75 %) in the two groups with osteoporosis and osteopenia, respectively [Table 4], whereas the Germans with osteopenia showed severe vitamin D deficiency in only four cases (40 %).
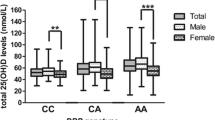
Turkish female immigrants showed a significant predominance of the Fokl-genotype FF (p = 0.048) [Table 6], whereas there were no significant differences in the distribution of the Bsml-polymorphism of the VDR-gene and the COLIA1-polymorphism between the Turkish and German participants. Furthermore, Turkish immigrants with Ff-genotype showed significantly decreased BMD and T-scores of the lumbar spine (Mann-Whitney U test, p < 0.046) and the right femur compared with FF-genotyped females [Table 7]. Due to the small group size of the ff-genotyped females, the value of a statistical analysis is limited. However, since the mean BMD and T-score values in the ff-group were higher than those in the FF- group, significance can be inferred. The Turkish participants demonstrated significant predominance of the Fokl-genotype FF (54.1 %, p = 0.048). Besides, there were no significant variances in the distribution of the Bsml-polymorphisms of the VDR-gene and the COLIA1-gene polymorphism between the two groups.
Moreover, COLIA1-gene polymorphisms did not show a significant correlation between BMD-values, T- and Z-scores of the lumbar spine and the right femur.
Discussion
Vitamin D and its metabolites have a dominant role in bone mineral homoeostasis by regulating calcium absorption, bone resorption, the differentiation of bone cells, and the secretion of parathyreoid hormones. Serum 25-hydroxyvitamin D3 [25(OH)D3] is the metabolite that needs to be measured to identify vitamin D status. Its major function is to avert rickets and osteomalacia which are both bone diseases characterized by inadequate bone formation and mineralization. The main clinical features in osteomalacia are bone pain, muscle weakness, and fractures. Accordingly, the most frequently cause of rickets and osteomalacia is an insufficient vitamin D status which is a very frequent problem in the Middle East such as Turkey, Lebanon, Jordan, and Iran [12, 13].
The first report of the histological incidence of adult osteomalacia took place in 1885, its clinical appreciation was described much later. In the 1930s, Maxwell evaluated that there should have been about 100,000 cases of adult osteomalacia in Chinese people at that time [28]. Some time later, a further study characterized the presence of osteomalacia in the USA caused by lack of vitamin D supplementation [29]. Immigrants from Asian countries also have an increased risk for severe vitamin D deficiency [5, 30, 31]. The first time in which osteomalacia was investigated in Turkish immigrants living in Germany was published in 1978 [32]. Chapuy et al. were the first to propose that a 25(OH)D3 value of less than 80 nmol/l is associated with higher PTH levels [33].
In a prior study, which is to our knowledge the first one analyzing the prevalence of vitamin D deficiency, secondary hyperparathyreoidism, and loss of bone mineral density in gender-mixed Turkish immigrants living in Germany, we detected a high prevalence of low vitamin D levels, secondary hyperparathyreoidism, and generalized bone pain, especially in veiled women. Based on these results, we concluded that this finding could be based on an independent ethnic risk factor for vitamin D deficiency in Turks compared to Germans. Furthermore, darker skin pigmentation and cultural differences in clothing habits in Turks, which result in a reduced ability to produce vitamin D in their skin during sunlight exposure, were identified as risk factors [14]. However, there are more factors influencing the vitamin D metabolism such as age, seasonal exposure to sunlight (lower levels between October and April) [34], and also genetic alterations. Additionally, an insufficient low vitamin D diet in the target population can further enhance the vitamin D hypovitaminosis.
In our study, we also found significantly decreased values of 25(OH)D3 in a large proportion of the Turkish women (98.0 %, severe vitamin D deficiency in 87.8 %), although it needs to be considered that the observation period was at the end of the winter time (March/April) with low sunlight exposure. In contrast, 27.3 % of the German controls showed sufficient vitamin D values, therefore 72.7 % of them had abnormal 25(OH)D3 levels (45.4 % severe vitamin D deficiency). It has to be underlined that none of the study participants had malabsorption, liver disease, renal tubular dysfunction, hypophosphatemia, or received anticonvulsant therapy which could have induced a vitamin D deficiency.
In vitamin D insufficiency, secondary hyperparathyreoidism is frequently present. Even less severe 25(OH)D3-deficiency can cause an increase of serum PTH leading to bone resorption, osteoporosis, and fractures. Accordingly, in the present study, we detected elevated PTH levels in 81.6 % of the Turkish women and 81.8 % of the Germans. The typical laboratory constellation of a manifest secondary hyperparathyreodism (elevated PTH, decreased calcium levels) was only seen in a small proportion of the participants in either groups (10.2 % of the Turkish immigrants, 9.1 % of the German controls).
Bone remodeling is characterized by two opposite mechanisms: the formation of new bone by osteoblasts and the resorption of aged bone by osteoclasts. Therefore, active bone metabolism can be described by measuring the enzymatic activity of osteoblasts and osteoclasts (AP, TRAP5b, CL, OC).
TRAP5b is released into serum by bone-resorbing osteoclasts and is a marker of osteoclast activity. In the group of the Turkish immigrants, we found increased TRAP5b levels in 18.4 % (20.7 % of the cases with osteopenia and 42.9 % of the cases with osteoporosis). The Crosslaps as biochemical indicators of bone resorption were also elevated in Turkish immigrants (10.3 % of the cases with osteopenia and 28.6 % of the cases with osteoporosis). Interestingly, despite the present strong vitamin D deficiency an AP increase could not be found. This finding excluded an additional osteomalacia component. Thus, it can be hypothesized that the vitamin D deficiency exists only a few months without an impact on bone metabolisms. Owing the fact that the included immigrants already lived in Germany for several years the vitamin D deficiency is not the result of a short stay in our region. Thus, it can be assumed that the decreased bone mineral density is more likely to be caused by a genetic component.
Moreover, we could not identify any differences in the genetic distribution of the Bsml-polymorphism of the VDR-gene and the COLIA1-Sp1-binding site polymorphism of the COLIA1-gene, neither in the group of the Turkish immigrants nor in the group of the German controls. In contrast, female Turkish immigrants showed a significant disposition in Fokl-polymorphism: the Ff-genotyped women had a significantly decreased BMD of the right femur and lumbar spine.
In conclusion, vitamin D deficiency and reduction of bone mineral density were found to be highly common among female Turkish immigrants. Thus, in this population an osteologic screening should be done on a routine basis.
In addition, it is important to inform this population about the consequences of decreased vitamin D values like the negative effect on bone status and even cancer or cardiovascular diseases. Female Turkish immigrants living in Germany should therefore be sensitized to the necessity of sufficient vitamin D levels facilitated well-balanced nutrition, frequent sunlight exposure, and even vitamin D supplementation.
Taken together, migration to “low osteoporosis countries” does not reduce the incidence of and risk for severe osteoporosis. The current study shows that genetic factors such as Fokl-polymorphisms at the VDR-gene seem to be of clinical impact, specifically in female Turkish immigrants living in Germany who are at risk for decreased bone mineral density (osteopenia/osteoporosis).
References
Haussler MR, Whitfield GK, Haussler CA, Hsieh JC, Thompson PD, Selznick SH, Dominguez CE, Jurutka PW (1998) The nuclear vitamin D receptor: biological and molecular regulatory properties revealed. J Bone Miner Res 13:325–349
Uitterlinden AG, Fang Y, Van Meurs JB, Pols HA, van Leeuwen JP (2004) Genetics and biology of vitamin D receptor polymorphisms. Gene 338:143–156
Slattery ML (2007) Vitamin D receptor gene (VDR) associations with cancer. Nutrition Rev 65:S102–104
Holick MF (2004) Vitamin D: importance in the prevalence of cancer, type 1 diabetes, heart disease and osteoporosis. Am J Clin Nutr 79:363–371
Meyer HE, Falch JA, Sogaard AJ, Haug E (2004) Vitamin D deficiency and secondary hyperthyreoidism and the association with bone mineral density in persons with Pakistani and Norwegian background living in Oslo, Norway. The Oslo Health Study. Bone 35:412–417
Norman AW (2008) From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. Am J Clin Nutr 88:491–499
Labuda M, Fujiwara TM, Ross MV, Morgan K, Garcia-Heras J, Ledbetter DH, Hughes MR, Glorieux FH (1992) Two hereditary defects related to vitamin D metabolism map to the same region of chromosome 12q13-14. J Bone Miner Res 7:1447–1453
Davis CD (2008) Vitamin D and cancer: current dilemmas and future research needs. Am J Clin Nutr 88:565–569
Morrison NA, Qi JC, Tokita A, Kelly PJ, Crofts L, Nguyen TV, Sambrook PN, Eisman JA (1994) Prediction of bone density from vitamin D receptor alleles. Nature 367:284–287
Hustmeyer FG, Peacock M, Hui S, Johnston SS, Christian J (1994) Bone mineral density in relation to polymorphism at the vitamin D receptor gene locus. J Clin Invest 94:2130–2134
Gross C, Eccleshall TR, Mallory PJ, Villa ML, Marcus R, Feldmann D (1996) The presence of a polymorphism at the translation initiation site of the vitamin D receptor gene is associated with low bone mineral density in postmenopausal Mexican-American women. J Bone Miner Res 11:1850–1855
Bartley J (2008) Prevalence of vitamin D deficiency among patients attending a multidisciplinary tertiary pain clinic. N Z Med J 121:57–62
Lips P (2007) Vitamin D status and nutrition in Europe and Asia. J Steroid Biochem Mol Biol 103:620–625
Erkal MZ, Wilde J, Bilgin Y, Akinci A, Demir E, Bödecker RH, Mann M, Bretzel RG, Stracke H, Holick MF (2006) High prevalence of vitamin D deficiency, secondary hyperparathyreoidism and generalized bone pain in Turkish immigrants in Germany: identification of risk factors. Osteoporos Int 17:1113–1140
Francis RM, Selby PL (1997) Osteomalacia. Baillieres Clin Endocrinol Metab 11:145–163
Solomon E, Hiorns L, Sheer D, Rowe D (1984) Confirmation that the type I collagen gene on chromosome 17 is COL1A1 (alpha 1(I), using a human genomic probe. Ann Hum Genet 48:39–42
Grant SFA, Reid DM, Blake G, Herd R, Fogelman I, Ralston SH (1996) Reduced bone density and osteoporosis associated with a polymorphic Sp1 binding site in the collagen type a1 gene. Nat Genet 14:203–205
Langdahl BL, Ralston SH, Grant SFA, Eriksen EF (1998) An Sp1 binding site polymorphism in the COLIA1 gene predicts osteoporotic fractures in both men and women. J Bone Miner Res 13:1384–1389
Siris ES, Selby PL, Saag KG, Borgström F, Herings RM, Silverman SL (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122:3–13
Gronholz MJ (2008) Prevention, diagnosis and management of osteoporosis-related fracture: a multifactorial osteopathic approach. J Am Osteopath Assoc 108:575–585
Seemann E, Hopper JL, Bach LA (1989) Reduced bone mass in daughters of women with osteoporosis. N Engl J Med 320:554–558
Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PN, Eberl S (1987) Genetic determinants of bone mass in adults. A twin study. J Clin Invest 80:706–710
Evans RA, Marel GM, Lancaster EK, Kos S, Evany N, Won SYP (1988) Bone mass in relatives of osteoporotic patients. Ann Intern Med 109:870–873
Ralston SH, Uitterlinden AG, Brandi ML, Balcells S, Langdahl BL, Lips P, Lorenc R, Obermayer-Pietsch B, Scollen S, Bustamante M, Husted LB, Carey AH, Diez-Perez A, Dunning AM, Falchetti A, Karczmarewicz E, Kruk M, van Leeuwen JP, van Meurs JB, Mangion J, McGuigan FE, Mellibovsky L, del Monte F, Pols HA, Reeve J, Reid DM, Renner W, Rivadeneira F, van Schoor NM, Sherlock RE, Ioannidis JP (2006) GENOMOS Investigators. Large-scale evidence for the effect of the COLIA1 Sp1 polymorphism on osteoporosis outcomes: the GENOMOS study. PLoS Med 3(4):e90
Rizzoli R, Bonjour JP, Ferrari SL (2001) Osteoporosis, genetics and hormones. J Mol Endocrinol 26:79–94
Obermayer-Pietsch BM, Lange U, Tauber G, Frühauf G, Fahrleitner A, Dobnig H, Hermann J, Aglas F, Teichmann J, Neeck G, Leb G (2003) Vitamin D receptor initiation codon polymorphism, bone density and inflammatory activity of patients with ankylosing spondylitis. Osteoporos Int 14:995–1000
Uitterlinden AG, Burger H, Huang Q, Yue F, MC Guigan FE, Grant SF, Hofmann A, van Leeuwen JP, Pols HA, Ralston SH (1998) Relation of alleles of the collagen type I alpha 1 gene to bone density and the risk of osteoporotic fractures in postmenopausal women. N Engl J Med 338:1016–1021
Maxwell JP, Pi HT, Lin HAC, Kuo CC (1939) Further studies in adult rickets (osteomalacia) and foetal rickets. Proc R Soc Med 32:287–297
Albright F, Reifenstein F (1948) The parathyreoid glands and metabolic bone disease: selected studies. The Williams and Wilkins Company, Baltimore
Preece MA, Mcintosh WB, Tomlinson S, Ford JA, Dunnigan MG, O’Riordan JLH (1973) Vitamin D deficiency among Asian immigrants to Britain. Lancet 301:907–910
Holvik K, Meyer HE, Haug E, Brunvand L (2005) Prevalence and predictors of vitamin D deficiency in five immigrant groups living in Oslo, Norway: the Oslo Immigrant Health study. Eur J Clin Nutr 59:57–63
Offermann G, Manhold C (1978) Osteomalacia in Turkish guest-workers in Germany. Inn Med 5:103–111
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ (1992) Vitamin D3 and calcium to prevent hip fractures in olderly women. N Engl J Med 327:1637–1642
Wemeau JL (1995) Calcitriopic hormones and ageing. Horm Res 43:76–79
Acknowledgments
This work did not get any financial support.
We acknowledge the statistical support of MoReData GmbH, Kerkrader Strasse 11, 35394 Giessen, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All voluntary study subjects gave written informed consent prior to the study which was approved by the local Ethics Committee of the Faculty of Medicine, Justus-Liebig-University Giessen, Germany.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Tastan, Y., Kann, P.H., Tinneberg, HR. et al. Low bone mineral density and vitamin d deficiency correlated with genetics and other bone markers in female Turkish immigrants in Germany. Clin Rheumatol 35, 2789–2795 (2016). https://doi.org/10.1007/s10067-016-3237-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3237-6