Abstract
Sleep-disordered breathing (SDB) is associated with an increased risk of adverse events in patients with heart failure (HF); however, its impact in patients implanted with a left ventricular assist device (LVAD) remains unclear. We aimed to investigate the prevalence of SDB in patients with LVAD and its impact on their clinical outcomes. Fifty consecutive patients with LVAD who underwent portable sleep monitoring between September 2017 and April 2018 were prospectively enrolled, and they were followed up for 170 ± 36 days. According to their respiratory disturbance indexes (RDIs), they were categorized into the SDB group (RDI ≥ 15, n = 12) and the non-SDB group (RDI < 15, n = 38). The incidence of adverse events during the follow-up period was investigated after enrollment. Multivariate logistic regression analysis revealed significant differences in SDB in LVAD-implanted patients in terms of the logarithmic transformation brain natriuretic peptide (BNP) values (p = 0.005). The optimal BNP cut-off value for SDB prediction in LVAD-implanted patients was 300 pg/mL (sensitivity: 58.3%, specificity: 94.7%). During follow-up, ventricular tachyarrhythmias (VTas) occurred significantly more frequently in the SDB group (4 [33%] vs. 2 [5%] patients, p = 0.02); Atrial tachyarrhythmia (ATa) also tended to occur more frequently in the SDB group (2 [25%] vs. 2 [2%] patients, p = 0.07). SBD was prevalent in 24% of the LVAD-implanted patients with advanced HF. Furthermore, SDB was significantly associated with high BNP levels and was also potentially associated with subsequent incidence of VTa in patients with LVAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sleep-disordered breathing (SDB) is one of the most common comorbidities in patients with heart failure (HF), with a reported prevalence of 40–76%. Further, it is known that the prevalence of SDB increases with increasing severity of HF [1]. Physiologically, SDB increases sympathetic nerve activity and intrathoracic pressure, both of which can negatively affect the cardiovascular performance. Moreover, complications of SDB include systemic inflammation and an increase in the release of vasoactive mediators, such as endothelin and angiotensin II, resulting in endothelial dysfunction [2, 3]. Thus, SDB complications accelerate the exacerbation of HF and increase the morbidity and mortality rates in patients with HF [4]. However, the prevalence of SDB decreases with standard pharmacological and non-pharmacological therapies for HF, including diuretics, angiotensin-converting-enzyme inhibitors, beta-blockers, and cardiac resynchronization therapy [5,6,7]. Therefore, SDB is strongly associated with the pathophysiology of HF, and both SDB and HF interact with each other from various perspectives.
Continuous-flow left ventricular assist device (LVAD) has become a mainstay of treatment for patients with advanced HF. LVAD draws blood from the diseased left ventricle (LV) and pumps it into the aorta, restoring circulation and markedly improving both the prognosis and quality of life of patients with HF. However, the prevalence and clinical impact of SDB in patients with LVAD remain unclear. Therefore, the present study aimed to investigate the prevalence of SDB in patients with LVAD and its impact on clinical outcomes.
Methods
Study design and patient selection
This single-center, prospective, cross-sectional, observational study was approved by the Institutional Review Committee (IRB) of the National Cerebral and Cardiovascular Center (IRB number: M30-020) and was conducted according to the tenets of the 1975 Helsinki Declaration and its later amendments. Written informed consent was obtained from all patients.
The subjects were consecutive patients with advanced HF supported with HeartMate II (HMII; Abbott, Lake Bluff, IL, USA) and who underwent portable sleep monitoring (PSM) between September 2017 and April 2018. Stable and ambulatory patients with HMII, who were hospitalized for scheduled annual medical check-ups, including echocardiogram and hemodynamics, were indicated for PSM. Patients who had clinical signs for worsening HF on LVAD support, such as deterioration of dyspnea, edema, and end-organ function, were not enrolled for this study. PSM was performed at various time points during the chronic phase when the patients were hospitalized for scheduled medical check-ups.
Sleep study
SDB was examined using the PSM device Apnomonitor Type 4 (Fukuda Denshi Pulsleep LS 120, Tokyo, Japan). Variables included the nasal flow and percutaneous oxygen saturation. Apnea was defined as > 10 s of complete shutdown of the airflow with a 3% decrease in the oxygen saturation. Hypopnea was defined as a decrease of at least 50% in the nasal flow for > 10 s with a 3% decrease in the oxygen saturation. Respiratory disturbance index (RDI) was defined as the average number of apnea or hypopnea episodes per hour during the examination.
The patients were divided into two groups according to the RDI value as the SDB group (RDI ≥ 15) and the non-SDB group (RDI < 15) [8].
Variables evaluated
Demographic data were collected from the medical records. Results of the preoperative SDB examination were also collected if available. Previous large trials have indicated that the equivalent dose of bisoprolol is one-fifth of that of carvedilol [9]. Laboratory tests were performed at the time of study enrollment.
Echocardiography and right heart catheterization (RHC) were performed to assess the hemodynamics at the time of enrollment. Echocardiography was performed by ultrasound imaging technologists and reviewed by attending cardiologists blinded to this study. Left ventricular end-diastolic diameter, left ventricular end-systolic diameter, left ventricular ejection fraction, and left atrial diameter were measured using standard methods [10]. The jugular vein approach was used for RHC. Hemodynamic measurements included pulmonary capillary wedge pressure (PCWP), pulmonary artery pressure (PAP), and right atrial pressure. The cardiac output (CO) and cardiac index were calculated using the Fick method. Pulmonary vascular resistance (PVR) was calculated as follows: PVR (Wood units) = (mean PAP − PCWP)/CO [11].
Clinical outcomes
Patients were prospectively followed for 180 days from the day of PSM. Follow-up was censored at death or heart transplantation. Adverse events were defined based on the definitions stipulated by the interagency registry for mechanically assisted circulatory support [12].
Briefly, atrial tachyarrhythmias (ATas), including atrial tachycardia, atrial fibrillation (AF), and atrial flutter, were defined as events that required hospitalization for treatment with pharmacotherapy, defibrillation, or arrhythmia ablation procedure.
Ventricular tachyarrhythmias (VTas), including sustained ventricular tachycardia (VT) and ventricular fibrillation, were defined as events that required hospitalization for treatment with pharmacotherapy, defibrillation, or arrhythmia ablation procedure.
Cerebrovascular accident (CVA) was defined as any new neurological event, including a transient ischemic attack or any transient and persistent, local and systemic ischemic, or hemorrhagic cardiovascular and cerebrovascular events. Standard neurological function assessments were performed either by certified neurologists or internal medicine physicians using appropriate diagnostic tests and confirmed using the patient records.
Hemolysis was defined as a serum lactate dehydrogenase level higher than two and one-half times the upper limits of the normal range at our center (572.5 IU/L), with any condition, including anemia, hyperbilirubinemia (total bilirubinemia above 2 mg/dL, with predominately indirect component), hemoglobinuria, pump malfunction, or abnormal pump parameters, 72 h after LVAD implantation.
Bleeding was defined as events, such as hemorrhagic death or requiring re-operation, hospitalization, or red blood cell transfusion, 7 days after LVAD implantation.
Driveline infection was defined as a percutaneous site or pocket infection with a positive pathogen culture, requiring antibiotic treatments, including clinical evidence of infection, such as pain, fever, drainage, or leukocytosis.
Statistical analysis
Continuous variables were expressed as means ± standard deviation or as medians (interquartile range), as appropriate. Categorical variables were expressed as counts and frequencies. Between-group comparisons were performed using an unpaired t test for normally distributed data or the Mann–Whitney U test for non-normally distributed data. The Chi-square test and the Fisher exact test were performed for categorical variables.
Univariate and multivariable logistic regression models were used to identify independent predictors of the presence of SDB. Significant variables in the univariate analysis (i.e., those with a p < 0.05) were included in the multivariable analysis; because brain natriuretic peptide (BNP) concentrations were markedly skewed, we assessed the logarithmic transformation (log10) of BNP concentration. Receiver operating characteristic (ROC) curves and areas under the curve (AUC) were used to determine the cut-off values of the potential predictive factors for the presence of SDB in patients with LVAD. The sensitivity, specificity, positive predictive value, and negative predictive values were also calculated.
Kaplan–Meier analysis and the log-rank test were performed to evaluate the event-free survival. All p-values were two-sided, and p < 0.05 was considered statistically significant. All statistical analyses were performed using the JMP 14 Statistics Software Package (SAS Institute Inc., Cary, North Carolina, NC, USA).
Results
Baseline characteristics
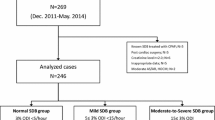
Of the 87 patients who underwent HMII implantation during the study period, 50 patients who underwent PSM were included in this study. During the follow-up period, 2 patients underwent heart transplantation, and 1 patient was transferred to another hospital; thus, the mean follow-up period was 170 ± 36 days.
Of the 50 HMII patients who underwent PSM, 12 patients (24%) experienced SDB. No significant between-group differences were noted with respect to the period from LVAD implantation to study enrollment (355 [155–555] vs. 428 [280–577] days, p = 0.60). Table 1 shows the patients’ baseline demographic data according to the SDB groups. The SDB group was older than the non-SDB group (mean age: 53 ± 4 years vs. 42 ± 2 years, p = 0.02), and they had a higher incidence of dyslipidemia before LVAD implantation.
Table 2 shows the patients’ baseline clinical data according to the SDB groups. The values of BNP (324 [132–627] vs. 88 [51–185] pg/mL, p = 0.009) and creatinine (Cr) (1.0 [0.7–1.4] vs. 0.8 [0.7–0.9] mg/dL, p < 0.05) were significantly higher in the SDB group. Echocardiographic and hemodynamic parameters were comparable between the groups. Fourteen patients underwent SDB examination preoperatively; changes in RDI values before and after LVAD implantation and occurrence of adverse events during the follow-up period in this cohort of 14 patients are shown in supplementary Table 1.
Predictors of SDB
Univariate and multivariable logistic regression analyses were conducted to identify factors associated with the presence of SDB (Table 3). The results showed that log10 BNP (odds ratio 0.24, 95% confidence interval [CI] 0.07–0.8, p = 0.005) was associated with the presence of SDB. ROC curve analysis revealed 300 pg/mL as the optimal cut-off value of BNP for predicting SDB following LVAD implantation, with a sensitivity of 58.3% and a specificity of 94.7%. The AUC was 0.82 (Fig. 1).
Receiver operating characteristic curve plot shows that the optimal brain natriuretic peptide (BNP) cut-off value for predicting sleep-disorder breathing (SDB) in patients with left ventricular assist device (LVAD) is 300 pg/mL (sensitivity: 58.3% and specificity: 94.7%). The area under the curve is 0.82
Clinical outcomes
During the follow-up period, VTa occurred more frequently in the SDB group than that in the non-SDB group (4 [33%] vs. 2 [5%] patients, p = 0.02, Table 4). No VTas were noted probably due to the malposition of the outflow cannula and left ventricular suction. Furthermore, ATa tended to occur more frequently in the SDB group (2 [25%] vs. 2 [2%] patients, p = 0.07), although the difference was not statistically significant (Table 4).
No significant between-group differences were noted with respect to the rates of CVA, hemolysis, bleeding, driveline infection, and death. Kaplan–Meier analysis demonstrated that the overall survival was comparable between the groups (100% vs. 97.1% at 180 days, p = 0.56), whereas the VTa-free survival was significantly lower in the SDB group (66.7% vs 94.4% at 180 days, p = 0.009) (Fig. 2).
Discussion
Primarily, we found that 24% of the patients with LVAD experienced SDB and that a high BNP level was an independent predictor of SDB in patients with LVAD. Further, SDB in patients with LVAD was potentially associated with a higher incidence of subsequent VTa.
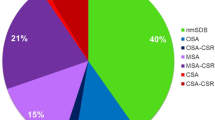
It has been previously reported that obstructive sleep apnea (OSA) and central sleep apnea (CSA) in patients with HF improved after LVAD implantation [13, 14]. However, in other reports, Cheyne–Stokes respiration (CSR) persisted even after LVAD implantation despite hemodynamic compensation by the LVAD [15]. Furthermore, in other cases, persistent CSA after LVAD implantation led to underfilling of the LV and susceptibility to PI events owing to the rise in pulmonary vascular resistance followed by impaired pulmonary venous return [16]. Despite these reports, evidence regarding the impact of SDB after LVAD implantation, including its prevalence, remains conflicting.
Although SDB was not assessed in all study subjects prior to LVAD implantation, the present study is the first to demonstrate the prevalence of SDB in a large number of patients with LVAD. Among the 50 patients analyzed, 12 patients (24%) with advanced HF still experienced SDB, defined as an RDI ≥ 15, following LVAD implantation. Because the preoperative prevalence of SDB was only available in 14 patients, our study did not correctly assess the prevalence of SDB before LVAD implantation, and the number of patients whose SDB improved postoperatively remains unclear. However, 24% of patients with LVAD developed SDB despite stable conditions with compensated hemodynamics after LVAD implantation, and our limited data regarding changes in RDI values before and after LVAD implantation from 14 study subjects imply that LVAD implantation may change the status of SDB in some patients.
Although the risk factors for SDB in patients with LVAD have not been clearly elucidated to date, some studies have investigated the clinical risk factors associated with SDB in patients with HF. Sin et al. reported that male sex, atrial fibrillation, age > 60 years, and hypocapnia were the risk factors for CSA. Body mass index was significantly associated with OSA in male patients, while age > 60 years was the only risk factor for OSA in female patients [17]. Another study investigating the risk factors for CSR in patients with HF reported that high BNP values and low partial pressure of carbon dioxide were independently associated with the presence of CSR in patients with HF [18]. Similar to this previous report, despite comparable hemodynamic parameters in both groups, the current study demonstrated that BNP was independently associated with the presence of SDB (RDI ≥ 15) in patients with LVAD, and BNP ≥ 300 pg/mL was determined as the optimal cut-off value to predict the presence of SDB in our cohort. The pathophysiological association between BNP and the presence of SDB were not well elucidated in our study. However, the high BNP values at the chronic stage after LVAD implantation might indicate the potential severity of the disease regardless of hemodynamics. We have previously reported that BNP values 60 days after implantation may act as a predictor of prognosis in patients with LVAD [19]. In this previous report, BNP ≥ 322 pg/mL was determined as the optimal cut-off value to predict prognosis, close to the current calculated BNP cut-off value for predicting SDB in patients with LVAD.
Several clinical factors have been found to be risk factors for VTa in various clinical settings. Among them, SDB has been reported to be one of the risk factors for VTa in patients with HF [20]. Serizawa et al. reported that the presence of SDB was an independent predictor for appropriate implantable cardioverter defibrillator (ICD) therapy in HF patients with reduced ejection fraction [21]. In this study, ICD therapy more frequently occurred from midnight to 6 PM, which might be a hotspot of SDB. Another study by Ryan et al. demonstrated that ventricular premature beats significantly reduced with continuous positive airway pressure therapy in HF patients with OSA [22]. These reports strongly suggest the close correlation between SDB and arrhythmic events in patients with HF. Physiologically, SDB accelerates myocardial ischemia, cardiac remodeling through hypoxemia, and sympathetic hyperactivity, which may also cause an increase in automaticity, upregulation of action potential activities, and formation of reentrant circuits in the failing myocardium [23]. Furthermore, OSA-induced negative intrathoracic pressure followed by myocardial dilation or stretch reportedly results in electrophysiological changes, such as stretch on action potential or early and delayed after-depolarization, which may facilitate ventricular arrhythmias [24, 25].
Several studies have investigated the risk factors for arrhythmic events in patients with LVAD. History of AF or VTa before LVAD implantation, presence of ischemic heart disease, and interruption of β-blockers have been reported to be the risk factors for VTa in patients with LVAD [26,27,28]. Malposition of the intraventricular inflow cannula could also represent a potential risk for VTa in patients with LVAD [29].
In the current study, no VTa caused by malposition of the inflow cannula and LV suction was noted, and all but 2 patients received β-blocker treatments. Furthermore, 90% of our study subjects were preoperatively diagnosed with non-ischemic cardiomyopathy. Under these conditions, the findings of this study indicate that the presence of SDB might be associated with subsequent VTa, and SDB might be a novel therapeutic target for post-LVAD VTa in patients with LVAD.
Limitations
This study had some limitations. First, since our study did not assess SDB before LVAD implantation in our study subjects, how the prevalence of SDB changed after LVAD implantation, which is another clinical issue regarding SDB and LVAD therapy, remains unclear. However, since there have been no previous studies regarding SDB and LVAD therapy, our study has enough clinical impact on encouraging a clinical study of this field, and how the prevalence of SDB changed after LVAD implantation should be our future study. Second, this was a single-center, cross-sectional study with a small sample size. Therefore, only a small number of adverse events occurred in this study, and a completely adjusted multivariable analysis could not be performed. Moreover, no clinical intervention was performed to the SDB noted in this study. However, all study subjects were enrolled for this study at their chronic stable conditions with compensated hemodynamics, and the development of major LVAD-related complications other than arrhythmic events was similar between groups. Therefore, we believe that differences in the univariate analysis regarding arrhythmic events between groups have a certain clinical implication to advanced HF clinical practice.
Third, the generally accepted cut-off values of RDI associated with adverse clinical outcomes have not been yet determined [30]. However, several previous studies suggest that patients with an RDI ≥ 15 in PSM or polysomnography (PSG) were defined as the SDP group [8]. Therefore, in this study, SDB was diagnosed as RDI ≥ 15 in PSM. Furthermore, since all patients could not undergo PSG, the underlying mechanisms of the sleep disorder (such as CSA or OSA) in each patient were not fully determined.
Fourth, since patients with LVAD occasionally develop VTa asymptomatically, there are possibilities that not all VTa events were collected during the follow-up period.
Conclusion
SBD was prevalent in 24% of the patients with LVAD, and BNP values ≥ 300 pg/mL at the chronic stage after LVAD implantation were associated with the presence of SDB regardless of the hemodynamic parameters. Furthermore, SDB in patients with LVAD might be associated with the incidence of subsequent VTa. The results of this study clearly demonstrate that SDB complications in patients with LVAD have a negative impact on their clinical course, even under chronic stable conditions with compensated hemodynamics.
References
Sharma B, Owens R, Malhotra A. Sleep in congestive heart failure. Med Clin North Am. 2010;94:447–64.
Phillips BG, Narkiewicz K, Pesek CA, Haynes WG, Dyken ME, Somers VK. Effects of obstructive sleep apnea on endothelin-1 and blood pressure. J Hypertens. 1999;17:61–6.
Takahashi S, Nakamura Y, Nishijima T, Sakurai S, Inoue H. Essential roles of angiotensin II in vascular endothelial growth factor expression in sleep apnea syndrome. Respir Med. 2005;99:1125–31.
Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. 2008;118:1080–111.
Bucca CB, Brussino L, Battisti A, et al. Diuretics in obstructive sleep apnea with diastolic heart failure. Chest. 2007;132:440–6.
Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J. Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest. 2007;131:130–5.
Gabor JY, Newman DA, Barnard-Roberts V, et al. Improvement in Cheyne–Stokes respiration following cardiac resynchronisation therapy. Eur Respir J. 2005;26:95–100.
Yagi H, Nakata S, Tsuge H, et al. Significance of a screening device (Apnomonitor 5) for sleep apnea syndrome. Auris Nasus Larynx. 2009;36:176–80.
Di Lenarda A, Remme WJ, Charlesworth A, et al. Exchange of beta-blockers in heart failure patients. Experiences from the poststudy phase of COMET (the carvedilol or metoprolol European Trial). Eur J Heart Fail. 2005;7:640–9.
Stainback RF, Estep JD, Agler DA, et al. Echocardiography in the management of patients with left ventricular assist devices: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2015;28:853–909.
Hoeper MM, Maier R, Tongers J, et al. Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med. 1999;160:535–41.
INTERMACS Executive Committee. INTERMACS adverse event definitions: adult and pediatric patients. http://www.uab.edu/medicine/intermacs/appendices-4-0/appendix-a-4-0. Accessed 17 Nov 2016.
Vazir A, Hastings PC, Morrell MJ, et al. Resolution of central sleep apnoea following implantation of a left ventricular assist device. Int J Cardiol. 2010;138:317–9.
Voortman M, Ramjankan FZ, Lahpor JR, De Jonge N, Kwakkel-Van Erp JM. Obstructive sleep apnea in heart failure with nearly complete resolution after implantation of a left ventricular assist device. J Heart Cardiol. 2014;1:1–3.
Padeletti M, Henriquez A, Mancini DM, Basner RC. Persistence of Cheyne–Stokes breathing after left ventricular assist device implantation in patients with acutely decompensated end-stage heart failure. J Heart Lung Transplant. 2007;26:742–4.
Schaffer SA, Bercovitch RS, Ross HJ, Rao V. Central sleep apnea interfering with adequate left ventricular filling in a patient with left ventricular assist device. J Clin Sleep Med. 2013;9:161–2.
Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med. 1999;160:1101–6.
Christ M, Sharkova Y, Fenske H, et al. Brain natriuretic peptide for prediction of Cheyne–Stokes respiration in heart failure patients. Int J Cardiol. 2007;116:62–9.
Sato T, Seguchi O, Iwashima Y, et al. Serum brain natriuretic peptide concentration 60 days after surgery as a predictor of long-term prognosis in patients implanted with a left ventricular assist device. ASAIO J. 2015;61:373–8.
Fichter J, Bauer D, Arampatzis S, Fries R, Heisel A, Sybrecht GW. Sleep-related breathing disorders are associated with ventricular arrhythmias in patients with an implantable cardioverter-defibrillator. Chest. 2002;122:558–61.
Serizawa N, Yumino D, Kajimoto K, et al. Impact of sleep-disordered breathing on life-threatening ventricular arrhythmia in heart failure patients with implantable cardioverter-defibrillator. Am J Cardiol. 2008;102:1064–8.
Ryan CM, Usui K, Floras JS, Bradley TD. Effect of continuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Thorax. 2005;60:781–5.
Bitter T, Westerheide N, Prinz C, et al. Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J. 2011;32:61–74.
Franz MR. Mechano-electrical feedback in ventricular myocardium. Cardiovasc Res. 1996;32:15–24.
Schlatzer C, Schwarz EI, Sievi NA, et al. Intrathoracic pressure swings induced by simulated obstructive sleep apnoea promote arrhythmias in paroxysmal atrial fibrillation. Europace. 2016;18:64–70.
Yoruk A, Sherazi S, Massey HT, et al. Predictors and clinical relevance of ventricular tachyarrhythmias in ambulatory patients with a continuous flow left ventricular assist device. Heart Rhythm. 2016;13:1052–6.
Bedi M, Kormos R, Winowich S, McNamara DM, Mathier MA, Murali S. Ventricular arrhythmias during left ventricular assist device support. Am J Cardiol. 2007;99:1151–3.
Refaat M, Chemaly E, Lebeche D, Gwathmey JK, Hajjar RJ. Ventricular arrhythmias after left ventricular assist device implantation. Pacing Clin Electrophysiol. 2008;31:1246–52.
Vollkron M, Voitl P, Ta J, Wieselthaler G, Schima H. Suction events during left ventricular support and ventricular arrhythmias. J Heart Lung Transplant. 2007;26:819–25.
Nakashima H, Katayama T, Takagi C, et al. Obstructive sleep apnoea inhibits the recovery of left ventricular function in patients with acute myocardial infarction. Eur Heart J. 2006;27:2317–22.
Funding
The authors have no source of funding statement.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumai, Y., Seguchi, O., Mochizuki, H. et al. Impact of sleep-disordered breathing on ventricular tachyarrhythmias after left ventricular assist device implantation. J Artif Organs 25, 223–230 (2022). https://doi.org/10.1007/s10047-021-01307-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-021-01307-y