Abstract
Background
Complex incisional hernia is still a debatable topic, with increasing incidence and an increased local and systemic postoperative morbidity and mortality. The size of the defect is a risk factor for both difficult closure and 30-day readmission due to complications. The main option for closure such defect is a mesh augmented component separation technique. The goal was to evaluate 30-day wound events and general complications including 90 days mortality.
Material and methods
We present a retrospective study that includes patients from two different university hospitals who underwent open incisional hernia repair with anterior component or posterior component separation between January 2015 and December 2021. Only non-contaminated adult patients (over 18 years old) with postoperative primary or recurrent median abdominal wall defects larger than 6 cm and with complete fascial closure were included. Demographics (age, gender, Body Mass Index—BMI, American Society of Anesthesiologists Classification—ASA score), recurrence rank, and co-morbidities), operative details, patient outcomes complications were collected. A native abdomen/pelvis computerized tomography (CT) scan was performed preoperatively in all patients and the anatomy of the defect and volumetry (abdominal cavity volume, incisional hernia volume and peritoneal volume) were evaluated. One of the component separation technique was performed according to Carbonell’s equation.
Results
Two hundred and two patients (101 from each group) were included. The patients with posterior component separation were more comorbid and with larger defects. The procedure was longer with 80 min but overall length of hospital stay shorter (p < 0.001) for posterior component separation. Seroma, hematoma and skin necrosis were equally distributed for both group of patients and there was no direct relation to surgery (OR 0.887, 95% CI 0.370–2.125, p = 0.788; OR 1.50, 95% CI 0.677–3.33, p = 0.318 and OR 0.386, 95% CI 0.117–1.276, p = 0.119). Surgical Site Infection rate was increased for anterior component separation (p =0.004).
Conclusion
Complex incisional hernia repair is a challenge given by a large amount of wound complications. Choosing between anterior and posterior component separation is still a source of significant debate. We were not able to depict significant different rates of complications between the procedures and we couldn’t find any specific factor related to complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Complex incisional hernia (CIH), despite the seminal paper of Slater et al. [1], is still a debatable topic, which raises many controversies but it is also an active area of surgical innovation and research [1, 2]. Its incidence is increased as older and older patients with multiple associated comorbidities are operated and leads to an increased local and systemic postoperative morbidity and mortality. The size of the defect (especially its width) is a risk factor for both difficult closure and 30-day readmission due to complications [3]. Closure of defects larger than 10 cm width are more likely to need component separation techniques (CST) as Smith et al. recently reported [4].
Following the introduction and popularization of Anterior Component Separation (ACS) by Ramirez et al. in 1990, Novitsky modified component separation is an attempt to minimize and optimize early and late complications [5]. Both CST act as natural tissue expanders but there are little published research especially multi-centric trials comparing the outcomes of anterior versus posterior component separation. The most proper and effective CST remains under active debate despite the new data that suggest the greater effectiveness of posterior compared to anterior component separation in terms of wound morbidity and recurrence [6].
Surgical repair for giant IH is a high-risk procedure with considerable early and late morbidity. Our study is focused mainly on complex hernias (defined by larger defects, difficult locations, etc.) that cannot be primary closed without excessive tension and management based on mesh augmented by CST. As wound morbidity is a measure of early success, we compared the early outcomes of patients undergoing open hernia repair based on the utilization of ACS and Posterior Component Separation with Transversus Abdominis Muscle Release (PCSTAR) with on lay and, respectively, sublay mesh reinforcement in two different tertiary university teaching hospitals. The second goal was to identify if the surgery itself is a major factor inducing wound morbidity and what other patient- and hernia-related factors contribute to poorer outcomes.
Material and methods
Patients
Our retrospective study is from a prospective data base and includes patients from two different university hospitals who underwent open incisional hernia repair with anterior component or posterior component separation between January 2015 and December 2021. Only non-contaminated adult patients (over 18 years old) with postoperative primary or recurrent median abdominal wall defects larger than 6 cm and with complete fascial closure were included. Emergent patient, lateral, and parastomal hernias were excluded as we believe they present higher complexity with different and specific complications and recurrence rates. Also, patients without a preoperative CT scan, dirty and infected wound class patients, patients in whom anterior fascia could not be closed, and single-sided separation were excluded.
Patients were distributed into two groups depending on the provenience and type of the procedure: group MS with ACS (Clinical County Hospital, Tirgu Mures) and group CJ (Clinical Military Hospital, Cluj-Napoca,) with PCSTAR; will refer to them as ACS group and PCSTAR group (posterior component separation). The Local Ethic Committee under Ad. 10781/19.04.2021 and A4528/25.11.2020 approved the study.
The written informed consent from each patient was obtained. Demographics (age, gender, Body Mass Index—BMI, American Society of Anesthesiologists Classification—ASA score, recurrence rank, and co-morbidities), operative details, patient outcomes and complications were collected. Four surgeons contributed to the database with surgical procedures (VO, MT, MG, and, CM) all of them senior surgeons with extended experience in visceral surgery and abdominal wall reconstruction.
CT protocol investigation
A native abdomen/pelvis computerized tomography (CT) scan was performed preoperatively in all patients. The surgeon and a radiologist reviewed all pre-operative CT scans. We removed all inconsistencies of the measurements after the cross review. Both, the surgeon and the radiologist, carefully identified and measured the length and the width of the defects in their maximal dimensions. The defect was approximated by an ellipse and the area of the defect was calculated using the formula ½ length × ½ width × π. The values were rounded to the nearest hundred or thousand. We also measured the width of both rectus sheath (RW). The ratio between their sum and the width of the defect (DW) was the basis for both ACS and Transversus Abdominis Muscle Release (PCSTAR) indication (2RW: DW = 2:1 Carbonell’s equation) [7]. The volumes of the abdominal cavity (ACV) and of the incisional hernia sac (IHV) are calculated according to the Tanaka method [8]. By adding up ACV and IHV, we obtained the volume of the peritoneal cavity (PV). The ratio of IHV and PV provides the peritoneal index (Sabbagh Index) as measurement of loss of domain [9]. A 25% cut-off of the Sabbagh index was considered for loss of domain as an arbitrary limit in both clinics. All the values were manually collected; differences of more than ± 10% between surgeon and radiologist’s measurements were reassessed until agreement was reached.
Surgical procedure
All the procedures were performed under general anesthesia according to the technique described by Ramirez [10] and Novitsky [11]. All patients had intravenous antimicrobial and antithrombotic prophylaxis according to each hospital protocols. No local adjuvants such as Botox or Progressive Preoperative Pneumoperitoneum were considered for this study.
After adhesiolysis, the peritoneal sac was dissected and the abdominal wall reconstructed according to each clinic and with the original technique [10, 11].
In patients with ACS, a slowly absorbable monofilament-running suture (1 polydioxanone) closed the abdominal wall. Medium weight macroporous monofilament polypropylene mesh was placed on-lay and fixed in place with interrupted monofilament non-absorbable suture (3/0 polypropylene) according to surgeons’ preference. The mesh surface was around 900 cm2 in almost all patients.
A slowly absorbable monofilament-running suture (2–0 polydioxanone) closed the posterior fascia in patients with PCSTAR. We fixed the mesh with slowly absorbable transfascial sutures (0 polydioxanone) or with cyanoacrylate (Histoacryl® B Braun). Medium weight macroporous monofilament polypropylene mesh (with the area fivefold larger than defect area) reinforced the abdominal wall in all circumstances. A slowly absorbable running suture (1 polydioxanone) closed the anterior fascia. For mesh recurrences the old mesh was completely removed whenever possible.
All PCS patients were drained with more than one suction drainage until the volume of the liquid was less than 30 ml/24 h for two consecutive days. Two drains were placed over the mesh in the retromuscular space and another one in the subcutaneous space. In patients with ACS one or two drains were left in place over the mesh until less than 30 ml were drained for two consecutive days.
In both groups, before skin closure, an elliptic curve of skin and subcutaneous fat was removed on both sides of the incision to eliminate the excess tissue. The amount of scared, fibrotic and de-vascularized skin with its underlying fat varied in relation with the hernia size. Abdominoplasty was not routinely performed.
Functional evaluation
The standard method for indirectly measuring intra-abdominal pressure (IAP) is to measure the intra-vesical pressure [12]. Briefly, the bladder drainage system was clamped just distally to the connection of the urinary catheter to the drainage bag. An 18-gauge needle was then inserted into the sampling port and connected via a sterile tube to the pressure transducer using two three-way stopcocks. A standard infusion bag of normal saline was attached to one stopcock, and a 60-ml syringe was connected to the second stopcock. Sterile saline (50–100 ml) was injected into the bladder. Measurements were taken at end-expiration while patients were in complete supine position and with the transducer zeroed at the symphysis pubis level. Intra-abdominal pressure was recorded before surgery, immediately after the end of the procedure, 24, and 48 h after TAR on the awakened patient. Intra-abdominal hypertension (IAH) is defined by a sustained or repeated elevation in IAP ≥ 12 mmHg. IAH was graded as follows: Grade I, IAP = 12–15 mmHg; Grade II, IAP = 16–20 mmHg; Grade III, IAP = 21–25 mmHg; and Grade IV, IAP > 25 mmHg [13]. Likewise, abdominal compartment syndrome (AbCS) was defined as IAP > 20 mmHg in combination with at least one organ failure.
Plateau pressure (PPLAT) is the pressure applied to small airways and alveoli during positive-pressure mechanical ventilation. It is measured during an inspiratory pause on the mechanical ventilator and it was recorded after 20 min since the onset of the procedure and 20 min after the anterior fascia was closed. The difference between the first and last record of the plateau pressure was noted as Δ plateau pressure.
The main outcomes of interest were 30-day wound events and general complications including 90 days mortality. Postoperative wound events included Surgical Site Infection (SSI), Surgical Site Occurrence (SSO), and Surgical Site Occurrences Requiring Procedural Intervention (SSOPI). According to the Centre for Disease Control and Prevention (CDC), SSI was defined as superficial, deep or organ space [14]. Surgical Site Occurrence included any SSI, in addition to wound cellulitis, non-healing incisional wound, skin or tissue ischemia, skin or soft tissue necrosis, fascial disruption, serous or purulent wound drainage, stich abscess, seroma, hematoma, infected or exposed mesh, enterocutaneous fistula. Procedural interventions which were considered SSOPI included wound opening and/or debridement, stich removal, percutaneous drainage, partial and/or complete mesh removal [14]. Length of hospital stay, 30-day readmission and mortality were also analyzed. Patients having multiple wound complications such seroma and infection, dehiscence and infection, were classified as were classified as the most severe. The follow-up for this study was short and extended for 90-days for all patients.
Statistical analysis
Descriptive statistics for approximately normally distributed continuous variables are presented as mean ± standard deviation, otherwise the median and quartiles are displayed. The numbers and percentages are shown for categorical data. The observed percentage with 95% Clopper–Pearson exact confidence interval are displayed by group.
Baseline and univariate differences between the groups were assessed by the two-sample t-test for approximately normally distributed continuous variables, the Kruskal–Wallis test for skewed continuous data and the Chi-squared test for categorical data.
Multivariable logistic regression models were fitted for binary endpoints and the adjusted odds ratio for surgery type (using ACS as the reference level) and adjusted p-value displayed. First, type of surgery was forced into the model. Then confounders entered the model, stepwise, if their p-value for entry was < 0.05 and remained in the model if their p-value for removal < 0.10. The following potential confounders are considered: sex, environment, diabetes, obesity, COPD, CVD and smoking history, ASA, location, plateau pressure day, age, BMI, recurrence, occurrence, length, width and surface area of the defect, IHV, PV, preoperative IAP, postoperative IAP, day 1 IAP, day 2 IAP, change in plateau pressure, operation time The receiver operated characteristics (ROC) curves and area under ROC (AUROC) were used to assess the model goodness of fit.
Statistics were performed using the statistical package SAS, version 9.4. All tests were two-sided with a significance level displayed without multiplicity adjustment.
Results
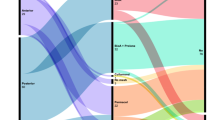
Two hundred and two patients (101 from each group) met the inclusion criteria and consented to be included in the research (Fig. 1). The patients undergoing component separation were examined for differences in preoperative factors (Table 1). There was no difference in gender, BMI, and ASA score (p > 0.05 for each). Patients in the ACS were younger than in the PCSTAR (mean age 59.13 ± 11.21 years vs. 63.00 ± 6.78 years; p = 0.021). There were major differences between the groups in terms of comorbidities, the patients of PCSTAR group being more comorbid (Table 1). Previous hernia repair has been performed in 71 (70.3%) and 27 (26.7%) patients in the ACS and PCSTAR groups, respectively (p < 0.001). For the detailed rank of recurrences, see Table 1. No patient had a previous component separation with or without mesh. In 42 patients (29 in ACS group) the recurrence was recorded after a mesh repair. According to pre-operative file reports the mesh was located as an on lay in 27 patients (19 in the ACS group), as a sub-lay in three (all of them in the PCSTAR group) and preperitoneal in the rest of them (all in the PCSTAR group).
Hernia characteristics in terms of length, width, defect surface and volumetry showed larger values for the PCSTAR patients with a significant difference for all of them (Table2). Loss of domain (Sabagh index higher than 0.25) was recorded in 179 patients (78.62%). One hundred and five were with a Sabbagh index between 0.26 and 0.33 (35 in the ACS group and 70 in the PCSTAR group), and 74 (36.63%) with an index larger than 0.33 (48 patients in the ACS vs. 26 in the PCSTAR. The mean preoperative intra-abdominal pressure was 7 mmHg for the ACS group (Q1–Q3 = 5–8) compared to 6 mmHg for the PCSTAR patients (Q1–Q3 = 5–8) (p = 0.059).
The median operative time was significantly longer for patients undergoing PCS (110 min vs. 190 min; p < 0.001) (Table 3). There was a significantly statistical difference in intraoperative complications with more complications occurring in ACS group compared to PCSTAR (15.84% vs. 6.93%; p < 0.01). At the end of the procedure, mean IAP was equal for both group of patients but significantly higher after 24 h in patients from the PCS group (16.72 vs. 18.18; p < 0.001). The median overall length of hospital stay was longer for ACS patients [9.0 days (Q1–Q3 = 7–11)] compared to PCSTAR patients [7 days (4–10)]; (p < 0.001). Postoperative length of stay for each group had median of 6 days, but different distributions (p = 0.031). Longer postoperative stays are associated with the ACS group.
There was no difference between groups for Intensive Care Unit (ICU) stay (p = 0.829).
Outcomes
-
1.
Overall length of hospital stays greater than 7 days: In univariate analysis, 117 events were recorded (72 for patients with ACS; p = 0.0001). The final model includes the type of surgery and log (OR time) with high specificity and sensitivity [area under curve (AUROC) = 0.7291; p < 0.0001; no outliers]. There was a significant difference between the surgeries adjusting for the confounders (type of surgery OR—0.070; 95% CI 0.026–0.191; p < 0.001 and log (OT in minutes) OR—7.850; 95% CI 2.901–21.242; p < 0.001).
-
2.
Postoperative hospital stay: Univariate analysis showed 34 events for patients with ACS and 36 for patients with PCSTAR; there was no significant difference between the groups (p = 0.7674). The final model includes surgery, log (OT in minutes) (p-value for entry = 0.0028), and BMI (p-value for entry = 0.040). There was a reasonable specificity and sensitivity for the model (AUROC = 0.6442; p = 0.0003; no outliers). A significant difference between the surgeries adjusting for these confounders was recorded.
-
3.
Intensive Care Unit stay: for Intensive Care admission (yes/no) univariate analysis showed no differences between the number of patients included in the ICU (11 patients in ACS group vs. 12 patients for PCSTAR; p = 0.8247). The multivariable logistic regression model was created for the types of surgery, log (OT in minutes), smoking, and fitted reasonably well (AUROC 0.7236; p < 0.0001). There is a significant difference between the surgeries adjusting for the confounders (type of surgery OR—0.287; 95% CI 0.084–0.976; p = 0.046 and log (OT) OR—6.093; 95% CI 1.462–25.392; p = 0.013). When comparing active smokers with non-smokers a threefold increase in ICU admission was found despite the type of surgery (OR—3.313; 95% CI 1.136–9.663; p = 0.028).
-
4.
Acute respiratory failure (ARDS): eleven events were recorded in univariate analysis (5.44% of all patients) equally distributed in both groups (6 patients for ACS group and 5 patients for PCSTAR group). No significant difference between groups was found (p = 0.757). The logistic regression final model includes besides type of surgery, preoperative IAP (p-value for entry 0.0106) and obesity (p-value for entry 0.0133) with a high sensitivity and specificity for confounders (AUROC = 0.822; p < 0.0001) and no outliers. There is no significant difference between the surgeries adjusting for the confounders. Adding preoperative IAP quartiles and the transformation of the raw data in the stepwise selection model did not reveal different data for this endpoint (data not shown).
-
5.
Seroma: nineteen events (18.81%) were recorded for ACS group of patients and only 15 for PCSTAR (14.85%). There was no significant difference between groups (p = 0.452). For the final model obesity with a BMI over 35 kg/m2 (p-value for entry 0.0236), age (entry p = 0.0408) and diabetes (entry p = 0.0451) were included. The model fits reasonably well with moderate sensitivity and specificity (AUROC = 0.6857; p = 0.0002) and no outliers. There is no significant difference between the surgeries adjusting for the confounders.
-
6.
Hematoma: overall 29 events were reported (12 patients after ACS and 17 for PCSTAR) without significant difference between groups (p = 0.316). No confounders were added, the final model including only the type of surgery with a moderate sensitivity and specificity (AUROC = 0.5503). There is no difference in the incidence of hematoma according to the type of abdominal wall reconstruction (OR—1.501, 95% CI 0.677–3.330; p = 0.318)
-
7.
Surgical Site Infection: In univariate analysis, we record 12 patients with SSI in the ACS group (11.88%) versus 6 for the PCSTAR group (5.94%). The difference between groups was insignificant (p = 0.318). The main confounder with predictive value included for logistic regression was OT in minutes (p entry value 0.0099). The model fits reasonably well with no outliers (AUROC = 0.6955; p = 0.0058). There was a significant difference between the surgeries adjusting for the confounders (p = 0.009) favouring PCSTAR. The analysis was extended to logarithmic transformation in the logistic regression model which included log (OT in minutes p = 0.022) and the IAP from the second postoperative day. There was an increased sensitivity and specificity for this model (AUROC = 0.7156; p = 0.0014). An increased statistical difference was found between the surgeries (OR—0.114; 95% CI 0.026–0.492; p = 0.004). The operative time (OR—6.022; 95% CI 1.370–26.466; p = 0.017) and the second day IAP (OR—1.196; (95% CI 0.995–1.437; p = 0.056) were independent predictors for SSI in logistic model.
-
8.
Skin necrosis: there was no significant difference between groups related to this complication in the univariate model (11 events for ACS group vs. four for PCSTAR group—p = 0.060). The final model includes the types of surgery and the cardiovascular diseases with a higher specificity and sensitivity (AUROC = 0.7098; p < 0.0001). No significant difference between the surgeries adjusting for the confounders (OR—0.386; 95% CI 0.117–1.276; p = 0.119) was identified. Cardiovascular diseases were the only independent predictors for skin necrosis.
-
9.
Bowel regulation: Only 43 patients in ACS group and 30 in the PCSTAR group resumed their intestinal movements within the first 48 h. There was no significant difference between groups. The final model includes log (OT in minutes) (p-value for entry 0.0182) and ASA score (p = 0.0321). The model fits reasonably well with a good sensitivity and specificity (AUROC 0.677, p < 0.0001) and no outliers. There was a significant difference between surgeries adjusting for the confounders (OR—0.236; 95% CI 0.099–0.559; p = 0.001).
A synthesis of all data is represented in Table 4 and Fig. 2.
No mortality was recorded after 90 day-follow-up. Systemic complications included thromboembolic disease (4 patients in ACS group and 3 in PCSTAR group), ileus (12 vs. 21 patients), and prolonged O2 requirements (11 vs. 7).
Discussion
The component separation techniques both anterior or posterior have gained popularity due to their promising short-and long-term results with acceptable 30-day wound morbidity despite complex and challenging patients. The effectiveness of these techniques was proved by the increased rate of fascial closure so they were quickly accepted as viable options for difficult cases [15]. The proper application of the most effective CST in patients with CIH is still a debate; choosing the optimal surgical procedure and space of mesh implantation for the proper patient and by the proper surgeon are paramount [16]. The open approach is still widely used despite the development of a large variety of minimally invasive (laparoscopic or robotic) approaches that are presumed to limit wound morbidity [5, 17, 18]. Our study, focused on patients with large midline abdominal wall defects, evaluated the early outcomes of patients with on lay ACS and PCSTAR and this is probably one of the few multi-centric analyses comparing the procedures.
Demographic data showed that our groups were homogenous in terms of gender, obesity, and ASA score; patients in the PCSTAR were older and more comorbid but with fewer recurrences than patients in ACS group. The incidence of smoking was higher in PCSTAR patients. Our results are somehow, opposite with Krpata’s study in which PCSTAR patients were younger, with a lower mean ASA score, and with more male patients [19]. In 2021, Pereira-Rodriguez et al. in large number of patients from Spanish Registry of Incisional Hernia (EVEREG), reported equal obese patients, equal comorbidities but more high-risk patients with larger defects for ACS patients [20].
Overall, in the univariate analysis there was no significant difference regarding the incidence of local wound complications (54 patients in ACS group vs. 33 in PCSTAR group; p = 0.061). The same results were obtained comparing groups for specific complications (seroma, hematoma, SSI, and skin necrosis). Our results are similar to Pereira-Rodriguez et al. who found equal distribution of Surgical Site Occurrence, seroma, and hematoma; there were more wound infections and skin necrosis in patients with ACS (10.6% vs. 7.0%, p = 0.05, respectively 4.4% vs. 0.1%, p < 0.001) [20]. Krpata reports more complications in ACS group while Blair found that PCSTAR was associated with less infections but without any significant difference (p = 0.07) [19, 21].
A very interesting and somehow controversial finding of this study was the fact that, contrary to what we expected, no hernia related factors were independently associated predictors with local complications. It was expected that the width of the defect to be highly correlated with local complications but this was not observed with our patients. Franklin et al. showed in 2013 that the patients defect in relation to abdominal wall circumference is a more reliable prediction factor; associated with the dynamic value of the patient specific anatomy and compliance it could better predict the onset of wound complications. The same authors demonstrated that fascial approximation decreased for every incremental increase in defect diameter [22]. In our patients mean width defects of 14 respective 17 cm were completely closed with the aid of medial translation provided only by the component separation technique. PCSTAR medialization effect was larger than for the ACS and is in accordance with Majumder et al. which results from a cadaveric study [23]. After a complete PCSTAR with large retro-muscular dissection, an average advancement of 10 cm for the anterior fascia and 11 cm for the posterior fascia on each side was obtained. This can provide a significant increase of the abdominal cavity inner diameters and, subsequently, an increase of the whole visceral sac volume, without or with minimal consequences upon normal physiology [24]. The reduced mean value of postoperative plateau pressure in patients with PCSTAR is a valid proof of the effectiveness of this advancement compared to ACS even if in the first postoperative day IAP pressure was higher.
Acute respiratory failure was the main reason for ICU admission but unusually, it was not influenced by hernia related factors. Smoking was the only factor associated with this and increased threefold the probability for ICU admission compared with non-smoking patients. Even if in the PCSTAR there were more active smokers than in the ACS group, the number of respiratory complications was similar. Similarly, smoking was not involved as a potential risk factor for wound complications. This is in accordance with the study of Lindmark et al. who demonstrated that smoking is an influencing factor of poor outcomes after IH repair [25]. On the other hand, recently Gräsbec et al. in a large population study (the sample included 158 638 surgeries) have demonstrated that smokers have increased odds of overall complications (OR = 1.17; 95% CI 1.14–1.20) and critical complications (OR = 1.21; 95% CI 1.14–1.29). Corresponding odds ratios of ex-smokers were 1.09 (95% CI 1.06–1.13) and 1.09 (95% 1.02–1.17). Smokers had increased odds of overall complications in all specialties with over 10 000 surgeries [26].
The type of surgery was an independent factor for complications only when it was associated with other confounders (operative time and IAP for SSI); there was no specific statistically significant difference between groups of patients related to the type of the procedure. The results are difficult to explain because we record longer operative time in PCSTAR patients with similar SSI, which is contradictory. Probably the association with a better optimization led to better results.
Obesity, known as a modifiable risk factor which increases rates of SSI, was in our study highly associated only with seroma formation and only when BMI was higher than 35 kg/m2.
The operative time was the only variable responsible for more poor outcomes than the traditional well documented risk factors. In a recent meta-analysis and systematic review Cheng et al. examined the relation between operative duration and incidence of SSI across surgical specialties [27]. Without any direct reference to incisional hernia, pooled analyses demonstrated that the likelihood of SSI increased by close to twofold in surgeries exceeding operative cutoff times of one, two, three, or four hours, and close to threefold in surgeries exceeding five hours. Interestingly, pooled analyses further demonstrated that the odds of developing an SSI increased with increasing operative time increments. This relation typically remained statistically significant across categories of time. For example, the likelihood of SSI was observed to increase by 5% for every 10 min of surgery, 13% for every 15 min of surgery, 17% for every 30 min of surgery, and 37% for every 60 min of surgery. The studies reporting mean operative time for patients with and without SSI, patients who developed an SSI had a mean duration that was, on average, 0.82 h–1.13 (median = 0.5 h) longer than those without SSI. In our study, patients with PCSTAR had a mean longer operative time which demonstrates a more complex procedure. It was interesting that the longer operative time associated with PCSTAR was not associated with an increased rate of SSI and we do not have a valid explication for this. Although operative time is mentioned as a significant predictor in some reviews, there is a poor understanding of how this risk factor varies across surgery types, the magnitude of the association, and the relation between increasing increments of operative time and SSI [28,29,30].
Finally, we acknowledge that our study has some limitations. Even if it is the result of the collaboration between two surgical departments, its retrospective nature is always subject to data entry errors and misinterpretation. Another limitation is the selection of the patients; in our study, we only include midline hernias and patients with complete fascial closure which can represent a potential bias for the result. Likewise, a potential bias for inquorate results can be the level of expertise all data being collected from a limited number of surgeons with large patient volume. The accurate comparative analysis of ACS and PCSTAR is difficult to be standardized in terms of preoperative evaluation, defining outcomes, and interpretations. We can also consider as a limitation the risk of over treating, especially in ACS group of patients. Another limitation is the short follow-up period. We considered in our report only immediate outcomes because we cannot evaluate the accuracy of long-term outcomes for the patients with ACS; the protocol of follow-up in patients with PCS was not superimposed with the protocol of ACS. Last, no emergency operation was included and this is a serious bias for the quality of the results being known that the rate of complications and mortality in this particular situation is almost double.
Conclusion
Our study demonstrates once again that complex incisional hernia repair is a challenge given by a large prevalence of wound complications. Choosing between ACS and PCSTAR is still a source of significant debate. We were not able to depict significant different rates of complications between the procedures and we could not find any specific factor related to complications. The operative time and obesity were factors related to more than two wound complications. Future controlled comparative trials with standardized outcome measures, particularly regarding the report of wound morbidity, are recommended to confirm our conclusions.
Data availability
Data are available and can be provided by the corresponding author by request.
References
Slater NJ, Montogomery A, Berrevoet F et al (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18:7–17. https://doi.org/10.1007/s10029-013-1168-6
Moores N, Conway H, Donato D et al (2019) Is release of the posterior lamella enough? A cadaveric exploration of posterior component separation techniques. Am J Surg 218:533–536. https://doi.org/10.1016/j.amjsurg.2018.12.011
Blatnik JA, Harth KC, Aeder MI, Rosen MJ (2011) Thirty-day readmission after ventral hernia repair: predictable or preventable? Surg Endosc 25:1446–1451. https://doi.org/10.1007/s00464-010-1412-4
Smith JR, Kyriakakis R, Pressler MP et al. (2022) BMI: does it predict the need for component separation? Hernia Published Online: 21 March 2022. https://doi.org/10.1007/s10029-022-02596-9
Yazid MM, De La Fuente Hagopian A, Farhat S et al (2022) Does surgeon specialty make a difference in ventral hernia repair with the component separation technique? Cureus 14(6):e26290. https://doi.org/10.7759/cureus.26290
Oprea V, Toma M, Grad O et al (2023) The outcomes of open anterior component separation versus posterior component separation with transversus abdominis release for complex incisional hernias: a systematic review and meta-analysis. Hernia 27:503–517. https://doi.org/10.1007/s10029-023-02745-8
Carbonell A (2018) The 9th annual abdominal wall reconstruction summit, Montana, USA
Tanaka EY, Yoo JH, Rodrigues AJ Jr et al (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernias with loss of domain. Hernia 14:63–69. https://doi.org/10.1007/s10029-009-0560-8
Sabbach C, Dummont T, Robert B et al (2011) Peritoneal volume is predictive of tension-free fascia closure of large incisional hernias with loss of domain: a prospective study. Hernia 15:559–565. https://doi.org/10.1007/s10029-011-0832-y
Ramirez OA, Ruas E, Dellon AL (1990) “Component separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86:519–526. https://doi.org/10.1097/00006534-199009000-00023
Novitsky YW, Elliot H, Orenstein SB, Rosen MJ (2012) Transversus abdominis release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204:709–716. https://doi.org/10.1016/j.amjsurg.2012.02.008
Ivatury RR (2018) Open abdomen: historical notes. In: Coccolini F, Ivaturi R, Sugrue M, Ansaloni L (eds) Open abdomen. A comprehensive practical manual. Springer, London, pp 1–26
Fugazzola P, Montori G, Rizoli S, Ansaloni L, Rezende-Neto J (2018) Basic research in open abdomen. In: Coccolini F, Ivaturi R, Sugrue M, Ansaloni L (eds) Open abdomen. A comprehensive practical manual. Springer, London, pp 27–53
National Healthcare Safety Network (2022) Surgical site infection event (SSI). http://cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.Pdf. Accessed 19 Feb 2022
Bilezikian JA et al (2021) Comparing the outcomes of external oblique and transversus abdominus release using the AHSQC database. Hernia 25:365–373
Fayezizadeh M, Majumder A, Belyansky I, Novitsky YW (2016) Outcomes of retromuscular porcine biologic mesh repairs utilizing transversus abdominis release reconstruction. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2016.06.008
Bueno-Lledó J, Bonafe-Diana S, Carbonell-Tatay F et al (2021) Component separation and large incisional hernia: predictive factors of recurrence. Hernia 25:1593–1600. https://doi.org/10.1007/s10029-021-02489-3
Chatzimavroudis G et al (2021) Outcomes of posterior component separation with transversus abdominis release (TAR) in large and other complex ventral hernias: a single-surgeon experience. Hernia 2021:1–9
Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ (2012) Posterior and open anterior component separation: a comparative analysis. Am J Surg 203:318–322. https://doi.org/10.1016/j.amjsurg.2011.10.009
Pereira-Rodriguez JA et al (2021) Early outcomes of component separation techniques: an analysis of the Spanish registry of incisional Hernia (EVEREG). Hernia 25(6):1573–1580
Higgins RM et al (2017) Cost analysis of robotic versus laparoscopic general surgery procedures. Surg Endosc 31:185–192
Franklin BR, Patel KM, Nahabedian MY et al (2013) Predicting abdominal closure after component separation for complex ventral hernias: maximizing the use of preoperative computed tomography. Ann Plast Surg 71:261–265. https://doi.org/10.1097/SAP.0b013e3182773915
Majumder A, Miller HG, del Campo LM et al (2018) Assessment of myofascial medialization following posterior component separation via transversus abdominis release in a cadaveric model. Hernia. https://doi.org/10.1007/s10029-018-1771-7
Oprea VC, Rosian M, Mardale S, Grad O (2020) Is transversus abdominis muscle release sustainable for the reconstruction of peritoneal volumes? A retrospective computed tomography study. Int J Abdom Wall Hernia Surg 3:25–33
Lindmark M, Strigård K, Löwenmark T et al (2018) Risk factors for surgical complications in ventral hernia repair. Worl J Surg 42:3528–3536. https://doi.org/10.1007/s00268-018-4642-6
Gräsbeck HL, Reito ARP, Ekroos HJ et al (2023) Smoking is a predictor of complications in all types of surgery: a machine learning-based big data study. BJS Open. https://doi.org/10.1093/bjsopen/zrad016
Cheng H, Chen BP-H, Soleas IM et al (2017) Prolonged operative duration increases the risk of surgical site infections: a systematic review. Surg Infections 18:722–735. https://doi.org/10.1089/sur.2017.089
Korol E, Johnston K, Waser N et al (2013) A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS ONE 8:e83743
Gibbons C, Bruce J, Carpenter J et al (2011) Identification of risk factors by systematic review and development of riskadjusted models for surgical site infection. Health Technol Assess 15:1–156
Mavros MN, Athanasiou S, Alexiou VG et al (2011) Risk factors for mesh-related infections after hernia repair surgery: a meta-analysis of cohort studies. World J Surg 35:2389–2398
Funding
No financial support was necessary for this study.
Author information
Authors and Affiliations
Contributions
MT, VO, MG, CM: surgical procedures database, study conception and design, acquisition, analysis and interpretation of data, drafting the work and revising, final approval of the version to be published; HS: statistical analysis and interpretation of data, final approval of the version to be published; OA, CEB, and OG: drafting the paper and final approval of the version to be published;
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
No animal was used for this study.
Informed consent
Informed written consent was obtained from all patients before surgery.
Thanks
Special thanks to Helen Staines at plotsRdata.com for producing the figures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Toma, M., Oprea, V., Grad, O. et al. Early outcomes of open anterior versus posterior components separation with transversus abdominis release for large median incisional hernias: a retrospective stepwise analysis. Hernia 28, 803–813 (2024). https://doi.org/10.1007/s10029-023-02920-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02920-x