Abstract
Purpose
To clarify the factors related to recurrence after component separation technique (CST).
Materials and methods
A retrospective study was conducted of 381 patients who underwent CST between May 2006 and May 2017 at a tertiary center. All patients had a transverse hernia defect grade W3 in EHS classification. Recurrence rate was determined by clinical examination plus confirmation by abdominal CT scan.
Results
At a median of 61.6 months of postoperative follow-up, we reported 34 cases of hernia recurrence (8.9%). On multivariate analysis, BMI > 30 (OR 2.20; CI 1.10–3.91, p = 0.031), immunosuppressive drug use (OR 1.06 CI 1.48–2.75, p = 0.003) and development of surgical site infection (OR 2.7; CI 1.53–4.01, p = 0.002) were factors of recurrence after CST. There was no difference in recurrence rate among repairs of primary and recurrent hernias, urgent repair, operative time, type of prosthesis, or concomitant procedures, even planned or unplanned enterotomies.
Conclusion
Obesity (BMI > 30), immunosuppressive drug use, and postoperative wound infections were predictors of recurrence after CST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The component separation technique (CST) has traditionally been used for large abdominal wall defects [1]. This technique has demonstrated to accomplish primary closure of hernia defect, while maintaining normal anatomy and physiology of the abdominal wall. Although several groups have evaluated a variety of endoscopically assisted approaches to limit wound morbidity classically associated to this technique, open CST is widely performed in the field of abdominal wall reconstruction [2]. Although the efficacy of this technique has been established, recurrence remains a challenge. Recurrence after primary repair of large incisional hernia (IHs) was reported to be 20–30% and as high as 30% after secondary repair of recurrent IHs [3]; the CST may decrease its risk and provide a reliable autologous reconstructive option for complex ventral defects, especially in midline hernias [4, 5]. Hernia recurrence rates of 8–22% have been reported after surgery performed using the CST, with mean follow-up periods ranging from 8.5 months to 4.6 years [2, 6].
There is little published research on risk factors for recurrence after hernia surgery using the CST. Current evidence suggests recurrent herniation is attributable to a combination of patient factors, operative technique, and quality of perioperative care. Analyzing clinical data on IHs recurrence, a similar set of patient’s risk factors are reported: increased age, obesity, diabetes, chronic obstructive pulmonary disease (COPD), steroid medication use, and operative factors as repair technique or surgical site occurrences [7,8,9,10,11,12]. Such research could shed light on how to prevent hernia recurrence.
According to the publications, few authors have reported so many cases in their research about CST. The goal of this manuscript was to describe our experience using the CST in a long series of patients with midline IHs, clarifying predictors for recurrence after the application of this technique.
Material and methods
The data of all patients with IHs who underwent surgery using the CST between May 2006 and May 2017 at a tertiary center were collected. All the patients underwent preoperative imaging, including an abdominal CT scan. All the patients had a transverse hernia defect greater than 10 cm (i.e., a grade W3 hernia according to the European Hernia Society classification) [13]. Ethics committee of our hospital approved our study.
Thromboembolic prophylaxis (enoxaparin), sequential compression devices, and antibiotic prophylaxis prior to a skin incision that continued throughout their hospital stay were applied in all the patients. The hernia repairs were performed by five surgeons, members of the Abdominal Wall Surgery unit. The whole cohort followed a “non-classical” CST, which was an open repair and using a mesh for the abdominal wall reconstruction. The hernia sac and fascial defect were first dissected, and adhesiolysis was performed as necessary to expose the hernia. The transverse and longitudinal dimensions of the fascial defect were then measured. A fasciotomy of the external oblique aponeurosis was performed, followed by dissection of the tissue plane between the external and internal oblique muscles before medial advancement of the rectus muscle, as it has been previously described [4]. After the rectus muscles were re-approximated in the midline, a polypropylene or polyvinylidene fluoride (PVDF) mesh was placed onlay. In some cases, the mesh was anchored to the costal margin and anterior iliac spine and pubis between the internal and external muscles using nonabsorbable tackers or nonabsorbable (Prolene) sutures. The decision on the type of prosthesis depended upon the surgeon. This constituted the “first level” of the CST. A “second level” of the repair was performed if primary closure of the fascia was not possible following the first-level procedure, with a retromuscular mesh reinforcement [4]. The final step of the surgical procedure was a myoplasty, fixing the border of the external oblique muscle to the mesh. Two closed suction drains were placed and maintained throughout the patients’ hospital stay. The drains were removed when drainage was less than 10–20 cc/24 h. In patients who had sufficient excess skin to warrant an abdominoplasty, plastic surgeons performed it at the time of the hernia surgery.
Recurrence was determined by a palpable mass at the site of the previous hernia repair in a clinical examination, in addition to confirmation by a CT scan. The patients were followed up 1 month, 3 months, and 1 year after the surgery, followed by subsequent annual follow-ups. Complete 5-year follow-up period was achieved in most patients, and a CT scan was performed to check their well-being at the end of this period.
Risk factors for recurrence after the CST were identified, and the occurrence of these factors in patients with and without recurrence during the follow-up period was compared. Demographic and following variables were recorded: body mass index (BMI), diabetes mellitus, COPD, immunosuppression, smoking, and American Society of Anesthesiologist’s score. They were identified using the physician-abstracted operative notes. Intraoperative and postoperative data collected included the number of previous hernia repairs, size and location of the IH at the time of the surgery according to the classification criteria of the European Hernia Society, types and sizes of the meshes used, suture material, operative duration, concomitant procedures, length of hospital stay, surgical site-related complications (i.e., wound hematomas, seromas, wound infections, or skin necrosis), mesh infections, abdominal compartment syndrome, mortality, and length of follow-up.
A software program SPSS Version 20.0 was used in the statistical analysis. A univariate analysis was performed using the Student’s t test to explore continuous variables, and a Chi-square or Fisher’s test was conducted for analysis of dichotomous variables. Variables with p values of < 0.25 were included in a multivariate logistic regression analysis (backward stepwise) to obtain odds ratios (ORs) and their 95% confidence intervals for all risk factors of IH recurrence. A Kaplan–Meier survivor analysis was used to assess the time to recurrence.
Results
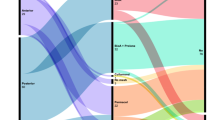
Three hundred and eighty-one consecutive patients who underwent surgery using the CST from May 2006 to May 2017 were included in the study. Complete 5-year follow-up period was achieved in 368 cases (96.5%). In a median postoperative follow-up of 61.6 months (range 51–71), there were 34 (8.9%) cases of recurrence. The Kaplan–Meier curve in Fig. 1 shows recurrence-free survival. In terms of hernia recurrence sites, they were suprapubic in 8 (23.5%) patients, lateral to the prosthesis in 9 (26.4%) patients, and subxiphoid in 16 (48.2%) patients. In one case, recurrence was due to rupture of the mesh at a supra-umbilical location, as detected on a CT scan and confirmed during subsequent hernia repair.
Table 1 provides information on the patients’ demographics and preoperative predictors of recurrence. All IHs were located in the midline and were classified as W3 (mean transverse and longitudinal defect diameters of 14.1 ± 3.7 cm and 24.4 ± 8.9 cm, respectively). Table 2 shows the operative and follow-up data related to recurrence. Five patients who completed the first 2 years of the follow-up did not attend subsequent follow-ups: two of these patients could not be contacted by phone, two other patients were re-operated by a laparotomy due to colon cancer, and one patient died after a brain stroke.
Complete fascial closure was feasible in all the patients. Sixty-four (16.8%) patients required a complementary second level of CST. The median operative time was 169 ± 42 min. Eighty (20.9%) patients had concurrent surgical procedures. In 24 patients, the enterotomy was unplanned. Abdominoplasties were performed in nine (2.2%) patients. Forty patients (10.4%) with severe comorbidities were admitted to the intensive care unit to ensure strict postoperative control for 24–48 h.
Comparing cohorts of patients under Level 1 and 2 of the CST, recurrence rates of 7.5% (23/317) versus 17.2% (11/64) were, respectively, reported. Patient characteristics and comparative analysis of both levels are shown in Table 3. The average transverse defect diameter of the hernia defect and hospital length of stay were significant in the univariate analysis, although they were not predictive factors comparing both approaches.
Surgical site-related complications postsurgery using the CST included seromas (20.8%), hematomas (9.5%), skin necrosis (7.4%), and wound infections (9.5%). Surgical debridement (n = 11; 2.8%) and negative pressure therapy (NPWT) (n = 34; 8.9%) were used. Other complications related to surgical repair included small bowel fistulas (n = 3; 0.7%) and mesh infections (n = 9; 2.3%). Re-operations for prosthesis excision were required in six of the nine (66.6%) mesh infection cases.
According to the multivariate analysis, a BMI > 30 (OR 2.20, CI 1.10–3.91, p = 0.031), steroid or immunosuppressive drug use (OR 1.06, CI 1.48–2.75, p = 0.003), and wound infections (OR 2.9; CI 1.53–4.01, p = 0.002) were predictors of recurrence after the CST. There was no difference in recurrence rate according to repairs of primary and recurrent hernias, smoking, COPD, diabetes, or urgent repair.
One patient with COPD developed abdominal compartment syndrome (bladder pressure = 28 mm Hg) requiring decompressive laparotomy and expired on postoperative day 6 due to respiratory distress syndrome. The average hospital length of stay was 9.6 days (range 6–18). Twenty-eight (82.3%) patients with hernia recurrence underwent additional AWHR, including posterior component separation with transversus abdominis release (TAR). Six (17.6%) patients refused additional repair surgery due to absence of symptoms or advanced age.
Discussion
Although the frequency of hernia recurrence after the CST is variable [5, 7, 8, 12, 14], the timing to recurrence has been relatively well documented, with the greatest number of them occurring within the first 3 postoperative years [15]. In the present study, recurrences occurred after a mean of 19.4 months (range 3–48): 29% within the first year following repair and 71% by the end of the third year. Identical results have been reported by other groups [11, 16].
When assessing recurrence, it is important to distinguish between clinical and radiological recurrences and to take into account the anticipated increase in recurrence rates with long follow-up periods. A minimum follow-up of at least of 5 years to prevent significant underestimation of these rates is advocated [16]. A CT scan should also be performed at the end of the follow-up period to confirm hernia absence of recurrence [10]. In our study, in terms of hernia recurrence sites, the most frequent location was subxiphoid (48.2%), as confirmed clinically and radiologically. This finding may be due to less gain achieved in subxiphoid and subcostal areas during the application of the CST, as reported in previous studies [14, 17]. Therefore, these areas may be under excessive tension, which causes recurrence in the long term.
In our multivariate analysis, a BMI of > 30 was a predictor of recurrence using the CST. Obesity is most likely only an indirect risk factor, although if it is related to wound infection can cause hernia recurrence, especially after a midline incision [18,19,20]. The findings of our study are comparable with those in the literature. Mittermair et al. estimated recurrence to be 2.3 times more likely in obese patients than nonobese patients [21]. Other authors postulated that increased intra-abdominal pressure may lead to weakened tissues and expansion of hernia defects, particularly in patients with central obesity [11, 16, 19]. Similarly, increased intra-abdominal pressure makes it more difficult to reduce the hernia contents, leading to higher rates of incarceration [22, 23]. Therefore, we believe that a preoperative protocol to address obesity is essential prior to surgery using the CST. Based on this protocol, the goal is for patients to achieve a preoperative BMI ≤ 30 in as short a time as possible. That’s the reason why some authors have suggested bariatric procedures to reduce the impact of morbid obesity on outcomes after AWHR. So, Kaminski et al. conclude that morbidly obese patients can be treated with a gastric restrictive procedure simultaneously with hernia repair to both decrease body weight and contribute to the control of ventral hernias [24].
According to our results, treatments with corticosteroids or immunosuppressive agents were predictors of recurrence. These findings are important due to the high incidence of repairs after organ transplantations [25]. Hernias following abdominal organ transplantation are of particular concern, as well as the use of immunosuppressive drugs postoperatively may increase their risk of IHs and the wound healing process. To achieve an overall reduction in the immune response, immunosuppressive agents may facilitate the development of biofilms, which are factors in the resistance of microorganisms to immune mechanisms [26].
Previous research reported that postoperative wound infections were directly associated with hernia recurrence [27]. In a number of studies, postoperative wound infection was strongly associated with late mesh failure and development of IHs [28, 29]. Bucknall et al. found that 48% of patients who developed IHs had postoperative wound infection, conferring a fivefold increase in the rate of IHs [30]. In our series, 8 of 34 (23.5%) patients with wound infections postsurgery experienced HI recurrence. In terms of the mechanism underlying the association of wound infections with hernia recurrence, an initial wound infection may seed the mesh, which then acts as a biofilm, potentially weakening the mesh and predisposing it to later failure or the eventual need for mesh removal [26].
In our study, a combination of antibiotics and drainage, with or without NPWT, was effective in 30 patients. Previous studies concluded that NPWT was associated with low wound infection rates, as well as acceptable recurrence rates [27, 31]. Some research suggested that NPWT represented an acceptable procedure in these high-risk patients. The same study indicated that the prosthesis may not need to be removed for complete healing when NPWT was applied in patients with grade 3 hernias [32]. In our study, nine patients with mesh infections required re-operations for prosthesis explantation: six (66.6%) patients due to chronic biofilms and no response to conservative management and seven (77.5%) patients with hernia recurrence after partial or total mesh removal.
In our multivariate analysis, there was no difference in the recurrence rate among repairs of primary and recurrent hernias, smoking, COPD, diabetes, urgent repair, operative time, type of prosthesis, levels 1 or 2 of CST, and concomitant procedures, even planned or unplanned enterotomies. Significantly, seroma and hematoma, variables related “per se” to the CST, were also not significant factors. This low incidence compared to wound infection rate may be due to the attempt to avoid excessive subcutaneous dissection, the use and maintenance of abdominal drains, and the closure of deep subcutaneous tissue in several planes to avoid these postoperative complications. Likewise, the use of the prosthesis in the modified technique compared to the original CST and the long experience of our group on this approach as a reference center have contributed to the reduction of these local complications.
Recurrence after surgery using the CST is problematic because external abdominal oblique release has already been performed to re-establish the original orientation of the rectus muscles. Thus, TAR may be the best approach in these cases. Previous studies on AWHR with TAR reported equivalent fascial closure rates to those obtained using the conventional CST, indicating similar myofascial advancement using the two techniques [33,34,35]. In our study, we performed TAR in 28 patients, with acceptable functional and esthetic results. Thus far, there have been no cases of recurrence detected in follow-up visits. TAR could have been performed in many patients in our study. Our department began to adopt this technique after its introduction at the end of 2012, with subsequent uptake of the technique in the surgical community. However, this was after completion of the present study.
Our study has some limitations. The retrospective chart review was limited by the information in the patients’ medical records, as well as possible observer bias of the reviewers. In addition, although our follow-up period was sufficient, five patients did not complete the study. The strengths of our study include the homogeneity of our outcomes, as all the procedures were performed by five hernia surgeons, therefore decreasing errors due to lack of experience or different applications of the CST. Future prospective studies should examine causal pathways in more detail. It would be interesting for long-term follow-up studies to investigate predictive factors in comparative studies that included endoscopic techniques and conventional and posterior CSTs.
In conclusion, the CST with mesh was effective in managing large IHs, especially in midline defects, with an acceptable recurrence rate. Obesity (BMI > 30), steroid or immunosuppressive drug use, and postoperative wound infections were predictors of recurrence after hernia surgery performed using the CST.
References
Ramírez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86:519–526
Ross SW, Oommen B, Huntington C et al (2015) National outcomes for open ventral hernia repair techniques in complex abdominal wall reconstruction. Am Surg 81:778–785
Moore M, Bax T, MacFarlane M et al (2008) Outcomes of the fascial component separation technique with synthetic mesh reinforcement for repair of complex ventral incisional hernias in the morbidly obese. Am J Surg 195:575–579
Torregrosa-Gallud A, Sancho Muriel J, Bueno-Lledó J et al (2017) Modified components separation technique: experience treating large, complex ventral hernias at a University Hospital. Hernia 21:601–608
Hultman CS, Clayton JL, Kittinger BJ et al (2014) Learning curves in abdominal wall reconstruction with components separation: one step closer toward improving outcomes and reducing complications. Ann Plast Surg 72:126–131
Diamond S, Cryer HG (2015) Revising recommendations and outcome measurements after complex open abdominal wall reconstruction. Am Surg 81:955–960
O’Halloran EB, Barwegen CJ, Dombrowski J et al (2014) Can’t have one without the other: component separation plus mesh for repairing difficult incisional hernias. Surgery 156:894–899
Wink JD, Wes AM, Fischer JP et al (2015) Risk factors associated with early failure in complex abdominal wall reconstruction: a 5 year single surgeon experience. J Plast Surg Hand Surg 49:77–82
Langer C, Schaper A, Liersch T et al (2005) Prognosis factors in incisional hernia surgery: 25 years of experience. Hernia 9:16–21
Hesselink VJ, Luijendijk RW, De Wilt JH et al (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
Vidovic D, Jurisic D, Franjic BD et al (2006) Factors affecting recurrence after incisional hernia repair. Hernia 10:322–325
Ko JH, Wang EC, Salvay DM et al (2009) Abdominal wall reconstruction: lessons learned from 200 “components separation” procedures. Arch Surg 144:1047–1055
Muysoms FE, Miserez M, Berrevoet F et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414
Reilingh DV, van Goor H, Rosman C et al (2003) Components separation technique” for the repair of large abdominal wall hernia. J Am Coll Surg 196:32–37
Anthony T, Bergen PC, Kim LT et al (2000) Factors affecting recurrence following incisional herniorrhaphy. World J Surg 24:95–100
Ríos A, Rodriguez JM, Munitiz V et al (2001) Factors that affect recurrence after incisional herniorrhaphy with prosthetic material. Eur J Surg 167:855–859
Sneiders D, Yurtkap Y, Kroese LF et al (2019) Anatomical study comparing medialization after Rives-Stoppa, anterior component separation, and posterior component separation. Surgery. https://doi.org/10.1016/j.surg.2018.11.013
Desai KA, Razavi SA, Hart AM et al (2016) The effect of BMI on outcomes following complex abdominal wall reconstructions. Ann Plastic Surg 76:295–297
Tastaldi L, Krpata DM, Prabhu AS et al (2019) The effect of increasing body mass index on wound complications in open ventral hernia repair with mesh. Am J Surg 218(3):560–566
Winfield RD, Reese S, Bochicchio K et al (2016) Obesity and the risk for surgical site infection in abdominal surgery. Am Surg 82:331–336
Mittermair R, Sucher R, Perathoner A (2014) Results and complications after laparoscopic sleeve gastrectomy. Surg Today 44:1307–1312
Lau B, Kim H, Haigh PI et al (2012) Obesity increases the odds of acquiring and incarcerating non-inguinal abdominal wall hernias. Am Surg 78:1118–1121
Eid GM, Wikiel KJ, Entabi F et al (2013) Ventral hernias in morbidly obese patients: a suggested algorithm for operative repair. Obes Surg 23:703–709
Chandeze MM (2019) Ventral hernia surgery in morbidly obese patients, immediate or after bariatric surgery preparation: results of a case-matched study. Surg Obes Relat Dis 15(1):83–88. https://doi.org/10.1016/j.soard.2018.09.490
Gillion JF, Palot JP (2012) Abdominal wall incisional hernias: infected prosthesis: treatment and prevention. J Visc Surg 149:20–31
Bueno-Lledó J, Torregrosa-Gallud A, Sala-Hernandez A et al (2016) Predictors of mesh infection and explantation after abdominal wall hernia repair. Am J Surg 30:243–247
Rodriguez-Unda N, Soares KC, Azoury SC et al (2015) Negative-pressure wound therapy in the management of high-grade ventral hernia repairs. J Gastrointest Surg 19:2054–2061
Danzig MR, Stey AM, Yin SS et al (2016) Patient profiles and outcomes following repair of irreducible and reducible Ventral Wall Hernias. Hernia 20:239–247
Holihan JL, Alawadi Z, Martindale RG et al (2015) Adverse events after ventral hernia repair: the vicious cycle of complications. J Am Coll Surg 221:478–485
Bucknall TE (1993) Factors influencing wound complications: a clinical and experimental study. Ann R Coll Surg Engl 65:71–77
Gassman A, Mehta A, Bucholdz E et al (2015) Positive outcomes with negative pressure therapy over primarily closed large abdominal wall reconstruction reduces surgical site infection rates. Hernia 19:273–278
Swanson EW, Cheng HT, Susarla SM et al (2016) Does negative pressure wound therapy applied to closed incisions following ventral hernia repair prevent wound complications and hernia recurrence? A systematic review and meta-analysis. Plast Surg 24:113–118
Gibreel W, Sarr MG, Rosen M et al (2016) Technical considerations in performing posterior component separation with transverse abdominis muscle release. Hernia 20:449–459
Jones CM, Winder JS, Potochny JD et al (2016) Posterior component separation with transversus abdominis release: technique, utility, and outcomes in complex abdominal wall reconstruction. Plast Reconstr Surg 137:636–646
Pauli EM, Wang J, Petro CC et al (2015) Posterior component separation with transversus abdominis release successfully addresses recurrent ventral hernias following anterior component separation. Hernia 19:285–291
Acknowledgements
We would like to thank Providencia Garcia-Pastor and Victoria Pareja of our surgical group for their helpful discussions.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare no disclosures relevant to this article or research. Drs. Bueno-Lledó, Bonafé, Carbonell, Torregrosa and Pous-Serrano have no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bueno-Lledó, J., Bonafe-Diana, S., Carbonell-Tatay, F. et al. Component separation and large incisional hernia: predictive factors of recurrence. Hernia 25, 1593–1600 (2021). https://doi.org/10.1007/s10029-021-02489-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02489-3