Abstract
Purpose
Synthetic non-absorbable mesh is used for elective inguinal hernia repair but is not commonly used for incarcerated or strangulated inguinal hernia requiring enterectomy to reduce the risk of surgical-site infection. This study aimed to evaluate the safety of synthetic non-absorbable mesh repair in patients with incarcerated or strangulated inguinal hernia requiring enterectomy versus non-mesh repair.
Methods
We analyzed patients with incarcerated or strangulated inguinal hernia with enterectomy from April 2012 to March 2017 using a nationwide inpatient database in Japan. We conducted overlap propensity score-weighted analyses to compare surgical-site infection (SSI), duration of anesthesia, antibiotic use at > 3 days after surgery, postoperative hospital stay, and 30 day readmission. Two sensitivity analyses were performed. First, we compared the proportions of patients requiring wound culture at ≥ 3 days after surgery. Second, we performed overlap propensity score-weighted logistic regression analyses for surgical-site infection.
Results
We identified 668 eligible patients, comprising 223 patients with mesh repair and 445 with non-mesh repair. Overlap propensity score-weighted analyses showed no significant differences between the mesh repair and non-mesh repair groups for SSI (2.5 vs. 2.8%, P = 0.79). Secondary outcomes did not differ significantly between the groups. Proportion of wound culture at ≥ 3 days after surgery was similar in the two groups (11.1 vs. 14.6%, P = 0.18). Logistic regression analysis showed no significant association between mesh repair and SSI (odds ratio, 0.93; 95% confidence interval, 0.34–2.57).
Conclusion
Synthetic non-absorbable mesh use may be safe for incarcerated or strangulated inguinal hernia requiring enterectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is one of the most common surgeries. As the first tension-free repair, the Lichtenstein technique was published in 1989 [1]. Currently, tension-free repair using synthetic non-absorbable mesh is the most common open repair. Although prevention of inguinal hernia recurrence is a primary objective in elective hernia repair, early recovery of intestinal function and prevention of infection are important in emergency surgery for incarcerated or strangulated inguinal hernia. Traditionally, non-mesh repair has been used for incarcerated or strangulated inguinal hernia requiring bowel resection. The safety of synthetic non-absorbable mesh for inguinal hernia surgery requiring bowel resection remains to be established, although mesh repair is sometimes selected in recent times.
Studies on surgical-site infection after mesh repair and non-mesh repair have been limited by their small sample sizes. Previous reports using single-center data showed similar incidence of surgical-site infection between mesh repair and non-mesh repair groups among patients with incarcerated hernia [2,3,4]. Furthermore, mesh repair was reported to reduce hospital stay [2]. In contrast, mesh repair was associated with higher incidence of surgical-site infection than non-mesh repair in another report [5].
Some incarcerated hernias require bowel resection while others do not. However, the previous studies mixed patients with and without bowel resection. In addition, the patient characteristics differed between the groups. Because the previous reports used single-center data with less than about 100 cases, generalizable data are lacking for the safety of synthetic non-absorbable mesh use for incarcerated inguinal hernia requiring bowel resection.
In this study, we aimed to evaluate the short-term safety of mesh repair in patients with emergency hernia repair requiring bowel resection by comparing postoperative infection between mesh repair and non-mesh repair.
Methods
Using the diagnosis procedure combination database in Japan, we extracted data for patients with incarcerated or strangulated inguinal hernia who required emergency admission and underwent open hernia repair on the day of admission or following day between April 2012 and March 2017. The database contains administrative claims and discharge data for approximately 8 million patients per year from more than 1,200 hospitals. All university hospitals in Japan are required to participate in the database, while participation by community hospitals is voluntary. The database includes the following information: hospital identifiers; age; sex; height; weight; diagnoses, comorbidities, and complications recorded with Japanese text data and International classification of diseases, tenth revision (ICD-10) codes [6]; procedures recorded with Japanese original codes; and discharge status. Details of the database were reported elsewhere [7, 8]. Patients were categorized into four groups according to body mass index (< 18.5, 18.5–24.9, 25.0–29.9, and ≥ 30.0 kg/m2) and three groups according to smoking index (0, 1–49, and ≥ 50 pack-years). Diabetes was defined as conditions requiring medications for diabetes treatment, including insulin and oral hypoglycemic agents. Catecholamine administration was defined as use of catecholamines before or on the day of surgery. We calculated the Charlson comorbidity index and summed the ICD-10 codes for 17 comorbidities based on Quan’s protocol [9]. Type of hospital was classified into teaching hospital or non-teaching hospital.
The primary outcome was incidence of surgical-site infection. We defined surgical-site infection as ICD-10 codes T793, T813, T814, and T941. The secondary outcomes were duration of anesthesia, antibiotic use at > 3 days after surgery, postoperative hospital stay and readmission within 30 days.
Patients with the following factors were excluded: non-emergency admission, interval from admission to surgery > 2 days, peritonitis on admission, pneumonia on admission, or missing data. The need for informed consent was waived for this study because of the anonymous nature of the data. Study approval was obtained from the Institutional Review Board at the University of Tokyo.
Statistical analysis
Overlap propensity score weighting
We conducted overlap propensity score weighting. Propensity scores for mesh repair were estimated from a generalized estimating equation model fitted with multivariable logistic regression analysis, after adjustment for sex, age, body mass index, smoking index, diabetes, Charlson comorbidity index, Barthel index, and hospital type to account for clustering of patients within hospitals. Overlap weighting involves weighting patients with the predicted probability of receiving opposite treatment. One feature of this method is that extreme weights are impossible because weights are calculated between 0 and 1 [10,11,12]. This method has some advantages over conventional propensity score methods, such as matching or inverse probability weighting, with respect to target population, balance, and precision. The created target population mimics the cohort of a randomized control trial without excluding patients from the original cohort. Overlap weighting achieves exact balance in measured variables and optimizes precision of the estimated association between treatment and outcome among other propensity score methods including inverse probability weighting and matching [13, 14]. An absolute standardized difference < 0.1 was considered to denote a negligible difference between the two groups [15].
We performed two sensitivity analyses for the results of surgical-site infection. First, we compared the proportions of patients who required wound culture at ≥ 3 days after surgery. Second, we performed overlap propensity score-weighted logistic regression analyses for surgical-site infection adjusted for the same variables used to estimate the propensity scores, in which the pseudo-population created by the overlap propensity score weighting was regressed by the variables [10]. The chi-square test was used to compare categorical variables. For continuous variables, Student’s t test was used. The significance level was set at P < 0.05 for all statistical analyses, and all P values were two-sided. All statistical analyses were conducted using Stata/MP™ version 15.0 (StataCorp, College Station, TX).
Results
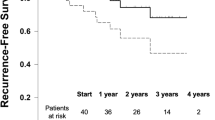
We extracted data for 934 patients who were admitted to hospital with incarcerated or strangulated inguinal hernia and underwent open hernia repair with enterectomy during the study period. We excluded the following patients: non-emergency admission (n = 25), interval from admission to surgery > 2 days (n = 54), peritonitis on admission (n = 88), pneumonia on admission (n = 34), and missing data (n = 65). As a result, we identified 668 eligible patients, comprising 223 patients who underwent mesh repair and 445 patients who underwent non-mesh repair (see Fig. 1).
Table 1 shows the characteristics of the patients with incarcerated or strangulated inguinal hernia treated with mesh repair and non-mesh repair. Before adjustment, there were significant imbalances in sex, age, Charlson comorbidity index, and catecholamine administration between the two groups (absolute standardized difference > 0.1). The proportion of female patients was lower in the mesh repair group than in the non-mesh repair group (17.5 vs. 23.1%). The proportion of patients aged ≤ 40 years was larger in the mesh repair group than in the non-mesh repair group (7.2 vs. 4.0%). The proportion of patients aged ≥ 80 years was the largest in both groups (36.3 vs. 33.7%). More than half of the patients had body mass index of 18.5–24.9 kg/m2 in both groups (67.7 vs. 70.8%). The proportion of patients who required catecholamine administration was lower in the mesh repair group than in the non-mesh repair group (53.4 vs. 61.1%). After adjustment by overlap propensity score weighting, the absolute standardized differences for all variables were < 0.1.
Table 2 shows the outcomes of the two groups before and after adjustment by overlap propensity score weighting. Before adjustment, the incidence of surgical-site infection was similar between the two groups (2.7 vs. 3.4%, P = 0.63). The duration of anesthesia was similar between the mesh repair and non-mesh repair groups (193.1 vs 192.2 min, respectively; P = 0.88). The proportion of antibiotic use at > 3 days after surgery was lower in the mesh repair group than in the non-mesh repair group (53.4 vs 63.4%, respectively; P = 0.01). Comparing the mesh repair group with the non-mesh repair group, respectively, postoperative hospital stay was similar (16.1 vs. 18.4 days, P = 0.19); the proportion of readmission within 30 days did not differ significantly (12.1 vs. 12.4%, P = 0.93); after adjustment, the incidence of surgical-site infection was similar (2.5 vs. 2.8%, P = 0.79); postoperative hospital stay was similar (16.5 vs. 18.0 days, P = 0.34); the duration of anesthesia was similar (193.4 vs 189.6 min; P = 0.88); the proportion of antibiotic use at > 3 days after surgery did not differ significantly (54.9 vs 62.3%; P = 0.056); and the proportion of readmission within 30 days was similar (12.0 vs. 12.5%, P = 0.86). In the sensitivity analyses, the proportion of patients who required wound culture ≥ 3 days after surgery was similar between the mesh repair and non-mesh repair groups (11.1 vs. 14.6%, respectively; P = 0.18). The overlap propensity score-weighted logistic regression analysis for surgical-site infection showed that the odds ratio (95% CI) for mesh use was 0.93 (0.34–2.57).
Discussion
In this study, we conducted overlap propensity score weighting using a nationwide inpatient database to compare the incidence of surgical-site infection between mesh repair and non-mesh repair for incarcerated or strangulated inguinal hernia requiring bowel resection. The incidence of surgical-site infection did not differ significantly or clinically between the mesh repair and non-mesh repair groups. Postoperative hospital stay and readmission within 30 days were similar in both groups. The multivariable regression analysis did not show an association between mesh repair and surgical-site infection. We excluded patients with non-emergency admission or with an interval from admission to surgery of > 2 days because these patients might have undergone reduction of an incarcerated hernia, receiving elective hernia repair with enterectomy. We believe emergent hernia repair is quite different from elective repair regarding preoperative and postoperative care. We also excluded patients with peritonitis on admission to exclude patients with contaminated wounds. Finally, we excluded patients with pneumonia on admission because duration of hospital stay may have been determined by pneumonia.
Our study showed that the incidence of surgical-site infection in the mesh repair and non-mesh repair groups was 2.5% and 2.8%, respectively, with no significant or clinical difference between the two groups. A prospective cohort study showed no surgical-site infection among 12 incarcerated inguinal hernia patients who underwent mesh repair with enterectomy [16]. Other prospective cohort studies showed no surgical-site infection in 42 and 32 patients requiring bowel resection [17, 18]. In a further study, despite an incidence of surgical-site infection as high as 20% after mesh repair with enterectomy, no significant difference was seen between the mesh repair and non-mesh repair groups [19]. Additionally, a meta-analysis involving two retrospective studies showed no association with surgical-site infection between the two groups [20]. A recent single-center study of 257 patients showed that mesh use was not associated with increased incidence of surgical-site infection [2]. However, the findings for all of these studies are difficult to generalize because of their small sample sizes and single-center designs. The results of the present study on surgical-site infection were consistent with those in the previous studies and are generalizable because the study used a nationwide database and included > 600 patients.
Some previous reports discussed the safety of mesh repair in incarcerated or strangulated hernia by mixing groin hernias (inguinal and femoral) and ventral hernias [18, 21, 22]. However, we believe that these hernias should be distinguished before analysis. In the present study, we identified only incarcerated or strangulated inguinal hernia requiring enterectomy to determine the safety of mesh use for inguinal hernia repair.
Previous studies showed longer postoperative hospital stay in the non-mesh repair group compared with the mesh repair group [2, 23]. The differences in hospital stay between the groups in these previous studies may be due to differences in postoperative pain. Non-mesh repair is usually associated with more severe pain than mesh repair [24]. However, in the present study, postoperative hospital stay did not differ significantly between the two groups. This may be explained by the difference in severity of incarcerated or strangulated hernias between the previous studies and the present study. The previous studies included patients with and without bowel resection, while the present study included only patients with bowel resection. The length of hospital stay may have been determined by intestinal function or oral intake after surgery in the present study.
In this this study, we used a Japanese nationwide database; more than 80% of the patients had a body mass index < 25 kg/m2; a small number had a body mass index of ≥ 30 kg/m2. Obesity is a reported risk factor for surgical-site infection after ventral hernia repair [25]. Care should be taken when interpreting the results of this study in a Western population, in which the proportion of obese and overweight patients is higher than in Japan.
Before adjustment, the proportion of catecholamine use was higher in the non-mesh repair group. It is plausible that surgeons hesitated to use foreign body implantation in patients with unstable vital signs requiring catecholamines before surgery. However, even after minimizing selection bias by overlap weighting, the rates of surgical-site infection and wound culture at ≥ 3 days after surgery did not differ significantly between mesh repair and non-mesh repair. This suggests that mesh repair itself was not associated with increased surgical-site infection rates.
The Centers for Disease Control and Prevention defined surgical-site infection as infection occurring within 30 days after surgery [26]. Readmission within 30 days was similar between the mesh repair and non-mesh repair groups in the present study. This result supports the notion that the disease severity was similar between the two groups and that the incidence of complications including surgical-site infection requiring readmission was similar between the two groups.
The present study has several limitations. First, the database did not have data on wound classification. Thus, our study included patients with clean-contaminated or contaminated wounds. If the strangulated bowel was necrotic or massive spillage was observed during surgery, the wound class was contaminated [27]. There was a possibility of imbalance regarding wound classification (severe local contamination) between the two groups; however, we reduced the selection bias as much as possible by excluding patients with apparent dirty wound classification (peritonitis) before surgery. Essentially, even if the incarcerated bowel was strangulated, the wound class was clean-contaminated as long as the bowel was not necrotic. Second, the details of the techniques were unknown, such as the layers in which the mesh was placed, the type of implanted mesh, surgeon’s experience, and what types of non-mesh repairs were performed (e.g., Bassini, Lichtenstein, Rutkow–Robbins). However, these details were not confounders in the present study. Third, there may have been unmeasured confounders, such as postoperative drain placement, although no imbalance was seen in the measured factors between the two groups. Finally, data on long-term outcomes, such as late infection or hernia recurrence, were lacking.
In conclusion, synthetic non-absorbable mesh repair for incarcerated inguinal hernia was not associated with higher incidence of short-term surgical-site infection compared with non-mesh repair. Permanent mesh placement at the time of enterectomy did not result in different short-term infection rates between mesh vs non-mesh repair. It may be reasonable to select mesh repair for incarcerated or strangulated inguinal hernias regarding the short-term safety. Further studies investigating the probability of long-term mesh infection and the recurrence rate are needed to justify permanent mesh placement after enterectomy.
Availability of data and material
The datasets analyzed during the current study are not publicly available due to contracts with the hospitals providing data to the database.
References
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157(2):188–193
Tastaldi L, Krpata DM, Prabhu AS, Petro CC, Ilie R, Haskins IN, Alkhatib H et al (2019) Emergent groin hernia repair: a single center 10-year experience. Surgery 165(2):398–405
Venara A, Hubner M, Le Naoures P, Hamel JF, Hamy A, Demartines N (2014) Surgery for incarcerated hernia: short-term outcome with or without mesh. Langenbecks Arch Surg 399(5):571–577
Sawayama H, Kanemitsu K, Okuma T, Inoue K, Yamamoto K, Baba H (2013) Safety of polypropylene mesh for incarcerated groin and obturator hernias: a retrospective study of 110 patients. Hernia 18(3):399–406
Xourafas D, Lipsitz SR, Negro P, Ashley SW, Tavakkolizadeh A (2010) Impact of mesh use on morbidity following ventral hernia repair with a simultaneous bowel resection. Arch Surg 145(8):739–744
International Classification of Diseases (ICD) Tenth Revision. http://apps.who.int/classifications/icd10/browse/2016/en. Accessed 1 Mar 2020.
Yasunaga H (2019) The diagnosis procedure combination database. Ann Clin Epidemiol 1(3):76–79
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H (2017) Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 27(10):476–482
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, Saunders LD et al (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139
Mehta N, Kalra A, Nowacki AS, Anjewierden S, Han Z, Bhat P, Carmona-Rubio AE et al (2020) Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol 5(9):1020–1026
Desai RJ, Franklin JM (2019) Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ 367:l5657
Li F, Thomas LE (2018) Addressing extreme propensity scores via the overlap weights. Am J Epidemiol 188(1):250–257
Thomas LE, Li F, Pencina MJ (2020) Overlap weighting: a propensity score method that mimics attributes of a randomized clinical trial. JAMA 323(23):2417–2418
Li F, Morgan KL, Zaslavsky AM (2017) Balancing covariates via propensity score weighting. J Am Stat Assoc 113(521):390–400
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28(25):3083–3107
Atila K, Guler S, Inal A, Sokmen S, Karademir S, Bora S (2008) Prosthetic repair of acutely incarcerated groin hernias: a prospective clinical observational cohort study. Langenbecks Arch Surg 395(5):563–568
Bessa SS, Abdel-fattah MR, Al-Sayes IA, Korayem IT (2015) Results of prosthetic mesh repair in the emergency management of the acutely incarcerated and/or strangulated groin hernias: a 10-year study. Hernia 19(6):909–914
Topcu O, Kurt A, Soylu S, Akgol G, Atabey M, Karakus BC, Aydin C (2013) Polypropylene mesh repair of incarcerated and strangulated hernias: a prospective clinical study. Surg Today 43(10):1140–1144
Ueda J, Nomura T, Sasaki J, Shigehara K, Yamahatsu K, Tani A, Shioda Y et al (2012) Prosthetic repair of an incarcerated groin hernia with small intestinal resection. Surg Today 42(4):359–362
Hentati H, Dougaz W, Dziri C (2014) Mesh repair versus non-mesh repair for strangulated inguinal hernia: systematic review with meta-analysis. World J Surg 38(11):2784–2790
Lin YT, Weng TY, Tam KW (2020) Effectiveness and safety of mesh repair for incarcerated or strangulated hernias: a systematic review and meta-analysis. World J Surg 44(7):2176–2184
Nieuwenhuizen J, van Ramshorst GH, ten Brinke JG, de Wit T, van der Harst E, Hop WCJ, Jeekel J et al (2011) The use of mesh in acute hernia: frequency and outcome in 99 cases. Hernia 15(3):297–300
Papaziogas B, Lazaridis C, Makris J, Koutelidakis J, Patsas A, Grigoriou M, Chatzimavroudis G et al (2005) Tension-free repair versus modified Bassini technique (Andrews technique) for strangulated inguinal hernia: a comparative study. Hernia 9(2):156–159
Grant AM, Collaboration EHT (2002) Open mesh versus non-mesh repair of groin hernia meta-analysis of randomized trials leased on individual patient data. Hernia 6(3):130–136
Park H, de Virgilio C, Kim DY, Shover AL, Moazzez A (2020) Effects of smoking and different BMI cutoff points on surgical site infection after elective open ventral hernia repair. Hernia 25:337–343
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, Reinke CE et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8):784–791
Birindelli A, Sartelli M, Di Saverio S, Coccolini F, Ansaloni L, van Ramshorst GH, Campanelli G et al (2017) 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg 12(1):37
Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (19AA2007 and H30-Policy-Designated-004) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (17H04141).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This study was approved by the Institutional Review Board of The University of Tokyo [approval number: 3501-(3) (December 25th, 2017)]. Because all data were de-identified, the requirement for patient informed consent was waived.
Human and animal rights
The need for informed consent was waived for this study because of the anonymous nature of the data. Study approval was obtained from the Institutional Review Board at the University of Tokyo.
Consent to participate
The requirement for informed consent was waived because of the anonymous nature of the data.
Consent for publication
All authors have approved the manuscript and meet the requirements for authorship.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sakamoto, T., Fujiogi, M., Ishimaru, M. et al. Comparison of postoperative infection after emergency inguinal hernia surgery with enterectomy between mesh repair and non-mesh repair: a national database analysis. Hernia 26, 217–223 (2022). https://doi.org/10.1007/s10029-021-02439-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02439-z