Abstract
Background
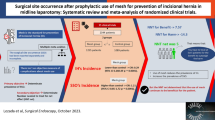
Hernia repair with mesh in patients with incarcerated or strangulated hernias is controversial. Moreover, the use of mesh for hernia repair with concomitant bowel resection poses a great dilemma. This study compared the outcomes of mesh and anatomic repairs in patients with acutely incarcerated or strangulated hernias.
Methods
PubMed, Embase, and Cochrane databases were searched for studies published before November 2019. Randomized controlled trials (RCTs) and prospective studies were included. We conducted meta-analyses using a random-effects model. The treatment outcome was measured by the incidence of surgical site infection (SSI), seroma formation, and hernia recurrence postoperatively.
Results
Two RCTs and six prospective studies with 978 patients were included. No significant difference in SSI incidence was observed between patients with incarcerated hernia from the mesh and anatomic repair groups. Recurrence was significantly lower in mesh repair group than in anatomic repair group (odds ratio, 0.08; 95% confidence interval, 0.01–0.45). Only two patients needed to have mesh explantation due to mesh infection. In the setting of hernia repair with concomitant bowel resection, the SSI rate with mesh repair was slightly higher, but most cases of infections were well controlled with conservative antibiotic therapy.
Conclusions
Mesh repair for incarcerated or strangulated hernias was feasible with a great benefit of lower recurrence rates. However, due to limited data, drawing conclusions regarding the use of mesh for hernia repair with concomitant bowel resection was difficult. Further studies with preset criteria for evaluating patients undergoing concomitant bowel resection may help elucidate this issue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hernia repair with mesh has become a standard procedure and is recommended for patients with symptomatic hernia to achieve less postoperative pain, lower complication rates, and lower recurrence rates [1]. However, mesh repair for incarcerated or strangulated hernias is still controversial. Some studies have indicated that in contaminated surgical fields, surgical site infections (SSIs) and complications increase with implanted mesh [2] while others revealed that synthetic mesh repair in patients with clean-contaminated wounds is associated with lower recurrence rates and similar postoperative infection rates compared with anatomic repair methods [3].
Some current reviews have reported an acceptable infection rate and fewer recurrences after mesh repair in patients with incarcerated hernia, but evidence supporting recommendation of mesh repair with concomitant bowel resection remains insufficient [4]. Moreover, previous reviews included retrospective data, which means that a high risk of bias should be considered [5,6,7]. Therefore, we conducted a systematic review and meta-analysis of current evidence to evaluate the outcomes and safety of mesh repair compared with anatomic repair in patients with acutely incarcerated or strangulated hernias.
Materials and methods
Inclusion and exclusion criteria
Randomized controlled trials (RCTs) and prospective studies were incorporated into the analysis. To be eligible, studies had to meet the following conditions: (1) included patients with strangulated or incarcerated hernias of ventral, umbilical or groin types; (2) evaluated the outcomes of mesh versus anatomic repair or mesh repair with or without bowel resection; (3) clearly reported the inclusion criteria of study participants; (4) described surgical procedures of hernia repair; and (5) assessed events of SSI, seroma, or hernia recurrence in mesh versus anatomic repair or mesh repair with or without concomitant bowel resection. Exclusion criteria were (1) patients with concomitant surgical procedures of abdominal repair, for instance, hiatal or parastomal hernia repair; (2) no available data regarding incidence of SSI or recurrence; or (3) studies with overlapping cohorts.
Literature search strategy
The PubMed, Embase, and Cochrane Library databases were searched. The search was performed using the Medical Subject Headings (MeSH): hernia OR hernia repair OR herniorrhaphy OR hernioplasty, incarcerated OR incarceration OR strangulated OR strangulation, mesh OR prosthetic and groin OR ventral OR inguinal OR abdominal OR incisional OR umbilical OR paraumbilical. Additionally, a hand-search of the references of review articles, previous meta-analyses, and key articles was also performed. No language restrictions were applied. The final search was performed in 2 November 2019. This systematic review has been accepted by the PROSPERO registry (CRD42018090151).
Data extraction
Two reviewers (YTL and TYW) independently extracted the following data. The study characteristics, types of interventions, surgical procedures, SSI rates, hernia recurrence rates, and perioperative parameters were extracted. Disagreements were resolved by a third reviewer (KWT).
Methodological quality appraisal
Two reviewers (YTL and TYW) independently assessed the methodological quality of each study by using the revised Cochrane Risk of Bias (RoB 2.0) tool for RCTs [8] and the Risk of Bias in Nonrandomized Studies of Interventions tool for prospective studies [9]. Several domains were assessed, including selection, performance, detection, attrition, reporting, and other biases in RCTs, as well as preintervention, peri-intervention, postintervention, and overall bias in prospective studies.
Outcomes and statistical analysis
The primary outcome was SSI incidence. Secondary outcomes were incidence of hernia recurrence, seroma, and postoperative mortality.
All meta‐analyses were performed with Review Manager version 5 software (Cochrane Collaboration, Oxford, UK). The meta-analysis was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [10]. Results of analysis of dichotomous outcomes were expressed as odds ratios (ORs), with 95% confidence intervals (CIs) estimated using the DerSimonian and Laird random-effects model [11].
The Cochrane’s Q and I2 test statistics were used to check the presence of observed difference between studies due to heterogeneity. A p value of <0.1 for Cochrane’s Q test was used to the heterogeneity, and the proportion of the total outcome variability was >50% based on the I2 test. Meta-analyses with subgroups were conducted according to the surgical strategy of the studies, either mesh repair or anatomic repair.
Results
Trial characteristics
The literature search generated a total of 523 records. A total of 212 duplicates were removed. Full-text screening resulted in exclusion of another 270 articles. The full texts of the remaining 41 reports were reviewed. Most of these were excluded from our final review for the following reasons: 13 enrolled different diseases, such as hiatal hernias, parastomal hernias, or ventral hernias with bowel obstruction by tumor; 7 discussed different topics concerning inguinal hernia, and 13 studies were excluded for being review articles. Finally, we selected two RCTs and six prospective studies (Fig. 1) [5,6,7, 12,13,14,15,16].
The two RCTs and six studies were published between 2007 and 2017. The sample sizes ranged from 42 to 234 patients, and overall, 978 patients were included. The mean age of the patients ranged from 34.6 to 75 years. Six included studies were conducted in Egypt [5,6,7, 13, 15, 16] and two were conducted in Turkey [12, 14]. All patients were diagnosed with incarcerated or strangulated hernias, including 552 inguinal, 61 femoral, 86 paraumbilical, 146 umbilical, 65 incisional, 6 epigastric, and 3 Spigelian hernias. All hernia repairs were performed as open procedures. Every patient received mesh repair for inguinal hernia using the Lichtenstein method. The mesh used in these studies was made of polypropylene material. Among the eight included studies, two RCTs and one prospective study compared mesh and anatomic repairs in patients with incarcerated hernia [7, 15, 16], and five studies evaluated mesh repair in patients with or without concomitant bowel resection [5, 6, 12,13,14]. In two of the three studies evaluating mesh and anatomic repairs, patients receiving concomitant bowel resection were equally distributed [15, 16]. Four studies reported the details of bowel resection, including 92 procedures involving the small intestine, 5 procedures involving the large intestine, and 2 procedures involving the small plus large intestines [5, 6, 12, 14]. All the meshes used in the eight studies we included were monofilament polypropylene meshes. Baseline characteristics and patient demographic data are listed in Table 1.
Table 2 presents a methodological quality summary of the included studies. One RCT had some concerns of allocation bias arising from the randomization process according to the patient’s odd or even registration number [16]. A risk with some concerns of performance bias was present for both included RCTs because of the awareness of participants’ assigned interventions during the trial [15, 16]. In two RCTs, no patient was lost to follow-up [15, 16]. Detection, attrition, and reporting biases were at low risk in both the RCTs. Among six prospective studies, three prospective studies had a serious risk of confounding bias during the preintervention period because of lack of adjustment for baseline comorbidity [5, 12, 14], and three prospective studies had a moderate risk of confounding bias because of insufficient adjustment for disease severity [6, 7, 13]. All six studies reported a low risk of bias during the intervention period for intervention classification [5,6,7, 12,13,14]. Two prospective studies had a moderate risk of deviations from intended interventions during the postintervention period due to differences in prophylactic antibiotic treatment [5, 12], and the study by Emile et al. had a moderate risk of deviations from intended interventions during the postintervention period due to imbalance of bowel resection patients between the mesh and anatomic repair groups [7]. Considering biases in the measurement or selection of reported results, all studies reported appropriate methods. Overall, four prospective studies had a moderate risk of bias, and two had a serious risk of bias (Table 2).
Mesh versus anatomic repair in patients with incarceration hernia
Surgical site infection
In three included studies, all patients received prophylactic antibiotics [7, 15, 16]. However, Elsebae et al. started the prophylactic ciprofloxacin orally only after the operation [16], and other studies used intravenous prophylactic antibiotics right before the surgery [7, 15]. Three studies reported SSI incidences of 7.02% (8 of 114) in the mesh repair group and 8.65% (9 of 104) in the anatomic repair group [7, 15, 16]. No significant difference in SSI rates was noted in the pooled data (OR 0.83; 95% CI 0.29–2.35) (Fig. 2). In studies only including ventral hernias repair, no significant difference in SSI rates was noted (OR 1.06; 95% CI 0.34–3.33) [7, 15]. Only one patient had mesh explantation due to resistant SSI [7].
Seroma
Regarding seroma formation, event rates of 16.67% (19 of 114) and 3.85% (4 of 104) in the mesh and anatomic repair groups, respectively, were reported in three studies [7, 15, 16]. The incidence of seroma formation was higher in the mesh repair group than in the anatomic repair group, and significant difference was noted (OR 4.14; 95% CI 1.48–11.6) (Fig. 2). In studies only including ventral hernias repair, the incidence of seroma formation was significantly higher in the mesh repair group than in the anatomic repair group (OR 4.02; 95% CI 1.35–11.98) [7, 15]. All cases of seroma formation were resolved with conservative treatment with no further complications.
Recurrence
Three studies reported recurrence rates of 0% (0 of 114) in the mesh repair group and 13.46% (14 of 104) in the anatomic repair group [7, 15, 16]. The recurrence rate was significantly lower in the mesh repair group than in the anatomic repair group (OR 0.08; 95% CI 0.01–0.45) (Fig. 2). In studies only including ventral hernias repair, the incidence of recurrence was significantly lower in the mesh repair group than in the anatomic repair group (OR 0.06; 95% CI 0.01–0.51) [7, 15].
Mortality
In three studies comparing mesh repair and anatomic repair, no deaths during follow-up were reported [7, 15, 16].
Hernia repair with mesh in patients with concomitant bowel resection
Surgical site infection
In the studies evaluating mesh repair in patients with or without bowel resection, SSI events were recorded in all five included studies [5, 6, 12,13,14]. SSI was defined as infection within 1 month postoperatively. All patients were started on prophylactic antibiotics right before the start of the operation. SSI incidence rates of 6.08% (9 of 148) in patients with concomitant bowel resection and 3.27% (20 of 612) in patients without concomitant bowel resection were reported (Table 3) [6, 12,13,14,15]. No major difference in SSI rates was reported between patients with versus without bowel resection, except in the study by Topcu et al., who reported a significantly higher SSI rate in patients treated with bowel resection [14]. Only one patient needed to have the mesh removed postoperatively due to mesh infection, and hernia patients with mesh repair had not received concomitant bowel resection [5].
Seroma
The incidence of seroma formation was evaluated in three of five studies, with rates of 5.88% (4 of 68) in patients with concomitant bowel resection and 0.68% (2 of 295) in patients without concomitant bowel resection [6, 12, 14]. In the pooled data, a significantly higher incidence of seroma formation was observed in patients with bowel resection [6, 12, 14] (Table 3). No deep infection resulting from seromas was recorded in all the three studies, and the seroma formation events were successfully treated with drainage or conservative treatment.
Recurrence
In five included studies, a 1.05% recurrence rate (8 of 760) was reported in hernia patients receiving mesh repair with and without concomitant bowel resection [5, 6, 12,13,14] (Table 3). Bessa et al. reported two recurrences (0.9%) in the total sample without providing individual rate of each group [5, 6, 12,13,14]. In four other studies, the recurrence rates were 0.86% (1 of 116) in patients with concomitant bowel resection and 1.22% (5 of 410) in patients without concomitant bowel resection [6, 12,13,14]. No recurrences were reported in two of five studies [6, 14], and no significant difference between patients with versus without bowel resection was observed (ORs, 1.10 and 0.79, respectively) [12, 13].
Mortality
Three of the five studies reported postoperative mortality [5, 12, 13]. In total, 13 of 492 (2.64%) patients died of concomitant diseases, including myocardial infarction, pulmonary embolism, severe pneumonia, and progressive liver failure.
Discussion
Our study indicated that mesh repair in patients with incarcerated or strangulated hernias was associated with a significantly lower recurrence rate and a similar infection rate compared with anatomic repair. In patients undergoing hernia repair with concomitant bowel resection, the SSI rate with mesh repair was slightly higher. However, most of the infections were well controlled with antibiotics, and further invasive procedures were not needed. According to our included prospective studies, the use of mesh was not contraindicated in patients receiving hernia repair with bowel resection due to strangulation.
SSI is the most worrisome issue related to mesh repair in patients with incarcerated hernias. The recent retrospective literature reported similar infection rates in patients treated with mesh repair, and only one patient underwent prosthesis explantation after conservative treatment [17, 18]. In the study by Sawayama et al., 110 patients with incarcerated groin hernias were included, and similar infection rates were reported in hernia patients with and without mesh repair (12.2% and 16.7%, respectively; OR 0.69; 95% CI 0.23–2.12) [19]. Moreover, no wound infection was reported in patients receiving mesh repair without concomitant bowel resection. Most retrospective studies have reported that the incidence of mesh explantation was rare in patients who received mesh repair for incarcerated and strangulated hernias [20, 21]. Similarly, in all three included prospective studies comparing mesh and anatomic repairs, the infection rates between the groups were similar [7, 15, 16]. Moreover, most of the infections reported were superficial and could be controlled successfully with conservative treatment.
The infection rate associated with the use of mesh for hernia repair with concomitant bowel resection was one of the most important and uncertain issues. In the retrospective study by Ueda et al., 27 patients underwent operations for incarcerated groin hernias with small intestine resection [22]. Similar infection rates were reported in the mesh and anatomic repair groups (20.0% and 17.6%, respectively), and no mesh explantation was needed during follow-up. Similarly, in the Tatar et al. retrospective study including 151 patients, a subgroup analysis revealed that the postoperative infection rate in hernia patients with concomitant bowel resection and mesh repair was 6.7% compared with 2.6% in those who received anatomic repair; no significant difference was noted, and no mesh was removed due to infection [23]. Some studies have noted that the bowel resection itself might predispose the patients to postoperative infection [17, 21, 24], and other risk factors should be considered when mesh repair is used along with bowel resection. The retrospective study of Xourafas et al. which included 177 patients who underwent bowel resection during ventral hernia repair, showed a significantly higher infection rate in the mesh repair group (21.6%) than in the anatomic repair group (4.8%) [24]. In the mesh group, 9 of 14 patients who had wound infections were deeply infected, and seven of them underwent mesh explantation. The recurrence rates were also high because of mesh explantation after advanced mesh infection. Notably, these patients mainly received bowel resection for bowel obstruction and malignancy, not for strangulated hernias, which might be the reason for the great difference from the results of the studies we included. In our included studies, among the 187 patients receiving mesh repair with concomitant bowel resection, only 1 patient had to have infected mesh removed 6 months after the operation [5, 6, 12,13,14]. On the basis of available data, hernia mesh repair was not associated with a significantly higher incidence of severe postoperative infection than anatomic repair, even in the setting of bowel resection performed for strangulated hernias, and the concomitant bowel resection itself may not be a contraindication for mesh application. However, use of mesh in strangulated hernia repair with concomitant bowel resection was associated with considerably lower postoperative comorbidity.
Some studies have mentioned that different mesh materials might lower the infection rates, especially in the setting of concomitant bowel resection. Some case reports have revealed the safety of biological mesh in a contaminated field, but the evidence supporting the use of biological mesh was still limited [25, 26]. In a retrospective study including 761 patients undergoing ventral hernia repair in a contaminated field with mesh, SSIs were not significantly different between the biological mesh, synthetic mesh, and anatomic repair groups [27]. All the meshes used in the eight studies we included were monofilament polypropylene meshes. The low mesh infection rates in these studies might indicate the safety of using synthetic mesh in incarcerated or strangulated hernia repair with bowel resection.
Regarding the incidence of recurrence, a retrospective study by Derici et al. including 131 patients with incarcerated inguinal hernias reported a significantly lower recurrence rate with mesh repair than with anatomic repair (4.0% vs. 20.8%; p = 0.036), and the complication rates were similar between groups [24]. The results of retrospective studies were consistent with those of our review in that the patients who received mesh repair for incarcerated or strangulated hernias had a lower recurrence rate and similar infection rate. The results of these studies support the safety and benefits of mesh repair in this situation. The contemporary WSES guideline which denoted grade 1A recommendation of synthetic mesh repair associated with a significant lower risk of recurrence for patients having a complicated hernia with intestinal strangulation and/or concomitant need of bowel resection without gross enteric spillage (clean-contaminated surgical field, CDC wound class II) [28] also supports our conclusion. However, the WSES guideline recommended anatomic repair for patients with strangulated hernias with bowel necrosis and/or gross enteric spillage during intestinal resection (contaminated, CDC wound class III) was in a dirtier situation compared with patients analyzed in our review [28].
Mild heterogeneity was present in this review. I2 was 0% for the three main outcomes of the three studies comparing mesh and anatomic repairs. However, the five studies comparing hernia patients receiving mesh repair with or without bowel resection might have baseline imbalance due to the different severity of strangulated bowel and the subjectivity of performing bowel resection. Meta-analysis was not performed in these five studies because of the baseline biases.
This analysis has limitations. First, although all the included studies were prospective, only two of eight studies were randomized and balanced in terms of patients who received bowel resection [15, 16]. Second, none of the studies was blinded in terms of judging who should receive bowel resection, owing to the practical limitations. Subjective patient selection for bowel resection might have greatly influenced the results. Also, the patients who received bowel resection were not excluded and were unevenly distributed in one of three studies comparing mesh and anatomic repairs [7], though the results were similar after patients receiving bowel resection were excluded from analysis. Third, the large baseline imbalance of disease severity between patients selected and not selected for bowel resection made comparison of the pooled outcome of mesh repair difficult. When evaluating mesh repair and concomitant bowel resection, we could only compare the effects in individual studies and review the retrospective results. Moreover, our review included hernia repairs of different locations. The SSI between different types of hernias might cause bias, despite the consistency within separate groups noted in our review. Further studies with stricter and systematic control of selection criteria of bowel resection should be well defined to enable stronger conclusions regarding mesh repair in this specific situation.
In conclusion, our results revealed that mesh repair for incarcerated or strangulated hernias was feasible and had a great benefit of a lower recurrence rate. Contemporary data revealed that mesh implementation was still beneficial even in the situation of concomitant bowel resection when considering recurrence. However, current research is limited and makes it difficult to draw conclusions about the safety of mesh repair in this situation, and the major worry of postoperative infection has not yet been well evaluated in studies of a comparable design. The trend of higher infection rates in patients receiving concomitant bowel resection should be examined. Further studies with preset criteria for evaluating patients for bowel resection might be helpful to elucidate this question.
References
Miserez M, Peeters E, Aufenacker T et al (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18:151–163
Choi JJ, Palaniappa NC, Dallas KB et al (2012) Use of Mesh During Ventral Hernia Repair in Clean-Contaminated and Contaminated Cases: Outcomes of 33,832 Cases. Ann Surg 255:176–180. https://doi.org/10.1097/SLA.0b013e31822518e6
Carbonell AM, Criss CN, Cobb WS et al (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2013.07.382
Hentati H, Dougaz W, Dziri C (2014) Mesh repair versus non-mesh repair for strangulated inguinal hernia: systematic review with meta-analysis. World J Surg 38:2784–2790. https://doi.org/10.1007/s00268-014-2710-0
Bessa SS, Abdel-fattah MR, Al-Sayes IA, Korayem IT (2015) Results of prosthetic mesh repair in the emergency management of the acutely incarcerated and/or strangulated groin hernias: a 10-year study. Hernia 19:909–914. https://doi.org/10.1007/s10029-015-1360-y
Ragab A (2014) Is bowel resection still a contraindication for mesh repair of strangulated inguinal. Hernia 2:220–236
Emile SH, Elgendy H, Sakr A et al (2017) Outcomes following repair of incarcerated and strangulated ventral hernias with or without synthetic mesh. World J Emerg Surg 12:1–9. https://doi.org/10.1186/s13017-017-0143-4
Higgins JP, Savović J, Page MJ, et al (2018) Revised Cochrane risk-of-bias tool for randomized trials (RoB 2). 9 October 2018. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD201601
Sterne J, Hernán M, Reeves B et al (2016) Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I): detailed guidance. BMJ 355:i4919
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34. https://doi.org/10.1016/j.jclinepi.2009.06.006
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Atila K, Guler S, Inal A et al (2010) Prosthetic repair of acutely incarcerated groin hernias: A prospective clinical observational cohort study. Langenbeck’s Arch Surg 395:563–568. https://doi.org/10.1007/s00423-008-0414-3
Abd Ellatif ME, Negm A, Elmorsy G et al (2012) Feasibility of mesh repair for strangulated abdominal wall hernias. Int J Surg 10:153–156. https://doi.org/10.1016/j.ijsu.2012.02.004
Topcu O, Kurt A, Soylu S et al (2013) Polypropylene mesh repair of incarcerated and strangulated hernias: A prospective clinical study. Surg Today 43:1140–1144. https://doi.org/10.1007/s00595-012-0397-0
Abdel-Baki NA, Bessa SS, Abdel-Razek AH (2007) Comparison of prosthetic mesh repair and tissue repair in the emergency management of incarcerated para-umbilical hernia: A prospective randomized study. Hernia 11:163–167. https://doi.org/10.1007/s10029-007-0189-4
Elsebae MMA, Nasr M, Said M (2008) Tension-free repair versus Bassini technique for strangulated inguinal hernia: A controlled randomized study. Int J Surg 6:302–305. https://doi.org/10.1016/j.ijsu.2008.04.006
Venara A, Hubner M, Le Naoures P et al (2014) Surgery for incarcerated hernia: Short-term outcome with or without mesh. Langenbeck’s Arch Surg 399:571–577. https://doi.org/10.1007/s00423-014-1202-x
Papaziogas B, Lazaridis C, Makris J et al (2005) Tension-free repair versus modified Bassini technique (Andrews technique) for strangulated inguinal hernia: A comparative study. Hernia 9:156–159. https://doi.org/10.1007/s10029-004-0311-9
Sawayama H, Kanemitsu K, Okuma T et al (2014) Safety of polypropylene mesh for incarcerated groin and obturator hernias: A retrospective study of 110 patients. Hernia. https://doi.org/10.1007/s10029-013-1058-y
Kamtoh G, Pach R, Kibil W et al (2014) Effectiveness of mesh hernioplasty in incarcerated inguinal hernias. Videosurgery Other Miniinvasive Tech 3:415–419. https://doi.org/10.5114/wiitm.2014.43080
Nieuwenhuizen J, Van Ramshorst GH, Ten Brinke JG et al (2011) The use of mesh in acute hernia: Frequency and outcome in 99 cases. Hernia 15:297–300. https://doi.org/10.1007/s10029-010-0779-4
Ueda J, Nomura T, Sasaki J et al (2012) Prosthetic repair of an incarcerated groin hernia with small intestinal resection. Surg Today 42:359–362. https://doi.org/10.1007/s00595-011-0019-2
Tatar C, Tüzün İS, Karşıdağ T et al (2016) Prosthetic mesh repair for incarcerated inguinal hernia. Balkan Med J. https://doi.org/10.5152/balkanmedj.2016.150137
Derici H, Unalp HR, Nazli O et al (2010) Prosthetic repair of incarcerated inguinal hernias: Is it a reliable method? Langenbeck’s Arch Surg 395:575–579. https://doi.org/10.1007/s00423-008-0326-2
Franklin ME, Portillo G, Treviño JM et al (2008) Long-term experience with the laparoscopic approach to perforated diverticulitis plus generalized peritonitis. World J Surg. https://doi.org/10.1007/s00268-007-9463-y
Catena F, Ansaloni L, Gazzotti F et al (2007) Use of porcine dermal collagen graft (Permacol) for hernia repair in contaminated fields. Hernia 11:57–60. https://doi.org/10.1007/s10029-006-0171-6
Bondre IL, Holihan JL, Askenasy EP et al (2016) Suture, synthetic, or biologic in contaminated ventral hernia repair. J Surg Res 200:488–494. https://doi.org/10.1016/j.jss.2015.09.007
Birindelli A, Sartelli M, Di Saverio S et al (2017) 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg 12:37. https://doi.org/10.1186/s13017-017-0149-y
Acknowledgements
This manuscript was edited by Wallace Academic Editing.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, YT., Weng, TY. & Tam, KW. Effectiveness and Safety of Mesh Repair for Incarcerated or Strangulated Hernias: A Systematic Review and Meta-Analysis. World J Surg 44, 2176–2184 (2020). https://doi.org/10.1007/s00268-020-05430-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05430-4