Abstract
Purpose
The aim of this article is to describe the technique and early follow-up results of abdominal wall reconstruction (AWR) by minimally invasive surgery (MIS); it concerns the already described endoscopic (retromuscular) Rives procedure (e-Rives) and posterior component separation with transversus abdominis release (TAR) by endoscopic approach (eTEP-TAR).
Method
This is a prospective study which consists of 60 patients operated on between May 2016 and December 2017 by a single surgeon and monitored until July 2018. This is a heterogenic cohort with different hernia types (lateral, median, combined) which were also treated with different meshes. This material includes physiological and biomechanical issues related to the abdominal wall, the key stages of the operation including port placement strategy.
Results
The group of patients are 55% male, having a mean age of 53.3 years old, mean BMI of 29.3 and median ASA score of 1.83. The majority of the hernia types is represented by incisional hernia (61.7%) located especially on the median side of the abdomen (80%); more than half of them (60%) are reducible. There were 6 (10%) intraoperative complications that lead to four conversions to open or traditional laparoscopic techniques. Postoperative re-admission—two cases: one case with small bowel obstruction, solved by laparoscopic surgery and one case with hemorrhagic gastritis because of non-steroidal anti-inflammatory treatment that required only medical treatment. Quality of life (assessed on a 0–10 scale) evaluating the postoperative pain, normal activity and aesthetics, shows a significant improvement after 2 weeks and 3 months postoperatively compared to the preoperative level. 93.3% of the patients have been monitored and no recurrences after a mean of 15 months have been reported.
Conclusion
A thorough understanding of the anatomy and surgical technique is mandatory. The eTEP approach is a feasible and safe option in MIS ventral hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Purpose
The gold-standard procedure in ventral hernia repair by open approach is, by general opinion, the Rives operation [1, 2]. Its principle is the restoration of the linea alba and mesh placement under the rectus muscles.
The minimally invasive techniques have been improved due to significant changes of the paradigm in AWR: from the “bridged-IPOM” of Leblanc in the 1990s to “IPOM plus” 20 years later—a concept introduced by J.F. Kukleta, representing a huge step for AWR, restoring the abdominal wall functionality and decreasing the rate of recurrences and other complications (postoperative seroma, bulging etc.) [3, 4].
A new, interesting idea occurred: pushing the mesh outside of the abdominal cavity. Miserez and Penninckx [5] repaired a ventral hernia placing the mesh pre-peritoneally and Wolfgang Reinpold placed the mesh under the rectus muscles by trans-hernial access (MILOS technique) [4,5,6].
Belyansky et al. [7] published a new technique combining the eTEP access described by Jorge Daes with the principles of TAR described by Novitsky [7,8,9,10]. The result (eRives/eTEP-TAR) is very promising and the technique has the potential to become one of the best solutions in laparoscopic ventral hernia repair (LVHR) [8].
An important improvement has been noticed in complex AWR: the principles of magistral component separation—anterior component separation (ACS)—Ramirez and Novitsky’s TAR are applied in MIS operations: eACS (Rosen) and eTEP-TAR (Belyansky) [11, 12].
One of the biggest advantages of this approach is the possibility to extend the retro-rectus dissection laterally to the semilunaris lines, performing TAR, or eTAR, respectively; in this way, large defects in the abdominal wall can be repaired. Sometimes the decision to perform a TAR can be made during the surgery.
Methods and patients
The biomechanics of the abdominal wall and abdominal cavity
Due to the tone of the abdominal wall muscles, the pressure inside the abdominal cavity is 5–7 mmHg [13].
According to Laplace’s law, this pressure acts equally on the abdominal wall, determining the tension.
So the “tension-free” concept, which Lichtenstein implemented in inguinal hernia repair in 1984, is not available if restoration of AW functionality is the aim.
The new surgical techniques have changed the attitude from tension-free repair to restoration under physiological pressure when the aim is the restoration of architecture and functionality of the abdominal wall; the focus of these procedures is the reconstruction of the linea alba, the “central tendon” of the abdominal wall [12] (Fig. 1).
Law of Laplace [14]
The most useful preoperative imaging exploration is the CT scan. It allows us to locate the defect, measure it, and establish the strategy for the surgery.
For example, in our practice, the Rives–Stoppa technique alone is enough when the sum of the bilateral rectus muscle width (RW) is at least twice the maximal defect width (DW)—Fig. 2, confirming Carbonell’s algorithm, presented at 9th Annual Abdominal Wall Reconstruction Summit, Montana US, 2018: additional myofascial release (TAR) may be necessary if the maximal defect width closely approximates or exceeds twice the rectus width—Fig. 3.
Before explaining the key stages of the surgery, it is important to first mention exclusion criteria of the patients: all the patients presenting mesh infection and/or fistula have an absolute contraindication to eTEP and MIS; the patients with dystrophic or ulcerated skin, the patients with loss of domain, the patients with previous pubo-xiphoidian incision and also the patients with a previous retromuscular ventral hernia repair have a relative contraindication to eTEP.
There are no contraindications related to the width of the defects. As in open retromuscular surgery, the eTEP approach can be used to repair all varieties of ventral hernias, from small umbilical hernias to large and complex ventral hernias.
The key stages of the eRives and eTEP-TAR procedures are:
-
1.
Development of the retro-rectus space and port placement.
-
2.
Cross-over of the midline.
-
3.
Connection of both retro-rectus spaces, left and right.
-
4.
3* TAR (when needed [8]).
-
5.
Closure of the defect and restoration of linea alba.
-
6.
Mesh placement.
-
7.
Exsufflation.
-
1.
Development of the retro-rectus space and port placement.
Conversely to the traditional laparoscopic approach, the ports have to be placed medially to the semilunaris lines for ergonomic reasons. The linea semilunaris is the most important landmark for port placement.
As a rule, the ports have to be placed opposite to the side of the abdomen related to the hernia location:
-
Hernia located in the lower part of the abdomen: the ports will be placed above the umbilicus (Fig. 4a, left).
-
Hernia located in the upper part of the abdomen: the ports will be placed below the umbilicus (Fig. 4a, right).
-
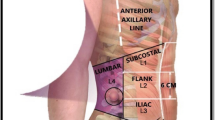
Hernia located laterally (hypochondrium, flank, lateral lower quadrant or lumbar): consider ports placement laterally, on the opposite side of the abdomen (Fig. 4b).
Port placement must also take the previous scar into consideration (in incisional hernia); the midline has to be crossed over, preferably in a virgin part of the abdomen, where the subjacent ligament (falciform or umbilical, respectively) is untouched and can protect against the accidental penetration of the peritoneal cavity.
The first step is developing the retro-rectus space. We can do that using an optic port or a balloon trocar.
After dissecting the retro-rectus space we inflate using CO2 and then we insert the ports just medially to the semilunaris line (Fig. 5).
Important! Introducing the ports laterally to the semilunaris line (outside of the rectus sheath) results in penetration of the (uninflated) peritoneal cavity and carries major risk of injury to the viscera!
-
2.
Cross-over of the midline should be done in the virgin part of the wall, on the opposite side to where the defect is located (Fig. 6).
Crossing the midline to the contralateral retro-rectus space must be totally extraperitoneal (TEP), anterior to the falciform ligament, when we start from left to right (if the defect is in the lower abdomen) and, respectively, anterior to the umbilical ligament, when the crossing starts from right to left, inferiorly to the umbilicus (if the defect is in the upper abdomen).
-
3.
Connection of both retro-rectus spaces, left and right
Dissecting both retro-rectus spaces (left and right) and connecting them by incising the posterior sheaths on their medial edges conducts to a common large retromuscular space (the left retro-rectus space connected to the right retro-rectus space). This space is linked by the preperitoneal bridge represented by the falciform ligament and/or umbilical ligament. The retro-rectus dissection is limited laterally by the semilunaris lines, where the neurovascular bundles pass through the posterior sheath to the rectus muscles (Fig. 7).
The dissection should be done preperitoneally as far as possible; opening the peritoneum at the level of the hernia neck is almost unavoidable. This step must be performed carefully, delicately and using sharp dissection to avoid injury to the bowel—if it is herniated in the sac. Keeping the sac will assist with the closure of the posterior defect.
3*. TAR. For more challenging defects that require large mesh placement, the TAR procedure is added. The incorporation of TAR was found beneficial in cases with a wide defect (10 cm), tension on the posterior layer, narrow retro-rectus space (< 5 cm) or when dealing with a poor compliant abdominal wall [8].
If we decide to perform TAR, it is important to identify the semilunaris lines, marked by the neuro-vascular bundles.
Incision of the posterior lamella of the internal oblique fascia 1 cm medially to the semilunaris line exposes the transversus abdominis (TA) muscle (Fig. 8).
This step can be done from “bottom to top” (first it is necessary to identify the arcuate Douglas line) or from “top to bottom” (Fig. 9).
The transection of the TA muscle and a posterior component separation (Fig. 10), which can be done laterally up to the psoas muscle, allows medial mobilization of the musculo-fascial edges.
-
4.
Closure of the defect and restoration of linea alba
Closure of the defect in the posterior layer (if the peritoneum was opened) is necessary to keep a barrier between the mesh and the viscera. This layer is not a resistance layer (Fig. 11).
Restoration of the linea alba is done by suturing the anterior sheaths of the rectus muscles on the midline. This step is performed using a non-resorbable barbed 0 (zero) suture. This suture is possible if we reduce the pressure of insufflation to 5–6 mmHg when we pull the stitch (Fig. 12).
-
5.
The mesh placement into the retro-rectus space will be done after measurement of the entire area to be covered by the mesh (Fig. 13).
Important! The surface covered by the mesh is not the surface of the defect; it is the entire dissected area.
The mesh has to be completely flat on the posterior layer.
In our practice, after correct dissection and thorough hemostasis, we do not consider drainage necessary.
-
6.
Slow exsufflation, under direct vision, allows us to ensure the mesh remains in the correct position.
Methods
We consider all the medical records of patients with ventral hernias (primaries or incisional) who underwent laparoscopic eTEP repairs between May 2016 and December 2017. The procedure is performed by the same surgical team within Life Memorial Hospital, Bucharest, Romania.
All the hernias are classified according to EHS criteria [15].
The main parameter regarding the postoperative evolution is hernia recurrence, which is systematically assessed at every clinical follow-up or by asking five questions in the event of telephone follow-up. Other measured parameters are: length of stay, surgical site occurrence (seroma, hematoma and infection), 30-day post-op readmission and any other medical or surgical complications during the period of follow-up.
The quality of life is measured by a scale derived from EuraHS Quality of Life Scale: there are three questions addressed to the patients on admission (before surgery), on the 1st postoperative day and at the 1st and 2nd clinical follow-up. These three questions evaluate the pain in resting position (lying down), the restriction of daily activities (walking, climbing stairs) and the cosmetics related to the abdomen and hernia site. The answers are reported numerically on a scale of 0–10.
Chronic pain is defined as pain which persists for more than 3 months postoperatively and influences daily activities.
The data are added to an electronic database and statistics are performed by SPSS 20.
Patients
This study includes 60 consecutive patients (33 male, 27 female) operated on between May 2016 and December 2017. The demographics are presented in Table 1.
The most frequent type of hernia is incisional (61.7%) and the most frequent hernia site is the median site of the abdomen (80%). Over half of them are reducible (60%).
The hernia characteristics are presented in Tables 2 and 3.
The median defect area is 99.5 cm2 (min 6 cm2–max 375 cm2) and the median width is 5.5 cm (min 1 cm–max 17 cm), but there are important variations according to the type of hernia and these are detailed in Table 4.
The diastasis recti associated with the ventral hernia
Diastasis recti is an abdominal wall deformity, which has numerous definitions and three major classifications, which are not the subject of this article. In our practice we have adhered to Rath’s classification, which states that any enlargement over 27 mm of the linea alba at the level of the umbilicus is considered a diastasis [16].
Diastasis recti is associated with the majority of primary ventral hernias (22 cases out of 25–88%) but also with incisional hernias (5 cases out of 28–17.8%). According to literature, correction of the umbilical hernia alone without correction of the diastasis is often associated with recurrence due to the poor quality of the surrounding tissue [17]. We have expanded on this to include all ventral and incisional hernias. Therefore, no matter the case, the linea alba is restored by suturing the anterior sheaths and reinforcing the suture line by placing an adequate-sized mesh into the retro-rectus space. In our data, the size of the weakness is considered to be the actual “diastasis defect” and not only the hernia defect (for example in a small umbilical hernia of 2 by 2 cm and a diastasis recti of 5 cm width and 20 cm length, we consider the area of the defect 100 cm2 and the mesh should be at least 30 cm in length; the width of the mesh in this case is shaped to fit into the retro-rectus space between the two semilunaris lines). In cases involving diastasis the mean length of the defect was 18 cm (min 10 cm to max 25 cm) and the mean length of the mesh was 28 cm (min 10 cm to max 30 cm). Regarding the diastasis’ width, it measures a mean of 5 cm (min 3 cm to max 9 cm) and the mesh is mean 17 cm width (min 10 cm to max 25 cm), to cover the entire dissected area.
Comments
Multiple site hernias are particular cases that involve at least two distinctive sites of hernia. In our series we encountered 7 such cases: two associating median and inguinal hernias, two median and former-stoma site incisional hernias, one case of double incisional hernia post laparoscopic cholecystectomy (umbilical and right flank), one case of subcostal incision spreading from epigastric to right flank region and one complex case with complete left semilunar line destruction and epigastric hernia. In these particular situations it is difficult to assess the correct defect area and the technical solutions usually need two meshes so we consider that they do not fit into our defect/mesh size analysis table.
Procedures
We use the eTEP technique as first option for all of our patients. Four patients needed conversion to open or laparoscopic approach. The conversion was due to: respiratory difficulties in two cases, intensive fibrosis in the retro-rectus space in one case and bowel adhesions to a previous mesh in another case (Table 5).
Analyzing the cases that needed TAR we find out that it was performed in 6 cases as unilateral TAR and in 13 cases as bilateral TAR. Unilateral TAR was performed in four cases of either lateral hernia (mean defect width of 7 cm; min 4 cm to max 11 cm) or multiple-sites hernia, but with a lateral component (two cases). Regarding the lateral hernias which occurred in this study (subcostal—L1, flank—L2 and iliac fossa—L3) the technique includes retro-rectus dissection and unilateral (ipsilateral) TAR. The dissection is enlarged as laterally as possible performing a posterior component separation. In this way the retro-rectus space and the pretransversalis space are connected obtaining a large retromuscular space. After closure of the hernia defect, the mesh is placed into this space, covering medially the posterior rectus sheath and, laterally, the peritoneum and fascia transversalis and augmenting the suture of the defect and reinforcing the abdominal wall.
Bilateral TAR was performed in ten cases of median hernia (mean defect width 7.9 cm; min 6 cm to max 15 cm) and in three cases of multiple-sites hernia.
The eTEP-RS procedure was performed in 38 cases of median hernia with a mean defect width of 5.5 cm (min 2 cm to max 10 cm). Nevertheless, there is a statistically significant difference between these two means (p = 0.006), but we can notice a “gray” area between 6 and 10 cm defect width where TAR procedure may be needed or not—that is the area where Carbonell’s algorithm may be applied (Fig. 14).
In all cases, the restoration of the linea alba (the “central tendon of the abdomen”) was achieved, as it represents the goal of abdominal wall reconstruction; it improves the isokinetic and isometric functions of the abdominal wall and ultimately the quality of life [18].
Mesh and fixation
The most frequently used mesh is Parietene Macroporous™ (55 cases, 91.7%), followed by self-fixating mesh (ProGrip™) in two cases and a more rigid, heavy-weight mesh (Assumesh®) in another two cases.
In 83.4% of the cases the mesh was fixated using cyanoacrylate: 75% applying glue alone; in the rest of the cases tackers or sutures were added if the defect was located in the suprapubic area. In 16.6% of the cases the mesh was placed into the retro-rectus space without any fixation. Mesh fixation by cyanoacrylate is an established method [19]. The first meshes were fixed by force of habit as we still do in inguinal hernia repair. In time, as far as ventral hernia repair was concerned, mesh fixation was deemed unnecessary due to the restrictive space and lack of orifices resulting in a low probability of mesh migration.
Operative time
For a proper analysis of surgical time we filtered out the four cases of conversion and analyze only the 56 procedures finished by eTEP approach. We noticed that this procedure is shorter for primary ventral hernias compared to incisional ones by 55 min (p = 0.005) and there is also a significant difference between eTEP and eTEP-TAR of 95 min (p = 0.005) in terms of surgery time (skin-to-skin). These differences also apply for operative room time (total duration of OR occupation).
Results
Postoperative length of stay was the same for most patients: 81.7% (49 patients) spent only one post-op night in the hospital. The median postoperative stay was similar for all eTEP patients, regardless of surgery time or underlying hernia pathology (Table 6).
This short hospital stay was mainly related to a low level of pain. To analyze this, we assessed the pain control methods and only eight out of the first 25 patients required analgesia by epidural catheter. This type of analgesia was “inherited” from the IPOM period when all patients with incisional hernia received one. After a few months we completely abandoned it and used only intravenous analgesics (NSAI) or opioids during hospital stay. If we rule out the patients with epidural catheter and count the doses of pain medications, it turns out that, on average, an eTEP patient gets 2.7 doses of painkiller for every 24 h of hospital stay.
Starting with the year 2017, we began to actively asses the quality of life of our patients and 42 patients filled out our questionnaire; the results are expressed in Fig. 15.
There is a significant improvement of overall score between preoperative, 2-week postoperative follow-up (p = 0.03) and 3-month postoperative follow-up (p = 0.02) (Table 7).
Intraoperative incidents were: rupture of the semilunaris line at the beginning of the procedure, while developing the retro-rectus space caused by overinflation of the balloon (one case), which needed a TAR to cover the damaged area and a small bowel perforation during dissection which required suturing (one case).
The conversion (four cases) was due to respiratory difficulties (two cases), intensive fibrosis in the retro-rectus space (one case) and bowel adhesions to a previous mesh in another case.
In-stay complications are represented by: one case of suture disruption (mechanical failure) that needed an open procedure to re-approximate the linea alba and one case of umbilical hematoma in a patient that stayed 3 days under medical supervision in the hospital but without the need for an active intervention.
One early readmission was due to a small bowel obstruction caused by a tear in the posterior layer that needed laparoscopic suture. We concluded retrospectively that this complication occurred because of too much tension in the posterior layer. From that point on we have always focused on reducing posterior layer tension. The other readmitted case was a hemorrhagic gastritis caused by excessive NSAI use.
Chronic pain (defined as pain persistence over 3 months postoperatively which impaired daily activities) was recorded in two cases: one of them was the patient with a semilunaris line tear during balloon inflation and the other one a patient with a multisite hernia. At the 2-year follow-up clinical control the patient with the semilunaris line tear showed a complete recovery, with no functional impairments or chronic pain.
There are no recorded recurrences in our cohort at the mean follow-up of 15 months (min 7 and max 26) in 56 out of 60 patients (4 patients were considered lost to follow-up).
Discussion
-
A detailed knowledge of the anatomy is a must. During the dissection it is important to recognize and avoid injury to the neuro- and vascular-elements (inferior epigastric pedicles, intercostal neurovascular bundles) and fascial structures, such as the semilunar line. Preservation of neurovascular supply leads to maintenance of native rectus function and thus a more robust and functional repair [14]. Also, injury to the semilunaris line causes an irreversible destabilization of the abdominal wall.
-
Restoration of the linea alba (the “central tendon of the abdomen”) remains the goal of abdominal wall reconstruction; it improves the isokinetic and isometric functions of the abdominal wall and ultimately the quality of life [18].
-
Mesh placement outside of the abdominal cavity represents a huge advantage, on one hand, avoiding contact between mesh and the viscera (with all of the associated late consecutive complications) and, on the other hand, reducing the cost (quite high for dual meshes and fixation devices).
-
The results of our prospective study are superposable with the early results of this procedure published in Surgical Endoscopy in 2017 [8].
Conclusion
The eTEP approach is a feasible and safe option for ventral hernia repair with a low postoperative rate of complications: no recurrences and low risk of chronic pain.
References
Cox TC, Pearl JP, Ritter EM (2010) Rives–Stoppa incisional hernia repair combined with laparoscopic separation of abdominal wall components: a novel approach to complex abdominal wall closure. Hernia 14(6):561–567
Forte A et al (2011) Rives technique is the gold standard for incisional hernioplasty. An institutional experience. Ann Ital Chir 82(4):313–317
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3(1):39–41
Bittner R et al (2014) Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc 28(1):2–29
Miserez M, Penninckx F (2002) Endoscopic totally preperitoneal ventral hernia repair. Surg Endosc 16(8):1207–1213
Schwarz J, Reinpold W, Bittner R (2017) Endoscopic mini/less open sublay technique (EMILOS)—a new technique for ventral hernia repair. Langenbeck’s Arch Surg 402(1):173–180
Belyansky I, Zahiri HR, Park A (2016) Laparoscopic transversus abdominis release, a novel minimally invasive approach to complex abdominal wall reconstruction. Surg Innov 23(2):134–141
Belyansky I et al (2018) A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc 32(3):1525–1532
Daes J (2012) The enhanced view-totally extraperitoneal technique for repair of inguinal hernia. Surg Endosc 26(4):1187–1189
Novitsky YW (2016) Posterior component separation via transversus abdominis muscle release: the TAR procedure. In: Novitsky YW (ed) Hernia surgery. Springer International Publishing, Cham, pp 117–135
Ramirez OM, Ruas E, Dellon AL (1990) ‘Components separation’ method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86(3):519–526
Rosen MJ (2015) Atlas of Abdominal Wall Reconstruction - ISBN: 9781437727517| US Elsevier Health Bookshop. Chap 11. pp 185–201 [Online]. http://www.us.elsevierhealth.com/product.jsp?isbn=9781437727517&navAction=&navCount=0. Accessed 8 Oct 2015
De Keulenaer BL, De Waele JJ, Powell B, Malbrain MLNG (2009) What is normal intra-abdominal pressure and how is it affected by positioning, body mass and positive end-expiratory pressure? Intensive Care Med 35(6):969–976
Losken A, Jeffrey J (2012) Advances in abdominal wall reconstruction. Thieme Publishers, New York
Muysoms FE et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414
Rath AM, Attali P, Dumas JL, Goldlust D, Zhang J, Chevrel JP (1996) The abdominal linea alba: an anatomo-radiologic and biomechanical study. Surg Radiol Anat 18(4):281–288
Nahabedian MY (2016) Diagnosis and management of diastasis recti. In: Novitsky YW (ed) Hernia surgery. Springer International Publishing, Cham, pp 323–336
Criss CN, Petro CC, Krpata DM, Seafler CM, Lai N, Fiutem J (2014) Functional abdominal wall reconstruction improves core physiology and quality-of-life. Surgery 156(1):176–182
Kukleta JF, Freytag C, Weber M (2012) Efficiency and safety of mesh fixation in laparoscopic inguinal hernia repair using n-butyl cyanoacrylate: long-term biocompatibility in over 1,300 mesh fixations. Hernia 16(2):153–162
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
The protocol was approved by the ethics committee of the institutions.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
All the patients gave the informed consent for procedure and scientific data use as standard in our hospital.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Radu, V.G., Lica, M. The endoscopic retromuscular repair of ventral hernia: the eTEP technique and early results. Hernia 23, 945–955 (2019). https://doi.org/10.1007/s10029-019-01931-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01931-x