Abstract
Purpose
From the current evidence, non-fixation of the mesh (NMF) in laparoscopic total extraperitoneal (TEP) repair appears to be a safe alternative for inguinal hernia patients in the short term. This study aims to demonstrate that NMF is as effective in the long term by following up a large number of patients with a mean follow-up of 6 years. The primary outcomes are chronic pain and recurrence rate.
Methods
A thorough review of medical records was conducted from a prospectively maintained database of 538 patients who underwent a laparoscopic TEP inguinal hernia repair by a single surgeon working in Sydney from the year 2005 to 2010. Patient demographics, perioperative outcomes, and postoperative complications were extracted from this database. All these patients were then interviewed using a modified questionnaire based on Franneby et al. [10].
Result
538 patients had TEP repair between 2005 and 2010. Out of this 11 were excluded as tacks were used for fixation of mesh. Out of the 649 repairs done on 527 patients during this period, 463 hernia repairs in 387 patients could be followed up with a mean follow-up of 6 years and 4 months. The mean age of patients was 63 years. Overall, there were seven (1.5%) recurrences, and the incidence of chronic pain was 1%, however 2.9% patients in total complained of pain.
Conclusion
This is the only study in literature having a long-term follow-up of more than 5 years for the patients having inguinal hernia repair by TEP technique without mesh fixation. It demonstrates that fixation of mesh with tacks or glue is unnecessary for TEP repair of inguinal hernia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is one of the most common surgical procedures performed worldwide [1]. Since the introduction of laparoscopic repair of inguinal hernia in 1990, it has evolved significantly. The two common methods that are used for laparoscopic inguinal hernia repair are transabdominal preperitoneal (TAPP) repair and total extraperitoneal (TEP) repair.
Laparoscopic TEP of inguinal hernia has been associated with less postoperative pain, decrease in recurrence rates, a faster recovery and earlier return to work, compared to the conventional open hernia repair [2].
One of the biggest controversies in laparoscopic TEP inguinal hernia repair is about fixation of mesh. The initial concern in laparoscopic inguinal hernia repair was recurrence; hence all the meshes were fixed with tacks. Soon it was realised that tacks could cause nerve entrapment and be a cause of chronic pain [3, 4]. With decreasing recurrence rate, the emphasis has shifted from recurrence to incidence of chronic pain. To decrease this incidence of chronic pain, alternative methods were used like different meshes and fibrin glue. While fibrin glue is reported to have good results in some studies, most of these studies had small sample size, shorter period of follow-up, and mainly done with TAPP technique [5–7].
From the current evidence, the non-fixation of mesh (NMF) in TEP appears to be a safe alternative for the selected inguinal hernia patients. It will not increase the risk of early hernia recurrence and has shown to have advantages with respect to costs, hospital stay, and operative time [1, 8].
Similar to mesh fixation by fibrin glue, the criticism of NMF has been the absence of long-term follow-up and smaller sample size [8, 9]. Additionally, very few studies doing long-term follow-up for chronic pain have used a standard questionnaire. In this study, we aim to follow a large number of patients with a mean follow-up of more than 6 years to see if NMF of inguinal hernia when done through a laparoscopic route is comparable to mesh fixation in terms of incidence of chronic pain and recurrence.
Materials and methods
The co-author (PM) in this article has been doing laparoscopic inguinal hernias since 1994. A thorough review of the database that was maintained prospectively was done to extract demographic and perioperative variables that included age, gender, diagnosis, unilateral or bilateral hernias, smoking habits, occupation, duration of stay, operative time, perioperative complications (intraoperative and postoperative), preoperative groin pain, recurrent hernia, on all patients who underwent a elective laparoscopic TEP inguinal hernia repair by the co-author (PM) from the year 2005 to 2010.
Hernias that were initiated laparoscopically but had to be converted to open were excluded from the final study group. This database of hernias also included the follow-up data of all the patients with the hospital clinic at 2 weeks and with the consultant after 6 weeks. In the follow-up, patients were interviewed for presence of any symptoms and were examined for any recurrence. All the patients in the database were then contacted and interviewed through telephone using a standard questionnaire. Inguinal Pain Questionnaire (IPQ) devised by Franneby et al. was used to evaluate chronic pain. The first part focuses on the frequency, severity, and type of pain. The second part of the questionnaire focuses on interference with daily activities, in line with a proposal by Kehlet et al. [10]. The questionnaire was modified to suit the lifestyle of the older demographic within the study, thus, the breadth of questions on occurrence of pain was tailored to activities that the study participants were likely to experience. Additionally, the questionnaire queried the history of swelling or discomfort noticed by the patient in the groin—especially when straining, lifting, coughing, or exercising—that improves when resting.
Questions about feelings, such as weakness, heaviness, burning, or aching in the groin or having noticed an enlarged scrotum in men or boys were also asked.
Those who complained of swelling or discomfort were then invited for physical examination and ultrasound examination to check for recurrence.
The operative technique was standardised and repeated in all the operations. Further, the operations were completed either by the consultant himself or by a registrar under the supervision of the consultant. Patients were advised to empty their bladder before the procedure. Under general anaesthesia, an infra-umbilical vertical incision is made, the anterior rectus sheath incised transversely, the rectus muscle retracted, and the extraperitoneal space developed with an extraview oval shaped balloon, followed by a structural balloon (Autosuture, Covidien, USA) insufflator. Two midline ports are used. For insertion of the first port, the umbilical port was pulled towards patient’s head, and the port was inserted as close as possible to this umbilical port. The second port was inserted few centimetres below this port. After identification of the epigastric vessels and pubic symphysis, dissection of the preperitoneal space was begun laterally. The hernia sac was then identified, skeletonised of the surrounding vessels and cord. Dissection was carried out between vessels and cord to ensure that all the peritoneum had been stripped off the cord. Either a Bard 3D mesh or Parietex mesh with preformed overlapping slit (14 × 10 cm) (Covidien, USA) with a slit was used in most cases to cover the myopectineal orifice of Fruchaud. Local anaesthesia is then put in, and the space deflated under vision to ensure that the peritoneum was behind the mesh.
Results
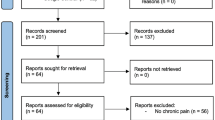
A total of 538 patients had laparoscopic inguinal hernia repair done by the surgeon from 2005 to 2010. Eleven were excluded from the study as tacks were used to fix the mesh because of unusually large size of the hernia [Type 3 = >3 cm (more than two fingers), P/R, L/M-EHS classification]. These hernias were generally large direct hernias with almost complete absence of posterior wall of the inguinal canal.
There were in total 649 TEP repairs done on 527 patients during that time. 607 hernias were primary repairs (did not have any previous repair done on that hernia), and 42 were secondary repairs (patients who had a previous repair done and had recurrence on the same side). None of these recurrent hernias had a preperitoneal mesh in place. They all were recurrences after open repair. All of these patients were included in the study group. The median age of the study sample was 63 years. There were 466 (88%) male patients and 61 (12%) female patients in this study group. Out of 527 patients, 405 (77%) were operated for unilateral hernia and 122 (23%) were operated for bilateral hernia. 271 (41.8%) were direct, 321 (49.5%) were indirect, and 57 (8.8%) were pantaloons hernias (Table 1). 101 (19%) out of total 527 patients were smokers and only one (14%) out of the seven recurrences was a smoker. Large Bard 3D mesh, Medium Bard 3D mesh and Parietex mesh with a slit was used in 351 (54%), 14 (2%), 284 (44%) hernias, respectively. Currently, the author favours parietex mesh with a slit in all his cases.
There was one major intraoperative complication which was a bladder perforation in a patient who had previous radical prostatectomy. This was detected intra-operatively and clipped laparoscopically. The urinary catheter was left in for a week and patient did not require any further intervention. There was no in-patient mortality. There were 19 incidental femoral hernias. The average operating time was 29.78 ± 9.66 min for unilateral hernias and 40.45 ± 12.04 min for bilateral hernias.
There were 16 seromas that were significant and caused symptoms to the patient. Other complications included six urinary retentions, seven rectus sheath haematomas, and twelve cases of wound infection. Major complications included two pelvic haematomas out of which one required laparotomy for evacuation. Non-surgical complications included one patient having seizure postoperatively and one having anaphylactic reaction to a drug postoperatively (Table 2).
26 (4.9%) patients had pain in the early follow-up after 2 weeks. 19 (3.6%) patients in this group did not have any pain prior to the operation. Most of them needed a second follow-up few weeks later with regular analgesia, with pain resolving for all of them within 3 months. Only one patient required steroid injection with good effect. None of these 19 patients complained of pain in long-term follow-up. Pain persisted in the remaining seven patients. These were the patients who had hernia repair for a recurrent hernia (secondary hernia) and had pain pre-operatively. These patients were happy to follow-up with their general practitioner.
Attempts were made to contact all these patients with 73% (387) success rate, which included 71% (463) hernias out of the 649 done during this time period. Out of them, 431 were primary repairs and 32 were secondary repairs.
The average duration of follow-up was 6 years and 4 months. The earliest was 3 years and 1 month, and the longest being 14.4 years. All these patients were interviewed using the described standardised questionnaire (Table 3).
There were seven (1.5%) recurrences in total (Table 4). All of them were unilateral; four recurrences were in patients in whom parietex mesh had been used, and the remaining three patients had Bard 3dMax mesh used in their hernia repairs. The earliest recurrence was 2 weeks post-surgery and latest was 41 months post-surgery. Notably, early recurrences in the group included one patient that suffered a seizure postoperatively and another patient who had angioedema postoperatively, the significance of which was difficult to ascertain.
14 (2.9%) patients reported pain through the telephone interview on long-term follow-up. Eight of these patients had parietex mesh used and the remaining six had Bard 3dMax mesh used in the repair of their hernias. No patient reported any swelling in the telephone interview. All 14 patients had a unilateral repair and were invited for a clinical examination, which was followed by ultrasound in all of them. No recurrences were detected. Seven out of the fourteen patients had recurrent hernia repaired and had pain prior to the operation on the same side (Table 5). This pain persisted in all of them with five of them reporting it occurred frequently 4–5 times a week, although none of them required regular painkillers or time off work (Table 3). Four out of five in this group described pain as stabbing or burning.
The rest of the seven patients described a mild pain that was often brought on after lifting heavy weight or standing for a long time. In all these seven patients, pain had developed 12–18 months after the operation. This could be the result of scarring around the mesh.
Discussion
Previous studies have already shown that non-mesh fixation of inguinal hernia is safe, cost-effective with comparable recurrence rate and decreased incidence of chronic pain [1, 11, 12]. Apart from validating those findings, this study attempts to demonstrate that non-mesh fixation is as effective in the long term.
Recurrence
It is well known that the recurrence rates are influenced not only by surgical expertise and method of repair, but also by the length and method of follow-up evaluation [13].
In a study by Messenger et al., recurrence rate of TEP repair of inguinal hernia with mesh fixation was noted to be 1.1% at 5 years and incidence of chronic pain around 7.6% [14]. Eklund et al. in their randomised multi-centred trial with mesh fixation showed a cumulative recurrence rate of 3.5% at 5 years [15]. During a 10-year follow-up period, M. Staarink found a recurrence rate of 4%. [13].
In their meta-analysis Sajid et al. noted a recurrence rate of 1.4% with glue fixation in a follow-up ranging from 1 to 27 months [16]. Most of these studies in this meta-analysis did TAPP repair with glue fixation. The study with longest follow-up (40 months) had nine patients included in it [9]. Most of other studies have reported a follow-up of around 6 months and recurrence rate of 0–1.6% [17, 18].
The follow-up of studies for NMF in TEP ranged from 6 to 24 months with an average recurrence rate ranging from none to 2% [12, 19–23]. Most of the studies published for TEP repair with glue fixation or NMF have only short-term follow-up. In our study with an average follow-up of 6 years and 4 months, we have shown recurrence rate of 1.5%, which is comparable to previous studies (Table 4).
Chronic pain
To assess chronic groin pain and inguinal pain, questionnaire developed by Franneby et al. was used [10]. The IPQ is a modification of the questionnaire of Kehlet et al. Chronic groin pain had a significant correlation with preoperative pain and early postoperative pain [24]. The incidence of chronic pain was found to be varying from 0 to 63% when all the studies for hernia repair were included (laparoscopic/open, with mesh/without mesh) [4].
The incidence of chronic pain varies in literature from 6 to 16% for laparoscopic repair with around 11% being reported by Eklund et al. [25]. Among the very few studies that have used a standardised questionnaire to assess chronic pain, Farley et al. from Mayo clinic found 2% of patients to have severe pain and 21% to have mild symptoms at an average of 5.7 years follow-up [26].
In our study, the incidence of chronic pain (as defined in Table 5) was 1.0%, and an additional 1.9% of patients complained of mild niggling pain. In the group of people with chronic pain, the severity was low and did not require them to take time off work or take regular painkillers. Studies reporting chronic pain after TEP repair using fibrin glue have reported chronic pain rate of from <1 to 13.2% [17, 18]. None of these studies have reported long-term follow-up or used a detailed questionnaire. Nerve injury rate varies from 0.5 to 14% in literature from staples used for fixation of mesh in inguinal hernia repair [27]. Four patients did describe burning or stabbing pain in this study, which would suggest nerve involvement. All of these four patients had previous hernia repair but they had exactly the same pain before the operation suggesting possible nerve involvement in the first operation.
Long-term follow-up
It is demonstrated that hernia recurrence occurred mostly within 2 years postoperatively [28]. In our study, the mean follow-up was 6 years and 4 months. The earliest recurrence was at 2 weeks and latest was 41 months. This is comparable to previous studies dealing with long-term follow-up, and this ranges from 58 to 94% [13, 14, 25].
Although it has been assumed that mesh will migrate in the immediate postoperative period if not fixed, one of the few studies done in humans to see if mesh migrates after movement showed that mesh stayed in place in spite of movements of hip [29]. We strongly believe that putting an adequate size mesh with satisfactory coverage around the hernia after adequate dissection holds the key to successful repair.
In this study, the mean operating time was 29 min for unilateral hernias and 40 min for bilateral hernias. Teng et al. in their meta-analysis found a significantly shorter operative time for the non-fixation group [1]. Studies have consistently showed that NMF is more cost-effective compared to MF by either staples or fibrin glue [1, 12, 19, 20]. The average length of stay in our study was 1 (1–2) day, which is comparable to the published literature.
Strengths of studies
The strength of this study has been the long-term follow-up using a standardised questionnaire in a large sample of population. The mean length of follow-up in this study was 6 years and 4 months, which is the longest for NMF in TEP repair. Chronic pain was evaluated using a validated questionnaire. High percentage of follow-up is another positive point for this study and this is comparable to the best follow-up achieved in published literature for long-term follow-up of laparoscopic inguinal hernia repair [13, 14, 30].
Drawbacks
As the size of the hernias was not initially recorded in all the cases, subgroup analysis based on size was not possible. This could be of importance in the case of recurrences. 11 out of 538 hernias were excluded because tacks were used considering their large size, which shows selection bias. Although these patients were not followed up in the long-term, but early data showed recurrence in two out of these eleven patients suggesting the difficulty associated with repairing the large hernias laparoscopically. Only 73% follow-up could be achieved. Although this is comparable to other published studies, it always raises the possibility of missing hernia recurrences and can be considered a measurement bias.
Conclusion
This study demonstrates that fixation of mesh with tacks or glue is unnecessary in cases of TEP repair of inguinal hernia. Not only does it increase the cost of repair but also it increases the operative time. Non-fixation of the mesh has good long-term outcomes both in terms of recurrence and incidence of chronic groin pain.
References
Teng YJ, Pan SM, Liu YL, Yang KH, Zhang YC, Tian JH, Han JX (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25:2849–2858. doi:10.1007/s00464-011-1668-3
Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90:1479–1492. doi:10.1002/bjs.4301
Wong J, Anvari M (2001) Treatment of inguinodynia after laparoscopic herniorrhaphy: a combined laparoscopic and fluoroscopic approach to the removal of helical tackers. Surg Laparosc Endosc Per Tech 11:148–151
Poobalan AS, Bruce J, Smith WCS, King PM, Krukowski ZH, Chambers WA (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19:48–54
Boldo E, Armelles A, Perez de Lucia G, Martin F, Aracil JP, Miralles JM, Martinez D, Escrig J (2008) Pain after laparascopic bilateral hernioplasty: early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc 22:1206–1209. doi:10.1007/s00464-007-9587-z
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 142:40–46. doi:10.1016/j.surg.2007.02.013
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231. doi:10.1097/01.sla.0000245832.59478.c6
Sajid MS, Ladwa N, Kalra L, Hutson K, Sains P, Baig MK (2012) A meta-analysis examining the use of tacker. Int J Surg 10:224–231. doi:10.1016/j.ijsu.2012.03.001
Novik B, Hagedorn S, Mork U-B, Dahlin K, Skullman S, Dalenback J (2006) Fibrin glue for securing the mesh in laparoscopic totally extraperitoneal inguinal hernia repair: a study with a 40-month prospective follow-up period. Surg Endosc 20:462–467. doi:10.1007/s00464-005-0391-3
Fränneby U, Gunnarsson U, Andersson M, Heuman R, Nordin P, Nyrén O, Sandblom G (2008) Validation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg 95:488–493. doi:10.1002/bjs.6014
Tam K-W, Liang H-H, Chai C-Y (2010) Outcomes of staple fixation of mesh versus nonfixation in laparoscopic total extraperitoneal inguinal repair: a meta-analysis of randomized controlled trials. World J Surg 34:3065–3074. doi:10.1007/s00268-010-0760-5
Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S (2008) Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc 22:757–762. doi:10.1007/s00464-007-9510-7
Staarink M, Veen RN, Hop WC, Weidema WF (2008) A 10-year follow-up study on endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc 22:1803–1806. doi:10.1007/s00464-008-9917-9
Messenger DE, Aroori S, Vipond MN (2010) Five-year prospective follow-up of 430 laparoscopic totally extraperitoneal inguinal hernia repairs in 275 patients. Ann R Coll Surg Engl. doi:10.1308/003588410X12628812458455
Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg 249:33–38. doi:10.1097/SLA.0b013e31819255d0
Sajid MS, Ladwa N, Kalra L, McFall M, Baig MK, Sains P (2013) A meta-analysis examining the use of tacker mesh fixation versus glue mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 206:103–111. doi:10.1016/j.amjsurg.2012.09.003
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty. Ann Surg 242:670–675. doi:10.1097/01.sla.0000186440.02977.de
Khaleal F, Berney C (2011) The role of fibrin glue in decreasing chronic pain in laparoscopic totally extraperitoneal (TEP) inguinal hernia repair: a single surgeon’s experience. ANZ J Surg 81:154–158. doi:10.1111/j.1445-2197.2010.05438.x
Birk D, Hess S, Garcia-Pardo C (2013) Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia 17:313–320. doi:10.1007/s10029-013-1053-3
Ferzli GS, Frezza EE, Pecoraro AM Jr (1999) Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg 188(5):461–465
Khajanchee YS, Urbach DR, Swanstrom LL, Hansen PD (2001) Outcomes of laparoscopic herniorrhaphy without fixation of mesh to the abdominal wall. Surg Endosc 15:1102–1107. doi:10.1007/s004640080088
Messaris E, Nicastri G, Dudrick SJ (2010) Total extraperitoneal laparoscopic inguinal hernia repair without mesh fixation: prospective study with 1-year follow-up results. Arch Surg 145(4):334–338
Pankaj Garg MI (2009) Laparoscopic total extraperitoneal repair in femoral hernia without fixation of the mesh. J Soc Laparoendosc Surg 13:597–600. doi:10.4293/108680809X12589999537995
Bansal VK, Misra MC, Babu D, Victor J, Kumar S, Sagar R, Rajeshwari S, Krishna A, Rewari V (2013) A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc 27:2373–2382. doi:10.1007/s00464-013-2797-7
Eklund A, Montgomery A, Bergkvist L (2010) Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg 97(4):600–608. doi:10.1002/bjs.6904
Koch CA, Greenlee SM, Larson DR, Harrington JR, Farley DR (2006) Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. J Soc Laparoendosc Surg 10(4):457–460
Phillips EH, Arregui M, Carroll BJ, Corbitt J, Crafton WB, Fallas MJ, Filipi C, Fitzgibbons RJ, Franklin MJ, McKernan B (1995) Incidence of complications following laparoscopic hernioplasty. Surg Endosc 9:16–21
Liem MS, van Duyn EB, van der Graaf Y, van Vroonhoven TJ, Coala Trial Group (2003) Recurrences after conventional anterior and laparoscopic inguinal hernia repair: a randomized comparison. Ann Surg 237(1):136–141
Choy C, Shapiro K, Patel S, Graham A, Ferzli G (2004) Investigating a possible cause of mesh migration during totally extraperitoneal (TEP) repair. Surg Endosc 18:523–525. doi:10.1007/s00464-003-8183-0
Ali SM, Zendejas B, Yadav S, Hernandez-Irizarry RC, Lohse CM, Farley DR (2013) Predictors of chronic groin discomfort after laparoscopic totally extraperitoneal inguinal hernia repair. J Am Coll Surg 217:72–78. doi:10.1016/j.jamcollsurg.2013.03.005 (discussion 78–80)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr SG and Dr PM have no competing interests or financial ties to disclose.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Statement of human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was indeed obtained from all individual participant included in the study.
Rights and permissions
About this article
Cite this article
Golani, S., Middleton, P. Long-term follow-up of laparoscopic total extraperitoneal (TEP) repair in inguinal hernia without mesh fixation. Hernia 21, 37–43 (2017). https://doi.org/10.1007/s10029-016-1558-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1558-7