Abstract
Purpose
Traumatic diaphragm rupture is a rare trauma that is easily overlooked. A missed diagnosis would result in chronic traumatic diaphragmatic herniation (CTDH). Surgical repair is the standard treatment that is conventionally performed by laparotomy or thoracotomy. Laparoscopic repair has been reported, but its efficacy remains controversial. In this study, we present our novel technique and experience of laparoscopic repair of CTDH and analyze the feasibility and effectiveness of this procedure.
Methods
We conducted a prospective collection with retrospective review of patients with CTDH treated at Chang Gung Memorial Hospital, Taiwan, from 2000 to 2013. The demographic characteristics, surgical procedure, perioperative results, length of hospital stay (HLOS) and follow-up were record and analyzed.
Results
There were 114 patients with traumatic diaphragm hernia, and 24 of them had CTDH with a mean age of 54.9 ± 13.3 years. The HLOS was 15.08 ± 8.17 days. Regarding the surgical method used, 19 patients had open surgery, and 5 patients underwent laparoscopic surgery. The demographic distribution, trauma mechanism, location and size of CTDH were comparable. In the laparoscopic group, the patients had a shorter median HLOS (6 days) than in the open surgery group (16 days; p = 0.002). There was no mortality or recurrence in both groups.
Conclusions
In this study and literature review, patients had laparoscopic repair with a smooth recovery. Laparoscopy provides good surgical exposure, allowing easy repositioning of the herniated content and a smooth repair of the defect without the morbidity of laparotomy. For CTDH, with caution, we can apply this technique with an acceptable result.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diaphragmatic injury remains a challenge in trauma settings and accounts for approximately 1 % of all torsal trauma patients [1, 2]. Although the diagnostic technology has advanced, there are still 9–41 % of patients with a missed diagnosis [3–7]. Due to symptomatic silencing and spontaneous hemostasis, these patients might be overlooked and might be delayed in being diagnosed for months, even years, after the initial traumatization [8, 9]. The gradient of pressure between the thoracic and abdominal cavity can enlarge the defect of the diaphragm, leading to chronic traumatic diaphragmatic herniation (CTDH) [1, 2]. Herniation of abdominal organs might remain asymptomatic for years after the trauma, and only in a few cases presenting with acute gastrointestinal and cardiopulmonary symptoms [10]. High mortality has been reported if patients have strangulated viscera in CTDH [2, 11].
Surgical repair is the standard management of diaphragmatic injury, and should be applied as soon as the diagnosis is confirmed. Conventionally, this injury is repaired by laparotomy or thoracotomy. With the improvement in instruments and familiarity of minimally invasive surgery, diagnostic laparoscopy has been advocated in recent years [5]. However, the therapeutic usage of the laparoscopic procedure for diaphragmatic injury remains infrequent. However, CTDH is somewhat different from the acute injury. CTDH induces intense fibrosis and severe adhesion, which leads to difficulty in the reduction of the herniated viscera and repair of the diaphragmatic defect. Therefore, limited experiences have been published about laparoscopic repair for CTDH [1, 3, 9, 12].
In this study, we present our experience with laparoscopic repair of CTDH and review the current literature to evaluate the feasibility and safety of laparoscopic repair of CTDH.
Materials and methods
Study population
We conducted a prospective data collection from the Trauma Registry at Chang Gung Memorial Hospital (CGMH), Linkou, Taiwan, which is a Level I trauma center in Taiwan. Demographic data, medical, perioperative and hospital course, follow-up and information regarding complications were recorded into a computerized database prospectively. By the diagnostic timing of TDH, we identified CTDH as the diagnosis of traumatic diaphragm herniation after the same admission of the injury episode. We performed a retrospective review of all patients with CTDH who were treated at our institute from January 2000 to December 2013. The study was approved by the Internal Review Board of CGMH.
All of the patients were managed by the trauma team from the emergency bay arrival to discharge. All of the management utilized the same clinical protocol. Demographic information was collected with the results of physiological and biochemical data and imaging findings. In addition, the herniation side, time to diagnosis and associated injury were recorded. All of the patients with traumatic diaphragm herniation were enrolled into the standard protocol (Fig. 1). The surgical method (open or laparoscopic surgery), operative time and perioperative recovery were recorded.
The post-operative recovery time, complications, and length of hospital stay (HLOS) were collected. All of the patients were followed-up in the outpatient department, and associated complications or sequelae were collected. The follow-up time was from the date of emergency department arrival to 31 December 2014. We excluded patients without a definite diagnosis of TDH or lost to follow-up. Furthermore, the data set was further limited by age to include patients older than 17 years. Patients who had congenital hernia or an intact diaphragm were excluded from this series.
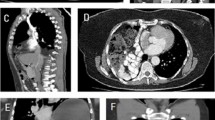
Surgical procedure: the pledgeted suture method
During the operation, the patient was placed in the supine position under general anesthesia, and a nasogastric tube and Foley tube were inserted. To prevent possible tension pneumothorax, the chest tube was prepared. A 10-mm subumbilical incision was made. A 10-mm visible trocar was inserted in the incision, and then a 30° rigid 10-mm videoscope was inserted. The pneumoperitoneum was increased to 12 mm Hg. One 5-mm port was created at the subxiphoid area at the proper height. Another 5-mm port was inserted at the left or right pararectus line at the proper height under direct visualization (Fig. 1). Next, the herniated viscera were explored, and the abdominal cavity was examined. The adhesion and fibrosis were dissected with an ultrasonic device, and then the hernia was reduced with blunt forceps. The fibrotic and fragile tissue at the edge of the diaphragm was removed, and then the size of the diaphragm defect was measured. After dissection and removal of the fibrotic edge, the pneumoperitoneum was reduced to 9 mm Hg to facilitate reapproximation of the edges of the diaphragm. Furthermore, an Fr.12 Pigtail drainage was inserted at the sixth intercostal space under the laparoscopic guidance before closure of the diaphragm.
The pledgeted suture method was applied for CTDR repair. Several double-armed 2-0 nonabsorbable braided polyester sutures with tiny Teflon pledgets were placed 1 cm from the edge of the diaphragm. Next, the knots were tied on the pledgets to compress the diaphragmatic edges together on the abdominal side of the diaphragm (Fig. 2b, arrow, pledgeted suture method the diaphragmatic edges were hold between two pledgets). Finally, the defect was closed gradually (Fig. 2c).
The laparoscopic pledgeted suture procedure to repair the chronic traumatic diaphragm hernia. a The large defect of the left diaphragm measures 8 × 5 cm, and the edge and herniated viscera were clear and reduced. b Interrupted sutures were applied on both edges of the defect. The suture sites were 1 cm from the edge with pledgets to prevent further tear of diaphragm tissue. After these sutures were applied on both sides, the ties were secured smoothly, and both edges of the defect were pinched together slowly. c After suture, the defect was closed under this method without obvious limitation
Statistical analysis
Fisher’s exact test was used as appropriate to compare categorical variables. Quantitative variables were compared using the Mann–Whitney U test. The odds ratios and 95 % confidence intervals were calculated by logistic regression in the case of qualitative variables and by linear regression for quantitative ones. Statistical analysis was performed using SPSS v 20.0 for Macintosh (SPSS, Inc., Chicago, IL, USA). A p value less than 0.05 was considered statistically significant.
Results
Study population
There were 114 patients with traumatic diaphragm hernia, and 24 of them had CTDH. The cohort consisted of 24 patients: 20 males (83.3 %) and 4 females (16.7 %). The mean age was 54.9 ± 13.3 years. Seventeen patients (70.8 %) were injured due to a vehicle collision, and six patients (25.0 %) were injured due to a fall. Seventeen patients had left side diaphragmatic herniation, and six patients had right side diaphragmatic herniation. There was one patient with a diaphragmatic defect on both sides. The ICU LOS was 2.79 ± 2.78 days, and the HLOS was 15.08 ± 8.17 days. Five patients had post-operative complications (20.8 %).
By the surgical method, 19 patients were divided into the open surgery group, and the other 5 patients were included in the laparoscopic surgery group. There was no obvious difference in age, gender, trauma mechanism, or location of herniation between both groups (Table 1). The median length (10.0 cm, 3.0–15.0 cm vs. 8 cm, 5.0–12.0 cm, p = 0.914) and area (20.0 cm2, 9.0–45.0 cm2 vs. 30.0 cm2, 15.0–48.0 cm2, p = 0.914) of herniation were similar between the open and laparoscopic groups, respectively. In the laparoscopic group, the patients had a shorter HLOS (6 days, 6–9 days) than in the open surgery group (16 days, 6–39 days) with a significant difference (p = 0.002). There was no recurrence or mortality in this cohort.
Discussion
In this series, 10.5 % of patients with a diaphragmatic injury developed CTDH, a finding that was comparable in the previous literature. Minimal invasive surgery has been adopted in the repair of diaphragmatic herniation because of decreased tissue trauma and a rapid recovery. Thoracoscopic repair for a missed diaphragmatic injury has been described [13]. However, thoracoscopy requires a double lumen endotracheal tube intubation. Furthermore, it might just allow the repair of small lesions and might limit the evaluation of the abdominal cavity [14, 15]. Laparoscopy is the method of choice because it allows for intraabdominal examination and massive reduction of herniated viscera. Several reports have been published to prove the efficiency of laparoscopy in acute diaphragmatic trauma [5, 16]. Unlike acute injuries, the long-standing nature of the hernia results in a substantial defect with possible extensive adhesion between the diaphragm and herniated viscera and between the herniated structures themselves [6, 7]. The surgical difficulty and complications in CTDH were increased compared with acute injury. Consequently, limited studies have been reported on laparoscopic repair for CTDH (Table 2). We presented our experience with laparoscopic repair for CTDH. Compared with open surgery, laparoscopic repair for CTDH showed a quick recovery and decreased HLOS with statistical significance. After a median follow-up of 16 months (range 6–24 months), there was no recurrent event. The safety and feasibility of laparoscopic repair for CTDH were acceptable.
In CTDR, viscera hernia with severe adhesion is commonly encountered, which obscures the dissection planes and normal anatomic landmarks. Proper dissection of the hernia sac to prevent injury to the surrounding viscera and to remove the fibrotic tissue will exacerbate the defect. Therefore, primary repair or placement with a synthetic mesh remains controversial in the laparoscopic repair of CTDH. Primary approximation and simple suture have been reported to easily tear tissue [3, 12], and synthetic mesh placement was advised for CTDH [17, 18]. However, erosion of the bowel and adjacent structures has been reported [3]. Moreover, the formation of fistulas and migration of the prosthesis used were other complications after mesh placement [10]. According to our experience, we applied the pledgeted suture method to compress and approximate the edge of the diaphragm together and release the shearing force when applying ties. By helping to reduce the pressure of the pneumoperitoneum to 9 mm Hg, we could re-approximate the edge of the diaphragm more easily. The edges of the defect often become fibrotic and fragile in CTDR [3]. Careful debridement of the fibrotic tissue and placement of the suture at the healthy diaphragm are essential to prevent tissue breakdown and hernia recurrence [1, 18]. Incorrect creation of shear and compressive forces would cause cutting-through and deformation of the fragile diaphragmatic tissue during suture placement. We recommend using double-armed suture placement at 1 cm from the edge to hold the healthy tissue. Compressing the diaphragmatic tissue between pledgets could prevent unnecessary shearing force. Furthermore, the knots tied on the pledgets could redistribute the shearing force from the diaphragm to the pledgets, reducing the possibility of tissue failure. Without placement of the mesh, possible adhesion, infection or migration can be prevented. All of our patients had a diaphragm defect more than 25 cm2 that could be repaired using this method without infection or symptomatic adhesion. Until now, no patient had recurrence after operation whether in the open or laparoscopy group; therefore, we recommend our method to repair CTDH under laparoscopic surgery.
Seventeen studies have been published concerning the laparoscopic repair of CTDH [3, 6–10, 12, 14, 17–25]. Most of the authors reported single or limited case reports. Because CTDH was rare, no conclusion could be drawn about an optimal therapeutic option. We summarized these studies in Table 2. Most of the CTDHs occurred or became symptomatic remote from the initial trauma. The laparoscopic repair of CTDH can be carried out without intraoperative hypoxemia, tension pneumothorax or increased peak airway pressures according to the available literature. Two cases were converted to open surgery due to difficulty in identifying the defect completely [3]. Most of the surgeons (n = 18, 60.0 %) used direct suture for repair, and 30 % of the surgeons placed a synthetic mesh. Some of them used both methods simultaneously (10 %). There was still no consensus regarding which method is superior. Most of the patients recovered smoothly, and the mean HLOS was 6.5 ± 3.8 days. The long-term results were favorable after a mean follow-up of 15.1 ± 11.9 months, and no recurrence was indicated during the follow-up. From this series and past experience, we could confirm the feasibility of laparoscopic repair of CTDH. Laparoscopic repair offered an acceptable HLOS (6.5 ± 3.8 days) without recurrent herniation after a long-term follow-up. Although the complication rate was approximately 6.9 %, however, most of them were grade I–II complications, which need no further intervention. The efficacy and safety of laparoscopic repair of CTDH should be established.
Although laparoscopic repair for CTDR seems to be feasible, there were several considerations that need to be emphasized. Because of the rarity of CTDH, a limited case number comprised this cohort, limiting the power of analysis. There was no recurrence noted in this series and previous works; however, long-term follow-up might be obtained in the future. Regarding the surgical technique, during the creation of pneumoperitoneum, the inflation should proceed slowly with caution to prevent rapid airflow into the thoracic cavity and tension pneumothorax. The surgeons and anesthesiologists should have a suspicion if the patients were hemodynamically unstable during inflation. The cessation of inflation and chest drain insertion might be considered.
In this study, our patients had laparoscopic repair uneventfully and recovered smoothly. Laparoscopy provides good orientation and surgical exposure of both the abdominal and thoracic cavity through the defect, allowing easy repositioning of the herniated content in the abdomen without the morbidity of laparotomy or thoracotomy. For CTDR, with caution, we can apply this technique with an acceptable result.
References
Thoman DS, Hui T, Phillips EH (2002) Laparoscopic diaphragmatic hernia repair. Surg Endosc 16:1345–1349. doi:10.1007/s00464-001-8162-2
Lewis JD, Starnes SL, Pandalai PK et al (2009) Traumatic diaphragmatic injury: experience from a level I trauma center. Surgery 146:578–584. doi:10.1016/j.surg.2009.06.040
Matthews BD, Bui H, Harold KL et al (2003) Laparoscopic repair of traumatic diaphragmatic injuries. Surg Endosc 17:254–258. doi:10.1007/s00464-002-8831-9
Liao C-H, Hsu C-P, Kuo I-M et al (2013) Factors affecting outcomes in penetrating diaphragmatic trauma. Int J Surg 11:492–495. doi:10.1016/j.ijsu.2013.03.014
Friese RS, Coln CE, Gentilello LM (2005) Laparoscopy is sufficient to exclude occult diaphragm injury after penetrating abdominal trauma. J Trauma 58:789–792
Schneider C, Tamme C, Scheidbach H et al (2000) Laparoscopic management of traumatic ruptures of the diaphragm. Langenbecks Arch Surg 385:118–123
Latic F, Delibegovic S, Latic A et al (2010) Laparoscopic repair of traumatic diaphragmatic hernia. Med Arh 64:121–122
Baldwin M, Dagens A, Sgromo B (2014) Laparoscopic management of a delayed traumatic diaphragmatic rupture complicated by bowel strangulation. J Surg Case Rep 2014. doi:10.1093/jscr/rju073
Andreev AL, Protsenko AV, Globin AV (2010) Laparoscopic repair of a posttraumatic left-sided diaphragmatic hernia complicated by strangulation and colon obstruction. JSLS 14:410–413. doi:10.4293/108680810X12924466006648
Fiscon V, Portale G, Migliorini G, Frigo F (2011) Laparoscopic repair of intrathoracic liver herniation after traumatic rupture of the diaphragm. Surg Endosc 25:3423–3425. doi:10.1007/s00464-011-1721-2
Shah R, Sabanathan S, Mearns AJ, Choudhury AK (1995) Traumatic rupture of diaphragm. ATS 60:1444–1449. doi:10.1016/0003-4975(95)00629-Y
Wadhwa A, Surendra JBK, Sharma A et al (2005) Laparoscopic repair of diaphragmatic hernias: experience of six cases. Asian J Surg 28:145–150. doi:10.1016/S1015-9584(09)60281-5
Ahmed N, Jones D (2004) Video-assisted thoracic surgery: state of the art in trauma care. Injury 35:479–489. doi:10.1016/S0020-1383(03)00289-4
Rashid F, Chakrabarty MM, Singh R, Iftikhar SY (2009) A review on delayed presentation of diaphragmatic rupture. World J Emerg Surg 4:32. doi:10.1186/1749-7922-4-32
Shaw JM, Navsaria PH, Nicol AJ (2003) Laparoscopy-assisted repair of diaphragm injuries. World J Surg 27:671–674. doi:10.1007/s00268-003-6747-8
Murray JA, Demetriades D, Asensio JA et al (1998) Occult injuries to the diaphragm: prospective evaluation of laparoscopy in penetrating injuries to the left lower chest. J Am Coll Surg 187:626–630
Pross M, Manger T, Mirow L et al (2000) Laparoscopic management of a late-diagnosed major diaphragmatic rupture. J Laparoendosc Adv Surg Tech A 10:111–114
Shah S, Matthews BD, Sing RF, Heniford BT (2000) Laparoscopic repair of a chronic diaphragmatic hernia. Surg Laparosc Endosc Percutan Tech 10:182–186
Campos LI, Sipes EK (1991) Laparoscopic repair of diaphragmatic hernia. J Laparoendosc Surg 1:369–373
Rasiah KK, Crowe PJ (1995) Laparoscopic repair of a traumatic diaphragmatic hernia. J Laparoendosc Surg 5:405–407
Slim K, Bousquet J, Chipponi J (1998) Laparoscopic repair of missed blunt diaphragmatic rupture using a prosthesis. Surg Endosc 12:1358–1360
Domene CE, Volpe P, Santo MA et al (1998) Laparoscopic treatment of traumatic diaphragmatic hernia. J Laparoendosc Adv Surg Tech A 8:225–229
Matz A, Landau O, Alis M et al (2000) The role of laparoscopy in the diagnosis and treatment of missed diaphragmatic rupture. Surg Endosc 14:537–539
Meyer G, Hüttl TP, Hatz RA, Schildberg FW (2000) Laparoscopic repair of traumatic diaphragmatic hernias. Surg Endosc 14:1010–1014
Torresini G, Sozio L, Crisci R, Amicucci G (2000) Laparoscopic repair of diaphragmatic iatrogenic hernia. Endoscopy 32:S2
Acknowledgments
The authors thank F.-P. Kuo, C.-J. Chen and H.-F. Tien as Members of the CGMH Trauma Registry Databank, which is acknowledged for its contribution to data collection of the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of our authors have no conflict of interest or financial ties to disclose.
Additional information
C.-H. Liao and C.-H. Chu have equally contributed to this manuscript.
Rights and permissions
About this article
Cite this article
Liao, CH., Chu, CH., Wu, YT. et al. The feasibility and efficacy of laparoscopic repair for chronic traumatic diaphragmatic herniation: introduction of a novel technique with literature review. Hernia 20, 303–309 (2016). https://doi.org/10.1007/s10029-015-1405-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-015-1405-2