Abstract
Oligodendroglioma, IDH-mutant and 1p/19q-codeleted is known for their relative chemosensitivity and indolent clinical course among diffuse gliomas of adult type. Based on the data from phase 3 clinical trials, the standard of post-surgical care for those tumors is considered to be initial chemoradiotherapy regardless of histopathological grade, particularly with PCV. However, partly due to its renewed definition in late years, prognostic factors in patients with those tumors are not well established. Moreover, the survival rate declines over 15 years, with only a 37% OS rate at 20 years for grade 3 tumors, even with the current standard of care. Given that most of this disease occurs in young or middle-aged adults, further improvements in treatment and management are necessary. Here, we discuss prognostic factors, standard of care and chemotherapy, and future perspectives with neoadjuvant strategy in those tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and overview
Oligodendroglioma is among the subtypes of adult-type diffuse glioma, and has been defined in the past based on histological characteristics such as round nuclei, honeycomb structure, and chicken-wire vasculature. In the pioneering era of molecular elucidation of brain tumors, codeletion of chromosome arms of 1p and 19q had been predominantly found in those tumors, and its reported correlation with chemosensitivity and favorable prognosis in anaplastic oligodendrogliomas has heralded the molecular classification of brain tumors [1, 2]. As a result, oligodendroglioma is now defined as diffuse glioma with both codeletion of 1p and 19q and mutation in the IDH 1 or 2 gene [3, 4]. Those tumors are known for their relatively favorable prognosis among diffuse gliomas, with retrospective studies reporting median OS of 12–16 years for grade 2, 5–10 years for grade 3 [5,6,7], and 13–14 years for grade 3 tumors treated with current standard of care [8]. However, the survival rate of patients with oligodendroglioma continuously declines over 15 years. Because the peak incidence of those tumors is in thirties to forties, improvement of the long-term survival rate and functional preservation in that period would be the issue to be challenged from now on. In this article, oligodendroglioma and astrocytoma indicate those defined based on WHO 2021, i.e., the former with IDH mutation and 1p19q codeletion, and the latter with IDH mutation, if not specifically designated.
Prognostic factors for oligodendroglioma
In general, diffuse gliomas have been established to be associated with several prognostic factors, such as younger age, better KPS, tumor resection rate, and histological grade. However, because of the recent definition of molecular oligodendroglioma, and thereby lack of the results of clinical trials, prognostic factors within those tumors have not been well elucidated. Only a few retrospective analyses on the prognostic factors in IDH-mutant and 1p19q-codeleted oligodendroglioma are available.
Multidimensional scaling analysis of the datasets of The Cancer Genome Atlas (TCGA) showed that both younger age (< 45 years) and better KPS (≥ 90) were significantly associated with improved OS in the multivariate analysis within grade 2 or 3 oligodendrogliomas [6]. The Prise en charge des Oligodendrogliomes Anaplasiques (POLA) network in France was a program for standardizing the management of histologically defined de novo grade 3 oligodendroglioma in adults, and the 1p/19q-codeleted cases had been strongly recommended to be treated by radiotherapy only (the standard of post-surgical care at that time) or included in the CODEL (Alliance-N0577; EORTC-26081/22086; NRG-1071; NCIC-CEC-2) clinical trial. Retrospective analyses of the POLA network cohort showed that among the 1p/19q-codeleted grade 3 oligodendrogliomas, OS was associated with younger age, but not KPS [9, 10] (Table 1).
The extent of tumor resection (ETR) and postsurgical residual tumor volume were shown to be one of the most important prognostic factors in diffuse gliomas. However, the impact of those appears different between molecular subtypes in lower grade gliomas (LrGG), with the strongest impact in astrocytoma, IDH-mutant. In IDH-mutant and 1p/19q-codeleted oligodendroglioma, the impact of resection was shown to be less strong. Retrospective analyses in the patients with grade 2 diffuse gliomas defined by WHO2016 in two center hospitals in Netherlands, showed that there was a trend towards better OS with more extensive resection in oligodendrogliomas (IDHmut and 1p/19qcodel), however, the trend was not statistically significant [11]. In contrast, post-surgical tumor volume was significantly associated with OS in astrocytomas (IDHmut), with any residual tumor showing negative impact for OS [11]. A single-institution study on LrGGs defined by WHO2016 showed that a larger percentage of resection was associated with improved OS in both oligodendrogliomas (IDHmut and 1p/19qcodel) (p = 0.01) and astrocytomas (IDHmut) (p = 0.0020) after adjustment for age, tumor grade, and therapy [12]. Among the three LrGG molecular subtypes, oligodendrogliomas are the most responsive to chemotherapy and radiotherapy; therefore, tumor resection might be less important in these tumors. However, it should be noted that many studies suggested a trend towards improved OS with more extensive resection in oligodendrogliomas, and a lesser ETR and a larger post-surgical residual volume are considered to be a negative prognostic factors across gliomas of all grades and subtypes [13].
Although the clear cutoff for distinction between grade 2 and 3 oligodendrogliomas has not been defined in WHO2021 as well as in WHO2016, brisk mitotic activity (i.e., ≥ 6 mitoses/10 HPF), microvascular proliferation (MVP), and necrosis have been suggested of particular importance as indicators of grade 3 oligodendrogliomas [3, 4]. In literature, the significance of histological grade on patient prognosis has been controversial in IDH-mutant LrGGs, particularly in oligodendrogliomas. In fact, a large comprehensive retrospective study on a Japanese cohort showed no significant difference in OS between grade 2 and 3 oligodendrogliomas [14]. On the other hand, a study on TCGA datasets and a retrospective study in Italy showed significantly better OS in grade 2 than in grade 3 oligodendrogliomas [5, 6]. A multivariate Cox regression analysis in 483 grade 3 oligodendrogliomas (IDHmut and 1p/19qcodel) demonstrated that older age and the presence of CDKN2A homozygous deletion, which was found in 7% (33/483) of the cohort, were independently associated with shorter OS [10]. Among the histological features, the presence of MVP and/or necrosis was predictive of poor prognosis, but only in cases that lacked CDKN2A homozygous deletion.
These data based on the retrospective studies suggested that the younger age (cutoff 45–50 y/o) might be favorable prognostic factor in oligodendrogliomas. The prognostic value of the other reported factors might prove with long-term follow-up of the uniformly treated cohorts. Molecular-histological criteria that delineate cases with poor prognosis is awaited.
Standard of care and chemotherapy for oligodendrogliomas
Three randomized phase 3 studies that compared radiotherapy with PCV and radiotherapy alone showed the superiority of chemoradiotherapy in the entire cohort of grade 2 or 3 diffuse gliomas [15,16,17]. The RTOG9802 trial on high-risk diffuse grade 2 gliomas and the RTOG9402 and EORTC 26951 trials on histologically defined grade 3 oligodendroglial tumors were designed and performed based on histological definition, because the significance of IDH mutations and 1p/19q codeletion has not been established when these trials were launched. Importantly, posthoc genomic analyses demonstrated that tumors with 1p/19q codeletion were associated with significantly prolonged OS regardless of treatment, and that the addition of PCV significantly improved not only PFS but also OS in patients with 1p/19q-codeleted tumors [15, 16, 18]. Although these findings were based on posthoc analyses, all three studies showed similar results, thereby, validating the findings and defining the current standard of care for oligodendrogliomas [13, 19]. Initial chemoradiotherapy was shown to be far more effective than sequential treatment (i.e., radiotherapy first and chemotherapy upon progression) [20], radiotherapy alone is no longer recommended as the initial treatment for oligodendrogliomas.
The intergroup CODEL trial was designed for newly diagnosed grade 3 gliomas with 1p/19q codeletion (i.e., grade 3 oligodendrogliomas), and original design included 3 treatment arms; radiotherapy alone, radiotherapy with concomitant and adjuvant temozolomide (up to 12 cycles), and temozolomide alone (5/28 day schedule, up to 12 cycles) [21]. Importantly, a major amendment in the trial design was conducted twice. First, the radiotherapy alone arm was replaced by radiotherapy followed by PCV, based on the results of RTOG9402 and EORTC26951. Later, analyses of the patients enrolled in the original CODEL design showed that patients treated with temozolomide alone was associated with significantly inferior PFS than those treated with radiotherapy-containing arms (pooled analysis) (PFS temozolomide alone arm: 2.9 y, radiotherapy-containing arms: not reached, HR 3.12, p = 0.009) [21]. Although the OS comparison was underpowered, the 5-year OS rate was 67% in the temozolomide arm, and 91% in the radiotherapy containing arms. These findings and previously reported data, which will be discussed in the following paragraph, led to the drop of the temozolomide alone arm (second amendment). Then, CODEL was redesigned to compare radiotherapy followed by PCV (up to 6 cycles) and radiotherapy with concomitant and adjuvant temozolomide (6–12 cycles) (NCT00887146), and has an ongoing enrollment of newly diagnosed adult grade 3 or high-risk grade 2 IDH-mutant and 1p/19q-codeleted oligodendrogliomas.
For the chemotherapy drugs, the reported PFS data favor PCV over temozolomide for oligodendrogliomas (Table 2) [7, 23,24,24]. A large retrospective analysis showed superior TTP in patients treated with PCV alone than in those treated with temozolomide alone (p = 0.0186) in grade 3 1p/19q-codeleted oligodendrogliomas [7]. In NOA04, which was a randomized phase 3 trial in grade 3 gliomas that compared radiotherapy alone and chemotherapy alone, the chemotherapy alone arm was further randomized 1:1 to PCV or temozolomide [25]. In the prospectively treated cohort, subgroup analysis demonstrated superior PFS (p = 0.0254) and OS (p = 0.0689) in the PCV arm than in the temozolomide arm [22]. Moreover, some may have concerns on mutagenesis effect for temozolomide [26].
Although radiotherapy alone is not recommended for newly diagnosed oligodendrogliomas, chemotherapy alone, especially PCV alone, may be a reasonable treatment with encouraging PFS data in literature and carries the advantage of delaying radiotherapy (Table 2). The ongoing clinical trials that compare PCV alone with radiotherapy plus PCV are expected to preserve the cognitive function of patients with high-risk grade 2 (NCT04702581, POLO) and grade 3 (NCT02444000, POLCA) oligodendroglioma. Moreover, there is an ongoing randomized study comparing CCNU plus temozolomide combination chemotherapy (CETEG) with radiotherapy plus PCV for grade 2 and 3 oligodendrogliomas (NCT05331211, ImproveCodel).
In Japan, PAV is generally used instead of PCV because lomustine is unavailable [28,29,29]. There has been no clinical study comparing PAV with PCV. A meta analysis reported survival gain as a measure of efficacy of various nitrosoureas; survival gain was measured by comparing predicted OS with or without each drug after considering prognostic factors such as histological grade, age, and resection [30]. In the analysis, significant survival benefits were found only with lomustine (5.3 months) and nimustine (8.9 months).
Neoadjuvant strategy for the treatment of oligodendrogliomas
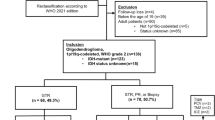
Preservation of brain function is critical, while the ETR is among the major prognostic factors in diffuse gliomas including oligodendrogliomas. Neoadjuvant chemotherapy is a strategy in which radical resection is performed after downstaging of cancer by chemotherapy and has been used in many cancers with the expectation of functional preservation without impairing OS. We have been treating oligodendrogliomas with the intent of a neoadjuvant strategy by predicting chemosensitivity based on 1p/19q codeletion, as follows: (1) if diffuse glioma is suspected based on imaging and clinical information, maximal safe resection is intended if possible; (2) for IDH-mutant and 1p/19q-codeleted oligodendroglioma, chemotherapy is given upfront in case of initial incomplete resection; and (3) for those with incomplete initial resection, a second-look resection is intended after decreasing tumor volume by chemotherapy (i.e., upfront chemotherapy and subsequent resection strategy) [27]. In cases that underwent initial resection for biopsy or that was partial, the median decrease rate in tumor volume after chemotherapy was − 35%. In fact, the strategy seemed beneficial at least in a subset of patients with long-term survival and functional preservation (Fig. 1). As of May 2023, the median PFS from the initiation of chemotherapy in 32 cases of oligodendroglioma (grade 2: 27 cases, grade 3: 5 cases), for which radiotherapy was deferred, was 6.8 years. Notably, in some of the cases for which second-look resection has been performed after chemotherapy, tumor relapse has not occurred for more than several years at resection margins where the extent of tumor was beyond there before chemotherapy (Fig. 1); this observation might suggest invading front of oligodendroglioma retracts by alkylating agent chemotherapy. In recent years, we routinely estimate tumor molecular subtype based on imaging characteristics before surgery by evaluating T2-FLAIR mismatch and 1p/19q score [31, 32], in order to personalize treatment of each patient before initial resection.
Serial FLAIR MRI showing an illustrative case treated with upfront chemotherapy and subsequent resection strategy. The tumor is located in the right precentral gyrus. A–C Before biopsy. D–G After biopsy and 12 courses of temozolomide. Note that the tumor, i.e., abnormal high intensity area on FLAIR images, was separated from the pyramidal tract, and became restricted into the face area of the precentral gyrus. H–K The FLAIR abnormality was completely resected with awake procedure. Tumor relapse has not occurred even at the medial resection margin where the extent of tumor was beyond there before chemotherapy (the dotted white circle in B), and the patient has been relapse free and KPS 100 for more than 13 years. (Reprinted from reference [27], Fig. 2)
Histopathological analyses were performed in 14 cases with paired pre and post chemotherapy oligodendrogliomas, comparing specimens resected following preoperative chemotherapy with those of initial resection [33]. The most frequent changes following chemotherapy were a spares glial cell background and abundant foamy cell infiltration (Fig. 2). Ki67 index was significantly decreased after chemotherapy. Importantly, the number and the ratio of M2 macrophage positive for CD163 and the ratio of putative glioma stem cells (GSCs) positive for nestin or CD133 to total tumor cells increased after chemotherapy [33]. Therefore, M2 macrophage and GSC might constitute the mechanism of resistance and recurrence after alkylating agent chemotherapy.
Histopathological findings in oligodendrogliomas after alkylating agent chemotherapy. A, C, E Hematoxylin and eosin (H&E) staining in the initial tumors. B, D, F H&E staining in the tumors resected after chemotherapy. Note that the glial fibrillar background is sparse as compared with that in the initial tumor. Black arrow in D indicates nuclear fragmentation and chromatin condensation. Foamy cell infiltration (black arrow in F) as well as gliosis with reactive astrocytes is conspicuous as compared with that in the initial tumor. A, B, E, F Original magnification × 200. C, D Original magnification × 400. (Reprinted from reference [33], Fig. 1)
Future perspectives with neoadjuvant strategy
As mentioned earlier, although oligodendrogliomas are known for their relatively indolent clinical course, the survival rate continuously declines over 15 years, with only a 37% OS rate at 20 years for grade 3 tumors, even with the current standard of care. Given that most cases occur in young or middle-aged adults, further improvement in treatment and management is clearly necessary. Owing to the lack of a medicine or immunotherapy for cure, staged resection using a neoadjuvant strategy may be one of the reasonable ways to achieve functional preservation by decreasing the resection volume and withholding radiotherapy. However, there are at least two reasons for not using the neoadjuvant strategy for the treatment for gliomas, even oligodendrogliomas. One is that biopsy, which is necessary for pathological examination before chemotherapy, requires either craniotomy or stereotactic procedure in most cases, and is not routinely performed in glioma management. In contrast, biopsy can be performed by less invasive procedure for cancers in other organs. For example, cancers in the gastrointestinal tract can be biopsied by endoscopic procedure, and breast cancers can be biopsied using local anesthesia. Moreover, because ETR is associated with patient prognosis, many neurosurgeons intend to perform maximal safe resection during craniotomy. The other reason is that the extent of tumor volume decrease by chemotherapy is less as compared with other cancers, even in oligodendrogliomas. For the former issue, prediction of tumor molecular signature by imaging features with artificial intelligence technology or development of less invasive, simplified automatic biopsy procedure may be among the promising approaches. For the latter issue, the use of novel medicines or combination therapy is anticipated to improve the extent of tumor volume decrease. Moreover, demonstration of benefit of initial biopsy by clinical trial would facilitate the initial biopsy and subsequent personalized treatment including neoadjuvant strategy for diffuse gliomas.
Abbreviations
- CDKN2A HD:
-
CDKN2A homozygous deletion
- EORTC:
-
European organization for research and treatment of cancer
- IDH:
-
Isocitrate dehydrogenase
- IDHmut:
-
IDH-mutant
- LGG:
-
Low grade glioma, i.e., grade 2 diffuse glioma, defined by WHO2016
- LrGG:
-
Lower grade gliomas, i.e., grade 2 or 3 diffuse gliomas, defined by WHO2016
- MVP:
-
Microvascular proliferation
- OS:
-
Overall survival
- PCV:
-
Procarbazine, CCNU (lomustine), and vincristine
- PAV:
-
Procarbazine, ACNU (nimustine), and vincristine
- PFS:
-
Progression free survival
- RTOG:
-
Radiation therapy oncology group
- TTP:
-
Time to progression
- WHO2016:
-
WHO Classification of Tumours. Central neuvous system tumours. Revised 4th Ed.
- WHO2021:
-
WHO Classification of Tumours. Central neuvous system tumours. 5th Ed.
- 1p/19qcodel:
-
1P/19q-codeleted
References
Cairncross JG, Ueki K, Zlatescu MC et al (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479
Ino Y, Betensky RA, Zlatescu MC et al (2001) Molecular subtypes of anaplastic oligodendroglioma: implications for patient management at diagnosis. Clin Cancer Res: Off J Am Assoc Cancer Res 7:839–845
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Ellison DW, Figarella-Branger D, Perry A, Reifenberger G, von Deimling A (2016) WHO classification of tumours of the central nervous system, 4th edn. International agency for research on cancer, Lyon
WHO Classification of Tumours Editorial Board (2021) Central nervous system tumours, 5th edn. International Agency for Research on Cancer, Lyon
Franceschi E, Tosoni A, Bartolini S et al (2020) Histopathological grading affects survival in patients with IDH-mutant grade II and grade III diffuse gliomas. Eur J Cancer 137:10–17
Cimino PJ, Zager M, McFerrin L et al (2017) Multidimensional scaling of diffuse gliomas: application to the 2016 World Health Organization classification system with prognostically relevant molecular subtype discovery. Acta Neuropathol Commun 5:39
Lassman AB, Iwamoto FM, Cloughesy TF et al (2011) International retrospective study of over 1000 adults with anaplastic oligodendroglial tumors. Neuro Oncol 13:649–659
Lassman AB, Hoang-Xuan K, Polley MC et al (2022) Joint final report of EORTC 26951 and RTOG 9402: phase III trials with procarbazine, lomustine, and vincristine chemotherapy for anaplastic oligodendroglial tumors. J Clin Oncol: Off J Am Soc Clin Oncol 40:2539–2545
Figarella-Branger D, Mokhtari K, Dehais C et al (2016) Mitotic index, microvascular proliferation, and necrosis define 3 pathological subgroups of prognostic relevance among 1p/19q co-deleted anaplastic oligodendrogliomas. Neuro Oncol 18:888–890
Appay R, Dehais C, Maurage CA et al (2019) CDKN2A homozygous deletion is a strong adverse prognosis factor in diffuse malignant IDH-mutant gliomas. Neuro Oncol 21:1519–1528
Wijnenga MMJ, French PJ, Dubbink HJ et al (2018) The impact of surgery in molecularly defined low-grade glioma: an integrated clinical, radiological, and molecular analysis. Neuro Oncol 20:103–112
Patel SH, Bansal AG, Young EB et al (2019) Extent of surgical resection in lower-grade gliomas: differential impact based on molecular subtype. AJNR Am J Neuroradiol 40:1149–1155
Weller M, van den Bent M, Preusser M et al (2021) EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol 18:170–186
Suzuki H, Aoki K, Chiba K et al (2015) Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet 47:458–468
Cairncross G, Wang M, Shaw E et al (2013) Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol: Off J Am Soc Clin Oncol 31:337–343
van den Bent MJ, Brandes AA, Taphoorn MJ et al (2013) Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin Oncol: Off J Am Soc Clin Oncol 31:344–350
Buckner JC, Shaw EG, Pugh SL et al (2016) Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med 374:1344–1355
Bell EH, Zhang P, Shaw EG et al (2020) Comprehensive genomic analysis in NRG oncology/RTOG 9802: a phase III trial of radiation versus radiation plus procarbazine, lomustine (CCNU), and vincristine in high-risk low-grade glioma. J Clin Oncol: Off J Am Soc Clin Oncol 38:3407–3417
National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology. Central Nervous System Tumours. (2023) https://www.nccn.org. Accessed 10 Jan 2024
van den Bent MJ (2014) Practice changing mature results of RTOG study 9802: another positive PCV trial makes adjuvant chemotherapy part of standard of care in low-grade glioma. Neuro Oncol 16:1570–1574
Jaeckle KA, Ballman KV, van den Bent M et al (2021) CODEL: phase III study of RT, RT + TMZ, or TMZ for newly diagnosed 1p/19q codeleted oligodendroglioma. Analysis from the initial study design. Neuro Oncol 23:457–467
Wick W, Roth P, Hartmann C et al (2016) Long-term analysis of the NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with PCV or temozolomide. Neuro Oncol 18:1529–1537
Taal W, van der Rijt CC, Dinjens WN et al (2015) Treatment of large low-grade oligodendroglial tumors with upfront procarbazine, lomustine, and vincristine chemotherapy with long follow-up: a retrospective cohort study with growth kinetics. J Neurooncol 121:365–372
Baumert BG, Hegi ME, van den Bent MJ et al (2016) Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol 17:1521–1532
Wick W, Hartmann C, Engel C et al (2009) NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol 27:5874–5880
Johnson BE, Mazor T, Hong C et al (2014) Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science (New York, NY) 343:189–193
Sasaki H, Hirose Y, Yazaki T et al (2015) Upfront chemotherapy and subsequent resection for molecularly defined gliomas. J Neurooncol 124:127–135
Hata N, Yoshimoto K, Hatae R et al (2016) Deferred radiotherapy and upfront procarbazine-ACNU-vincristine administration for 1p19q codeleted oligodendroglial tumors are associated with favorable outcome without compromising patient performance, regardless of WHO grade. Onco Targets Ther 9:7123–7131
Iwadate Y, Matsutani T, Hara A et al (2019) Eighty percent survival rate at 15 years for 1p/19q co-deleted oligodendroglioma treated with upfront chemotherapy irrespective of tumor grade. J Neurooncol 141:205–211
Wolff JE, Berrak S, Koontz Webb SE, Zhang M (2008) Nitrosourea efficacy in high-grade glioma: a survival gain analysis summarizing 504 cohorts with 24193 patients. J Neurooncol 88:57–63
Kanazawa T, Fujiwara H, Takahashi H et al (2019) Imaging scoring systems for preoperative molecular diagnoses of lower-grade gliomas. Neurosurg Rev 42:433–441
Patel SH, Poisson LM, Brat DJ et al (2017) T2-FLAIR mismatch, an imaging biomarker for IDH and 1p/19q status in lower-grade gliomas: a TCGA/TCIA project. Clin Cancer Res: Off J American Assoc Cancer Res 23:6078–6085
Kanazawa T, Ohara K, Kitamura Y et al (2021) Histopathological investigation of the 1p/19q-codeleted gliomas resected following alkylating agent chemotherapy. J Neurooncol 155:235–246
Acknowledgements
We thank very much for every support by corroborators in multiple institutions.
Funding
The present work was supported in part by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science [15K10343, 19K09490 to H.S.], and by research grant from Eisai Japan [HHCS20200922004 to H.S.].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HS received grant for clinical trial which was not related to the contents of the present work from Ono pharmaceutical. HS received research grant from Eisai pharmaceutical in 2020 and 2021, a part of which was used for histological study. The authors declare there is no conflict of interest concerning the contents of the present work.
Ethical approval
Treatment with neoadjuvant strategy and histopathological investigation were performed with approval by the institutional review board (20130250, 20050002).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sasaki, H., Kitamura, Y., Toda, M. et al. Oligodendroglioma, IDH-mutant and 1p/19q-codeleted-prognostic factors, standard of care and chemotherapy, and future perspectives with neoadjuvant strategy. Brain Tumor Pathol 41, 43–49 (2024). https://doi.org/10.1007/s10014-024-00480-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10014-024-00480-1