Abstract
The ability to recognize emotions evident in people’s faces contributes to social functioning and might be affected by ADHD and irritability. Given their high co-occurrence, we examined the relative contribution of ADHD and irritability to facial emotion recognition (FER). We hypothesized that irritability but not ADHD traits would predict increased likelihood of misrecognizing emotions as negative, and that FER performance would explain the association of ADHD and irritability traits with social skills. FER was measured using the Reading the Mind in the Eyes Test (RMET) in children (6–14 years old) referred for ADHD assessment (n = 304) and healthy controls (n = 128). ADHD, irritability and social skills were measured using parent ratings. We used repeated measure logistics regression, comparing the effects across emotion valence of images (i.e., neutral/positive/negative). High irritability but not ADHD diagnosis predicted lower RMET accuracy. ADHD traits predicted lower RMET accuracy in younger but not older participants, whereas irritability predicted poorer accuracy at all ages. ADHD traits predicted lower RMET accuracy across all emotion valences, whereas irritability predicted increased probability of misrecognizing neutral and positive but not negative emotions. Irritability did not increase the probability for erroneously recognizing emotions as negative. ADHD and irritability traits fully explained the association between RMET and social skills. ADHD and irritability traits might impact the ability to identify emotions portrayed in faces. However, irritability traits appear to selectively impair recognition of neutral and positive but not negative emotions. ADHD and irritability are important when examining the link between FER and social difficulties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ability to decode emotions expressed in human faces is central to successful social behavior [1]. Difficulty in face emotion recognition (FER) could explain at least some of the social problems that are common in children and youth with a diagnosis of attention-deficit/hyperactivity disorder (ADHD) [2,3,4,5]. The ability to sustain attention on a task and to optimally inhibit a response are impaired in children with ADHD. Nonetheless, executive functions may not be the only factor involved in children with ADHD’s difficulty in FER [6, 7].
Previous studies of FER in ADHD have not distinguished the effect of irritability traits, defined as proneness to anger, propensity for behavioral outbursts and negative emotional reactivity [8], from that of ADHD traits. This is a problem because high irritability is a common feature of children with ADHD [9, 10] negatively affecting 25–45% of this population when measured in the broader definition of emotional dysregulation [11]. Moreover, irritability is thought to predict social problems [12, 13] and is shown to predict difficulty in FER in particular [14,15,16,17]. Nevertheless, no study has examined the possible contribution of irritability to FER dysfunction observed in children and youth with ADHD.
Studies of children and adolescents with ADHD show a decrease in overall FER accuracy compared to normal controls [3, 18, 19]. Yet, none of these studies have investigated specific mechanisms that might cause the lower FER accuracy found in this population [2,3,4, 20,21,22,23]. The few studies that examined the association of ADHD and the identification of face emotions of specific valence show inconsistent results [4, 22, 24, 25]. In contrast, severe or chronic irritability in children and youth has been associated with altered performance across different emotion valences of the images [14, 15, 17, 26, 27] and with a tendency to interpret ambiguous emotions as reflecting a negative emotion such as anger rather than a positive one such as happiness [15, 26, 28]. These results suggest that irritability might be associated with a bias toward interpreting motional information from faces as reflecting negative emotions [29].
However, the direction of the association between irritability and social cognition is unclear, i.e., whether altered social information processing serves as an underlying mechanism responsible for the emergence of irritability traits [8], or vice versa [15, 26].
In this study, we examined the relative contribution of ADHD and irritability to FER ability in the same model. We hypothesized that both ADHD and irritability traits would predict lower accuracy in FER. We hypothesized that ADHD traits would predict poorer accuracy across all valences of emotions (i.e., neutral, positive and negative). We hypothesized that irritability traits would predict lower accuracy in recognizing positive or neutral rather than negative facial emotions and increased probability for erroneously recognizing emotions as negative (i.e., a bias toward negative emotions). Finally, there are many potential factors that might affect social functioning in children with ADHD or with high irritability [8, 30]. While it has been suggested that the ability to recognize emotions evident in people’s faces provides essential information for human social interaction, there are no data indicating whether FER deficits mediate the association between ADHD/irritability and social functioning. We predicted that FER accuracy would partially mediate the association of ADHD and irritability traits with social functioning.
Methods
Setting
Participants were children and their parents referred to an ADHD clinic in a tertiary care hospital as part of the Province of Ontario (Canada) Neurodevelopmental Disorders Network (POND), a collaboration of 4 medical centers [4]. Typically developing controls were recruited via advertisements of local hospitals. Participants did not take stimulants for 24 h prior to testing. Parents provided written informed consent and participants gave assent. All procedures were approved by the Research Ethics Board at participating institutions.
Study population
The sample consisted of individuals, 6 to 14 years of age (M = 10.1; SD = 2.3; 31.5% females), with a clinical diagnosis of ADHD (n = 304) and typically developing controls (n = 128). In-depth diagnostic assessment was performed using the Parent Interview for Child Symptoms (PICS) updated to correspond with DSM-5 criteria to confirm clinical diagnoses [31]. Twenty-two percent (n = 68) of the 304 participants had been referred for clinical assessment of ADHD and showed marked ADHD traits but did not meet criteria for ADHD diagnosis (Subthreshold ADHD. Table 1). Typically developing controls were born after 35 weeks gestation and did not have any neurological or psychiatric diagnoses, as confirmed through interview. Participants of both groups were excluded if they had a previous history or current diagnosis of intellectual disability, language disorder, autism spectrum disorder, obsessive–compulsive disorder, psychosis, bipolar disorder, or Full-Scale IQ < 80 (Table S1, Supplementary Information).
Exclusion from the study due to missing data is detailed in Table S1. Where only one or two items were missing, the total score was pro-rated to adjust for missing values by taking the average of non-missing items and multiplying by the total number of items in the given scale. SWAN-ADHD inattention and hyperactive/impulsive scores were pro-rated separately.
IQ was measured using either a full Wechsler Intelligence Scale for Children (WISC–IV n = 90 or WISC-V n = 33), or an abbreviated Wechsler Scale of Intelligence (WASI n = 6 or WASI-II n = 178). When the Full-Scale IQ was not considered to be valid due to a gap of > 15 points between the Verbal Comprehension Index (VCI) and the Perceptual Reasoning Index (PRI) Full scale IQ could not be determined. In these cases (n = 125), the VCI was used instead of the Full-Scale IQ based on studies showing that VCI may play a more important role in RMET accuracy than PRI in samples of children not diagnosed of Autism [32, 33]. Reliability of clinical assessments was ensured by pre-study training and monitoring of protocol fidelity via taped and in-person assessments.
Measures
Strengths and Weaknesses of ADHD Symptoms and Normal Behavior Rating Scale ADHD traits (SWAN-ADHD)
ADHD traits were measured by summing the scores on the Strengths and Weaknesses of ADHD Symptoms and Normal Behavior Rating Scale [34]. The SWAN-ADHD traits scale consists of the 18 DSM-5 ADHD items [e.g., “Give close attention to detail and avoid careless mistakes” and “Sit still (control movements of hands/feet or control squirming)”] rated on a 7-point scale ranging from − 3 (far below average) to 3 (far above average) about the participant over the past month (sum score could vary from − 54 to + 54). The SWAN-ADHD scores were reversed so that more positive scores correspond to higher ADHD traits. The internal consistency of the SWAN-ADHD scale as measured in this study using Cronbach’s α was 0.97.
Child Behavior Checklist (CBCL)-irritability traits
We measured irritability traits by summing the scores of 4 items from the Child Behavior Checklist (CBCL) of the Achenbach System of Empirically Based Assessment [35]. The items included in this scale were: “Stubborn, sullen or irritable”, “Sudden changes in mood or feelings”, “Temper tantrums or hot temper” [36], as well as “Sulks a lot”. The internal consistency of the irritability scale measured in our study using Cronbach’s α was 0.84.
Adaptive Behavior Assessment System II (ABAS-II)-social skills area
Social skills were measured with the parent reported Adaptive Behavior Assessment System II (ABAS-II) Social Skills Area scale [37]. This scale was designed to measure the child’s adaptive social skills using 23 items (e.g., “Keeps a stable group of friends” and “Shows sympathy for others when they are sad or upset.”) rated on a four-point scale ranging from 0 (Is not able to perform the task) to 3 (Always or almost always performs the task). The Social skills scale scores are standard scores with a norm referenced mean of 10 and standard deviation of 3.
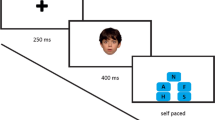
Reading the Mind in the Eyes Test (RMET)
Facial emotion recognition was examined using the children’s version of the Reading the Mind in the Eyes Test (RMET) [1]. RMET is used in children as from 6 years of age. Nonetheless, RMET accuracy is lower in younger age [32]. We controlled for age in all our analyses, so the residual effects would be related to the traits measured. Participants viewed 28 black-and-white images of eyes portraying different emotions and were instructed to select one out of four optional written descriptor that best matched the emotions portrayed. Written descriptors were reviewed with participants prior to testing and were present throughout testing. Data regarding the internal consistency of the children’s version of RMET are limited. Preliminary evidence suggested acceptable internal consistency, equivalent to the internal consistency levels measured in adults [38, 39]. The Cronbach’s α internal consistency of RMET in our study was 0.63. RMET items were classified as having one of three different valences (positive, negative, or neutral) as per previous studies [4] with the exception of 3 items which we re-categorized as suggestive of negative rather than neutral expressed emotions based on their face-validity prior to analysis of the data (items: “nervous”, “thinking about something sad”, and “not believing”).
Data analysis
RMET accuracy was modeled across individual items using repeated measures logistic regression, treating items as random effects. This model allows the inclusion of item-specific effects while modeling the proportion of correct responses on the task. Age, sex, IQ, and an age × IQ interaction were associated with RMET accuracy and were included as extraneous variables in all models of RMET accuracy. We first modeled the proportion of correct responses across diagnosis (Control, ADHD, and Subthreshold ADHD). To provide a simple descriptive summary, we further grouped participants according to their irritability trait scores into Low and High Irritability. High Irritability was calculated using a cut-off score of ≥ 5 on the CBCL-Irritability scale requiring at least one far above average response on the irritability items. Then we examined the correlates of the trait measures SWAN-ADHD and CBCL-Irritability scores. The emotional valence of the image (neutral, negative, or positive) was then added to the model along with an interaction term with SWAN-ADHD or CBCL-Irritability traits to determine if the effects of the trait measures varied across valences of the images. Where CBCL-Irritability was found to have an effect on RMET accuracy, error type was further classified into two groups, negative valence vs non-negative valence (i.e., positive or neutral) incorrect responses, to determine if a propensity toward selecting incorrect negative valence response options was responsible for the effect of irritability on RMET accuracy. Correct responses versus each of the two incorrect response types (negative valence and non-negative valence incorrect responses) were then modeled using a repeated measures nominal multinomial logistic regression model and the effect of irritability was compared between the two incorrect response types. Linear regression was used to predict scaled scores in the ABAS-II social skills area (n = 396). Although the normed scores are ordinal with a restricted range of possible values, after controlling for covariates, the residuals were found to be normally distributed, meeting the assumptions of the linear regression model. An α value of 0.05 was set for all hypotheses. Given the exploratory nature of this last analysis, corrections for multiple comparisons were not performed.
Results
Association of age, sex, and IQ with RMET item accuracy
Age, female sex, and IQ were all significant predictors of increased probability of obtaining a correct response on RMET in univariable repeated measures logistic regression models [age: F(1,430) = 136.7, p < 0.0001; sex: F(1,430) = 6.5, p = 0.011; IQ: F(1,430) = 35.7, p < 0.0001]. Adding age, sex and IQ into a single model, a significant age by IQ interaction indicated that IQ exerts a higher effect on RMET percent correct in younger participants [Age × IQ: F(1,427) = 7.7, p = 0.006; Sex: F(1,427) = 8.6, p = 0.004] (Table S2, Supplementary Information). Females were significantly more accurate than males (OR(F:M): 1.14, 95%CL: 1.05,1.25, p = 0.004). We therefore controlled for all these covariates in our models examining the effects of ADHD and irritability.
RMET accuracy by group
As illustrated in Fig. 1, there was no difference across the ADHD, Subthreshold ADHD and Control groups in RMET accuracy [F(2,425) = 2.22, p = 0.11; Control vs. Subthreshold ADHD: OR = 1.03, 95%CI: 0.90,1.18, p = 0.6; Control vs. ADHD: OR = 0.96, 95%CI: 0.87,1.07, p = 0.5]. In participants diagnosed with ADHD, High Irritability predicted lower RMET accuracy (ADHD with High Irritability vs, ADHD without High Irritability: OR = 0.85, 95%CI: 0.76, 0.94, p = 0.003).
The probability of obtaining a correct response on the reading the mind in the eyes test in participants with or without high irritability in the ADHD, Subthreshold ADHD and typically developing control diagnostic groups. Note High Irritability was calculated using a cut-off score of ≥ 5 on the CBCL-Irritability scale. RMET percent correct was adjusted for age, sex and IQ as well as age by IQ interaction. Bars represent 95%CI. Significance was calculated using pairwise comparison between groups. RMET Reading the Mind in the Eyes Test. The control group was not divided into High and Low irritability as there were no controls meeting criteria for High Irritability
ADHD and irritability traits, and RMET accuracy
There was a significant interaction between SWAN-ADHD scores and age in predicting RMET accuracy (F(1,425) = 13.91, p = 0.0002). Illustrated in Fig. 2, higher SWAN-ADHD scores predicted a lower RMET accuracy at younger ages but had no significant effect at older ages (Table S3, Supplementary Information). When added to the model, CBCL-Irritability scores significantly predicted lower RMET accuracy (OR = 0.97, 95% CI 0.95; 0.99, p = 0.0063) with no significant interaction with SWAN-ADHD and negligible impact on SWAN-ADHD effects already in the model (Table S4, Supplementary Information).
The probability of obtaining a correct response on the reading the mind in the eyes test by strengths and weaknesses of ADHD symptoms and normal behavior rating scale score as predicted from a repeated measures logistic regression model equation at ages 7, 10, and 13. Note In addition to the SWAN and SWAN × age interaction, the repeated measures logistic regression model controlled for age, sex, and IQ as well as an age × IQ interaction. Predicted values and 95%CI were estimated using the equation were obtained with IQ fixed at 100 and sex set to an equal proportion of males and females. Ages at which predicted values were estimated from the model equation were chosen to illustrate the effect of the SWAN × age interaction across a broad age range. SWAN Strengths and Weaknesses of ADHD Symptoms and Normal Behavior Rating Scale; RMET Reading the Mind in the Eyes Test
ADHD, irritability, and RMET accuracy across neutral, positive and negative emotion valence items
Emotion valence of the images on RMET significantly moderated the effect of CBCL-Irritability on RMET accuracy [F(2,11 653) = 6.1, p = 0.002]. Higher CBCL-Irritability scores predicted significantly lower accuracy on neutral images (OR = 0.94, 95%CI 0.91, 0.97, p < 0.0001), marginally significant lower accuracy on positive images (OR = 0.97, 95%CI 0.93, 0.99, p = 0.046) but no significant effect on negative images (OR = 1.01, 95%CI 0.99, 1.04, p = 0.5. Figure 3).
Relationship of reading the mind in the eyes test accuracy and irritability scores across neutral, positive and negative emotion valence items. Note The repeated measures logistic regression model controlled for age, sex, IQ, age × IQ interaction as well as a SWAN effect. To allow for visual representation of the effects of irritability and valence on RMET item accuracy, accuracy and 95%CI were predicted from the model equation with age fixed to 10 years, IQ at 100, SWAN at 0, for a population with an equal number of males and females. SWAN Strengths and Weaknesses of ADHD Symptoms and Normal Behavior Rating Scale, RMET Reading the Mind in the Eyes Test; CBCL Child Behavior Checklist
RMET accuracy was significantly lower with increased CBCL-Irritability for items with positive or neutral images compared to negative images (neutral vs negative OR p < 0.0001; positive vs negative OR p = 0.02). Although the SWAN-ADHD × valence interaction was also significant [F(2,11 655) = 3.5, p = 0.032], when both SWAN-ADHD × valence and CBCL-Irritability × valence were included together in the model, only the CBCL-Irritability × valence interaction remained significant [F(2, 11 653) = 0.4, p = 0.6; F(2,11 653) = 6.1, p = 0.002, respectively].
Irritability and the probability of erroneously selecting negative emotion valence response on RMET
Given our findings of a significant effect of irritability on RMET accuracy on items with images of neutral valence but not of positive or negative valence, we checked if errors were associated with a preference for choosing a response with negative valence on the neutral valence items while. For this analysis, we only used the 10 items of the neutral emotion valence condition. We then classified RMET responses into three groups: correct responses, negative valence incorrect responses and non-negative (neutral and positive combined) valence incorrect responses. We modeled RMET response type using a repeated measures multinomial nominal logistic regression to determine if irritability was associated with more incorrect responses with negative valence than non-negative valence. Higher CBCL-Irritability scores were associated with poorer accuracy relative to both negative valence and non-negative valence incorrect responses (OR for correct vs negative incorrect responses: 0.88, 95%CI 0.83, 0.94, p = 0.0002; OR for correct vs non-negative incorrect responses: 0.92, 95%CI 0.85, 0.98, p = 0.0097) with no significant difference between the likelihood of selecting negative valence compared to non-negative valence incorrect responses (p = 0.8). That is, higher irritability predicted more negative and non-negative incorrect responses equally.
ADHD, irritability, RMET and ABAS-II Social Skills scores
Linear regression was used to predict scaled scores on the ABAS-Social Skills Area (n = 396) controlling for sex (neither age nor IQ were significant predictors of ABAS-Social Skills Area scores after controlling for SWAN-ADHD or CBCL-Irritability). Higher number of RMET correct responses predicted greater ABAS-Social Skills Area scores (increase in ABAS-Social Skills Area scores for each additional correct RMET response: 1.79, 95%CL: 1.11, 2.46, p < 0.0001). However, the main effect of RMET was no longer significant when both SWAN-ADHD and CBCL-Irritability were included in the model (10-point SWAN-ADHD effect: − 0.48, 95%CL 0.65, − 0.31, p < 0.0001; CBCL-Irritability effect: − 0.51, 95%CL 0.66,-0.37, p < 0.0001; RMET score effect: 0.06, 95%CL: − 0.02, 0.14, p = 0.20. Detailed in Table S5, Supplementary Information). These results indicated that ADHD and irritability traits mediated the association between RMET accuracy and ABAS-Social Skills Area. These results were in the opposite direction of our hypothesis that reduced FER accuracy would mediate the association between ADHD and irritability traits and lower social functioning.
Discussion
Difficulty recognizing facial emotions has been associated with ADHD and with irritability in previous research [4, 15]. Given that these two traits often occur together in the same individual, we examined their relative and unique contribution to the ability to identify emotions portrayed in faces. We hypothesized that ADHD traits would predict poorer accuracy on an FER task irrespective of the emotion valence (positive, negative, or neutral) of the image because of poor attention to detail or impulsive responding [6, 7]. In contrast to ADHD traits, irritability describes a set of traits including proneness to anger and of negative emotional reactivity that might affect the individual’s perception of others’ emotions by various mechanisms [8]. Previous studies showed that highly irritable children make more errors than typically developing children in FER [16] with altered performance across different emotion valences of the images [14, 15, 17, 26, 27]. We hypothesized that irritability traits would predict lower FER accuracy with a bias toward errors characterized by choice of responses portraying negative emotions.
We hypothesized that ADHD traits would predict poorer FER accuracy irrespective of age. Nevertheless, the results indicated that ADHD traits predicted poorer FER in younger children but not in those who have crossed into early adolescence. The improvement in FER accuracy with age is consistent with findings in children diagnosed with other neurodevelopmental disorders [4, 32]. The effect of ADHD traits did not interact with the emotional valence of the facial images, suggestive that difficulty in identifying emotions in the younger children was a function of inattentiveness or impulsiveness rather than a bias toward processing specific emotion.
The current study extends evidence of a deficit in FER to the range of irritability typical of people presenting for assessment of ADHD and typically developing controls, and not just to those with severe and chronic forms of irritability as in previous research [15, 17, 26, 27]. Importantly, the association of irritability and accuracy was independent of the effect of ADHD traits and was significant across ages.
In contrast to ADHD traits, irritability traits interacted with the emotion valence in increasing the probability of not being accurate in FER. Our results suggested that negative face expressions conferred an advantage in FER performance over positive and negative face expressions (negative vs. neutral: p < 0.0001; negative vs. positive: p = 0.02) for those with higher irritability, altering recognition accuracy of others’ expressed emotions when the expressed emotions are neutral and possibly positive but not negative. This result is in line with studies demonstrating that the deficit in FER observed in children and youth with chronic or severe irritability might be affected by the specific emotions being portrayed in the stimulus [14, 17, 27]. Irritable children were shown to have low threshold for identifying ambiguous emotions as reflecting anger rather than happiness in a task employing a gradient of the expressed emotions [15, 26], and to rate neutral faces as fear-inducing [28]. The marginally significant association between irritability and REMT accuracy in the positive emotion valence condition may alternatively suggest that the more salient is the emotional stimulus the lower it the negative effect of irritability on facial emotion recognition accuracy [17].
Using face and auditory emotion recognition tasks, Cadesky et al. (2000), demonstrated emotion recognition tasks that can provide us with data regarding biased interpretations of others’ expressed emotion. Examining the distribution of errors by type of emotion, they showed that in children with ADHD errors were random, whereas children with conduct disorder tended to misrecognize emotions as reflecting anger. In the current study, we examined if irritability would be associated with increased probability of misrecognizing face expressions as reflecting negative emotions. Irritability was significantly associated with lower RMET accuracy only in items of neutral valence. Thus, the examination of our next hypothesis that irritability would be associated with increased likelihood of selecting incorrect negative valence response options was relevant only to the condition in which the exposure was to neural-valence face emotions. Our results did not confirm this hypothesis, and irritability was just as likely to predict negative and non-negative emotional valence incorrect response options. Future studies are needed to confirm the lack of association between irritability and a tendency to erroneously recognize face expressions as negative [15, 26, 28].
ADHD, irritability and RMET scores individually predicted lower scores on a measure of social skills, consistent with previous research [40, 41]. However, the hypothesis that poor FER accuracy would mediate between ADHD, irritability, and social skills was not supported by our results. In fact, the current results suggested that the association between FER accuracy and social skills was fully explained by associated ADHD and irritability traits. Studies are needed to further validate these results in children in with ADHD and to examine whether ADHD and irritability traits are responsible for the association between FER performance and social skills in other populations (e.g., in children diagnosed with autism spectrum disorder) [4].
Results of our primary trait-based analyses were supported by comparison of participants classified as Control, ADHD, Subthreshold ADHD, and as High versus Low Irritability. In these comparisons, we found no difference in FER accuracy among Control, Subthreshold ADHD and ADHD groups, but did find that High Irritability predicted lower FER across the clinical groups. This confirms findings indicating that when both age and IQ are included in the model, there is no difference in FER accuracy between subjects diagnosed with ADHD and controls [4, 14, 42].
Following previous literature emphasizing the possible association between subthreshold ADHD traits and psychiatric disorders frequently related with ADHD, such as substance use disorder and conduct disorder [43], as well as other adverse psychosocial outcomes [44, 45], we found it relevant to examine the study outcomes in this particular subgroup of participants as well.
Our results indicated that ADHD in younger individuals and irritability across ages independently predicted the ability to accurately identify facial emotions. Given the possible importance of FER to social perspective taking and the capacity to accurately ascribe mental states to other people in particular [46], practitioners should assess the impact of these traits on social cognition and skills. Moreover, irritability was found to be associated with spared emotion recognition functioning when the face emotion was negative, implying an emotional valence-related systematic error associated with these traits. Future studies are needed to confirm the lack of association between irritability and a tendency to erroneously recognize face expressions as negative.
Strengths of this study are its large and well-characterized clinic sample of children and consideration of effects on social skills. In addition, this study is the first to conduct an error analysis of performance on the RMET, a widely used measure in the study of social cognition, [39]. Nonetheless, there were several limitations that should be considered when interpreting our findings. We did not consider other dimensions of pathology that could be associated with ADHD or irritability and could affect FER. Oppositional, conduct problems, callous unemotional traits and mood disorders are examples of such traits [3, 24]. Further studies validating the RMET emotion valence categorization reliability and predictive validity are still needed [4]. Levels of irritability in the Control group were low, thus the effect of High Irritability on RMET accuracy in this subgroup of participants could not be estimated. The VCI was used instead of Full-Scale IQ in 28.9% of the total sample (n = 125) when there was a gap of > 15 points between the VCI and the PRI. Studies are needed to confirm the negative interaction between age and Full-Scale IQ in predicting RMET accuracy.
Conclusion
We examined the relative and the unique contribution of ADHD and irritability traits to the ability to identify emotions portrayed in faces of others. Our results indicated that both ADHD and irritability traits independently impact FER accuracy. However, while ADHD traits predicted poor FER accuracy irrespective of the emotion valence, possibly because of poor attention to detail or impulsive responding, irritability was associated with a systematic error in FER, increasing the propensity for misrecognizing neutral and positive but not negative emotions. In addition, the current results raise a question regarding the implied causal linkage between FER and social skills [1], indicating that ADHD and irritability traits fully explain the negative association between FER and social skills.
This study highlights the importance of assessing social cognition in clinical practice in the presence of ADHD or irritability. Future studies examining emotion recognition functioning in ADHD should validate the current results using other measures or tasks and may examine if disruptive behavior and mood symptoms play a role in this association.
References
Baron-Cohen S, Wheelwright S, Spong A et al (2001) Are intuitive physics and intuitive psychology independent? A test with children with Asperger Syndrome. J Dev Learn Disord 5:47–78
Bühler E, Bachmann C, Goyert H et al (2011) Differential diagnosis of autism spectrum disorder and attention deficit hyperactivity disorder by means of inhibitory control and “theory of mind.” J Autism Dev Disord 41:1718–1726. https://doi.org/10.1007/s10803-011-1205-1
Romani M, Vigliante M, Faedda N et al (2018) Face memory and face recognition in children and adolescents with attention deficit hyperactivity disorder: a systematic review. Neurosci Biobehav Rev 89:1–12. https://doi.org/10.1016/j.neubiorev.2018.03.026
Baribeau DA, Doyle-Thomas KAR, Dupuis A et al (2015) Examining and comparing social perception abilities across childhood-onset neurodevelopmental disorders. J Am Acad Child Adolesc Psychiatry 54:479–486. https://doi.org/10.1016/j.jaac.2015.03.016
Quintero J, Ramos-Quiroga JA, Sebastián JS et al (2018) Health care and societal costs of the management of children and adolescents with attention-deficit/hyperactivity disorder in Spain: a descriptive analysis. BMC Psychiatry 18:40. https://doi.org/10.1186/s12888-017-1581-y
Noordermeer SDS, Luman M, Buitelaar JK et al (2020) Neurocognitive deficits in attention-deficit/hyperactivity disorder with and without comorbid oppositional defiant disorder. J Atten Disord 24:1317–1329. https://doi.org/10.1177/1087054715606216
Hobson CW, Scott S, Rubia K (2011) Investigation of cool and hot executive function in ODD/CD independently of ADHD. J Child Psychol Psychiatry Allied Discip 52:1035–1043. https://doi.org/10.1111/j.1469-7610.2011.02454.x
Brotman MA, Kircanski K, Leibenluft E (2017) Irritability in children and adolescents. Annu Rev Clin Psychol 13:317–341. https://doi.org/10.1146/annurev-clinpsy-032816-044941
Stringaris A, Goodman R (2009) Longitudinal outcome of youth oppositionality: Irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry 48:404–412. https://doi.org/10.1097/CHI.0b013e3181984f30
Sobanski E, Banaschewski T, Asherson P et al (2010) Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): Clinical correlates and familial prevalence. J Child Psychol Psychiatry Allied Discip 51:915–923. https://doi.org/10.1111/j.1469-7610.2010.02217.x
Shaw P, Stringaris A, Nigg J, Leibenluft E (2014) Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry 171:276–293. https://doi.org/10.1176/appi.ajp.2013.13070966
Qian Y, Chang WL, He X et al (2016) Emotional dysregulation of ADHD in childhood predicts poor early-adulthood outcomes: a prospective follow up study. Res Dev Disabil 59:428–436. https://doi.org/10.1016/j.ridd.2016.09.022
Wehmeier PM, Schacht A, Barkley RA (2010) Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. J Adolesc Heal 46:209–217. https://doi.org/10.1016/j.jadohealth.2009.09.009
Guyer AE, McClure EB, Adler AD et al (2007) Specificity of facial expression labeling deficits in childhood psychopathology. J Child Psychol Psychiatry Allied Discip 48:863–871. https://doi.org/10.1111/j.1469-7610.2007.01758.x
Stoddard J, Tseng WL, Kim P et al (2017) Association of irritability and anxiety with the neural mechanisms of implicit face emotion processing in youths with psychopathology. JAMA Psychiat 74:95–103. https://doi.org/10.1001/jamapsychiatry.2016.3282
Kim P, Arizpe J, Rosen BH et al (2013) Impaired fixation to eyes during facial emotion labelling in children with bipolar disorder or severe mood dysregulation. J Psychiatry Neurosci 38:407–416. https://doi.org/10.1503/jpn.120232
Rich BA, Grimley ME, Schmajuk M et al (2008) Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Dev Psychopathol 20:529–546. https://doi.org/10.1017/S0954579408000266
Weyandt LL (2007) Book review: Barkley RA (2006). Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment, 3rd edn. Guilford, New York
Demirci E, Erdogan A (2016) Is emotion recognition the only problem in ADHD? Effects of pharmacotherapy on face and emotion recognition in children with ADHD. ADHD Atten Deficit Hyperact Disord 8:197–204. https://doi.org/10.1007/s12402-016-0201-x
Corbett BA, Constantine LJ, Hendren R et al (2009) Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Res 166:210–222. https://doi.org/10.1016/j.psychres.2008.02.005
Da Fonseca D, Seguier V, Santos A et al (2009) Emotion understanding in children with ADHD. Child Psychiatry Hum Dev 40:111–121. https://doi.org/10.1007/s10578-008-0114-9
Pelc K, Kornreich C, Foisy ML, Dan B (2006) Recognition of emotional facial expressions in attention-deficit hyperactivity disorder. Pediatr Neurol 35:93–97. https://doi.org/10.1016/j.pediatrneurol.2006.01.014
Singh SD, Ellis CR, Winton ASW et al (1998) Recognition of facial expressions of emotion by children with attention-deficit hyperactivity disorder. Behav Modif 22:128–142. https://doi.org/10.1177/01454455980222002
Cadesky EB, Mota VL, Schachar RJ (2000) Beyond words: How do children with ADHD and/or conduct problems process nonverbal information about affect? J Am Acad Child Adolesc Psychiatry 39:1160–1167. https://doi.org/10.1097/00004583-200009000-00016
Jusyte A, Gulewitsch MD, Schönenberg M (2017) Recognition of peer emotions in children with ADHD: evidence from an animated facial expressions task. Psychiatry Res 258:351–357. https://doi.org/10.1016/j.psychres.2017.08.066
Hommer RE, Meyer A, Stoddard J et al (2014) Attention bias to threat faces in severe mood dysregulation. Depress Anxiety 31:559–565. https://doi.org/10.1002/da.22145
Thomas LA, Brotman MA, Muhrer EJ et al (2012) Parametric modulation of neural activity by emotion in youth with bipolar disorder, youth with severe mood dysregulation, and healthy volunteers. Arch Gen Psychiatry 69:1257–1266. https://doi.org/10.1001/archgenpsychiatry.2012.913
Brotman MA, Rich BA, Guyer AE et al (2010) Amygdala activation during emotion processing of neutral faces in children with severe mood dysregulation versus ADHD or bipolar disorder. Am J Psychiatry 167:61–69. https://doi.org/10.1176/appi.ajp.2009.09010043
Tottenham N, Phuong J, Flannery J et al (2013) A negativity bias for ambiguous facial-expression valence during childhood: converging evidence from behavior and facial corrugator muscle responses. Emotion 13:92–103. https://doi.org/10.1037/A0029431
Storebø OJ, Andersen ME, Skoog M et al (2019) Social skills training for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008223.PUB3
Tremblay LK, Hammill C, Ameis SH et al (2020) Tracking inhibitory control in youth with ADHD: a multi-modal neuroimaging approach. Front Psychiatry 11:831. https://doi.org/10.3389/FPSYT.2020.00831/BIBTEX
Peñuelas-Calvo I, Sareen A, Sevilla-Llewellyn-Jones J, Fernández-Berrocal P (2019) The “reading the mind in the eyes” test in autism-spectrum disorders comparison with healthy controls: a systematic review and meta-analysis. J Autism Dev Disord 49:1048–1061. https://doi.org/10.1007/s10803-018-3814-4
Peterson E, Miller SF (2012) The eyes test as a measure of individual differences: how much of the variance reflects verbal IQ? Front Psychol 3:220. https://doi.org/10.3389/FPSYG.2012.00220/BIBTEX
Burton CL, Wright L, Shan J et al (2019) SWAN scale for ADHD trait-based genetic research: a validity and polygenic risk study. J Child Psychol Psychiatry Allied Discip 60:988–997. https://doi.org/10.1111/jcpp.13032
Renaud B, Buda M, Lewis BD, Pujol JF (1975) Effects of 5,6-dihydroxytryptamine on tyrosine-hydroxylase activity in central catecholaminergic neurons of the rat. Biochem Pharmacol 24:1739–1742. https://doi.org/10.1016/0006-2952(75)90018-0
Evans SC, Bonadio FT, Bearman SK et al (2020) Assessing the irritable and defiant dimensions of youth oppositional behavior using CBCL and YSR items. J Clin Child Adolesc Psychol 49:804–819. https://doi.org/10.1080/15374416.2019.1622119
Harrison PL, Oakland T (2018) Adaptive behavior assessment system: third edition. Encycl Clin Neuropsychol 57–60. https://doi.org/10.1007/978-3-319-57111-9_1506
Girli A (2014) Psychometric properties of the Turkish child and adult form of “Reading the Mind in the Eyes Test.” Psychology 05:1321–1337. https://doi.org/10.4236/psych.2014.511143
Vellante M, Baron-Cohen S, Melis M et al (2013) The “reading the Mind in the Eyes” test: systematic review of psychometric properties and a validation study in Italy. Cogn Neuropsychiatry 18:326–354. https://doi.org/10.1080/13546805.2012.721728
Ros R, Graziano PA (2018) Social functioning in children with or at risk for attention deficit/hyperactivity disorder: a meta-analytic review. J Clin Child Adolesc Psychol 47:213–235. https://doi.org/10.1080/15374416.2016.1266644
Murray-Close D, Hoza B, Hinshaw SP et al (2010) Developmental processes in peer problems of children with attention-deficit/hyperactivity disorder in the multimodal treatment study of children with ADHD: developmental cascades and vicious cycles. Dev Psychopathol 22:785–802. https://doi.org/10.1017/S0954579410000465
Rinke L, Candrian G, Loher S et al (2017) Facial emotion recognition deficits in children with and without attention deficit hyperactivity disorder: a behavioral and neurophysiological approach. NeuroReport 28:917–921. https://doi.org/10.1097/WNR.0000000000000858
Shankman SA, Lewinsohn PM, Klein DN et al (2009) Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child Psychol Psychiatry 50:1485–1494. https://doi.org/10.1111/J.1469-7610.2009.02117.X
Norén Selinus E, Molero Y, Lichtenstein P et al (2016) Subthreshold and threshold attention deficit hyperactivity disorder symptoms in childhood: psychosocial outcomes in adolescence in boys and girls. Acta Psychiatr Scand 134:533–545. https://doi.org/10.1111/ACPS.12655
Schiavone N, Virta M, Leppämäki S et al (2019) ADHD and subthreshold symptoms in childhood and life outcomes at 40 years in a prospective birth-risk cohort. Psychiatry Res 281:112574. https://doi.org/10.1016/J.PSYCHRES.2019.112574
Cassels TG, Birch SAJ (2014) Comparisons of an open-ended vs. forced-choice “mind reading” task: implications for measuring perspective-taking and emotion recognition. PLoS ONE 9(12):e93653. https://doi.org/10.1371/JOURNAL.PONE.0093653
Acknowledgements
This research was conducted with the support of the Ontario Brain Institute (POND, PIs: Anagnostou/Lerch), an independent non-profit corporation, funded partially by the Ontario government. The opinions, results and conclusions are those of the authors and no endorsement by the Ontario Brain Institute is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This study has been approved by the Internal Review Board of our institution and was performed in accordance with the ethical standards of the Declaration of Helsinki.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Levy, T., Dupuis, A., Andrade, B.F. et al. Facial emotion recognition in children and youth with attention-deficit/hyperactivity disorder and irritability. Eur Child Adolesc Psychiatry 32, 2271–2280 (2023). https://doi.org/10.1007/s00787-022-02033-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-022-02033-3