Abstract
Autism spectrum disorders (ASD) and attention deficit hyperactivity disorders (ADHD) are both associated with deficits in executive control and with problems in social contexts. This study analyses the variables inhibitory control and theory of mind (ToM), including a developmental aspect in the case of the latter, to differentiate between the disorders. Participants with an ASD (N = 86), an ADHD (N = 84) and with both disorders (N = 52) in the age range of 5–22 years were compared. Results were differences in inhibitory control (ADHD < ASD) and in the ToM performance among younger (ASD < ADHD) but not among older children. We discuss whether common deficits in ToM differ in the developmental course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorders (ASD) and attention deficit hyperactivity disorders (ADHD) share a critical amount of symptoms. While the diagnostic guidelines highlight social deficits as especially evident in ASDs, the cardinal symptom of an ADHD is a deficit in the area of attention functioning (Adrien et al. 1993; APA 2005). However, childrenFootnote 1 with ADHD are frequently found to exhibit social difficulties in a degree comparable to disorders of the autistic spectrum (Clark et al. 1999; Greene et al. 1996; Luteijn et al. 2000; Mulligan et al. 2009; Santosh and Mijovic 2004). Greene and colleagues thus describe 22% of a sample of children with an ADHD as ‘socially disabled’ (Greene et al. 1996) and Santosh and Mijovic use the term ‘autistic-like’ to describe the social deficits of a group of children with ADHD (Santosh and Mijovic 2004). When Clark and his team analysed the presence of autistic symptoms in an ADHD-sample via the parent-rated Autism Criteria Checklist, a ‘lack of awareness of the feelings of others’ was the most common autistic symptom (65–80%) reported (Clark et al., 1999).
Children diagnosed with a high-functioning ASD on the other hand are found to manifest deficits in their executive control functions (Frazier et al. 2001; Goldstein and Schwebach, 2004; Leyfer et al. 2006; Sinzig et al. 2008). Jensen and colleagues report of 74% from a sample of autistic children who had initially been falsely diagnosed with an ADHD (Jensen et al. 1997). In a study from Goldstein and Schwebach about a quarter (26%) of the children met the criteria for an additional ADHD (Goldstein and Schwebach 2004).
An overlap in symptom hinders the diagnostic process and as shown above, increases the risk of false diagnoses. In the classification systems ICD-10 and DSM-IV an exclusionary criterion is held for the two disorders (APA 2005; WHO 1993). What is more, in the DSM-IV source book it is stated that the questions of hierarchical diagnoses relate primarily to philosophical or pragmatic considerations and that the empirical literature provides little direction for deciding these issues (McBurnett 2005). Given the high amount of shared symptoms more and more researchers question the approach held in the ICD-10 and DSM-IV (Frazier et al. 2001; Gadow et al. 2004; Goldstein and Schwebach 2004; Holtmann et al. 2005, 2007; Leyfer et al. 2006; Sinzig et al. 2009) and clinicians call for specifying research to facilitate the diagnostic process (First et al. 2004; Frazier et al. 2001; Jensen et al. 1997). The adoption of a co-morbid approach would imply the possibility of a differentiation of the symptom overlap.
In the light of the high clinical relevance of this problem, this work seeks to contribute to the research process of differentiating between high-functioning ASDs and ADHD by a detailed analysis of selected neuropsychological parameters.
Previous attempts to differentiate between the two disorders have been focussing on several neuropsychological aspects and the resulting evidence indicates a possible differentiation within the areas of executive control functions and Theory of Mind (ToM). While there is ample evidence for children with an ADHD to show a marked deficit in their inhibitory control (Aman et al. 1998; Iaboni et al. 1995; Nigg 1999; Schachar et al. 1995; Shue and Douglas 1992), the picture in the case of ASD is less clear and implicates a broader impairment across a range of executive functions occasionally including deficits in the inhibitory control (Corbett et al. 2009; Courchesne et al. 1994; Geurts et al. 2004; Ozonoff and Jensen 1999; Nyden et al. 1999; Happe et al. 2006; Noterdaeme et al. 2001).
ASDs on the other hand are strongly associated with deficits within the area of ToM (Bolte and Poustka 2003; Bruning et al. 2005; Davies et al. 1994; Downs and Smith 2004; Kuusikko et al. 2009; Ozonoff et al. 1991). Morphological research could show that individuals with high-functioning autism (HFA) and Asperger’s syndrome (AS) show activation in different brain areas than healthy controls when solving tasks of ToM (Brieber et al. 2007; Monk 2008; Monk et al. 2010; Schultz 2005; Schultz et al. 2000). It appears however that a higher level of cognitive functioning in subjects with HFA and AS allows them to learn how to solve simple ToM tasks e.g. emotion recognition tasks and thereby compensate for their deficits (Baron-Cohen 1989; Brook and Bowler 1992; Klin 2000; Dyck et al. 2001; Sinzig et al. 2008) whereas deficits in the spontaneous social attribution are found to remain relatively stable (Abell et al. 2000; Klin 2000). In the case of children with ADHD deficits in certain ToM tasks, including the recognition of facial emotions, have been reported, though less profound than in the case of ASD (Corbett and Glidden 2000; Singh et al. 1998; Norvilitis et al. 2000; Da Fonseca et al. 2009; Pelc et al. 2006). A direct comparison of children with ADHD and ASD on a range of first- and second-order ToM tasks as well as an emotion recognition task revealed an impaired performance in both groups, which did not allow for a differentiation between the disorders (Buitelaar et al. 1999).
A theoretical approach furthered by Sodian and Hülsken outlines the possibility of a difference in the development of ToM-deficits. While children with an ASD show deficits from an early age (DiCicco-Bloom et al. 2006; Jones and Klin 2009), children with an ADHD are assumed to develop ToM-deficits in relation to their difficulties in inhibitory control. Sodian and Hülsken found that in children with an ADHD, ToM impairments come to light in tasks with high inhibitory demands. A point in case being false belief tasks, where the child has to withhold or inhibit its knowledge of the situation and answer from the perspective of one of the actors in the task (Sodian and Hülsken 2005). Correspondingly the children were unimpaired on tasks of ToM not requiring inhibitory control. Based on this observation the authors suggest that the ability of ToM itself is intact but that there is a failure to express this ability in situations that require inhibitory control. According to this rationale, a primary deficit in inhibitory control leads to a mal-adaptation during development, manifest in a failure to develop particular ToM skills in comparison to normally developing peers. Contrary to children with ASD then, there is no primary deficit in ToM-skills but the deficits develop in the course of the inhibitory deficit.
Only few studies considered a developmental aspect in the analysis of the disorders and might serve as empirical reference. When Sinzig and colleagues compared the performance of children with ASD and ADHD on an emotion recognition task across three age-groups (6–10, 11–14, 15–18 years) they found no significant difference between the diagnostic groups in any of the age-groups (Sinzig et al. 2007). In a later study however, the authors report a highly significant, positive correlation between inhibitory control and the performance on a task of facial emotion recognition in children with ADHD (Sinzig et al. 2008).
Based on the reviewed literature we decided to conduct a confirmatory analysis focussing on the two neuropsychological parameters inhibitory control and Theory of Mind (emotion recognition and social attribution). To investigate the developmental hypothesis we are the first to specifically analyze developmental differences in ToM-deficits. We expected the ADHD and a co-morbid group (ADHD + ASD) to show a more profound impairment in a task of inhibitory control than children with an ASD. Children with ASD on the other hand would be more impaired within the area of ToM—these are the recognition of facial emotion expressions and the attribution of social intention to abstract stimulus material. Also, they would show a longer reaction time in this task due to the adoption of compensatory strategies. On a more exploratory ground, we expected to observe a difference in the developmental course of impaired emotion recognition. We thus anticipated a significant difference between the two diagnostic groups in early childhood, which would no longer be observable among the older children.
Methods
Participants
Participants came from the special consultation program for ASDs of the University hospital of Giessen and Marburg (Germany) where they had received a diagnosis within the autistic spectrum. The group of children with an ADHD were patients from the clinic who had been diagnosed with a Hyperkinetic disorder (F90.0) or a Conduct disorder (F90.1). This was necessary since not enough children with the diagnosis F90.0 could be identified who did not suffer from a co-morbid emotional disorder. Another group consisted of children who fulfilled the diagnostic criteria for both disorders in the clinic in Marburg.
All participants had given their written consent for participation in the study. The period of data collection was from 2004–2009. Testing took place during morning hours and was occasionally scheduled over 2 days. The german adaptation of the Wechsler scales for children were administered to all children to estimate the level of cognitive functioning (Petermann and Petermann 2007; Tewes 1993; Tewes et al. 1999). Presence or absence of an ASD was tested by administering the ADOS-G (Rühl et al. 2004) and the ADI-R (Bölte et al. 2006), currently referred to as the ‘gold-standard’ for diagnosing ASDs. If available, home-videos were included in the diagnostic process. Co-morbid disorders, including learning disabilities, were captured via the semi-structured interview “Diagnostisches Interview für Psychiatrische Störungen” (DIPS) which was administered to the parent or legal guardian of the child (Unnewehr et al. 1998). Children with co-morbid disorders were excluded from the study. The diagnoses were made by versed psychiatrists and psychologists strictly according to the established criteria in the ICD-10. The administration of the procedures ADOS-G and ADI-R was undertaken by experienced psychologists who were working in the special consultation program for ASDs and had undergone training in the administration of the paradigms. Table 1 summarizes the characteristics of the subjects, including the distribution of diagnoses, intelligence quotient (IQ) as well as means, SD and range of age within each group. See Table 1 for further sample characteristics.
Measures
ADOS-G and ADI-R: The Autism Diagnostic Observation schedule (ADOS-G) and the Autism Diagnostic Interview-Revised (ADI-R) are diagnostic instruments that strictly operationalize the guidelines for ASDs in the ICD-10 (Bolte and Poustka 2003). While the ADOS-G addresses the current psychopathology by the elicitation of a number of social stimuli, the ADI-R is an interview with the parents or principal caregivers and covers the life time perspective and includes questions on language development (Le Couteur et al. 1989). The items in both instruments are divided into a) qualitative impairment in social interactions b) qualitative impairment in communication c) restricted, repetitive and stereotypic patterns of behaviours, interests and activities (Le Couteur et al. 1989).
Test battery for attention performance (TAP): The TAP is a computer-based neuropsychological procedure developed by Zimmermann and Fimm (1993) which is of frequent use within the clinical diagnosis of neurological or psychiatric disorders (Földenyi et al. 2000; Grodzinsky and Barkley 1999). Age-norms exist for the age-range of 6–19 years (N = 184) (Zimmermann and Fimm 1993). The reliability is reported as good to superior and a high degree of objectivity is assured since the demands to perceptive, mnestic, verbal and motor capabilities are minimal and both the procedure and the interpretation are computerised (Zimmermann and Fimm 1993).
The subtest Go/Nogo is a task of selective attention that exists in two versions with either one or two target stimuli. We administered the simpler version to children < 10 years and the more difficult version to children ≥10 years. The test comprises 40 stimuli presentations made up of 20 non-target stimuli and 20 target stimuli, each trial lasting 2 ss with 0 ss in between. The child is instructed to press a button when the target stimulus appears on the screen, which allows for commission mistakes (the child responds to a non-target stimulus) and omission mistakes (the child fails to respond to the target stimulus) (Zimmermann and Fimm 1993).
Facial Emotion Matching (FEM): The FEM is a computer-based task of facial emotion recognition developed by the neuropsychological testing system candit (http://www.candit.com). The paradigm was initially used in adult neurological contexts. Today, emotion recognition tasks are frequently used to asses ToM-skills in both children and adults. The pictures in the FEM stem from a well known battery of emotion pictures from Ekman et al. (1972) based on a concept of seven cross-cultural, basic emotional states that have been used extensively in studies of facial expressions (Bolte and Poustka 2003; Buitelaar et al. 1999; Singh et al. 1998).
In all, 24 adult faces are presented one after the other and the participant is asked to compare each face to six other faces presenting six different emotions (joy, sadness, fear, anger, amazement and disgust), only one of them showing the same as the stimulus face. Since the comparison emotions are occasionally presented in a different version than the stimulus face, there is a risk for detailed mistakes, where the subject falsely compares the faces according to the position of the mouth or eyes only. Age-norms exist for the range of pre-school-age up to adulthood and stem from a constantly updated database open for access on candit.com. No other studies could be retrieved that used this version of facial emotion recognition task; however, the pictures from Ekman are used in other tasks and are well validated.
Social Attribution Task (SAT): The Social Attribution Task (SAT) (Klin 2000) measures the ability to spontaneously attribute social meaning to ambiguous visual stimuli. It consists of an animated sequence developed from Heider and Simmel (1944) in which three geometrical shapes enact a social plot by moving around each other either synchronously or against one another.
The instrument was administered in an unpublished and un-standardised version in German language. The sequence (duration 50 s) is presented twice in its full length and the third presentation is divided into 6 sequences with 19 multiple choice questions posed directly after each sequence. Findings have consistently been showing an impaired performance in children with an ASD (Abell et al. 2000; Klin 2000). To the knowledge of the authors, no studies have been conducted that included children with ADHD.
Statistical Analysis
The statistical analysis was made by help of the Statistical Package for Social Science (SPSS) version 17.0. Mean differences between the ADHD and the ASD group concerning the metric test scores were tested by means of the Mann–Whitney U test or the t test was used to test for significant group-differences depending on whether the scores were normally distributed or not. Mean differences for the 3 diagnostic groups concerning testscores, which were not normally distributed, were tested with the Kruskall–Wallis test for comparison of several independent groups and followed up by post hoc tests if the result was significant. Effect sizes concerning the mean differences of non normally distributed testscores were calculated as Z/√N (Field 2009). A discriminant function analysis was undertaken to define a linear combination of characteristics that best separated the diagnostic groups from each other.
There was a significant difference between the groups in the level of cognitive functioning (F(2,161) = 3,29, p = 0.04), which is why the analysis was controlled for this potentially confounding factor. In order to control for multiple testing, the level of significance was restricted to p < 0.0125 regarding the main analysis of the parameters before the division into age-groups. Other exploratory calculations, as well as calculations after division into age-groups, were based on the conventional level of p < 0.05 and the obtained results need to be regarded as preliminary.
Results
Inhibitory control (TAP): The analysis within inhibitory control revealed a highly significant difference between the groups ASD and ADHD with a medium effect size (z = −4.302 p = .000, r = 0.35). A significant Kruskall–Wallis test regarding the data of the TAP (H(2) = 6.901, p = 0.00) was followed up by post hoc tests between the groups. According to the restricted level of significance, a trend was found between the ASD + ADHD-group (Mdn. 35.79) and the ASD-group (Mdn. 48.41) with a small to medium effect size (z = −2.429, p = 0.015, r = −0.22). For an illustration of the result see Fig. 1.
ToM (FEM and SAT)
The between-group comparisons regarding the groups ASD and ADHD showed no significant differences on the amount of correct answers (t(157) = −2.411, p = 0.017) according to the restricted alpha-level. Nor did the reaction time (t(1,157) = −1.231, p = 0.22) on the FEM and the amount of correct answers on the SAT (z = −1.712, p = 0.044). With regard to detailed mistakes (mistakes due to comparison of faces based solidly on the position of the eyes or the mouth) the comparison revealed that the ASD-group committed significantly more mouth-mistakes (t(157) = −2.609, p = 0.01) but not more eye-mistakes (t(157) = −1.627, p = 0.106). A comparison including all three groups revealed no significant difference on the FEM (p = 0.059) and the SAT (p = 0.032) (see Fig. 2).
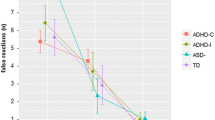
FEM within age-groups: The children < 10 years with ASD (M = 50.1, SD 14.78) made significantly more mistakes than the same-aged children with ADHD (M = 55.16, SD 15.3) (t(71) = −2.125, p = 0.037). Meanwhile, in the group of older children (≥10) the difference between the two groups (ASD: M 68.11, SD 13.07; ADHD: M 67.82, SD 10.2) was no longer significant (t(88) = −0.289, p = 0.774). The performance is illustrated in Fig. 3.
Discriminant function analysis: To examine how well the diagnostic groups could be distinguished based on their test performance in the younger and in the older groups respectively, we ran a stepwise discriminant function analysis within age-groups. It was found that the scores of the commission mistakes in the Go/Nogo and eye-mistakes in the FEM made out a highly significant discriminant function to group membership among younger children (<10 years) (Wilk’s λ = 0.669, p = 0.00) and could classify 71% of children with an ASD and 73% of children with ADHD correctly. In this age group the positive predictive value for ASD was 0.65, meaning that 65% of the children above the cutoff of the discriminant function actually had received a diagnosis within the autistic spectrum. The positive predictive value for ADHD is 0.79. In the older group of children (≥10 years) the variables of commission mistakes in the Go/Nogo and the reaction time (T values) in the FEM could discriminate significantly between the groups (λ = 0.837, p = 0.005). Here, 63% of subjects with ASD and 54% of subjects with an ADHD were correctly classified according to group membership. In this age group the positive predictive value for ASD was 0.66 and the positive predictive value for ADHD was 0.51. Controlling for differences in the level of IQ caused only marginal changes in the results.
Discussion
The main findings of our study are (a) the presence of a significant difference in inhibitory control function between the ASD-group and the co-morbid group, the latter showing a more impaired inhibitory control; (b) the absence of a significant difference between the ASD-group and the ADHD-group on two tasks of ToM; (c) a moderate predictive value of the discriminatory function analysis in terms of differentiation between ASD and ADHD; (d) a significant difference on the FEM task within the younger-age group of ASD and ADHD respectively, which was not observable between the older-age groups, where a more impaired performance (T values) of the ADHD-group was observed.
In support of the previously mentioned co-morbid approach, favoured by many researchers (McBurnett 2005), our results allow for the separate detection of the presence of an ADHD in children with a known ASD by considering their inhibitory control functioning. This is important since inhibitory deficits need a special treatment which might differ from interventions regarding the autistic symptomatology (Yoshida and Uchiyama 2004).
We found no significant difference between the two groups performances on the FEM, when the adjusted alpha-level was applied. This is consistent with the study from Buitelaar and colleagues who equally found both disorders to be associated with impairments on similar tasks (Buitelaar et al. 1999). Together these findings suggest that children with ADHD suffer from deficits in facial emotion recognition comparable to their peers with an ASD and highlight the potential symptom overlap between the two disorders. According to the results, the FEM seems not suited to differentiate clearly between the two disorders. The discriminatory function analysis also indicates that an exact discrimination between the disorders is difficult.
However, the subsequent analysis within age-groups sheds another light on the missing group difference that was found initially. A significant difference between the younger children but not among the older children regarding the amount of mistakes in the FEM indicates that children with ADHD develop deficits in ToM as they become older. This is in agreement with the theoretical model and preliminary findings on the relation between a deficient inhibitory control and deficits in ToM, outlined earlier (Moses et al. 2005; Sodian and Hülsken 2005).
Moreover, the present task of facial emotion recognition can be rated as rather low in its inhibitory demands. It consists of a well-structured task with explicit instructions and without potentially distracting context information. In contrast to false-belief-tasks, in the FEM the child does not have to hold knowledge in its mind. Consequently, while Sodian and Hülsken speak of a deficit in the expression of intact ToM-skills in children with ADHD (Sodian and Hülsken 2005), we might interpret the present finding as indicating the development of deficits that persist independently of the initially causative inhibitory deficit. Accordingly, the difference between ASD and ADHD lies in the development of the deficits. While children with an ASD lack a prerequisite for the development of a ToM and show early deficits (Webb et al. 2006), children with ADHD develop deficits across development. In typically developing children, the development of a ToM is seen as strongly dependent on stimulation from the parents and later in development especially on the peer group. Carpenter Rich et al. (2009) note in this regard that children with ADHD are often found to be disliked and rejected within minutes in social contexts. Being excluded from the social interaction with peers they are at the same time denied further opportunities to practice adequate social skills and to develop competences in ToM. The nature of deficits in ToM in children with ADHD needs to be investigated more thoroughly elsewhere—nevertheless, in comparison to children with ASD a difference in the developmental course of the deficits is crucial information for the diagnostic process. Due to the absence of reference data in the case of developmental differences, the outlined conclusions can only be seen as preliminary and further studies should address the issue. In the sole earlier study that compared children with ADHD and ASD and included a division into age-groups, no comparable results were found (Sinzig et al. 2007). However, a small sample size (8–15 children in each age group) might be a limiting factor for the interpretation of the data.
The discriminatory function of the reaction time in the FEM in the age-group equal or above 10 reveals another important developmental aspect that might help to improve a differentiation between the disorders. It indicates that the children with an ASD adapt cognitive strategies to compensate for their deficits. This is consistent with a study from Dyck and colleagues who highlight the influence of cognitive abilities on performance at emotion recognition tasks (Dyck et al. 2001). There is thus a subsequent developmental deficit in that children with ASD potentially get better throughout development while children with ADHD risk the development of deficits, as argued above. We have to mention in this regard that the results in our study are restricted to the high-functioning end of the autistic spectrum and therefore no conclusions on less cognitively capable children can be drawn.
Several aspects potentially limit the interpretation of the obtained results. The main caveat is a performance of both the ASD—and the ADHD-groups within the range of normal on the FEM. This contradicts a large amount of previous studies that consistently found children with ASD to be impaired in their facial emotion recognition when compared to normal controls (Davies et al. 1994; Downs and Smith 2004; Ozonoff et al. 1991; Rump et al. 2009). The high intellectual functioning within the group or an artefact produced by the standardization of the instrument might have played a role in this regard. Future studies should include a matched control group in order to be able to directly compare the performances. The pictures in the FEM were taken from adults and performance might have been different if the stimulus material had consisted of child faces. The undifferentiated inclusion of children in the ADHD group ignoring the presence or absence of hyperactivity is a further possible confound. While some findings indicate a difference in the inhibitory control functioning others do not find them to perform differently (Barkley et al. 1991; Diamond 2005). Finally, no socioeconomic data were collected on the participating children, which leaves open whether differences in socioeconomic variables (e.g. number of siblings, socioeconomic status) have had an influence on the results.
In conclusion, a specification of the existing categories ASD and ADHD in terms of the parameter inhibitory control and by adopting a developmental perspective on deficits within ToM, allows to differentiate between the disorders. For clinical contexts, our results suggest that a co-morbid approach would be of help in order to capture the complexity of the symptomatology. Our study also showed that the inclusion of a developmental perspective seems to be promising in the quest of learning more about the disorders in question.
Notes
For the sake of simplicity, in what follows the term ‘children’ will be used even if the age-range in the sample of the study was 4–22 years.
References
Abell, F., Happe, F., & Frith, U. (2000). Do triangles play tricks? Attribution of mental states to animated shapes in normal and abnormal development. Cognitive Development, 15, 1–16.
Adrien, J. L., Lenoir, P., Martineau, J., Perrot, A., Hameury, L., Larmande, C., et al. (1993). Blind ratings of early symptoms of autism based upon family home movies. Journal of the American Academy of Child & Adolescent Psychiatry, 32(3), 617–626.
Aman, C. J., Roberts, R. J., Jr., & Pennington, B. F. (1998). A neuropsychological examination of the underlying deficit in attention deficit hyperactivity disorder: Frontal lobe versus right parietal lobe theories. Developmental Psychology, 34(5), 956–969.
APA. (2005). Diagnostic and statistical manual of mental disorders (4th ed.). Wahington: American Psychologic Association.
Barkley, R. A., DuPaul, G. J., & McMurray, M. D. (1991). Attention deficit disorder with and without hyperactivity: Clinical response to three dose levels of methylphenidate. Pediatrics, 87(4), 519–531.
Baron-Cohen, S. (1989). The autistic child’s theory of mind: A case of specific developmental delay. Journal of Child Psychology and Psychiatry and Allied Disciplines, 30(2), 285–297.
Bolte, S., & Poustka, F. (2003). The recognition of facial affect in autistic and schizophrenic subjects and their first-degree relatives. Psychological Medicine, 33(5), 907–915.
Bölte, S., Rühl, D., Schmötzer, G., & Poustka, F. (2006). ADI-R - Diagnostisches Interview für Autismus - Revidiert. Bern: Huber.
Brieber, S., Neufang, S., Bruning, N., Kamp-Becker, I., Remschmidt, H., Herpertz-Dahlmann, B., et al. (2007). Structural brain abnormalities in adolescents with autism spectrum disorder and patients with attention deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48(12), 1251–1258.
Brook, S. L., & Bowler, D. M. (1992). Autism by another name? Semantic and pragmatic impairments in children. Journal of Autism and Developmental Disorders, 22(1), 61–81.
Bruning, N., Konrad, K., & Herpertz-Dahlmann, B. (2005). Relevance and results of Theory of Mind research for autism and other psychiatric disorders. Zeitschrift für Kinder Jugendpsychiatrie und Psychotherapie, 33(2), 77–88.
Buitelaar, J. K., van der Wees, M., Swaab-Barneveld, H., & van der Gaag, R. J. (1999). Theory of mind and emotion-recognition functioning in autistic spectrum disorders and in psychiatric control and normal children. Development & Psychopathology, 11(1), 39–58.
Carpenter Rich, E., Loo, S. K., Yang, M., Dang, J., & Smalley, S. L. (2009). Social functioning difficulties in ADHD: Association with PDD risk. Clinical Child Psychology and Psychiatry, 14(3), 329–344.
Clark, T., Feehan, C., Tinline, C., & Vostanis, P. (1999). Autistic symptoms in children with attention deficit-hyperactivity disorder. European Child and Adolescent Psychiatry, 8(1), 50–55.
Corbett, B. A., Constantine, L. J., Hendren, R., Rocke, D., & Ozonoff, S. (2009). Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Research, 166(2–3), 210–222.
Corbett, B., & Glidden, H. (2000). Processing affective stimuli in children with attention-deficit hyperactivity disorder. Child Neuropsychology, 6(2), 144–155.
Courchesne, E., Townsend, J., Akshoomoff, N. A., Saitoh, O., Yeung-Courchesne, R., Lincoln, A. J., et al. (1994). Impairment in shifting attention in autistic and cerebellar patients. Behavioral Neuroscience, 108(5), 848–865.
Da Fonseca, D., Seguier, V., Santos, A., Poinso, F., & Deruelle, C. (2009). Emotion understanding in children with ADHD. Child Psychiatry and Human Development, 40(1), 111–121.
Davies, S., Bishop, D., Manstead, A. S., & Tantam, D. (1994). Face perception in children with autism and Asperger’s syndrome. The Journal of Child Psychology and Psychiatry, 35(6), 1033–1057.
Diamond, A. (2005). Attention-deficit disorder (attention-deficit/ hyperactivity disorder without hyperactivity): A neurobiologically and behaviorally distinct disorder from attention-deficit/hyperactivity disorder (with hyperactivity). Development and Psychopathology, 17(3), 807–825.
DiCicco-Bloom, E., Lord, C., Zwaigenbaum, L., Courchesne, E., Dager, S. R., Schmitz, C., et al. (2006). The developmental neurobiology of autism spectrum disorder. Journal of Neuroscience, 26(26), 6897–6906.
Downs, A., & Smith, T. (2004). Emotional understanding, cooperation, and social behavior in high-functioning children with autism. Journal of Autism and Developmental Disorders, 34(6), 625–635.
Dyck, M. J., Ferguson, K., & Shochet, I. M. (2001). Do autism spectrum disorders differ from each other and from non-spectrum disorders on emotion recognition tests? European Child and Adolescent Psychiatry, 10(2), 105–116.
Ekman, P., Friesen, W. V., & Ellsworth, P. (1972). Emotion in the human face. New York: Pergamon.
Field, A. (2009). Discovering statistics using SPSS (3rd ed.). London: Sage Publications.
First, M. B., Pincus, H. A., Levine, J. B., Williams, J. B., Ustun, B., & Peele, R. (2004). Clinical utility as a criterion for revising psychiatric diagnoses. The American Journal of Psychiatry, 161(6), 946–954.
Földenyi, M., Imhof, K., & Steinhausen, H. C. (2000). Klinische Validität der computergestützten TAP bei Kindern mit Aufmerksamkeits-/ Hyperaktivitätsstörungen. Zeitschrift für Neuropsychologie, 3, 154–167.
Frazier, J. A., Biederman, J., Bellordre, C. A., Garfield, S. B., Geller, D. A., Coffey, B. J., et al. (2001). Should the diagnosis of attention-deficit/hyperactivity disorder be considered in children with pervasive developmental disorder? Journal of Attention Disorders, 4, 203–211.
Gadow, K. D., DeVincent, C. J., Pomeroy, J., & Azizian, A. (2004). Psychiatric symptoms in preschool children with PDD and clinic and comparison samples. Journal of Autism and Developmental Disorders, 34(4), 379–393.
Geurts, H. M., Verte, S., Oosterlaan, J., Roeyers, H., & Sergeant, J. A. (2004). How specific are executive functioning deficits in attention deficit hyperactivity disorder and autism? The Journal of Child Psychology and Psychiatry, 45(4), 836–854.
Goldstein, S., & Schwebach, A. J. (2004). The comorbidity of pervasive developmental disorder and attention deficit hyperactivity disorder: Results of a retrospective chart review. Journal of Autism and Developmental Disorders, 34(3), 329–339.
Greene, R. W., Biederman, J., Faraone, S. V., Ouellette, C. A., Penn, C., & Griffin, S. M. (1996). Toward a new psychometric definition of social disability in children with attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 35(5), 571–578.
Grodzinsky, G. M., & Barkley, R. A. (1999). Predictive power of frontal lobe tests in the diagnosis of attention deficit hyperactivity disorder. Clinical Neuropsychology, 13(1), 12–21.
Happe, F., Booth, R., Charlton, R., & Hughes, C. (2006). Executive function deficits in autism spectrum disorders and attention-deficit/hyperactivity disorder: Examining profiles across domains and ages. Brain and Cognition, 61(1), 25–39.
Heider, F., & Simmel, M. (1944). An experimental study of apparent behavior. American Journal of Psychology, 57, 243–259.
Holtmann, M., Bolte, S., & Poustka, F. (2005). ADHD, Asperger syndrome, and high-functioning autism. Journal of the American Academy of Child and Adolescent Psychiatry, 44(11), 1101.
Holtmann, M., Bolte, S., & Poustka, F. (2007). Attention deficit hyperactivity disorder symptoms in pervasive developmental disorders: Association with autistic behavior domains and coexisting psychopathology. Psychopathology, 40(3), 172–177.
Iaboni, F., Douglas, V. I., & Baker, A. G. (1995). Effects of reward and response costs on inhibition in ADHD children. Journal of Abnormal Psychology, 104(1), 232–240.
Jensen, V. K., Larrieu, J. A., & Mack, K. K. (1997). Differential diagnosis between attention-deficit/hyperactivity disorder and pervasive developmental disorder—not otherwise specified. Clinical Pediatrics (Phila), 36(10), 555–561.
Jones, W., & Klin, A. (2009). Heterogeneity and homogeneity across the autism spectrum: The role of development. Journal of the American Academy of Child & Adolescent Psychiatry, 48(5), 471–473.
Klin, A. (2000). Attributing social meaning to ambiguous visual stimuli in higher-functioning autism and Asperger syndrome: The Social Attribution Task. Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(7), 831–846.
Kuusikko, S., Haapsamo, H., Jansson-Verkasalo, E., Hurtig, T., Mattila, M. L., Ebeling, H., et al. (2009). Emotion recognition in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(6), 938–945.
Le Couteur, A., Rutter, M., Lord, C., Rios, P., Robertson, S., Holdgrafer, M., et al. (1989). Autism diagnostic interview: A standardized investigator-based instrument. Journal of Autism and Developmental Disorders, 19(3), 363–387.
Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36(7), 849–861.
Luteijn, E. F., Serra, M., Jackson, S., Steenhuis, M. P., Althaus, M., Volkmar, F., et al. (2000). How unspecified are disorders of children with a pervasive developmental disorder not otherwise specified? A study of social problems in children with PDD-NOS and ADHD. European Child and Adolescent Psychiatry, 9(3), 168–179.
McBurnett, K. (2005). Attention-deficit/hyperactivity disorder: A review of diagnostic issues. In T. Widiger, A. Frances, H. A. Pincus, R. Ross, M. B. First, & W. Davis (Eds.), DSM-IV sourcebook (Vol. 3, pp. 111–144). Washington: American Psychiatric Association.
Monk, C. S. (2008). The development of emotion-related neural circuitry in health and psychopathology. Development & Psychopathology, 20(4), 1231–1250.
Monk, C. S., Weng, S.-J., Wiggins, J. L., Kurapati, N., Louro, H. M. C., Carrasco, M., et al. (2010). Neural circuitry of emotional face processing in autism spectrum disorders. Journal of Psychiatry & Neuroscience, 35(2), 105–114.
Moses, L. J., Carlson, S. M., & Sabbagh, M. A. (2005). On the specificity of the relation between executive function and children’s theories of mind. In W. Schneider, R. Schumann-Hengsteler, & B. Sodian (Eds.), Young children’s cognitive development: Interrelationships among executive functioning, working memory, verbal ability, and theory of mind (pp. 131–145). New Jersey: Lawrence Erlbaum Associates.
Mulligan, A., Anney, R. J., O’Regan, M., Chen, W., Butler, L., Fitzgerald, M., et al. (2009). Autism symptoms in attention-deficit/hyperactivity disorder: A familial trait which correlates with conduct, oppositional defiant, language and motor disorders. Journal of Autism and Developmental Disorders, 39(2), 197–209.
Nigg, J. T. (1999). The ADHD response-inhibition deficit as measured by the stop task: Replication with DSM-IV combined type, extension, and qualification. Journal of Abnormal Child Psychology, 27(5), 393–402.
Norvilitis, J. M., Casey, R. J., Brooklier, K. M., & Bonello, P. J. (2000). Emotion appraisal in children with attention-deficit/hyperactivity disorder and their parents. Journal of Attention Disorders, 4(15), 15–26.
Noterdaeme, M., Amorosa, H., Mildenberger, K., Sitter, S., & Minow, F. (2001). Evaluation of attention problems in children with autism and children with a specific language disorder. European Child and Adolescent Psychiatry, 10(1), 58–66.
Nyden, A., Gillberg, C., Hjelmquist, E., & Heiman, M. (1999). Executive function/attention deficits in boys with Asperger syndrome, attention disorder and reading/writing disorder. Autism Research, 3(3), 213–228.
Ozonoff, S., & Jensen, J. (1999). Brief report: Specific executive function profiles in three neurodevelopmental disorders. Journal of Autism and Developmental Disorders, 29(2), 171–177.
Ozonoff, S., Pennington, B. F., & Rogers, S. J. (1991). Executive function deficits in high-functioning autistic individuals: Relationship to theory of mind. The Journal of Child Psychology & Psychiatry, 32(7), 1081–1105.
Pelc, K., Kornreich, C., Foisy, M.-L., & Dan, B. (2006). Recognition of emotional facial expressions in attention-deficit hyperactivity disorder. Pediatric Neurology, 35(2), 93–97.
Petermann, F., & Petermann, U. (2007). Hamburg-Wechsler-Intelligenztest für Kinder – IV. Göttingen: Hogrefe.
Rühl, D., Bölte, S., Feineis-Matthews, S., & Poustka, F. (2004). ADOS, Autism Diagnostic Observation Schedule for autistic disorders [German]. Bern: Huber.
Rump, K. M., Giovannelli, J. L., Minshew, N. J., & Strauss, M. S. (2009). The development of emotion recognition in individuals with autism. Child Development, 80(5), 1434–1447.
Santosh, P. J., & Mijovic, A. (2004). Social impairment in hyperkinetic disorder—Relationship to psychopathology and environmental stressors. European Child and Adolescent Psychiatry, 13(3), 141–150.
Schachar, R., Tannock, R., Marriott, M., & Logan, G. (1995). Deficient inhibitory control in attention deficit hyperactivity disorder. The Journal of Abnormal Child Psychology, 23(4), 411–437.
Schultz, R. T. (2005). Developmental deficits in social perception in autism: The role of the amygdala and fusiform face area. International Journal of Developmental Neuroscience, 23(2–3), 125–141.
Schultz, R. T., Gauthier, I., Klin, A., Fulbright, R. K., Anderson, A. W., Volkmar, F., et al. (2000). Abnormal ventral temporal cortical activity during face discrimination among individuals with autism and Asperger syndrome. Archives of General Psychiatry, 57(4), 331–340.
Shue, K. L., & Douglas, V. I. (1992). Attention deficit hyperactivity disorder and the frontal lobe syndrome. Brain and Cognition, 20(1), 104–124.
Singh, S. D., Ellis, C. R., Winton, A. S., Singh, N. N., Leung, J. P., & Oswald, D. P. (1998). Recognition of facial expressions of emotion by children with attention-deficit hyperactivity disorder. Behaviour Modification, 22(2), 128–142.
Sinzig, J., Bruning, N., Morsch, D., & Lehmkuhl, G. (2007). [Age-dependent differences in neuropsychological performance profiles in ADHD and autism]. Zeitschrift für Kinder & Jugendpsychiatrie & Psychotherapie, 35(2), 95–104; quiz 105–106.
Sinzig, J., Morsch, D., & Lehmkuhl, G. (2008). Do hyperactivity, impulsivity and inattention have an impact on the ability of facial affect recognition in children with autism and ADHD? European Child and Adolescent Psychiatry, 17(2), 63–72.
Sinzig, J., Walter, D., & Doepfner, M. (2009). Attention deficit/hyperactivity disorder in children and adolescents with autism spectrum disorder: Symptom or syndrome? Journal of Attention Disorders, 13(2), 117–126.
Sodian, B., & Hülsken, C. (2005). The developmental relation of theory of mind and executive functions: A study of advanced theory of mind abilities in children with ADHD. In W. Schneider, R. Schumann-Hengsteler, & B. Sodian (Eds.), Young children’s cognitive development: Interrelationships among executive functioning, working memory, verbal ability, and theory of mind (pp. 175–188). New Jersey: Lawrence Erlbaum Associates.
Tewes, U. (1993). Hamburg-Wechsler-Intelligenztest für Erwachsene-Revision. Göttingen: Hogrefe.
Tewes, U., Rossmann, R., & Schallberger, R. (1999). Hamburg-Wechsler-Intelligenztest für Kinder. Dritte Auflage. Bern: Huber.
Unnewehr, S., Schneider, S., & Margraf, J. (1998). Kinder-DIPS—Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter. Berlin: Springer.
Webb, S. J., Dawson, G., Bernier, R., & Panagiotides, H. (2006). ERP evidence of atypical face processing in young children with autism. Journal of Autism Developmental Disorders, 36(7), 881–890.
WHO. (1993). Internationale Klassifikation psychischer Störungen (2nd ed.). Bern, Toronto: World Health Organization.
Yoshida, Y., & Uchiyama, T. (2004). The clinical necessity for assessing attention deficit/hyperactivity disorder (AD/HD) symptoms in children with high-functioning pervasive developmental disorder (PDD). European Child and Adolescent Psychiatry, 17(2), 307–314.
Zimmermann, P., & Fimm, B. (1993). Die Testbatterie zur Aufmerksamkeitsprüfung (TAP). In G. Büttner & L. Schmidt-Atzert (Eds.), Diagnostik von Konzentration und Aufmerksamkeit. Jahrbuch der pädagogisch-psychologischen Diagnostik (pp. 177–202). Göttingen: Hogrefe.
Acknowledgments
Dr Kamp-Becker was paid for public speaking by Medice. There is no conflict of interest for all other authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bühler, E., Bachmann, C., Goyert, H. et al. Differential Diagnosis of Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder by Means of Inhibitory Control and ‘Theory of Mind’. J Autism Dev Disord 41, 1718–1726 (2011). https://doi.org/10.1007/s10803-011-1205-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-011-1205-1