Abstract
Background
We examined the association between childhood poverty and mental health disorders (MHD) in childhood and early adulthood. We also investigated whether the association between poverty in childhood and MHD is mediated by exposure to stressful life events (SLE).
Methods
We used data from a prospective community cohort of young people assessed at baseline (M = 9.7 years, SD = 1.9), first (M = 13.5 years, SD = 1.9), and second (M = 18.2 years, SD = 2.0) follow-ups (N = 1,590) in Brazil. Poverty was assessed using a standardized classification. Exposure to 20 different SLE was measured using the Life History instrument. Psychiatric diagnoses were evaluated using the Development and Well-Being Assessment. Latent growth models investigated the association between poverty at baseline and the growth of any MHD, externalizing, and internalizing disorders. Mediation models evaluated whether the association between childhood poverty and MHD in early adulthood was mediated by exposure to SLE.
Results
Poverty affected 11.4% of the sample at baseline and was associated with an increased propensity for presenting externalizing disorders in adolescence or early adulthood (standardized estimate = 0.27, p = 0.016). This association was not significant for any disorder or internalizing disorders. Childhood poverty increased the likelihood of externalizing disorders in early adulthood through higher exposure to SLE (OR = 1.07, 95 CI% 1.01–1.14). Results were only replicated among females in stratified analyses.
Conclusions
Childhood poverty had detrimental consequences on externalizing MHD in adolescence, especially among females. Poverty and SLE are preventable risk factors that need to be tackled to reduce the burden of externalizing disorders in young people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poverty is a complex phenomenon composed of overlapping deprivations that entail more than the lack of income [1]. Over one billion children and adolescents worldwide are multidimensionally poor, meaning that they face deprivation in nutrition, housing, sanitation, health, education, and other areas of life [2]. Mental health (MH) problems in childhood are one of several possible adverse consequences of living in poverty [3, 4]. However, it is unclear the extent to which poverty during childhood impacts the development of externalizing and internalizing disorders later in life and how exposure to stressful life events (SLE) may contribute to the association between poverty and mental health disorders (MHD). Exploring these questions can provide us clues to potentially preventable risk factors—poverty and SLE—that could be tackled to reduce the prevalence of MHD in young people. This is particularly important if we consider that MH problems can have long-term impacts on health and social outcomes into adulthood, including low educational attainment and criminal activities [5,6,7,8,9], increasing the likelihood of remaining in poverty [10].
A positive association either between poverty or social disadvantage and MH problems among young people has been consistently reported [3, 4, 10,11,12,13]. Yet, the significance and magnitude of this association is highly heterogeneous, depending on the study design, indicators of poverty, populations, and diverse outcomes assessed in particular investigations [3, 4]. For example, cross-cultural differences were observed in a study conducted with adolescents aged 12–18 from 12 European countries [14]. Interestingly, low economic status increased the odds of MH problems by 1.41 (95% CI 1.18–1.69) for the combined sample, whereas results disentangled by country only showed a significant association in Spain and the United Kingdom. Among poverty indicators, low household income and low parental education appear to have a stronger association with MH, when compared to parental unemployment or low occupational status [3, 4]. A study conducted by McLaughlin et al. [12] compared the relative impact of childhood financial hardship, low parental education, and parental occupation on the onset, severity, and persistence of MHD during childhood, adolescence, early adulthood, and middle-later adulthood. They found that childhood financial adversity predicted the onset of MHD only during childhood (OR = 1.3, 95% CI 1.0–1.6), while low parental education did not predict the onset but predicted MHD severity (OR = 1.7, 95% CI 1.1–2.6) and persistence of behavioral MHD (OR = 1.6, 95% CI 1.0–2.7) across life-course stages. Parental occupation was not associated with MHD. This suggests that financial hardship can have acute detrimental impacts during childhood, while lower parental education may impact the course of MHD later in life.
Regarding outcomes assessed, systematic reviews [3, 4] show that poverty tends to be more strongly associated with the incidence of externalizing conditions (conduct disorder, oppositional defiant disorder, and attention-deficit/hyperactivity disorder [ADHD]) than with internalizing conditions (anxiety and depression). Moreover, there are natural experiments [13] and quasi-experimental studies [15] showing that improvements in poverty were associated with a small, significant reduction in externalizing problems but had null effects on internalizing problems. A different pattern was observed in the unique cohort study conducted in Brazil exploring the association between changes in poverty (income tertile) status from birth to 11 years on MH outcomes at the age of 15 [16]. Children who were poor at birth had higher attentional/hyperactivity problems at age 15, even if they were out of poverty at age 11 (β = 0.450, p < 0.05), and no association between poverty and emotional problems was found.
The literature is not clear as to why poverty would have this differential impact on externalizing versus internalizing disorders among young people. One hypothesis raised [13, 15] is that malnutrition among children living in poverty may impact neurocognitive development specifically related to externalizing disorders. However, the unique longitudinal study that examined the association between food insecurity and MHD found a similar impact on both externalizing and internalizing disorders [11]. Another study [17] found that early adverse experiences, including poverty, altered connectivity in the inferior frontal gyrus (brain region important for impulse control and emotion regulation), predicting greater externalizing symptoms over childhood and early adolescence but not internalizing symptoms. However, internalizing MHD typically emerge later in adolescence [10], and the number of longitudinal studies on the long-term effects of childhood poverty is limited. Similarly, most longitudinal studies in this area focus on the incidence of MH problems at a specific end-point and do not use appropriate statistical methods that take account of individual and inter-individual variation in change of psychiatric disorders over time [18]. Latent growth models are a useful statistical approach to evaluate the underlying development of MHD in longitudinal studies and can help to understand: why do some children increase or decrease their propensity to present any, externalizing or internalizing MHD over time? [19, 20]. The use of latent growth models is particularly relevant to understanding whether and how poverty is associated with the development of MHD across youth [18].
Even if this association is identified, it is important to better understand the mechanisms underlying the relationship between poverty and MH. SLE, such as the death of parents or relatives, exposure to accidents, family conflicts, and school problems, among others, occur more often among poor children and adolescents than their non-poor peers [21]. Furthermore, the effect of SLE on brain systems, such as reductions in the medial prefrontal cortex, hippocampal and amygdala volume, involved in the development of behavioral and emotional issues is well documented [22]. However, there is a lack of longitudinal studies investigating whether SLE act as a mediator for the impact of poverty on young people’s MH. This evaluation can provide us with insights into preventable risk factors—SLE—that can be addressed to reduce the prevalence of MH conditions.
Additionally, we have identified other gaps in the literature to disentangle the effect of poverty on young people’s MH. First, evidence of the effect of poverty on MH is limited by definitions of poverty that include only one or two indicators of socioeconomic disadvantage, usually family income, parental occupation, or education [3, 4]. As stated earlier, poverty is a multidimensional phenomenon, which can be comprised of several deprivations that go beyond the lack of income, such as low education, sanitation, and housing conditions [1, 2]. A critical review on the measurement of poverty in psychiatric epidemiology [23], recommends the use of compressive indicators that can capture the complexity of poverty when evaluating its potential effect on MH. Second, adolescence represents a critical period for the development of psychiatric disorders. MHD account for 16% of the global burden of disease and injury in people aged 10–19 [24], and half of all MHD start by 14 years of age [25]. Nonetheless, little is known about the effect of poverty during the critical periods of adolescence (early, middle, and later adolescence). Moreover, to the best of our knowledge, there are no longitudinal studies evaluating the effect of poverty on the trajectory of adolescent MHD (e.g., with more than one follow-up) in low- and middle-income countries, where nearly 90% of the world’s adolescent population lives [26]. Third, most studies have used general screening measures of emotional and behavioral problems to assess MH, and little is known about the effect of poverty on the trajectory of psychiatric diagnoses [10, 12]. The assessment of diagnosis can identify individuals presenting a MH condition that produces impacts on daily life, a fundamental stage to orient and prioritize interventions and policies. Fourth, few studies have controlled for parental and child psychopathology at the point of exposure [3].
In this study, we examined the association between childhood poverty and growth in any, externalizing, and internalizing MHD, from childhood to early adulthood through the application of latent growth curve models. Furthermore, to advance our understanding of the mechanisms by which living in poverty may be associated with the development of MHD among young people, we investigated whether poverty was associated with increased exposure to SLE and whether this, in turn, was associated with an increase in MHD in early adulthood. We hypothesized that a) poverty during childhood would be associated with the growth of psychiatric disorders in adolescence and early adulthood; b) the magnitude of this association would be stronger in relation to externalizing disorders, compared to internalizing disorders; and c) the effect of poverty on externalizing disorders would be mediated by higher exposure to SLE among young people living in poverty.
Methods
Participants
We analyzed data from the Brazilian High-Risk Cohort (BHRC), an ongoing prospective longitudinal study conducted in São Paulo and Porto Alegre, Brazil. A detailed description of the sample and procedures can be found elsewhere [27]. Briefly, during the registry day, 12,500 parents of children aged 6–14, attending 57 schools (22 in Porto Alegre and 35 in São Paulo), were invited to a screening interview using the Family History Screen (FHS) [28]. The FHS is used to screen all family members for Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM‐IV) MHD. A total of 8012 families (9937 eligible children, 45394 family members) were interviewed with the FHS (primary informant in 87% of cases was the biological mother). An index of family load was computed for each of the potential eligible children based on the percentage of members in the family that screened positively for each of the disorders assessed, adjusted for relatedness. Finally, the cohort was composed of 2511 children; 957 were randomly selected, and 1554 were a sub‐sample of children at increased risk of mental disorders based on FHS. Data of the present study were collected at baseline when children were aged 6–14 years (T0: 2010–2011, n = 2511), at first follow-up (T1: 9–17 years, 2014–2015, N = 2010) and second follow-up (T2: 15–23 years, 2018–2019, N = 1905, where we included 1796 [94.3%] participants who completed the socioeconomic evaluation). A total of 1590 individuals (63% from the original cohort) participated at the three assessments (206 individuals did not participate at first follow-up and were reached at second follow-up).
All procedures were approved by the Ethics Committee of the Federal University of São Paulo and Hospital de Clínicas de Porto Alegre. Child assent and parental informed consent were obtained from the research subjects.
Exposure
Childhood poverty was defined according to the poverty status reported by caregivers/parents at baseline using a standardized questionnaire created by the Brazilian Association of Research Companies with the aim of stratifying households according to the Brazilian Economic Classification Criteria [29]. This instrument evaluates (1) head of household education; (2) assets (number of bathrooms, domestic workers, cars, computers, dishwashers, refrigerators, freezers, washing machines, DVD players, microwave ovens, motorcycles, and clothes dryers); and (3) access to public utility services (piped water and paved streets). A total score ranging from 0 to 46 is given. According to the 2010 Brazilian criteria thresholds [29, 30], households with scores ≤ 13 are part of the poorest strata of the population. We classified as “poor” cohort participants with total scores ≤ 13 and “non-poor” participants were those who scored > 13. This instrument has been widely used in Brazilian epidemiological studies (see, for example, [31]) and has also been used as a proxy of poverty to evaluate the impacts of anti-poverty interventions [32]. This classification has been considered a good proxy of poverty and extreme poverty using income-based approaches [22, 23] but with the advantage of considering diverse deprivations faced by children living in poverty: poor housing conditions, low parental education, lower purchasing power, and low access to basic services. This approach is consistent with the definition of poverty as a multidimensional phenomenon adopted by the United Nations [1].
Outcomes
Any psychiatric diagnosis at T1 and T2 were assessed using the Brazilian-Portuguese version of the Development and Well-being Assessment (DAWBA) [33, 34], which is a highly structured interview used to generate DSM-IV diagnoses. The validation of the Brazilian-Portuguese version [34] showed an agreement between DAWBA diagnoses and clinical diagnoses of 78%, and the inter-rater reliabilities were k = 0.93 for any disorder, k = 0.91 for internalizing disorders, and k = 1.0 for externalizing disorders. Trained interviewers gathered information on current problems causing significant distress or social impairment. Baseline diagnostic assessment was performed considering only caregivers’ reports. At T1, the diagnostic assessment was performed considering caregivers’ reports and additional information from interviews with the young people about internalizing conditions. At T2, caregivers’ and youths’ reports were considered for all diagnoses. Computerized diagnostic probabilities were then generated based on responses, which were carefully evaluated by nine trained psychiatrists who ascertained the diagnoses. Baseline psychiatric diagnoses were used to estimate the intercepts in the latent growth models.
Broad psychiatric diagnostic categories at T1 and T2: Based on previous literature [35], DAWBA diagnoses were grouped into two broad categories: internalizing disorders (including distress-related diagnoses: depression, generalized anxiety disorder, obsessive–compulsive disorder, tic, eating disorder, and fear-related disorders: panic, agoraphobia, social anxiety, specific phobia, and separation anxiety) and externalizing disorders (including conduct disorder, oppositional defiant disorder, and ADHD). An additional category of comorbidity was generated for individuals with internalizing and externalizing diagnoses.
Potential mediator
Stressful life events at T1 and T2 were reported by parents/caregivers using the Life History instrument, created by BHRC’s authors [27] based on a literature review of instruments that assess youth’s exposure to common SLE [36]. The instrument assesses exposure to 20 different SLE since the last follow-up. Participants were also asked if the exposure generated any perceived problems for their child. Each item was scored 0 = no exposure to the event, 1 = exposure to the event but no perceived problem due to exposure, or 2 = exposure to the event and perceived problem due to exposure. More details on the development of the SLE variable are presented in Online Resource 1. Briefly, exploratory factor analysis yielded a five-factor solution that was submitted to confirmatory factor analysis. The final latent model was comprised of a high-order factor named “SLE,” informed by five first-order factors that showed a good fit to the data. The five first-order factors were classified as “unpredictable event-related stressors” (informed by the items victim of a robbery, victim of a robbery with physical violence, car accident, the house burned down or flooded [or other natural catastrophes]), “interpersonal-related stressors” (items: parental divorce, constant fights between family members, parental unemployment, serious household financial problems, important problems with friends), “context change-related stressors” (items: moving to another house, moving to another school, and moving to another city), “school-related stressors” (items: school suspension, school drop-out, school failure, and school expulsion), and “health/loss-related stressors” (items: death of parents, death of relative or friend, pet’s death [or runaway], and serious health problem of a close relative or friend). A total score ranging from 0 to 40 was generated at each follow-up, and we also created a cumulative SLE score by adding T1 and T2 scores. Cumulative sub-scores, according to the five types of events, were also computed. Prevalence of exposure to each event is presented in Online Resource 1.
Confounders
We considered as potential confounders the following baseline characteristics (provided by caregivers): gender, age, ethnicity (white and non-white: Black, Asian, indigenous or mixed race), maternal current psychiatric condition using the Mini International Psychiatric Interview Plus [37], and perinatal risk factors: preterm childbirth, any tobacco use during pregnancy, any alcohol consumption during pregnancy, and whether the mother was an adolescent at childbirth (< 18 years).
Data analysis
To reduce attrition bias, all analyses were adjusted using inverse propensity score weighting (IPSW) [38]. Probit regression models were used to estimate baseline variables that predicted the propensity of attrition at T2. Site (São Paulo), full-term pregnancy, no child, and maternal psychiatric diagnosis predicted attrition at follow-up. The predicted probabilities of attrition were used to estimate propensity scores. According to these scores, complete cases were weighted by the inverse of their probability of being a complete case [38]. These IPSW were used as sample weights to adjust all the analysis, to reproduce the baseline sample profile.
We first present the bivariate association between poverty status at baseline and sociodemographic characteristics, perinatal risk factors, and baseline psychiatric diagnosis using logistic regression models. We then present the bivariate association between poverty at baseline and poverty status (logistic regression) and SLE (generalized linear models). To describe the prevalence of psychiatric diagnosis by poverty status, we present the bivariate association between poverty and psychiatric diagnosis at T1 and T2 using logistic (for any psychiatric diagnosis) or multinomial (for broad diagnostic group) regression models. Potential covariates associated with psychiatric diagnosis at both follow-ups were evaluated using bivariate logistic and multinomial regression models. These analyses were conducted using Stata version 16 [39]. We adopted a significance level of 5% (two-tailed).
Latent growth curve models (LGCM)
Categorical LGCM tested the association between poverty in childhood and the growth of any psychiatric disorder (Model 1) and type of broad psychiatric diagnostic groups (Model 2: externalizing disorders and Model 3: internalizing disorders), using Mplus version 8.6 [40]. In LGCM, repeated categorical indicators can be specified in the measurement model and the growth factors – the intercept, or initial level, and the slope, or the rate of change over time – can be specified as latent variables in the structural part of the model [19, 20]. LGCM can evaluate growth underlying the observed clinical diagnosis presentation at each time point and estimate which characteristics would be associated with the variability on the rate of change of psychiatric diagnosis over time [19, 20].
We first specified unconditional models (i.e., models without observed predictors) to evaluate the model fits and the variability of growth factors (intercept and slope) of psychiatric diagnosis. Significant slope variance suggests inter-individual differences surrounding the average rate of change and would justify investigating predictors of this variability through conditional models. The model specification of categorical LGCM [19, 20] includes continuous latent response variables as growth indicators (intercept and slope), and the thresholds are set to be invariant over time. The covariance between a person’s starting value (intercept) is set to correlate with his/her rate of change (slope). The time was centered at baseline (0), and subsequent time intervals were specified as 1 and 2.3 (due to three-year and four-year intervals between follow-ups).
In the second stage, as LGCM allow for the prediction of the subsequent outcome by the growth factors and other predictors within the same model [20], we specified conditional models, including our main predictor (poverty at baseline) and covariates. Models 1, 2, and 3 had similar covariates. Poverty at baseline and other time-invariant covariates (sex, gender, perinatal risk factors, and maternal MH at baseline) were regressed on the intercept and the slope those, in turn, predicted the presentation of diagnosis at follow-ups. Time-varying covariates (age and poverty) at each follow-up were regressed on the diagnosis presented at the respective time point (e.g., age and poverty at T1 on diagnosis at T2). We present standardized results (STDY) of the fixed-effect prediction of the random intercepts (γi) and slopes (γs) by each predictor. STDY can be interpreted as analogous to Cohen’s d effect sizes, where 0.20, 0.50, and 0.80 would indicate small, medium, and large effects, respectively, on a standardized unit of the outcome [41].
LGCM analyses were performed using the mean- and variance-adjusted weighted least squares estimator (WLSMV). The evaluation of the model’s fit was conducted using the following indices: Root Mean Square Error of Approximation (RMSEA < 0.06), the Comparative Fit Index (CFI > 0.90), and the Tucker–Lewis Index (TLI > 0.90) [41]. All models included the IPSW as sampling weight to reduce attrition bias.
Sensitivity analyses
Sensitivity analyses were conducted for all LGCM using an alternative categorization of poverty based on low household income, where the first decile of the cohort was classified as poor, and participants between the second and tenth deciles were classified as non-poor. We also conducted stratified analysis by gender.
Mediation model
In a final step, for those outcomes that significantly associated with poverty according to the LGCM, we performed mediation models (using Mplus version 8.6 [40]) to test whether the effect of poverty during childhood on the presentation of psychiatric diagnosis at the second follow-up was mediated by cumulative exposure to SLE (combined total and specific scores by types of events from T1 and T2). We used the maximum-likelihood estimator, and the model adjusted for gender, baseline psychiatric diagnosis, maternal psychiatric diagnosis, whether the mother was an adolescent at childbirth and/or smoked during pregnancy, and state. The indirect effect was estimated using the bootstrap bias-corrected method that generates 95% confidence intervals (CI) [42]. CIs that do not include zero indicate significant effects. We used 10000 bootstrap replications for the analyses [42]. Finally, to examine potential moderation effect by gender, multigroup mediation analyses were performed for all models using gender as the grouping variable.
Results
From the original cohort (n = 2511), a total of 1796 (71.5%) individuals were reached seven years later at T2. Online Resource 2 shows baseline characteristics that predicted attrition (site [São Paulo], full-term pregnancy, no child, and maternal psychiatric diagnosis) and how differences between the original and completed sample were attenuated using IPSW.
Poverty affected 205 (11.4%) cohort participants at baseline. Table 1 shows the sample description and child and family characteristics associated with poverty. Poor participants were more likely to be Black and indigenous, to live in Porto Alegre, to have mothers with low education, who smoked during pregnancy. There were no differences in other sociodemographic, clinical, and perinatal characteristics, according to poverty status at baseline.
Online Resource 3 presents the bivariate association between poverty at baseline and clinical outcomes, poverty status, and SLE at follow-ups. Overall, between baseline and T2, there was a reduction in externalizing disorders and an increase in internalizing disorders. Poverty at baseline was associated with remaining in poverty and with increased exposure to SLE at both follow-ups. The association between poverty at baseline and the rate of externalizing disorders at T2 was marginally significant. Bivariate analysis by specific types of externalizing diagnoses showed that poverty at baseline was associated with the presentation of an ADHD diagnosis at T2 (OR = 2.11, CI 95% 1.10–4.17, p = 0.032).
We then investigated potential sociodemographic, family, and perinatal covariates associated with psychiatric diagnosis at the second follow-up. Female gender, smoking during pregnancy, and maternal psychiatric diagnosis were associated with any psychiatric disorder at T2 (Online Resource 4). Characteristics associated with internalizing diagnosis were female gender and maternal psychiatric diagnosis (Online Resource 5). Externalizing diagnoses were associated with site (São Paulo), adolescent mother at childbirth, smoking during pregnancy, and maternal psychiatric diagnosis. Comorbidity was associated with maternal psychiatric diagnosis.
LGCM
Model 1: association between poverty and any psychiatric disorder
We first tested whether poverty at baseline was associated with the growth of any psychiatric diagnosis over time. The unconditional LGCM (i.e., model without covariates) is presented in Online Resource 6. Figure 1A presents the conditional LGCM for Model 1 where we added our main predictor, poverty at baseline, and additional time-invariant and time-varying covariates. This model had an acceptable fit to the data (RMSEA = 0.03, CFI = 0.95, TLI = 0.88). Poverty at baseline was not associated with the growth of any psychiatric diagnosis (γi = -0.16, p = 0.279, γs = 0.25, p = 0.170). Poverty at subsequent follow-ups was also not associated with the presentation of any psychiatric disorder at any time point.
Latent growth model: the effect of poverty at baseline on the trajectory of any mental health disorders. Notes: Standardized estimates are showed. **Significant at the 5% level. Observed repeated outcomes were any psychiatric diagnosis at baseline (Diag0), at first (Diag1) and second (Diag2) follow-ups. Time-invariant covariates regressed on the intercept and slope: Poverty at baseline (Pov0), gender, maternal mental health diagnosis (Mini International Psychiatric Interview Plus) and smoking during pregnancy (Smok)
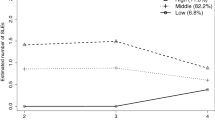
Broad psychiatric diagnosis: externalizing diagnosis (Model 2)
We then analyzed whether childhood poverty was associated with the growth of psychiatric diagnosis at both follow-ups by type of diagnosis. In Model 2, the reference category was no diagnosis versus externalizing diagnosis. The unconditional LGCM results are presented in Online Resource 7. Figure 2A presents the conditional LGCM for Model 2. This model had a good fit to the data (RMSEA = 0.03, CFI = 0.96, TLI = 0.92). Childhood poverty was associated with lower levels of externalizing disorders at baseline (γi = − 0.27, p = 0.023) but was associated with growth in externalizing conditions at follow-ups (γs = 0.27, p = 0.016). This means that children from poor families had an average level of externalizing disorders 0.27 standard deviations lower compared with non-poor participants at baseline, but their propensity to present externalizing disorders increased over time, surpassing non-poor participants. In terms of probabilities [40], poor children had increased probability of presenting externalizing disorders by 0.63, while the probability among non-poor children decreased by 0.37 over time. Poverty status at T1 and T2 was not associated with the presentation of externalizing disorders at either time point.
Latent growth models: the effect of poverty at baseline on the trajectory of externalizing and internalizing disorders. Fig. 2A Broad diagnostic group: externalizing disorders. Fig. 2B Broad diagnostic group: internalizing disorders. Notes: Standardized estimates are showed. **Significant at the 5% level. Time-invariant covariates regressed on the intercept and slope: Poverty at baseline (Pov0), gender, maternal mental health diagnosis (Mini), state, adolescent mother at childbirth (Mothad) and smoking during pregnancy (Smok). Time-varying covariates for both models: age and poverty at T1 (Pov1) and T2 (Pov2)
Broad psychiatric diagnosis: internalizing diagnosis (Model 3)
In Model 3, the outcome of reference was no diagnosis versus internalizing diagnosis. The unconditional LGCM results are presented in Online Resource 8. Figure 2B presents the conditional LGCM for Model 3. Overall, this model presented an acceptable fit to the data (RMSEA = 0.03, CFI = 0.92, TLI = 0.86). Poverty at baseline was associated with lower initial levels of internalizing disorders (γi = − 0.33, p = 0.015) but was not associated with the growth of internalizing diagnosis over time (γs = 0.21, p = 0.177). This means that participants from poor families were more likely than those who were non-poor to exhibit lower levels of internalizing disorders at baseline (0.33 standard deviations), but their propensity for presenting internalizing disorders over time reached similar levels of non-poor participants.
Sensitivity analysis
A non-significant association between low household income and the trajectory of general, externalizing, and internalizing psychiatric disorders (Online Resource 9) was found in sensitivity analyses. Results of general and internalizing psychiatric diagnoses were similar for both genders. However, we only observed an association between poverty and growth in externalizing disorders over time among females (γs = 0.34, p = 0.034) (Online Resource 10).
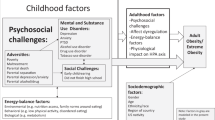
Mediation model: the effect of poverty on externalizing disorders through SLE
A mediation analysis examined the indirect effect of childhood poverty on externalizing diagnoses at T2 through greater exposure to SLE. For ease of interpretation, these results are shown in Fig. 3. The indirect effect of childhood poverty on the increased odds of externalizing disorders at T2 through SLE was statistically significant, and the direct effect of poverty on externalizing disorders became non-significant with the inclusion of SLE in the model, suggesting a totally mediated effect. This means that children living in poverty had greater exposure to SLE compared to non-poor children, and this exposure increased their propensity for presenting externalizing disorders later in early adulthood. Results by specific types of events (Online Resource 11) showed an indirect effect from interpersonal and health/loss-related stressors. Multigroup mediation analyses (Online Resource 12) were only significant for females, suggesting a moderation effect of gender on the mediation between poverty and externalizing disorders through overall, interpersonal, school, and health/loss-related SLE.
Poverty at baseline and externalizing disorders at T2: The indirect effect of cumulative stressful life events. Notes: **p < 0.05. Model adjusted by age, gender, smoking during pregnancy, maternal psychiatric diagnosis (all had a p > 0.05), and externalizing diagnosis at baseline (p < 0.001). Standardized direct effects are showed. Predictor: Poverty at baseline (Poverty0). Outcome: externalizing disorder at T2 (Ext2). Continuous Mediator: cumulative stressful life events between T1 and T2 (SLE)
Discussion
We investigated the association between childhood poverty and the development of MHD across adolescence and early adulthood in a large community cohort of young people in Brazil. The results revealed a complex association between poverty and the trajectory of MHD: Poverty was associated with decreased initial levels of both internalizing and externalizing disorders in childhood, but children living in poverty showed increased externalizing disorder levels across adolescence and early adulthood compared with non-poor children. This positive association with externalizing disorders was mediated by increased exposure to SLE. Results were only replicated for females in stratified analyses, suggesting a moderating role of gender on the development of externalizing disorders associated with poverty.
The lower initial levels of internalizing and externalizing disorders among poor versus non-poor children was an unexpected result considering previous evidence [3, 4]. Because this is a cross-sectional result (i.e., the contemporaneous effect of poverty on MH), it requires cautious interpretation. However, this finding is in line with the results of a study conducted in one of the least developed regions of Brazil, which showed that low income at birth was associated with a reduced risk of emotional problems when children were aged 7–9 years [43]. A possible explanation is that, in our study, poverty at baseline was not associated with important risk factors for psychopathology [44], such as perinatal risk factors (alcohol consumption during pregnancy, preterm childbirth, adolescent mother) and maternal psychiatric diagnosis. It is also possible that unobserved confounders, such as religiosity [45] and family support [46], may have contributed to lower initial levels of psychopathology among poor children, but this hypothesis needs to be confirmed in further studies.
We found a harmful effect of childhood poverty on the development of externalizing disorders across adolescence, even controlling for poverty status at each follow-up. This suggests that the consequences of living in poverty during childhood had detrimental consequences later in adolescence. This is in line with the findings of McLaughlin et al. [12], who reported that lower parental education predicted persistence and severity of MH problems but not their onset, whereas financial problems predicted the onset but not the course of MH problems. Our sensitivity analysis suggested that poverty indexed by low household income was not associated with MHD, reinforcing the value of including comprehensive measures of poverty to understand its potential impacts on MH [23]. We used broad measures of poverty, including parental education, purchase power, housing conditions, and access to public utilities. These may reveal their effect on MH later than the cross-sectional effect of acute financial problems [12].
As in the majority of the literature in this area, we also found that the effect of poverty on MH was stronger on externalizing disorders compared to internalizing disorders [3, 4, 13]. As stated earlier, there are no clear explanations on why poverty would have this differential impact on externalizing versus internalizing disorders. Potential pathways that need to be investigated include the differential impacts of community violence, inequality, access to low-quality schools, and malnutrition faced by young people living in poverty on the development of externalizing versus internalizing disorders [46]. It is also possible that we will be able to observe the effect of poverty on internalizing disorders later in adulthood [47] in future cohort follow-ups.
A novel result that we found is the mediation effect of SLE, which helps to explain the association between childhood poverty and externalizing disorders in early adulthood. Children living in poverty had greater exposure to cumulative, interpersonal, and health/loss-related SLE during adolescence. Non-poor children had a decreased likelihood of presenting externalizing disorders over time, whereas poor children had an increased propensity for presenting externalizing disorders later in adolescence. Regarding type of SLE, interpersonal and loss/health-related stressors were the main drivers of this mediation. This result is in line with previous studies showing a positive association between poverty and SLE [21] and between SLE and externalizing disorders [48], but these pathways have only been tested using cross-sectional data from adolescents living in a high-income country [49]. In the cited study, environmental stressors (including family conflicts and illness/death of relatives and friends) also had a stronger indirect effect between poverty and externalizing problems compared to person-related (school, accidents, and violence) SLE.
Interestingly, results of stratified analyses suggested a moderation effect of gender, where females were at higher risk of the negative impacts of poverty on the development of externalizing disorders. This is particularly interesting because males are usually at higher risk of externalizing conditions [50]. However, our result is in line with one study conducted in the United States [51] that found a small but significant negative association between low household income at age 5 and the growth in externalizing problems only among females by the age of 17. However, they also found an association with internalizing problems that was not replicated in our study. Our mediation analyses moderated by gender are particularly useful for understanding the impact of vulnerabilities and SLE, which are more commonly faced by poor girls and which increase their chances of developing externalizing disorders that could be attenuated if not exposed to preventable risk factors, such as poverty and SLE. Particularly, girls living in poverty were more exposed to school, interpersonal, and health/loss-related stressors.
We have two interpretations of these findings. First, childhood poverty, by definition, is associated with lower access to health and high-quality educational services [2]. This may decrease the chances of early detection of externalizing symptoms, especially among girls that are less expected to present these symptoms [50]. These girls started with lower levels of externalizing disorders but were more likely to present school-related stressors (suspension, drop-out, repetition, and expulsion) during adolescence, increasing their externalizing problems over time. This finding reinforces the need for including educational and health components into anti-poverty interventions [2], especially if we consider that low educational attainment diminishes the likelihood of overcoming poverty. Second, different cultural roles may increase the burden of SLE among females [52]. Girls living in poverty were also exposed to greater interpersonal and health/loss-related stressors. Gender-based violence, diverse roles as carers [52], for example, caring for younger siblings or sick relatives, may elevate the burden and stress on female adolescents, increasing their propensity to develop externalizing conditions.
Strengths of this study include its contribution to understanding the association between poverty and the trajectory of MHD among young people in a middle-income country. We analyzed data collected prospectively from a large school-based cohort, enriched for psychiatric disorders. The use of a validated measure of psychiatric disorders and a comprehensive measure of poverty are also strengths of our study.
Nevertheless, a few limitations need to be considered. First, there was attrition among the cohort. However, we handled potential selection effects using data weighting methods. Second, SLE were reported by parents, who are not necessarily aware of some events that youth may face (e.g., problems with friends or loss/health problems of a friend). However, we have no reason to hypothesize that poverty status may contribute to underreporting of SLE. Third, we investigated the growth of psychiatric disorders across three time-points, which is the minimum to analyze LGCM. Further waves will allow us to investigate the impact of changes in poverty status over time on the growth of psychiatric disorders and to explore alternative growth shapes (e.g., quadratic). Fourth, we did not include a measure of inequality that could help us to differentiate the effects of poverty and inequality on MH [53]. Finally, we use a measure of poverty standardized for the Brazilian population that is not necessarily generalizable to other contexts. However, we also present sensitivity analysis using a low household income criterion.
Our results support previous research that childhood poverty can lead to negative consequences on MH in adolescence and early adulthood. Our findings are particularly useful for understanding the impact of poverty on the development of externalizing disorders, especially among females. Moreover, as externalizing disorders can have long-term impacts on health and social outcomes into adulthood, these findings reinforce the importance of anti-poverty interventions early in life. Understanding how adversities lead to MH problems during upbringing can inform early identification and interventions, which is particularly important in countries with limited access to MH care. For this reason, further research in low- and middle-income countries are needed to improve our understanding of the impacts of poverty on the development of externalizing disorders across the lifespan and to evaluate interventions that aim to reduce poverty, to strengthen resilience toward mental disorders, and to reduce externalizing behaviors among young people living in poverty [54].
Availability of data and material
CZ have full access to all the data used in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Data were provided by the Brazilian High-Risk Cohort study and are available upon request in the Open Science Framework public repository (https://osf.io/ktz5h/).
Code availability
Please, contact the corresponding author.
References
United Nations (2020) Ending poverty. https://www.un.org/en/sections/issues-depth/poverty/index.html. Accessed 31 Jul 2020
UNICEF (2021) Child poverty. https://www.unicef.org/social-policy/child-poverty. Accessed 18 Feb 2021
Reiss F (2013) Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med 90:24–31. https://doi.org/10.1016/j.socscimed.2013.04.026
Levesque AR, MacDonald S, Berg SA, Reka R (2021) Assessing the impact of changes in household socioeconomic status on the health of children and adolescents: a systematic review. Adolesc Res Rev. https://doi.org/10.1007/s40894-021-00151-8
Knapp M, King D, Healey A, Thomas C (2011) Economic outcomes in adulthood and their associations with antisocial conduct, attention deficit and anxiety problems in childhood. J Ment Health Policy Econ 14:137–147
Kim-Cohen J, Caspi A, Moffitt TE et al (2003) Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry 60:709–717. https://doi.org/10.1001/archpsyc.60.7.709
Richards M, Abbott R (2009) Childhood mental health and life chances in post-war Britain. Insights from three national birth cohort studies. The Smith Institute, Sainsbury Centre for Mental Health & Unison, London
Chen H, Cohen P, Kasen S et al (2006) Impact of adolescent mental disorders and physical illnesses on quality of life 17 years later. Arch Pediatr Adolesc Med 160:93. https://doi.org/10.1001/archpedi.160.1.93
Fergusson DM, John Horwood L, Ridder EM (2005) Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry 46:837–849. https://doi.org/10.1111/j.1469-7610.2004.00387.x
Miech RA, Caspi A, Moffitt TE et al (1999) Low socioeconomic status and mental disorders: a longitudinal study of selection and causation during young adulthood. Am J Sociol 104:1096–1131. https://doi.org/10.1086/210137
Slopen N, Fitzmaurice G, Williams DR, Gilman SE (2010) Poverty, food insecurity, and the behavior for childhood internalizing and externalizing disorders. J Am Acad Child Adolesc Psychiatry 49:444–452. https://doi.org/10.1016/j.jaac.2010.01.018
McLaughlin KA, Breslau J, Green JG et al (2011) Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Soc Sci Med 73:1088–1096. https://doi.org/10.1016/j.socscimed.2011.06.011
Costello EJ, Compton SN, Keeler G, Angold A (2003) Relationships between poverty and psychopathology. JAMA 290:2023. https://doi.org/10.1001/jama.290.15.2023
Ravens-Sieberer U, Erhart M, Gosch A, Wille N (2008) Mental health of children and adolescents in 12 European countries—results from the European KIDSCREEN study. Clin Psychol Psychother 15:154–163. https://doi.org/10.1002/cpp.574
Ozer EJ, Fernald LCH, Manley JG, Gertler PJ (2009) Effects of a conditional cash transfer program on children’s behavior problems. Pediatrics 123:e630–e637. https://doi.org/10.1542/peds.2008-2882
Anselmi L, Menezes AMB, Hallal PC et al (2012) Socioeconomic changes and adolescent psychopathology in a Brazilian birth cohort study. J Adolesc Heal 51:S5–S10. https://doi.org/10.1016/j.jadohealth.2012.06.026
Barch DM, Belden AC, Tillman R et al (2018) Early childhood adverse experiences, inferior frontal gyrus connectivity, and the trajectory of externalizing psychopathology. J Am Acad Child Adolesc Psychiatry 57:183–190. https://doi.org/10.1016/j.jaac.2017.12.011
Curran PJ, Hussong AM (2003) The use of latent trajectory models in psychopathology research. J Abnorm Psychol 112:526–544. https://doi.org/10.1037/0021-843X.112.4.526
Masyn KE, Petras H, Liu W (2014) Growth curve models with categorical outcomes. Encyclopedia of criminology and criminal justice. Springer, New York, pp 2013–2025
Lee TK, Wickrama K, O’Neal CW (2018) Application of latent growth curve analysis with categorical responses in social behavioral research. Struct Equ Model Multidiscip J 25:294–306. https://doi.org/10.1080/10705511.2017.1375858
Reiss F, Meyrose A-K, Otto C et al (2019) Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort-study. PLoS ONE 14:e0213700. https://doi.org/10.1371/journal.pone.0213700
McLaughlin KA, Weissman D, Bitrán D (2019) Childhood adversity and neural development: a systematic review. Annu Rev Dev Psychol 1:277–312. https://doi.org/10.1146/annurev-devpsych-121318-084950
Cooper S, Lund C, Kakuma R (2012) The measurement of poverty in psychiatric epidemiology in LMICs: critical review and recommendations. Soc Psychiatry Psychiatr Epidemiol 47:1499–1516. https://doi.org/10.1007/s00127-011-0457-6
World Health Organization (2020) Adolescent mental health. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health. Accessed 22 Feb 2021
Kessler RC, Angermeyer M, Anthony JC et al (2007) Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6:168–176
United Nations (2016) Human development report: human development for everyone
Salum GA, Gadelha A, Pan PM et al (2015) High risk cohort study for psychiatric disorders in childhood: rationale, design, methods and preliminary results. Int J Methods Psychiatr Res 24:58–73. https://doi.org/10.1002/mpr.1459
Weissman MM, Wickramaratne P, Adams P et al (2000) Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry 57:675–682. https://doi.org/10.1001/pubs.Arch
Associação Brasileira de Empresas de Pesquisa (2018) Critério de Classificação Econômica Brasil. http://www.abep.org/criterio-brasil. Accessed 15 Apr 2020
Kamakura W, Mazzon JA (2016) Critérios de estratificação e comparação de classificadores socioeconômicos no Brasil. Rev Adm Empres 56:55–70. https://doi.org/10.1590/S0034-759020160106
Confortin SC, Ribeiro MRC, Barros AJD et al (2021) RPS Brazilian Birth Cohorts Consortium (Ribeirão Preto, Pelotas and São Luís): history, objectives and methods. Cad Saude Publica. https://doi.org/10.1590/0102-311x00093320
de Silva F, de Queiroz RC, dos Branco M et al (2020) Bolsa Família program and incomplete childhood vaccination in two Brazilian cohorts. Rev Saude Publica 54:98. https://doi.org/10.11606/s1518-8787.2020054001774
Goodman R, Ford T, Richards H et al (2000) The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 41:645–655
Fleitlich-Bilyk B, Goodman R (2004) Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry 43:727–734. https://doi.org/10.1097/01.chi.0000120021.14101.ca
Martel MM, Pan PM, Hoffmann MS et al (2017) A general psychopathology factor (P factor) in children: structural model analysis and external validation through familial risk and child global executive function. J Abnorm Psychol 126:137–148. https://doi.org/10.1037/abn0000205
Williamson DE, Birmaher B, Ryan ND et al (2003) The Stressful Life Events Schedule for children and adolescents: development and validation. Psychiatry Res 119:225–241. https://doi.org/10.1016/S0165-1781(03)00134-3
Sheehan D, Lecrubier Y, Sheehan K et al (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59:22–33
Seaman SR, White IR (2013) Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res 22:278–295. https://doi.org/10.1177/0962280210395740
StataCorp (2019) STATA Base reference manual release 16®. In: StataCorp LLC
Muthén L, Muthén B (2021) Mplus user’s guide, 8th edn. Muthen & Muthen, Los Angeles
Brown T (2015) Confirmatory Factor Analysis for Applied Research. Guilford Press, New York
MacKinnon DP, Lockwood CM, Williams J (2004) Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res 39:99–128. https://doi.org/10.1207/s15327906mbr3901_4
Rodriguez JDM, da Silva AAM, Bettiol H et al (2011) The impact of perinatal and socioeconomic factors on mental health problems of children from a poor Brazilian city: a longitudinal study. Soc Psychiatry Psychiatr Epidemiol 46:381–391. https://doi.org/10.1007/s00127-010-0202-6
La Maison C, Munhoz TN, Santos IS et al (2018) Prevalence and risk factors of psychiatric disorders in early adolescence: 2004 Pelotas (Brazil) birth cohort. Soc Psychiatry Psychiatr Epidemiol 53:685–697. https://doi.org/10.1007/s00127-018-1516-z
Wong YJ, Rew L, Slaikeu KD (2006) A Systematic Review of recent research on adolescent religiosity/spirituality and mental health. Issues Ment Health Nurs 27:161–183. https://doi.org/10.1080/01612840500436941
Devenish B, Hooley M, Mellor D (2017) The pathways between socioeconomic status and adolescent outcomes: a systematic review. Am J Community Psychol 59:219–238. https://doi.org/10.1002/ajcp.12115
Lund C, Breen A, Flisher AJ et al (2010) Poverty and common mental disorders in low- and middle-income countries: a systematic review. Soc Sci Med 71:517–528. https://doi.org/10.1016/j.socscimed.2010.04.027
March-Llanes J, Marqués-Feixa L, Mezquita L et al (2017) Stressful life events during adolescence and risk for externalizing and internalizing psychopathology: a meta-analysis. Eur Child Adolesc Psychiatry 26:1409–1422. https://doi.org/10.1007/s00787-017-0996-9
Amone-P’Olak K, Ormel J, Huisman M et al (2009) Life stressors as mediators of the relation between socioeconomic position and mental health problems in early adolescence: the TRAILS study. J Am Acad Child Adolesc Psychiatry 48:1031–1038. https://doi.org/10.1097/CHI.0b013e3181b39595
Leban L (2021) The effects of adverse childhood experiences and gender on developmental trajectories of internalizing and externalizing outcomes. Crime Delinq 67:631–661. https://doi.org/10.1177/0011128721989059
Leve LD, Kim HK, Pears KC (2005) Childhood temperament and family environment as predictors of internalizing and externalizing trajectories from ages 5 to 17. J Abnorm Child Psychol 33:505–520. https://doi.org/10.1007/s10802-005-6734-7
Lund C, Stansfeld S, De SM (2013) Social determinants of mental health. Global mental health. Oxford University Press, Oxford, pp 116–136
Ribeiro WS, de Mari J, Quintana MI et al (2013) The impact of epidemic violence on the prevalence of psychiatric disorders in Sao Paulo and Rio de Janeiro, Brazil. PLoS ONE 8:e63545. https://doi.org/10.1371/journal.pone.0063545
Blattman C, Jamison JC, Sheridan M (2017) Reducing crime and violence: experimental evidence from cognitive behavioral therapy in liberia. Am Econ Rev 107:1165–1206. https://doi.org/10.1257/aer.20150503
Funding
The research presented in this article was supported by the National Institute of Developmental Psychiatry for Children and Adolescents, a science and technology institute funded by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; National Council for Scientific and Technological Development; Grant numbers 573974/2008–0 and 465550/2014–2) and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP Grant number 2008/57896–8 and 2014/50917–0). CZ receives a Young Talent Research Scholarship by the Coordination for the Improvement of Higher Education Personnel (CAPES, Brazil, Grant number 88887.575201/2020–00).
Author information
Authors and Affiliations
Contributions
CZ and AG participated in the conception and analytic strategies of the current study. CZ and JS did the analysis. CZ drafted the manuscript. PMP, EM, RAB, GS, JM, LAR, JS, and AG, developed and conducted the BHRC. All authors made substantial contributions to the interpretation of the data and revision of the text. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
CZ, SEL, MCRA, MH, LF, MB, PMP, EM, RAB, GS, JS, and JM have no conflict of interest to declare. LAR has received grant or research support from, served as a consultant to, and served on the speakers’ bureau of Aché, Bial, Medice, Novartis/Sandoz, Pfizer/Upjohn, and Shire/Takeda in the last three years. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by Dr LAR have received unrestricted educational and research support from the following pharmaceutical companies in the last three years: Novartis/Sandoz and Shire/Takeda. Dr LAR has received authorship royalties from Oxford Press and ArtMed. AG has been a consultant and/or advisor to or has received honoraria from Aché, Daiichi-Sankyo, Torrent, Cristalia, and Janssen.
Ethics approval
All procedures were approved by the Ethics Committee of the Federal University of São Paulo and Hospital de Clínicas de Porto Alegre.
Consent to participate
Child assent and parental informed consent were obtained from all the research subjects.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ziebold, C., Evans-Lacko, S., Andrade, M.C.R. et al. Childhood poverty and mental health disorders in early adulthood: evidence from a Brazilian cohort study. Eur Child Adolesc Psychiatry 32, 903–914 (2023). https://doi.org/10.1007/s00787-021-01923-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01923-2