Abstract
This study was the first to examine the relationship between neurophysiological abnormalities and symptoms of sluggish cognitive tempo (SCT) in children. Thirty children aged 6–12 years were recruited. Their heart rate variability (HRV) was measured under resting and warning signal conditions. At rest, the children’s SCT symptoms were found to be positively associated with their HRV (indicated by the standard deviation of the Poincaré plot along the line of identity in normalized units, SD2 nu). SCT symptoms were also positively associated with a change in SD2 nu between the resting and warning signal conditions. When controlling for symptoms of attention deficit hyperactivity disorder, the children’s SCT symptoms were significantly predicted by their resting SD2 nu and by changes in SD2 nu and the percentage of successive RR intervals that differ by more than 50 ms (pNN50) between the resting and warning signal conditions. These findings suggest that the readiness and regulation of the autonomic nervous system may contribute to symptoms of SCT. Specifically, disturbances in the internal neurophysiological system may explain the difficulties experienced by children when exposed to environmental stimulation. These initial data support the hypothesis that SCT results from deficiencies in arousal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“Sluggish cognitive tempo” (SCT) describes a group of symptoms characterized by inconsistent alertness (e.g., daydreaming) and delays in thought and behavior (e.g., drowsiness and delayed responsiveness) [4, 5]. These symptoms, which manifest in both children and adults, are often associated with real-life impairments such as the internalization of behavioral difficulties (e.g., anxiety and depression), social problems, and academic learning difficulties [4, 46]. Although some researchers have suggested that SCT represents a purer form of the inattentive subtype of attention deficit/hyperactivity disorder (ADHD) [30], more recent findings indicate that SCT is distinct from any form of ADHD [4, 5].
Although increasing evidence has been found that SCT is independent of other childhood psychopathologies, the nature of this condition remains somewhat poorly understood [4]. This lack of understanding may have multiple consequences. First, clinicians may find it difficult to accurately assess symptoms of SCT in their patients because the underlying factors are not well understood. Second, this lack of accurate assessment may render the clinician unable to suggest appropriate treatment for children who exhibit symptoms of SCT. Therefore, researchers must evaluate the factors contributing to SCT and determine how these factors distinguish SCT from other mental disorders, especially those with similar clinical manifestations, such as ADHD.
Conceptualization of SCT within the research domain criteria (RDoC) framework
Previous studies have attempted to conceptualize SCT using behavioral symptoms, and have made considerable progress in this area [5]. However, the conceptualization of SCT or any other mental disorder as a group of purely behavioral symptoms (e.g., in the Diagnostic and Statistical Manual of Mental Disorders and International Statistical Classification of Diseases) has some drawbacks. For example, using these systems to delineate the symptoms or presentations of disorders may not fully capture the underlying pathophysiological mechanisms [22].
The RDoC project provides a pathophysiological framework that can inform future classifications of mental disorders and offer insight into the underlying functional dimensions associated with normal and abnormal behavior [33]. Currently, the RDoC framework comprises five domains: negative valence systems, positive valence systems, cognitive systems, systems for social processes, and arousal/regulatory systems [33]. Researchers have suggested that the latter domain, arousal/regulatory systems, relates to the symptoms of SCT [4, 8]. The characteristic SCT symptoms of inattention, anxiety, and withdrawn behavior have been attributed to both hypo- and hyper-arousal [8]. However, no evidence has been found to support this potential association.
Dysregulated brain arousal and SCT symptoms
Barkley [4] suggested that SCT, which is associated with the symptoms of sleepiness and low energy, may be a form of arousal disorder. Notably, SCT symptoms have been shown to correlate with sustained deficits in attention/alertness during neuropsychological tests [50, 55], and a close relationship has been identified between arousal and alertness [35].
The warning signal effect can be enhanced or suppressed in response to an increase or decrease in norepinephrine (NE), which is associated with the alerting system [35]. Consequently, this warning signal effect can be blocked by drugs that reduce the release of NE. Alertness in response to a warning signal is accompanied by activity in the locus coeruleus (LC), which has been identified as the source of NE [1]. The thalamus has also been identified as a component of arousal regulation [3, 29, 42].
The influence of NE and dopamine (DA) on various functions of the prefrontal cortex (PFC), including attention and executive functioning (EF), can be represented as an inverted U-shaped curve [10, 32]. The shape of this relational curve indicates that the release of either insufficient or excess NE and DA can impair the functions of the PFC [10, 32, 56]. Therefore, NE and DA may act as chemical switches that turn on the PFC in a state of alertness and turn it off in states of drowsiness and stress [10]. In other words, the previously observed deficiencies in attention and executive functioning in individuals exhibiting SCT symptoms [4, 6, 50, 55] may be attributable to states of both hypo- and hyper-arousal in the brain, which can be reflected in autonomic nervous system (ANS) activity.
Autonomic functioning and SCT symptoms
The LC and ANS are linked by a reciprocal pathway [39, 53]. The ability of LC neurons to receive and process cardiovascular-related information and alter LC activity accordingly may be mediated by the output of the rostral ventrolateral medulla, which regulates cardiovascular function [39, 53]. Previous studies have also shown that activity in the LC can induce changes in cardiovascular responses. Wang et al. [54] found that subjecting LC neurons to photo-stimulation increased the neurotransmission of inhibitory signals to parasympathetic cardiac vagal neurons in the mouse brainstem, thus decreasing the parasympathetic affluent to the heart. Regarding autonomic function control, the LC has been shown to project directly to the spinal cord and the autonomic nuclei, including the dorsal motor nucleus of the vagus, nucleus ambiguus, and rostro-ventrolateral medulla [39]. This evidence suggests that the pathway between the LC and ANS is bidirectional and that changes in brain arousal may affect ANS activity.
The ANS, which comprises the sympathetic nervous system (SNS; NE is the primary neurotransmitter) and parasympathetic nervous system (PNS; acetylcholine is the primary neurotransmitter) [23], has also been identified as a crucial modulator of physiological arousal during tasks requiring attention and EF [27, 43, 48, 57]. The SNS and PNS work interactively to innervate different human organs. Specifically, the SNS controls resource mobilization, while the PNS controls restorative/vegetative function [12]. During sustained attention tasks, parasympathetic vagal tone is decreased via the vagal nerve, which promotes the influence of the SNS within the ANS and enables immediate mobilization during real-life tasks [43].
The literature concerning the neurovisceral integration model [47, 48] has described the central autonomic network (CAN) as an important component of an internal regulation system in the ANS through which the brain controls the visceral-motor, neuroendocrine, and behavioral responses crucial to goal-directed behavior [47]. Structurally, the CAN includes the following central nervous system (CNS) components: the anterior cingulate, insular, orbitofrontal and ventromedial prefrontal cortices; the central nucleus of the amygdala; the paraventricular and related nuclei of the hypothalamus; the nucleus of the solitary tract; the nucleus ambiguous; the ventrolateral medulla; the ventromedial medulla; and the medullary tegmental field [47]. All these components are connected reciprocally, which facilitates the bidirectional transfer of information between the lower and higher levels of the CNS [47]. Consequently, the output of the CAN is related directly to heart rate variability (HRV), because this output is mediated through preganglionic sympathetic and parasympathetic neurons linked to the heart via the stellate ganglia and vagus nerve, respectively [47].
According to Thayer et al. [47], the effects of the PFC on subcortical structures (e.g., the amygdala and thalamus) may enable an individual to control their psychophysiological resources during attention and executive function processes and organize their behavior efficiently to meet environmental challenges. Lane et al. [26] reported that the level of PNS functioning, indicated by high-frequency (HF) band measures of HRV, was positively correlated with the level of blood flow in various cortical regions (e.g., the medial prefrontal cortex, thalamus, caudate nucleus, and left mid-insula) in participants exposed to film clips and encouraged to recall personal experiences eliciting different emotions (e.g., happiness, sadness, and disgust). Examining a cohort of 53 adults aged 18–34, Hansen et al. [19] found that the resting ANS function, as reflected by HRV, was associated with cognitive performance during various attention and executive functioning tasks (e.g., the n-back working memory task). In a study of 99 children and adolescents aged 8–17 years who were exposed to a condition intended to arouse frustration, a higher level of parasympathetic activity was associated with better attention performance [14]. Additionally, two recent meta-analyses evaluated the relationship between ANS function and executive function, using HRV as an index of the former variable [21, 57]. Notably, both meta-analyses identified significant positive associations between HRV and executive functioning [21, 57]. These findings suggest a link between cognitive functioning (e.g., executive functioning and attention) and ANS functioning as reflected by HRV. However, although previous findings suggest that individuals with (vs. without) SCT symptoms face greater difficulties with EF and attention, HRV has not previously been evaluated in this population. Therefore, the potential associations of these difficulties with ANS functioning remain unclear.
Notably, recent studies have investigated ANS functioning in children with attention deficits, such as ADHD [16, 24, 37]. Koenig et al. [24] reported an association between the severity of ADHD symptoms and the level of ANS functioning (as reflected by HRV). In another study, the levels of vagally mediated HRV measures such as HF during cognitive and emotional tasks were lower in the ADHD group relative to the control group [37]. The low–high frequency ratio (LF/HF) was also higher in children with ADHD than in their control counterparts under conditions of resting and sustained attention [16]. Therefore, the effects of ADHD symptoms on the ANS are likely to confound the results of HRV measures at baseline and under experimental conditions. As a result, individuals who have been diagnosed as having ADHD or elevated symptoms of ADHD were included as exclusion criteria. Exclusion of participants with ADHD would allow investigation of the HRV and SCT symptoms be free from the known confound. The control set on the ADHD symptoms would inevitably impede generalization of the results, which will be highlighted in the discussion of this paper.
Conceptual framework of study
This study conceptualized SCT as a condition that involves abnormalities in the level and regulation of brain arousal that lead to a deficit in attention (e.g., alertness). Brain arousal is defined as a brain state related to the level of NE in the cortical area of the PFC, which is regulated by the LC. Readiness and regulation are considered two components of ANS functioning. The former is defined as an individual’s physiological readiness to prepare for a real-life challenge. The use of the resting HRV to measure this component is well-established [47]. The latter component is defined as an individual’s ability to regulate their physiological activity during real-life changes and challenges. In the present study, ANS regulation was measured as the change in HRV from a resting to a warning signal condition.
This study postulated a link between the LC and ANS. Accordingly, abnormalities in the LC and ANS were expected to lead to abnormalities in brain arousal (e.g., under-arousal due to a lower NE level) in individuals with SCT symptoms. These chained actions between the LC and ANS were hypothesized to affect executive functioning and attention, thus leading to SCT symptoms. Within this framework, the severity of SCT symptoms was expected to correlate with ANS readiness and regulation, as measured by HRV. An understanding of this association is important for multiple reasons. First, the results obtained using a dimensional approach provide insights into how variations in the RdoC domains may affect the severity of SCT symptoms. Second, a RdoC-based evaluation of SCT symptoms combines behavioral and neurophysiological data (e.g., HRV) to differentiate this unique condition from other psychopathologies, such as ADHD and affective disorders [8]. Third, psychopathologies (including SCT) rarely have a single etiology. Therefore, studying SCT within the RdoC framework helps us to understand how different processes (e.g., RdoC constructs) might contribute interactively to the complex behavioral symptoms of SCT [8].
Aim and hypotheses
This study aimed to examine the relationships between ANS functioning and SCT symptoms in school-aged children. Specifically, it sought to characterize the possible link between arousal/regulation and SCT symptoms by exploring more deeply the specific parameters of HRV measures that contribute to SCT symptoms. The findings had the potential to confirm or exclude the involvement of the SNS, the PNS, or both systems in the pathology of SCT. Reduced LC activation was expected to relieve the inhibition of PNS activity. In contrast, elevated LC activation was expected to further inhibit PNS activity and consequently increase SNS activity and thus arousal level [54]. Therefore, we hypothesized that:
-
1.
Resting HRV measures are significantly associated with SCT symptoms.
-
2.
Changes in HRV measures from a resting to a warning signal condition are associated significantly with SCT symptoms.
-
3.
Both resting HRV measures and changes in these measures significantly predict the severity of SCT symptoms.
Methods
Participants
The participants involved in this study were required to meet the following inclusion criteria: (a) aged 6–12 years and (b) a full scale IQ score ≥ 80. Potential participants who met the following criteria were excluded: (a) any psychiatric diagnosis, including ADHD, oppositional defiant disorder, conduct disorder, or dyslexia; (b) a T-score > 85 in the Chinese version of the Strengths and Weaknesses of ADHD Symptoms and Normal Behavior scale (SWAN; [44]; (c) a T-score > 70 in any subscale of the Child Behavior Checklist (CBCL) (Chinese version) [2]; (d) any uncorrected visual or auditory problems; and (e) a history of diabetes or cardiac and/or respiratory problems. Children with an ADHD diagnosis or elevated symptoms of ADHD were excluded because these symptoms would have confounded the neurophysiological measures used in the study (i.e., HRV measures). Those with other psychiatric disorders (e.g., childhood anxiety or oppositional defiant disorder/conduct disorder) were excluded because these disorders have also been found to be associated with different patterns of HRV [38, 40]. In other words, these conditions could have confounded the relationship between the HRV variables and SCT symptoms.
Thirty primary school students aged 6–12 [mean age = 104.2 months, standard deviation (SD) = 20.1; 56.7% female; mean IQ score = 102.92, SD = 9.95] were recruited via posters sent to primary schools and parent chat groups. Most of the participants were recruited from primary schools (93.3%), and the remainder (6.7%) were recruited via the parent chat group channel. Parents who expressed an interest in joining the study were instructed to contact the researcher. Each parent received information on the nature and purpose of the study and a written consent form. The consent forms were signed prior to the collection of data.
Procedure and experimental setup
Before the data collection, the children’s demographic information (i.e., name, date of birth, and gender) and medical histories were obtained from their parents. Each participant was then asked to attend two 1.5-h testing sessions conducted in a laboratory free from visual or auditory distractions. Additional requirements were set to safeguard the quality of the HRV measures, including (a) an illumination level of 10 lux, (b) a room temperature of 23–25 °C, and (c) a background noise level of 40–45 dB. During the first session, each participant completed an IQ test and neuropsychological tests. During the second session, each participant completed the HRV measures. The participants were reminded to avoid the following before the second session: (a) the intake of caffeinated drinks; (b) the intake of food for 1.5 h before testing; (c) participating in vigorous activities for 24 h before testing; and (d) the use of any treatment or medication that could affect ANS activity. Breaks were offered before or during the tests.
Measurement instruments
Each participant underwent four neuropsychological tests and neurophysiological measures of HRV.
Neuropsychological tests
-
Wechsler Intelligence Scale for Children, Fourth Edition (Hong Kong) short-form (WISC-IV [51]): This is a short version of the WISC-IV, a formal intelligence scale. It comprises four subscales: similarities, matrix reasoning, coding, and digit span. The raw scores for these four subscales are combined to give a total raw score and subsequently transformed into a full-scale IQ score.
-
Child Behavior Checklist for Ages 6–18 (CBCL/6–18) [2]: The CBCL/6–18 is a parent rating scale measuring the emotional and behavioral problems of children aged 6–18. The respondent rates every item using a 3-point scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true). The CBCL comprises eight scales: anxiety/depression, somatic complaints, social problems, thought problems, attention problems, rule-breaking behavior, and aggressive behavior. The total raw score for each scale is then transformed into a standardized subscale score. The CBCL has been reported to yield good to excellent test–retest reliability (intra-class correlation coefficient: 0.66–0.87) and good discriminant validity [28].
-
SWAN—Chinese version: SWAN is a parent and teacher rating scale used to screen for ADHD symptoms [44] The Chinese-translated version used in this study has been validated for use with children in Hong Kong (Education Bureau of HKSAR, 2010). The scale comprises 18 items that measure a child’s control of their attention, impulses, and activity. The items are divided into two subscales of nine items each, which address inattention and hyperactivity/impulsivity, respectively. The total and subscale scores are generated by summing the raw item scores, which can be expressed as T-scores. A higher score indicates fewer ADHD symptoms. In this study, only the total SWAN scores were used. All of the total and subscale scores for both the parent and teacher versions of SWAN have been found to yield a very good internal consistency (alpha > 0.9) (Education Bureau of HKSAR 2010) and a good discriminant validity (AUC > 0.8) (Education Bureau of HKSAR 2010).
-
SCT Scale [34]: This 14-item parent and teacher scale is used to measure SCT symptoms in children. Each item is rated on a 7-point scale (range: 0 = not at all to 6 = very much). As with those previous researches using this measure [9, 20], 10 items were selected for use instead of the full scale in the present study. These 10 items were found to yield consistent loadings on the SCT factor but not the ADHD inattention factor [7]. This unified 10-item construct was consistent with the participants’ characteristics and the hypotheses of the study. The internal consistency of the 14-item SCT is high when measured by both parent (alpha > 0.8) and teacher ratings (alpha > 0.9) [34]. Additionally, the 10-item version yielded a high level of internal consistency in the present study (Cronbach’s alpha = 0.898).
Neurophysiological tests
-
ANS measures: HRV measures ANS activity [45]. Here, HRV was used to evaluate SNS and PNS activity under each experimental condition (resting and warning signal conditions; refer to the next section for details). The sampling rate of 5 kHz was set using an H2 heart-rate monitor (Polar Electro, Finland).
Experimental paradigm
Warning signal paradigm
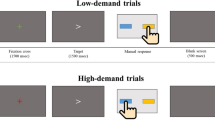
Figure 1 depicts the experimental paradigm used in this study. This paradigm was adapted from Gomez et al. [17] and Lai [25], who modified the sensory challenging protocol proposed by Miller et al. [31]. The paradigm described by Gomez et al. [17] and that of the present study differed mainly in the former’s inclusion of a recovery condition. The recovery condition was omitted here because the study focused solely on the change in HRV from the resting condition to the warning signal condition. In the experimental protocol, the HRV was measured continuously across the two conditions: resting and warning signal. During the resting condition, each participant was shown a silent animated video for 200 s. Subsequently, the monitor screen turned blank, and the participant was exposed to a warning signal condition block comprising 10 trials of a 4-kHz pure tone at 85 dB. The duration of each trial was 3 s. A pseudorandomized interval of 10–15 s was set to avoid adaptation to the stimulus.
HRV signal processing
HRV was defined as the variation in the time intervals between adjacent heartbeats [41]. All of the raw HRV data were initially converted into tachograms using aHRV software (Nevrokard, Slovenia). The tachograms were visually scanned to identify ectopic beats, movement artifacts, and abnormal noise signals. Subsequently, the data were epoched into specific time events according to the experimental paradigm. Values corresponding to 20% below or above the mean of the preceding 25 beats were treated as artifacts during short-term recording and edited by interpolation. Data with a correction rate 3% higher than the total normalized HRV data samples were discarded, as recommended by the [45].
Previous studies have used three major types of HRV measurement, following the recommendations of the [45]: time domain, frequency domain, and non-linear measurements. Time domain indices quantify the variability in the measured time interval between successive heartbeats [41] and can be derived from direct measurements of the NN intervals or the instantaneous heart rate and from the differences between NN intervals. The most common measures are the root mean square of successive RR interval differences (RMSSD) and the percentage of successive RR intervals that differ by more than 50 ms (pNN50). Both measures are closely correlated with PNS activity [41].
Frequency domain measurements estimate the distribution of absolute or relative power into four frequency bands: ultra low frequency (ULF < 0.003 Hz), very low frequency (VLF 0.0033–0.04 Hz), low frequency (LF 0.04–0.15 Hz), and high frequency (HF 0.15–0.4 Hz). In this study, autoregressive modeling was used to stratify HRV into these four frequency bands. Absolute power is defined as ms squared divided by cycles per second (ms2/Hz). Relative power is calculated as the percentage of total HRV power or in normalized units (nu), wherein the absolute power for a specific frequency band is divided by the summed absolute power of the LF and HF bands [41]. In this study, the frequency domain measurements were expressed in terms of relative power (nu), as this enabled the direct comparison of frequency domain measurements between participants. Notably, HF has been found to reflect PNS activity, whereas LF may reflect both SNS and PNS activity [45].
Finally, non-linear measurements indicate the unpredictability of a time series, which arises from the complexity of the sympatho-vagal mechanism that regulates HRV [41]. The standard deviation of the Poincaré plot perpendicular to the line of identity (SD1) and along the line of identity (SD2) are commonly used in this context [41]. A Poincaré plot can be created by plotting every RR interval against the prior interval [41], and can be analyzed by fitting an ellipse to the plotted dots. SD1 represents the width of this ellipse, and is thought to reflect short-term variability in HRV, a measure of PNS activity [49]. SD2 represents the length of the ellipse, and is thought to reflect long-term variability in HRV [11, 18, 41]. In several studies, a decrease in SD2 has been associated with an increase in sympathetic activity [13, 15, 36, 49]. However, changes in SD2 may also be modulated partly by changes in parasympathetic activity [36]. Both SD1 and SD2 can be expressed in nu.
Data analysis
Partial correlation analysis was used to examine the correlations between the resting HRV measures (RMSSD, pNN50, SD1 nu, SD2 nu, LF nu, and HF nu) and SCT scores (hypothesis 1). This method was also used to measure the correlations between changes in these HRV measures from the resting to warning signal conditions and SCT scores (hypothesis 2) when controlling for the ADHD symptoms included in SWAN. Strong correlations were observed between the HRV variables (r = 0.64–0.94). Therefore, to minimize multicollinearity, stepwise regression was conducted to examine the contributions of the different HRV variables to the severity of SCT symptoms. All of the analyses were conducted using SPSS 23.0 (IBM, USA), and the significance level was set at 0.05.
Results
Associations of resting HRV measures with SCT scores
Partial correlation analysis was used to test the associations of the resting ANS measures with the participants’ SCT scores. The means and standard deviations of the resting HRV measures and rating scale scores are shown in Table 1. When controlling for SWAN ADHD scores, SCT scores exhibited a significant positive relationship with SD2 nu (p = 0.022) (Table 2). No other significant correlations between the participants’ SCT scores and other resting HRV measures were observed (Table 2).
Associations of changes in HRV from resting to warning signal conditions with SCT scores
Partial correlation analysis was also used to test the associations between the magnitude of changes in the HRV measures from the resting to warning signal conditions and the participants’ SCT scores. The means and standard deviations of the changes in the HRV measures and rating scale scores are shown in the Table 3. When controlling for SWAN ADHD score, a change in SD2 nu was significantly associated with the SCT score (p = 0.031) (Table 4). Moreover, a change in pNN50 exhibited a marginally significant association with the SCT score (p = 0.053). No significant correlations were observed between changes in the other HRV measures and the participants’ SCT scores (Table 4).
Use of resting HRV measures to predict SCT symptoms
The intercorrelations between resting HRV measures and behavioural rating scale scores are shown in Table 5. Stepwise regression was conducted to determine the ability of HRV measures to predict the SCT score after entering the SWAN ADHD score into the model to control for ADHD symptoms (step 1). Subsequently, the HRV measures (RMSSD, pNN50, SD1 nu, SD2 nu, LF nu, and HF nu) were entered using the stepwise method (entry probability = 0.05; removal probability = 0.10) (step 2) (Table 6). The SWAN ADHD score did not contribute significantly to the regression model [F (1, 28) = 2.601, p > 0.05] (Table 6). The stepwise analysis identified only the resting SD2 nu as a significant predictor in the regression model. This measure explained 16.5% of the variance in SCT score [F (2, 27) = 4.497, p < 0.05].
Use of changes in HRV measures to predict SCT symptoms
The intercorrelations between changes in HRV measures and behavioural rating scale scores are shown in Table 7. Stepwise regression was conducted again to determine the extent to which changes in the HRV measures predicted the participants’ SCT scores. Again, the SWAN ADHD score was entered into the model first (step 1), followed by changes in RMSSD, pNN50, SD1 nu, SD2 nu, LF nu, and HF nu in a stepwise manner (step 2) (Table 8). The SWAN ADHD score alone was not a significant predictor of the SCT score (Table 8). However, after controlling for this parameter, three significant predictors of the SCT score were identified. First, changes in SD2 nu and changes in pNN50 were identified as significant independent predictors in the regression models (steps 2 and 3). Changes in SD2 nu alone explained 14.8% of the variance in the SCT scores [F (2, 27) = 4.098, p < 0.05]. The addition of changes in pNN50 to the model accounted for an additional 13.8% of the variance in SCT score [F (3, 26) = 5.117, p < 0.01]. Changes in SD2 nu were, therefore, a stronger predictor of SCT scores than changes in pNN50.
Discussion
The current study was the first to examine the relationships between SCT symptoms and the arousal/regulatory system in children. The results support our hypothesis that different HRV parameters across resting and warning signal conditions correlate with the symptoms of SCT in children. First, ANS readiness, as measured by resting SD2 nu, was significantly associated with SCT symptoms. Second, ANS regulation, as measured by changes in SD2 nu from the resting to the warning signal condition, correlated significantly with SCT symptoms. Third, ANS readiness and ANS regulation, as measured by SD2 nu and changes in SD2 nu and pNN50, respectively, were identified as significant predictors of SCT symptoms in children after controlling for ADHD symptoms.
ANS readiness and SCT symptoms
As previously noted, resting SD2 nu correlated positively with the symptoms of SCT. SD2 nu is thought to reflect sympathetic activity in the ANS [13, 15, 36, 49], such that a higher SD2 nu was associated with lower sympathetic activity. Accordingly, the participants with more pronounced SCT symptoms appeared to exhibit lower sympathetic activity in the resting condition. Pronounced SCT symptoms, including apathy, slowness in completing tasks, and lack of motivation, are probably associated with under-arousal in the brain [4, 8]. Notably, the significant correlation identified between SD2 nu and SCT symptoms was not confounded by symptoms of ADHD, as the latter was statistically controlled for in the analysis.
As noted above, the LC plays a major role in modulating arousal [1] and cardiovascular responses [53]. An increase in LC activity inhibits parasympathetic cardiac vagal neurons in the brainstem, thus reducing parasympathetic activity to the heart [54]. Conversely, a decrease in LC activity reduces the inhibition of parasympathetic cardiac vagal neurons in the brainstem and subsequently decreases sympathetic activity to the heart. In this study, more severe symptoms were associated with lower levels of sympathetic activity, as indicated by the resting SD2 nu values (the strongest predictor). Under-arousal may be a deficit associated with SCT symptoms [4, 8]. The preliminary results of a drug trial indicated significant improvements in SCT symptoms in patients treated with atomoxetine, an NE reuptake inhibitor [52]. The latter trial further supported an association between arousal level and the severity of SCT symptoms. The findings of the current study suggest that children with more severe SCT symptoms may experience an ANS preparatory state characterized by lower levels of sympathetic activity than those observed in their counterparts with less severe SCT symptoms. ANS readiness may be a good indicator of an individual’s ability to adapt to new challenges [47]. Consequently, a lower level of ANS readiness may explain the increased difficulties experienced by children with SCT symptoms.
ANS regulation and SCT symptoms
This study also revealed a link between SCT symptoms and heightened arousal in the participants. Changes in the magnitude of SD2 nu from the resting to the warning signal condition were positively associated with SCT symptoms, and both these changes and changes in pNN50 were identified as significant predictors of SCT symptoms after controlling for ADHD symptoms. The participants may have experienced a simultaneous increase in sympathetic activity and decrease in parasympathetic activity when exposed to the warning signal condition after the resting condition. Previous studies have attributed such an increase in sympathetic activity and such a decrease in parasympathetic activity to an increase in LC activity and consequently the frequency of inhibitory postsynaptic currents in the cardiac vagal neurons [54]. The participants with more severe SCT symptoms were more likely to exhibit greater pNN50 changes and SD2 nu changes upon exposure to the warning signal, which may reflect a higher level of arousal in the brain. However, the variables in this study were based on the magnitude of changes from the resting to the warning signal condition. Therefore, the participants with more severe SCT symptoms may have experienced lower levels of arousal in the resting condition or excessive arousal in the warning signal condition. Future studies should explore the modulating effect of baseline arousal on the responses of SCT participants.
Some researchers have speculated that SCT symptoms, particularly those related to withdrawal, may be attributable to a state of heightened arousal [8]. The results of the current study appear to support the hypothesized association between increased arousal and an exacerbation of SCT symptoms such as apathy. The withdrawn behaviors exhibited by individuals with SCT may be caused by an increased level of arousal in response to environmental and especially stress-related events. In other words, SCT symptoms do not seem to be correlated solely with under-arousal. Our findings also indicate that SCT symptoms are associated with heightened arousal in response to environmental stimuli or events.
The observed deficiencies in ANS readiness and regulation in individuals with SCT may explain the sustained attention deficiencies reported previously [50, 55]. These deficiencies may be associated with two neurophysiological deficits. First, as demonstrated in this study, individuals with exacerbated SCT symptoms may exhibit a lower level of appropriate ANS readiness associated with under-arousal. This presents challenges when preparing to meet the demands of real-life tasks. Second, people with exacerbated SCT symptoms find it more difficult to maintain the optimal change to the ANS needed to meet the requirements of the internal and external environment. Therefore, as shown in this study, the observed deficiencies in sustained attention may be attributable to abnormalities in both ANS readiness and ANS regulation.
This study had some limitations worth noting. First, the data were correlational. Future studies should directly compare the HRV values of children exhibiting high levels of SCT symptoms with those of children exhibiting typical development under resting and warning signal conditions. Second, the study did not include children with ADHD. It was, therefore, impossible to examine the associations of HRV measures with ADHD symptoms and compare these relationships with the neurophysiological factors associated with SCT in the same population. Although both ADHD and SCT symptoms may be associated with HRV measures, the patterns and/or strength of these associations may differ. More information on these associations may help to clarify the physiological differences between SCT and ADHD. Therefore, future studies should also recruit children with ADHD to compare their neurophysiological deficits with those of children with SCT symptoms.
In conclusion, this study identified significant associations between SCT symptoms and ANS readiness/regulation, which may be attributable to abnormalities in the subjects’ arousal levels at rest, as well as to their regulation of arousal in response to environmental stimuli. These findings suggest that SCT may be related to abnormalities in neurophysiological functioning. Future studies should address these factors when investigating the etiology of SCT to provide a better understanding of the condition and improve treatment options accordingly.
References
Aston-Jones G, Cohen JD (2005) An integrative theory of locus coeruleus-norepinephrine function: adaptive gain and optimal performance. Annu Rev Neurosci 28:403–450
Achenbach T (2001) Child Behavior Checklist (CBCL), Achenbach System of Empirically Based Assessment. ASEBA, Burlington
Baker JL, Ryou J, Wei XF, Butson CR, Schiff ND, Purpura KP (2016) Robust modulation of arousal regulation, performance, and frontostriatal activity through central thalamic deep brain stimulation in healthy nonhuman primates. J Neurophysiol 116:2383–2404. https://doi.org/10.1152/jn.01129.2015
Barkley RA (2013) Sluggish cognitive tempo (concentration deficit disorder?): current status, future directions, and a plea to change the name. J Abnorm Child Psychol 42:117–125
Becker SP, Garner AA, Byars KC (2016) Sluggish cognitive tempo in children referred to a pediatric sleep disorders center: examining possible overlap with sleep problems and associations with impairment. J Psychiatr Res 77:116–124. https://doi.org/10.1016/j.jpsychires.2016.03.005
Becker SP, Langberg JM (2014) Attention deficit hyperactivity disorder and sluggish cognitive tempo dimensions in relation to executive functioning in adolescents with ADHD. Child Psychiatry Hum Dev 45:1–11. https://doi.org/10.1007/s10578-013-0372-z
Becker SP, Leopold DR, Leonard Burns G, Jarret MA, Langberg JM, Marshall S, Willcutt EG et al (2016) The internal, external, and diagnostic validity of sluggish cognitive tempo: a meta-analysis and critical review. J Am Acad Child Adolsc Psychiatry 55:163–178. https://doi.org/10.1016/j.jaac.2015.12.006
Becker SP, Willcutt EG (2018) Advancing the study of sluggish cognitive tempo via DSM, RDoC, and hierarchical models of psychopathology. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-018-1136-x
Becker SP, Garner AA, Tamm L, Antonini TN, Epstein JN (2019) Honing in on the social difficulties associated with sluggish cognitive tempo in children: withdrawal, peer ignoring, and low engagement. J Clin Child Adolesc Psychol 48:228–237. https://doi.org/10.1080/15374416.2017.1286595
Brennan AR, Arnsten AFT (2008) Neuronal mechanisms underlying attention deficit hyperactivity disorder: the influence of arousal on prefrontal cortical function. Ann N Y Acad Sci 1129:236–245. https://doi.org/10.1196/annals.1417.007
Brennan M, Palaniswami M, Kamen P (2001) Do existing measures of Poincaré plot geometry reflect nonlinear features of heart rate variability? IEEE Trans Biomed Eng 48:1342–1347
Cannon WB (1915) Bodily changes in pain, hunger, fear and rage: an account of recent researches into the function of emotional excitement. D. Appleton and Company, New York
Castaldo R, Montesinos L, Melillo P, James C, Pecchia L (2019) Ultra-short term HRV features as surrogates of short term HRV: a case study on mental stress detection in real life. BMC Med Inform Decis Mak 19:12. https://doi.org/10.1186/s12911-019-0742-y
Chapman HA, Woltering S, Lamm C, Lewis MD (2010) Hearts and minds: coordination of neurocognitive and cardiovascular regulation in children and adolescents. Biol Psychol 84(2):296–303. https://doi.org/10.1016/j.biopsycho.2010.03.001
De Vito G, Galloway SDR, Nimmo MA, Maas P, McMurray JJV (2002) Effects of central sympathetic inhibition on heart rate variability during steady-state exercise in healthy humans. Clin Physiol Funct Imaging 22:32–38
Griffiths KR, Quintana DS, Hermens DF, Sponner C, Tsang TW, Clarke S, Kohn MR (2017) Sustained attention and heart rate variability in children and adolescents with ADHD. Biol Psychol 124:11–20. https://doi.org/10.1016/j.biopsycho.2017.01.004
Gomez IN, Lai CYY, Chan CCH, Tsang HWH (2018) The role of ethnicity and environment in the regulation of response to sensory stimulus in children: protocol and pilot findings of a neurophysiological study. JMIR Res Protoc 7:e7. https://doi.org/10.2196/resprot.8157
Guzik P, Piskorski J, Krauze T, Schneider R, Wesseling KH, Wykretowicz A, Wysocki H (2007) Correlations between the Poincaré Plot and conventional heart rate variability parameters assessed during paced breathing. J Physiol Sci 57:63–71
Hansen AL, Johnsen BH, Thayer JF (2003) Vagal influence on working memory and attention. Int J Psychophysiol 48:263–274
Holdaway AS, Becker SP (2018) Sluggish cognitive tempo and student-teacher relationship quality: short-term longitudinal and concurrent associations. Sch Psychol Q 33:537–546. https://doi.org/10.1037/spq0000245
Holzman JB, Bridgett DJ (2017) Heart rate variability indices as bio-markers of top down self-regulatory mechanisms: a meta-analytic review. Neurosci Biobehav Rev 74:233–255. https://doi.org/10.1016/j.neubiorev.2016.12.032
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Wang P et al (2010) Research domain criteria (RDOC): toward a new classification framework for research on mental disorders. Am J Psychiatry 167:748–751. https://doi.org/10.1176/appi.ajp.2010.09091379
Janig W (2008) Integrative action of the autonomic nervous system: neurobiology of homeostasis. Cambridge University Press, Cambridge
Koenig J, Rash JA, Kemp AH, Buchhorn R, Thayer JF, Kaess M (2017) Resting state vagal tone in attention deficit (hyperactivity) disorder: a meta-analysis. World J Biol Psychiatry 18(4):256–267
Lai CYY (2013) A study of behavioural and autonomic responses in autistic children with sensory processing difficulty (doctoral dissertation). http://theses.lib.polyu.edu.hk/handle/200/7242
Lane RD, McRae K, Reiman EM, Chen K, Ahern GL, Thayer JF (2009) Neural correlates of heart rate variability during emotion. Neuroimage 44:213–222. https://doi.org/10.1016/j.neuroimage.2008.07.056
Lesley JC, Dywan J, Tays WJ, Elmers JL, Witherspoon R, Segalowitz SJ (2014) Factors influencing the role of cardiac autonomic regulation in the service of cognitive control. Biol Psychol 102:88–97. https://doi.org/10.1016/j.biopsycho.2014.07.015
Leung PWL, Kwong SL, Tang CP, Ho TP, Hung SF, Lee CC, Liu WS et al (2006) Test-retest reliability and criterion validity of the Chinese version of CBCL, TRF, and YSR. J Child Psychol Psychiatry 47:970–973
Liu X, Zwart JD, Scholvinck ML, Chang C, Ye FQ, Leopold DA, Duyn JH (2018) Subcortical evidence for a contribution of arousal to fMRI studies of brain activity. Nat Commun 9:395. https://doi.org/10.1038/s41467-017-02815-3
Milich R, Balentine AC, Lynam DR (2001) ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clin Psychol Sci Pract 8:463–488. https://doi.org/10.1093/clipsy.8.4.463
Miller LJ, McIntosh DN, McGrath J, Shyu V, Lampe M, Taylor AK, Hagerman RJ et al (1999) Electrodermal responses to sensory stimuli in individuals with fragile X syndrome: a preliminary report. Am J Med Genet 83:268–279
Mokler DJ, Miller CE, McGaughy JA (2017) Evidence for a role of corticopetal, noradrenergic systems in the development of executive function. Neurobiol Learn Mem 143:94–100. https://doi.org/10.1016/j.nlm.2017.02.011
National Institute of Mental Health (2016) Behavioral assessment methods for RDoC constructs: a report by the national advisory mental health council workgroup on tasks and measures for research domain criteria (RDoC). https://www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/reports/rdoc_council_workgroup_report_153440.pdf
Penny AM, Washbusch DA, Klein RM, Corkum P, Eskes G (2009) Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychol Assess 21:380–389. https://doi.org/10.1037/a0016600
Petersen SE, Posner ML (2012) The attention system of the human brain: 20 years after. Annu Rev Neurosci 35:73–89. https://doi.org/10.1146/annurev-neuro-062111-150525
Rahman S, Habel M, Contrada RJ (2018) Poincaré plot indices as measures of sympathetic cardiac regulation: responses to psychological stress and associations with pre-ejection period. Int J Psychophysiol 133:79–90. https://doi.org/10.1016/j.ijpsycho.2018.08.005
Robe A, Dobrean A, Cristea IA, Păsărelu CR, Predescu E (2019) Attention-deficit/hyperactivity disorder and task related heart rate variability: a systematic review and meta-analysis. Neurosci Biobehav Rev 99:11–22. https://doi.org/10.1016/j.neubiorev.2019.01.022
Rozenman M, Sturm A, McCracken JT, Piacentini J (2017) Autonomic arousal in anxious and typically developing youth during a stressor involving error feedback. Eur Child Adolesc Psychiatry 26(12):1423–1432. https://doi.org/10.1007/s00787-017-1001-3
Samuels ER, Szabadi E (2008) Functional neuroanatomy of the noradrenergic locus coeruleus: its roles in the regulation of arousal and autonomic function part I: principles of functional organization. Curr Neuropharmacol 6:235–253. https://doi.org/10.2174/157015908785777229
Schoorl J, Van Rijn S, Wied De, Van Goozen SHM, Swaab H (2016) Variability in emotional/behavioural problems in boys with oppositional defiant disorder or conduct disorder: the role of arousal. Eur Child Adolescent Psychiatry 25:821–830. https://doi.org/10.1007/s00787-015-0790-5
Shaffer F, Ginsberg JP (2017) An overview of heart rate variability metrics and norms. Front Public Health 5:258. https://doi.org/10.3389/fpubh.2017.00258
Song AH, Kucyi A, Napadow V, Brown EN, Loggia ML, Akeju O (2017) Pharmacological modulation of noradrenergic arousal circuitry disrupts functional connectivity of the locus ceruleus in humans. J Neurosci 37:6938–6945. https://doi.org/10.1523/JNEUROSCI.0446-17.2017
Suess PE, Porges SW, Plude DJ (1994) Cardiac vagal tone and sustained attention in school age children. Psychophysiology 31:17–22
Swanson JM, Schuck S, Porter MM, Carlson C, Hartman CA, Sergeant JA, Clevenger W, Wasdell M, McCleary R, Lakes K, Wigal T (2012) Categorical and dimensional definitions and evaluations of symptoms of ADHD: history of the SNAP and the SWAN rating scales. Int J Educ Psychol Assess 10(1):51–70
Task Force of the European Society of Cardiology and North American Society of Pacing and Electrophysiology (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17:354–381
Tamm L, Garner AA, Loren REA, Epstein JN, Vaughn AJ, Ciesielski HA, Becker SP (2016) Slow sluggish cognitive tempo symptoms are associated with poorer academic performance in children with ADHD. Psychiatry Res 242:251–259. https://doi.org/10.1016/j.psychres.2016.05.054
Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH (2009) Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaption, and health. Ann Behav Med 37:141–153. https://doi.org/10.1007/s12160-009-9101-z
Thayer JF, Lane RD (2000) A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord 61:201–216
Tulppo MP, Mäkikallio TH, Takala TE, Seppänen T, Huikuri HV (1996) Quantitative beat-to-beat analysis of heart rate dynamics during exercise. Am J Physiol 271:H244–H252
Wåhlstedt C, Bohlin G (2010) DSM-IV-defined inattention and sluggish cognitive tempo: independent and interactive relations to neuropsychological factors and comorbidity. Child Neuropsychol 16:350–365. https://doi.org/10.1080/09297041003671176
Wechsler D (2010) Wechsler intelligence scale for children, 4th edn. Pearson Inc, Hong Kong
Wietecha L, Williams D, Shaywitz S, Shaywitz B, Hooper SR, Wigal SB, McBurnett K et al (2013) Atomoxetine improved attention in children and adolescents with attention-deficit/hyperactivity disorder and dyslexia in a 16 week, acute, randomized, double-blind trial. J Child Adolesc Psychopharmacol 23:605–613. https://doi.org/10.1089/cap.2013.0054
Wood SK, Valentino RJ (2017) The brain norepinephrine system, stress and cardiovascular vulnerability. Neurosci Biobehav Rev 74:393–400. https://doi.org/10.1016/j.neubiorev.2016.04.018
Wang XW, Piñol RA, Byrne P, Menodelowitz D (2014) Optogenetic stimulation of locus ceruleus neurons augments inhibitory transmission to parasympathetic cardiac vagal neurons via activation of brainstem α1 and β1 receptors. J Neurosci 34:6182–6189. https://doi.org/10.1523/JNEUROSCI.5093-13.2014
Willcutt EG, Chhabildas N, Kinnear M, DeFries JC, Olson RK, Leopold DR, Pennington BF et al (2014) The internal and external validity of sluggish cognitive tempo and its relation with DSM-IV ADHD. J Abnorm Child Psychol 42:21–35
Xing B, Li YC, Gao WJ (2016) Norepinephrine versus dopamine and their interaction in modulating synaptic function in the prefrontal cortex. Brain Res 1641:217–233. https://doi.org/10.1016/j.brainres.2016.01.005
Zahn D, Adams J, Krohn J, Wenzel M, Mann CG, Gomille LK, Kubiak T et al (2016) Heart rate variability and self-control—a meta-analysis. Biol Psychol 115:9–26. https://doi.org/10.1016/j.biopsycho.2015.12.007
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any relevant conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Yung, T.W.K., Lai, C.Y.Y., Chan, J.Y.C. et al. Neuro-physiological correlates of sluggish cognitive tempo (SCT) symptoms in school-aged children. Eur Child Adolesc Psychiatry 29, 315–326 (2020). https://doi.org/10.1007/s00787-019-01353-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-019-01353-1