Abstract
Objective
This meta-analysis was designed to provide new insights into the relationship between Helicobacter pylori (H. pylori) infection and recurrent aphthous stomatitis (RAS).
Materials and methods
We included and evaluated studies on H. pylori infection and RAS from PubMed, EMBASE, Cochrane Library, and Web of Science databases published up to January 31, 2023. The characteristics of these studies were collected, and the quality was evaluated by Newcastle-Ottawa Scale (NOS). The random effects model was used to calculate the pooled odds ratio (OR) and 95% confidence interval (CI). To further explore the sources of heterogeneity, meta-regression analysis and subgroup analyses were performed. Funnel plot, Egger’s test, and Begg’s test were used to assess publication bias.
Results
In total, fifteen case-control studies with 1137 individuals (601 cases and 536 controls) were included. The H. pylori was found to be significantly associated with RAS (OR: 1.83 95% CI: 1.41–2.37, P = 0.001). In the subgroup analyses, studies that used PCR (OR: 2.03 95% CI: 1.31–3.15) or UBT (OR: 1.83 95% CI: 1.13–2.96) yielded a significant positive association, while a non-significant association (OR: 1.12 95% CI: 0.61–2.08) was found from studies that used ELISA method. Sensitivity analyses showed that the results were robust. No significant publication bias was found.
Conclusions
The current evidence does not rule out an association between H. pylori and RAS. The effect of H. pylori on RAS varies in detection methods and sources of sample. Large samples, multiple clinical studies, and improved methods are still needed to determine the exact effect of H. pylori on RAS.
Clinical significance
H. pylori infection may be a risk factor for the pathogenesis of RAS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent aphthous stomatitis, also known as aphthous ulcers (AU), is one of the most common oral mucosal lesions. It is characterized by recurrent round or oval superficial ulcer on the mucous membrane of the mouth, with periodic, progressive, and self-limiting features. Nearly 2 to 66% of the population suffers persistent and repeated pain causes by RAS in the world, which can interfere with important functions such as eating, drinking, swallowing, speaking, and negatively affect the quality of life [1, 2]. The etiology and pathogenesis of RAS remain unclear, but several factors have been proposed as possible etiopathogenesis, including nutritional deficiency (vitamins and minerals), microbial infections, local trauma, food allergy, psychological factors, and genetic factors [3].
Helicobacter pylori (H. pylori) is a gram-negative, microaerophilic, rod-shaped bacteria. It was first isolated from gastritis mucosal biopsies of patients suffering from chronic gastritis in 1983 and recognized as a pathogenic factor for many upper gastrointestinal diseases, such as chronic gastritis and peptic ulcer [4, 5]. More than half of the global population is infected with H. pylori, and the prevalence rates vary across regions, ranging from approximately one-third in North Europe and North America, to higher than 50% in South, East Europe, South America, and Asia [6, 7]. H. pylori has been detected in oral cavity and has been reported to be associated with oral diseases, such as periodontitis, erosive oral lichen planus (OLP), and oral squamous cell carcinoma (OSCC) [8,9,10].
In recent years, there has been growing scientific interest in the association between H. pylori infection and RAS. Numerous studies have shown that anti-pyloric therapy can promote RAS healing, such as shortening the improvement time and reducing the recurrence rate [11]. To date, there have been three meta-analyses explored the relationship between H. pylori and RAS, but the results were conflicting [12,13,14]. Li L et al. conducted a meta-analysis in 2014 included articles limited to September 2013, which showed a positive association [12]. After the previous meta-analyses, many relevant original studies were published. It is necessary to update the pooled OR of H. pylori for RAS with the latest evidences. Besides, there is still lack evidence regarding the effects of test methods, sample sources on the results. Therefore, we conducted this meta-analysis included recently published studies and addressed the aforementioned shortcomings to explore the correlation between H. pylori infection and RAS.
Methods
Protocol and registration
This systematic review was performed according to Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [15]. It was registered at PROSPERO under CRD42023404955.
Search strategy
We searched for a detailed systematic literature published up to January 31st, 2023 from PubMed, EMBASE, Cochrane Library, and Web of Science for all relevant articles.
The following MeSH terms and combinations of words were used for the literature search: (‘Helicobacter pylori’ [MeSH] OR ‘Helicobacter nemestrinae’ OR ‘Campylobacter pylori’ OR ‘Campylobacter pylori subsp. pylori’ OR ‘Campylobacter pyloridis’) AND (‘Stomatitis, Aphthous’ [MeSH] OR ‘Aphthous Stomatitides’ OR ‘Aphthous Stomatitis’ OR ‘Stomatitides, Aphthous’ OR ‘Ulcer, Aphthous’ OR ‘Aphthous Ulcer’ OR ‘Aphthous Ulcers’ OR ‘Ulcers, Aphthous’ OR ‘Aphthae’ OR ‘Canker Sore’ OR ‘Canker Sores’ OR ‘Sore, Canker’ OR ‘Sores, Canker’). Furthermore, a manual retrieval was performed to obtain additional studies (Table S1).
Inclusion criteria and exclusion criteria
The inclusion criteria were as follows: (1) cohort studies or case-control studies; (2) the clinical diagnosis of RAS was based on the description of its clinical presentation and classification: one or several round, shallow, painful oral ulcers, recurrent from months to days apart [16]; and (3) the outcome index of interest was the number of H. pylori positive patients in the RAS group and the control group (non-RAS group), respectively.
The exclusion criteria were as follows: (1) cross-sectional studies, animal experiments, conference abstracts, reviews, duplicate publications, and case reports; (2) incomplete or unavailable original data; (3) studies in specific population; and (4) the low-quality studies (a score of less than 5 points).
Data extraction
The following data items were extracted by two trained reviewers (JS & ZY) independently; any discrepancy between the two reviewers was solved by a third reviewer (YW):
We retrieved relevant information from the final selected studies:
-
A.
Demographic and clinical characteristics: (1) the first author, (2) publication year, (3) country of the study, (4) region, (5) mean age, (6) sex ratio, (7) the number of case group (RAS patients)/control group, and (8) the number of H. pylori positive patient.
-
B.
Methodological characteristics: (1) study design, (2) sample sources of the study, (3) detection methods, and (4) the effect sizes and confidence intervals reported in the studies.
Quality assessment
The quality of the included studies was independently assessed by two researchers (JS & ZY). The Newcastle-Ottawa Scale (NOS) consisting of a nine-point scale was used as a standard international tool to evaluate the quality of the studies [17, 18]. Studies with scores of 5 or higher were categorized as medium to high-quality studies.
Statistical analysis
A meta-analysis was performed to assess the association between H. pylori infection and RAS using STATA/SE 17.0 statistical software. ORs and CIs were calculated. Since the included studies had a small total number of events, ORs were obtained using Peto’s assumption-free method, which is considered the least biased and most powerful approach [19, 20]. Heterogeneity was assessed by the Cochrane Q test and I2 statistics. Given the substantial level of heterogeneity observed (I2 > 60%, P > 0.05), we employed a random effects model for the statistical analysis [21]. To explore the sources of heterogeneity, we conducted subgroup analyses based on factors such as geographic region, detection method, source of sample, study quality score, and publication year. The Funnel plots, Begg’s test, and Egger’s test were used to explore publication bias in the included studies [22, 23]. Sensitivity analyses were conducted to investigate the effect of each individual study on overall analysis.
Results
Systematic search
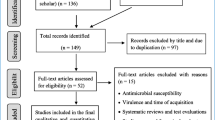
A systematic search identified 169 articles, including 38 articles from PubMed, 93 articles from EMBASE, 5 articles from Cochrane Library, 33 articles from Web of Science. No additional articles were identified through manual searches of reference lists. After excluding duplicate publications (n = 38), 131 articles remained for full-text screening. Based on the predetermined eligibility criteria, a total of 13 articles with 15 case-control studies were included in the review (Fig. 1). In instances where articles encompassed multiple studies featuring diverse clinical groups, we regarded each study as a distinct analysis.
Flowchart diagram of the study selection according to Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [24]
Study characteristics
The main characteristics of the included studies are presented in Table 1. All articles represented a range of geographical areas in Asia (n = 6), Europe (n = 5), South America (n = 1), Africa (n = 1), and Turkey, which straddles both Asia and Europe (n =2). Regarding the detection methods, 7 studies used PCR (PCR and nest-PCR); 3 studies used 13/14C-UBT, 1 study used RUT; 3 studies used ELISA, and 1 study used gastroscopy. In terms of sample sources, there were 8 studies from intraoral tissues, 4 studies from gastric tissue, and 3 studies from venous blood. The results for assessment of quality according to the NOS are presented in Table 2 and Fig. S4.
Main results of the included studies
In the RAS patient group, 601 subjects were included, out of which 242 cases were H. pylori positive. In the control group, 536 cases were included, with 211 positive for H. pylori. The estimated results indicated a statistically significant association between H. pylori infection and RAS, with OR value was 1.83 (95% CI: 1.41–2.37, P = 0.001, as shown in Fig. 2). These findings suggested that H. pylori infection may be linked to RAS. Fig. 2 shows forest plot of the relationship between H. pylori infection and RAS.
Subgroup analyses and meta regression
Subgroup analysis (Table 3) revealed significant positive associations between H. pylori infection and the risk of RAS in studies conducted in Europe (OR: 1.90, 95% CI: 1.26–2.86) and Asia (OR: 1.97, 95% CI: 1.44–2.71) (Fig. S1). Stratification by different H. pylori detection methods showed a significant positive association in studies using PCR (OR: 2.03, 95% CI: 1.31–3.15) and UBT (OR: 1.83, 95% CI: 1.13–2.96), rather than in studies using ELISA (OR: 1.12, 95% CI: 0.61–2.08) (Fig. S2). Furthermore, an association between H. pylori and RAS was found in samples from oral (OR: 2.38, 95% CI: 1.60–3.56) and gastric (OR: 1.72, 95% CI: 1.14–2.60) samples but not venous blood (Fig. S3).
A meta-regression was conducted to explore possible sources of heterogeneity. There were significant differences in the heterogeneity between strata by detection method (P in meta-regression = 0.032).
Sensitivity analysis
A sensitivity analysis was performed to evaluate the stability and reliability of the meta-analysis. Similar results were obtained when each study was sequentially excluded, indicating that no individual study had a significant impact on the overall risk estimates (Fig. 3). To assess the potential publication bias, we examined the symmetry of the funnel plot (Fig. S6) with Begg’s (Fig. S7) and Egger’s tests (Fig. S8). The results indicated a low risk of publication bias. There was no substantial publication bias detected in any of the analyses.
Discussion
The etiology of RAS still remains unclear. Most attempts to culture H. pylori from oral samples have failed [38,39,40]. While H. pylori has been detected on RAS lesions, a definitive connection between microbial infection and RAS has not yet to be established [41]. In this study, our meta-analysis provides evidence to the correlation between H. pylori infection and RAS.
Our results showed that H. pylori was found to be significantly associated with RAS. To the best of our knowledge, H. pylori infection can effect gastric mucosal inflammation and may also act on systemic autoimmune responses [42, 43]. The exact mechanism of tissue damage induced by H. pylori is not clear. Many researchers suggest the immune-mediated mechanisms induced by H. pylori in the development of RAS. H. pylori has the ability to stimulate the production of immune cytokine, particularly IL-8 and lymphocyte chemotactic factors which plays a role inthe formation of particular T lymphocyte subpopulations. Infiltrating neutrophils can also be activated by H. pylori or its extracts, resulting in the production of reactive oxygen metabolites (hydrogen peroxide and hypochlorous acid) [44]. Furthermore, the involvement of cytokine production, over expression of lymphocyte adhesion molecules, and the recruitment of specific subsets of T-lymphocytes have been demonstrated to play a role in both RAS and H. pylori–associated gastritis [11].
The subgroup analyses conducted by regions revealed a positive association between the risk factor H. pylori and RAS in Europe and Asia. Although heredity is widely recognized as one of the well-established underlying causes of RAS [45], its geographical variations have not been reported. The results in South America and Africa subgroups were affected by the limitation of study number, since there was only one study included in each subgroup.
Considering the effect of detection methods and sample sources on the results, we performed subgroup analyses based on these two factors. In the studies using PCR and UBT, we found a positive association between H. pylori and RAS. However, no statistically significant difference was found when ELISA was used as the detection method. Currently, the combination of culture and histologic examination is generally regarded as the “gold standard” for the diagnosis of H. pylori [44,45,46]. The detection of H. pylori in oral cavity mostly relied on traditional methods, such as RUT, immunological method, PCR, and UBT. UBT is one of the commonly used detection methods for gastric H. pylori in clinic, which requires 13C and 14C to react with H. pylori [47]. Whether UBT is suitable for detecting H. pylori in the oral cavity is still worth exploring, given the differences in oral and gastric micro-environment. PCR detection has the advantages of high sensitivity, strong specificity, and low requirements for specimens compared to other diagnostic methods [47, 48]. But the possible transmission of H. pylori by the gastro-oral route and specificity of primers may lead to false positive results [38, 49]. In RUT detection, the urease produced by H. pylori breaks down urea to form ammonia, which increases the PH value of mucosal tissue and changes the color of the detection indicator [47]. However, the oral cavity has many bacteria with a weak alkaline PH value, which may easily lead to false positives [50]. ELISA is a non-invasive, simple, and inexpensive method for the diagnosis of H. pylori infection. While, the serology ELISA detection was unable to distinguish infection status and site [48, 51]. Given the comparative analysis of the above detection mechanism, PCR and UBT methods are relatively accurate, which is also the source of heterogeneity in this meta-analysis.
Serology detection of H. pylori in studies often used ELISA, which could not distinguish the infection site, and the serum antibodies could persist for a period of time after the eradication of the pathogen [52]. This may lead to the inaccurate results, and the limited number of studies may also lead to false negative results. Therefore, the result of ELISA detection methods was consistent with that of serum source in subgroup analyses.
Our meta-analysis included the latest research in recent years compared to previous meta-analyses. We strictly screened the study design and RAS diagnostic basis of the included studies, which increased the comparability of study data and the authenticity of the results. We also performed subgroup analyses according to region, detection method, and source of sample. This study aims to provide new insights into the relationship between H. pylori and RAS. To better interpret the results, some limitations of this meta-analysis should be noted, such as the small sample size of each included study, the absence of a cohort study with high reliability, and the poor quality of the included articles. Furthermore, this study did not analyze the source of H. pylori. There is still controversy on whether H. pylori is resident or transient in oral cavity. Many literatures suggest a correlation and homology between oral H. pylori and gastric H. pylori [24, 53,54,55]. In oral sample collection, many researches did not consider reflux and hiccup, which may bring H. pylori from the stomach to the oral [49]. Therefore, for exploring the relationship between different sources of H. pylori and RAS, careful sampling techniques can help reduce the likelihood of contamination, for instance, taking oral samples at least 2 h after reflux [49]. For many detection methods, the positive results may not mean the H. pylori infection since the potential cross-reactions with other bacteria. The whole-genome sequencing of the isolates and subsequent deposition of the organisms in a culture collection are needed to confirm the H. pylori colonization of the oral cavity [49]. If possible, comparing the genetic characteristics of the oral H. pylori strains to strains isolated from the stomach can provide insights into whether they are similar or distinct. This may help us clarify the association between H. pylori and oral diseases.
Conclusion
In conclusion, the current evidence does not rule out an association between RAS and H. pylori. The effect of H. pylori on RAS varies in detection methods and the sources of sample. However, due to the limitations of oral H. pylori detection methods, we cannot determine the source of H. pylori in detection samples definitely. Large samples, multiple clinical studies, and improved detection methods are still needed to determine the exact effect of H. pylori on RAS.
Data availability
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author.
References
Rivera C, Muñoz-Pastén M, Núñez-Muñoz E, Hernández-Olivos R (2022) Recurrent aphthous stomatitis affects quality of life. A case-control study. Clin Cosmet Investig Dent 14:217–223. https://doi.org/10.1101/2022.04.01.22273300
Xu KY, Zhou CC, Huang F, Duan N, Wang YY, Zheng LC, Wang X, Wang WM (2021) Relationship between dietary factors and recurrent aphthous stomatitis in China: a cross-sectional study. J Int Med Res 5:30006052110177. https://doi.org/10.1177/03000605211017724
Rees TD, Binnie WH (1996) Recurrent aphthous stomatitis. Dermatol Clin 2:243–256. https://doi.org/10.1016/s0733-8635(05)70353-3
Wei X, Zhao HQ, Ma C, Zhang AB, Feng H, Zhang D, Liu C (2019) The association between chronic periodontitis and oral Helicobacter pylori: a meta-analysis. PLoS One 12:e0225247. https://doi.org/10.1371/journal.pone.0225247
Xue Y, Zhou LY, Lu HP, Liu JZ (2019) Recurrence of Helicobacter pylori infection: incidence and influential factors. Chin Med J 7:765–771. https://doi.org/10.1097/CM9.0000000000000146
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, Malfertheiner P, Graham DY, Wong VWS, Wu JCY, Chan FKL, Sung JJY, Kaplan GG, Ng SC (2017) Global prevalence of Helicobacter pylori infection: systematic review and meta-Analysis. Gastroenterol 2:420–429. https://doi.org/10.1053/j.gastro.2017.04.022
Eusebi LH, Zagari RM, Bazzoli F (2014) Epidemiology of Helicobacter pylori infection. Helicobacter 1:1–5. https://doi.org/10.1111/hel.12165
Liu Y, Li R, Xue X, Xu T, Luo Y, Dong Q, Liu J, Liu J, Pan Y, Zhang D (2020) Periodontal disease and Helicobacter pylori infection in oral cavity: a meta-analysis of 2727 participants mainly based on Asian studies. Clin Oral Investig 7:2175–2188. https://doi.org/10.1007/s00784-020-03330-4
Li S, Zhang Y, Yang Z, Li J, Li Y, Li H, Li W, Jia J, Ge S, Sun Y (2021) Helicobacter pylori infection is correlated with the incidence of erosive oral lichen planus and the alteration of the oral microbiome composition. BMC Microbiol 1:122. https://doi.org/10.1186/s12866-021-02188-0
Gupta AA, Kheur S, Raj AT, Mahajan P (2020) Association of Helicobacter pylori with oral potentially malignant disorders and oral squamous cell carcinoma-a systematic review and meta-analysis. Clin Oral Investig 1:13–23. https://doi.org/10.1007/s00784-019-03125-2
Albanidou-Farmaki E, Giannoulis L, Markopoulos A, Fotiades S, Aggouridaki X, Farmakis K, Papanayotou P (2005) Outcome following treatment for Helicobacter pylori in patients with recurrent aphthous stomatitis. Oral Dis 1:22–26. https://doi.org/10.1111/j.1601-0825.2004.01053.x
Li L, Gu H, Zhang G (2014) Association between recurrent aphthous stomatitis and Helicobacter pylori infection: a meta-analysis. Clin. Oral Investig 6:1553–1560. https://doi.org/10.1007/s00784-014-1230-5
Gomes CC, Gomez RS, Zina LG, Amaral FR (2016) Recurrent aphthous stomatitis and Helicobacter pylori. Med Oral Patol Oral Cir Bucal 2:e187–e191. https://doi.org/10.4317/medoral.20872
Zou LT, Hu YL (2013) A meta-analysis of the association between Helicobacter pylori and recurrent oral ulcers. Infect Inflamm Repair 2:102–106. https://doi.org/10.3969/j.issn.1672-8521.2013.02.013
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 10:1006–1012. https://doi.org/10.1371/journal.pmed.1000097
Slebioda Z, Szponar E, Kowalska A (2014) Etiopathogenesis of recurrent aphthous stomatitis and the role of immunologic aspects: literature review. Arch Immunol Ther Exp 3:205–215. https://doi.org/10.1007/s00005-013-0261-y
Wells GA, Wells G, Shea B, Shea B, O'Connell D, Peterson J, Welch, Losos M, Tugwell P, Ga SW, Zello GA, Petersen JA (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Semantic Scholar https://www.semanticscholar.org/paper/The-Newcastle-Ottawa-Scale-(NOS)-for-Assessing-the-Wells-Wells/c293fb316b6176154c3fdbb8340a107d9c8c82bf. Accessed 13 Apr 2013
Stang A, Jonas S, Poole C (2018) Case study in major quotation errors: a critical commentary on the Newcastle–Ottawa scale. Eur J Epidemiol 11:1025–1031. https://doi.org/10.1007/s10654-018-0443-3
Mohr SB, Gorham ED, Alcaraz JE, Kane CJ, Macera CA, Parsons JK, Wingard DL, Garland CF (2011) Serum 25-hydroxyvitamin D and prevention of breast cancer: pooled analysis. Anticancer Res Sep 31(9):2939–48. https://pubmed.ncbi.nlm.nih.gov/21868542
Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A (2007) Much ado about nothing: a comparison of the performance of meta-analytical methods with rare events. Stat Med 1:53–77. https://doi.org/10.1002/sim.2528
Barili F, Parolari A, Kappetein PA, Freemantle N (2018) Statistical primer: heterogeneity, random- or fixed-effects model analyses? Interact Cardiovasc Thorac Surg 3:317–321. https://doi.org/10.1093/icvts/ivy163
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 4:1088–1101. https://doi.org/10.2307/2533446
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 7109:629–634. https://doi.org/10.1136/bmj.315.7109.629
Silva DG, Tinoco EM, Rocha GA, Rocha AM, Guerra JB, Saraiva IE, Queiroz DM (2010) Helicobacter pylori transiently in the mouth may participate in the transmission of infection. Mem Inst Oswaldo Cruz 5:657–660. https://doi.org/10.1590/s0074-02762010000500009
Long BJ, Chen K, Wu BL, Duan JM (2007) Detection of Helicobacter pylori in patients with recurrent oral ulcer. J Southern Med Univ 4:477–478. https://doi.org/10.3321/j.issn:1673-4254.2007.04.040
Al-Amad SH (2020) Helicobacter pylori and gastric hyperacidity, and their association with recurrent aphthous stomatitis. Int J Oral Maxillofac Surg 12:1599–1604. https://doi.org/10.1016/j.ijom.2020.05.013
Gülseren D, Karaduman A, Kutsal D, Nohutcu RM (2016) The relationship between recurrent aphthous stomatitis, and periodontal disease and Helicobacter pylori infection. Clin Oral Investig 8:2055–2060. https://doi.org/10.1007/s00784-015-1704-0
Rajendra K, Purnachandra SM, Patel PC, Cota J, Singh VR, Vatsal A (2017) A clinical and microbiological evaluation of Helicobacter pylori in recurrent aphthous stomatitis. J Contemp Dent Pract 12:1194–1197. https://doi.org/10.5005/jp-journals-10024-2199
Maleki Z, Sayyari AA, Alavi K, Sayyari L, Baharvand M (2009) A study of the relationship between Helicobacter pylori and recurrent aphthous stomatitis using a urea breath test. J Contemp Dent Pract 1:9–16. https://doi.org/10.5005/jcdp-10-1-9
Iamaroon A, Chaimano S, Linpisarn S, Pongsiriwet S, Phornphutkul K (2003) Detection of Helicobacter pylori in recurrent aphthous ulceration by nested PCR. J Oral Sci 2:107–110. https://doi.org/10.2334/josnusd.45.107
Victória JM, Kalapothakis E, Silva Jde F, Gomez RS (2003) Helicobacter pylori DNA in recurrent aphthous stomatitis. J Oral Pathol Med 4:219–223. https://doi.org/10.1034/j.1600-0714.2003.00136.x
Riggio MP, Lennon A, Wray D (2000) Detection of Helicobacter pylori DNA in recurrent aphthous stomatitis tissue by PCR. J Oral Pathol Med 10:507–513. https://doi.org/10.1034/j.1600-0714.2000.291005.x
Porter SR, Barker GR, Scully C, Macfarlane G, Bain L (1997) Serum IgG antibodies to Helicobacter pylori in patients with recurrent aphthous stomatitis and other oral disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83:325–328. https://doi.org/10.1016/S1079-2104(97)90237-7
Saeed SA, Zaidan TF (2020) Clinical evaluation of recurrent aphthous stomatitis and its correlation with Helicobacter pylori. Indian J Forensic Med Toxicol 4:2154–2159. https://doi.org/10.37506/ijfmt.v14i4.11870
Uyar M, Kilic SB, Uyar Y, Ozkaya E, Iriz A, Eryilmaz A (2014) The place of the Helicobacter pylori on the etiopathogenesis of idiopathic recurrent aphthous stomatitis (RAS). ResearchGate. https://www.researchgate.net/publication/266208526. Accessed 5 August 2023
Elsheikh MN, Mahfouz ME (2005) Prevalence of Helicobacter pylori DNA in recurrent aphthous ulcerations in mucosa-associated lymphoid tissues of the pharynx. Arch Otolaryngol Head Neck Surg 9:804–808. https://doi.org/10.1001/archotol.131.9.804
Yakar T, Serin E, Coşar AM, Arslan Taş D, Ataç FB (2015) The relationship of recurrent aphthous stomatitis and Helicobacter pylori, cytokine gene polymorphism and cobalamin. Turk J Gastroenterol 4:1461–1464. https://doi.org/10.5152/tjg.2015.0161
Al-Ahmad A, Kürschner A, Weckesser S, Wittmer A, Rauberger H, Jakob T, Hellwig E, Kist M, Waidner B (2012) Is Helicobacter pylori resident or transient in the human oral cavity? J Med Microbiol 8:1146–1152. https://doi.org/10.1099/jmm.0.043893-0
Teoman I, Ozmeriç N, Ozcan G, Alaaddinoğlu E, Dumlu S, Akyön Y, Baloş K (2007) Comparison of different methods to detect Helicobacter pylori in the dental plaque of dyspeptic patients. Clin Oral Investig 3:201–205. https://doi.org/10.1007/s00784-007-0104-5
Allaker RP, Young KA, Hardie JM, Domizio P, Meadows NJ (2002) Prevalence of Helicobacter pylori at oral and gastrointestinal sites in children: evidence for possible oral-to-oral transmission. J Med Microbiol 4:312–317. https://doi.org/10.1099/0022-1317-51-4-312
Mansour-Ghanaei F, Asmar M, Bagherzadeh AH, Ekbataninezhad S (2005) Helicobacter pylori infection in oral lesions of patients with recurrent aphthous stomatitis. Med Sci Monit 11(12):CR576–CR579. https://pubmed.ncbi.nlm.nih.gov/16319788
Bodger K, Wyatt JI, Heatley RV (1997) Gastric mucosal secretion of interleukin-10: relations to histopathology, Helicobacter pylori status, and tumor necrosis factor-a secretion. Gut 6:739–744. https://doi.org/10.1136/gut.40.6.739
Gasbarrini A, Franceschi F, Arnuzzi A, Ojetti V, Candelli M, Torre ES, De Lorenzo A, Anti M, Pretolani S, Gasbarrini G (1999) Extradigestive manifestations of Helicobacter pylori infection. Gut Suppl 1:1–12. https://doi.org/10.1136/gut.45.2008.i9
Birek C, Grandhi R, McNeill K, Singer D, Ficarra G, Bowden G (1999) Detection of Helicobacter pylori in oral aphthous ulcers. J Oral Pathol Med 5:197–203. https://doi.org/10.1111/j.1600-0714.1999.tb02024.x
Diouf A, Martinez-Gomis J, Miquel M, Quesada M, Lario S, Sixou M (2009) Comparison of four different primer sets for detection of Helicobacter pylori in gastric biopsies and oral samples by using real-time PCR. Pathol Biol (Paris) 57(1):30–35. https://doi.org/10.1016/j.patbio.2008.07.008
Xue CY, Tan Y, Wang YJ (2020) Correlation analysis between oral Helicobacter pylori infection and peri-implantitis and its clinical indexes. J Huazhong University Sci Technol 6:728–731. https://doi.org/10.3870/j.issn.1672-0741.2020.06.015
Ye GQ (2012) Clinical detection of oral Helicobacter pylori infection: current hot spots in the field of diagnosis. Chin Med J 16:1084–1086. https://doi.org/10.3760/cma.j.issn.0376-2491.2012.16.002
Wang YK, Kuo FC, Liu CJ, Wu MC, Shih HY, Wang SS, Wu JY, Kuo CH, Huang YK, Wu DC (2015) Diagnosis of Helicobacter pylori infection: current options and developments. World J Gastroenterol 40:11221–11235. https://doi.org/10.3748/wjg.v21.i40.11221
Mao X, Jakubovics NS, Bächle M, Buchalla W, Hiller KA, Maisch T, Hellwig E, Kirschneck C, Gessner A, Al-Ahmad A, Cieplik F (2021) Colonization of Helicobacter pylori in the oral cavity - an endless controversy? Crit Rev Microbiol 5:612–629. https://doi.org/10.1080/1040841X.2021.1907740
Ding YF, Xiao XR, Li AM, Dai CB (2002) Detection of Helicobacter pylori infection in gastric and oral cavity. Mod Prev Med 4:474–475. https://doi.org/10.3969/j.issn.1003-8507.2002.04.004
Zhang QF, Yu XQ, Liu JT (2016) Research progress on detection methods of gastric Helicobacter pylori and oral Helicobacter pylori. Int J Gastroenterol 2:111–114. https://doi.org/10.3969/j.issn.1673-534X.2016.02.012
Deng XD, Qiang L, Chen X, Bao Y (2022) Research progress on detection technology of Helicobacter pylori. J Cancer Control Treat 7:659–665. https://doi.org/10.3969/j.issn.1674-0904.2022.07.013
Rasmussen LT, Labio RW, Gatti LL, Silva LC, Queiroz VF, Smith Mde A, Payão SL (2010) Helicobacter pylori detection in gastric biopsies, saliva and dental plaque of Brazilian dyspeptic patients. Mem Inst Oswaldo Cruz 3:326–330. https://doi.org/10.1590/s0074-02762010000300015
Assumpção MB, Martins LC, Melo Barbosa HP, Barile KA, de Almeida SS, Assumpção PP, Corvelo TC (2010) Helicobacter pylori in dental plaque and stomach of patients from Northern Brazil. World J Gastroenterol 24:3033–3039. https://doi.org/10.3748/wjg.v16.i24.3033
Cai H, Li W, Shu X, Peng K, Zhang Y, Jiang M (2014) Genetic variation of Helicobacter pylori in the oral cavity and stomach detected using thymine adenine cloning in children with chronic gastritis. Pediatr Infect Dis J 1:e1–e6. https://doi.org/10.1097/INF.0000000000000017
Acknowledgements
Thanks to James K. H. Tsoi, Hangzhou Qiantang Specialty Appointed Expert (Hospital of Stomatology, Zhejiang Chinese Medical University, Hangzhou), for his supervision and guidance on this article.
Funding
This work was supported by the Program of Xinmiao Talents in Zhejiang Province (grant no. 2022R41A044) and Innovation and Entrepreneurship Training Program for College Students of Zhejiang Province (grant no. S202210344118).
Author information
Authors and Affiliations
Contributions
Y. Chen: Study concept and Writing –review & editing, Supervision, Visualization. Y. Wu: Study design and Writing – review & editing. J. Shen: Conceptualization, Methodology, Formal analysis, Writing – original draft. Z. Ye: Methodology, Investigation, Formal analysis. H. Xie: Methodology, Investigation, Formal analysis. D. Ling: Conceptualization, Writing – review & editing, Supervision. The authors had full access to the data and take full responsibility for the results. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
For this type of study, formal consent is not required.
Competing interests
The authors declare no competing interests.
Registration
The review was registered in PROSPERO (ref: CRD42023404955).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 0.98 MB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, J., Ye, Z., Xie, H. et al. The relationship between Helicobacter pylori infection and recurrent aphthous stomatitis: a systematic review and meta-analysis. Clin Oral Invest 27, 6345–6356 (2023). https://doi.org/10.1007/s00784-023-05273-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05273-y