Abstract
Objectives
To evaluate the effects of different types of restorations on observer ability to detect proximal caries in CBCT images.
Materials and methods
Forty human premolars and molars with artificial proximal caries were placed proximal and distal to 5 molars having different restorations (amalgam, composite, resin-modified glass ionomer cement (RMGIC) fillings, zirconia, and lithium disilicate crowns) and a non-restored molar. CBCT scans were obtained using i-CAT® Next Generation. Images were rated twice by 2 observers. The exact depth of artificial caries was histologically established. Sensitivity, specificity, and area under the receiver operating characteristic curve (Az) values were calculated.
Results
Caries detection in teeth surfaces mesial and distal to amalgam showed compromised specificity and accuracy. Moreover, caries detection in teeth surfaces mesial to zirconia crown showed low sensitivity, specificity, and accuracy. Capability of CBCT in detection of proximal caries in teeth adjacent to composite, RMGIC, and lithium disilicate was comparable to those adjacent to non-restored molar.
Conclusions
CBCT scans performed for tasks other than caries detection should be assessed for proximal caries in absence of any restorations as well as in presence of composite, RMGIC fillings, and lithium disilicate crowns. However, CBCT should not be used for proximal caries detection in teeth adjacent to amalgam and teeth surfaces mesial to zirconia crowns.
Clinical significance
It is important to investigate the influence of artifacts produced by various restorations on CBCT-based caries detection to optimize CBCT benefits, caries diagnosis and avoid unnecessary treatment of sound surfaces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early detection of dental caries is very important, as caries progression leads to substantial health and economic burdens on patients and society [1]. Although proximal caries in posterior teeth is commonly detected with the aid of intraoral bitewing radiography[2], bitewing detects only about 60% of proximal carious lesions [3].
Cone beam computed tomography (CBCT) is a valuable addition to 2-dimensional radiographic modalities in maxillofacial region examinations, as it provides clear images free of superimpositions, magnification, and distortions. When there are no adjacent restorations, several studies reported better sensitivity, specificity, and accuracy of CBCT images compared to those of intraoral radiography in the detection of proximal caries [4,5,6]. While some studies revealed that CBCT diagnostic accuracy was similar to that of conventional and digital intraoral modalities [7,8,9], other studies stated that CBCT proximal caries detection accuracy was lower than that of intraoral radiographs [10, 11].
A variety of restorative materials are used by dentists and recognized on projection radiographs. They have variable levels of radiopacity depending on their atomic number, thickness, and density [12]. In CBCT, interaction of the polyenergetic X-ray beam with high-density materials commonly produces beam hardening artifacts [13, 14]. Such artifacts are presented as bright streaks and dark bands. The bright streaks may cover the carious lesion leading to false-negative diagnosis, while dark bands may convey false impressions of carious lesions [15, 16]. These artifacts inhibit the diagnostic ability of CBCT images by decreasing contrast, concealing structures, and consequently impairing diagnosis [17].
Many studies have investigated the effect of different restorative materials on detection of recurrent caries by CBCT with conflicting results. Some studies found that CBCT has a similar diagnostic ability in detection of recurrent caries under amalgam and composite fillings [18, 19]. Other studies declared better accuracy of CBCT images for recurrent caries detection in presence of composite than amalgam restorations [20, 21]. Recurrent caries under zirconia and lithium disilicate crowns was accurately detected using CBCT [22].
Few studies have evaluated the accuracy of CBCT in detection of proximal caries in presence of different restorations. Amalgam fillings were assessed in two previous studies regarding their effect on detection of proximal caries by CBCT [15, 16]. Only one study assessed composite, resin-modified glass-ionomer cement (RMGIC), and zirconia inlay restorations [15]. Zirconia and lithium disilicate crowns were not previously evaluated regarding their influence on proximal caries detection by CBCT.
Considering the continuous influx of new dental materials with various X-ray attenuating properties and the increased use of CBCT in dental practice, this study aimed to evaluate the impact of artifacts produced by 5 current and frequently used restorative materials on the accuracy of CBCT-based detection of proximal carious lesions.
Materials and methods
This ex vivo study was expedited from review by Ain Shams University Faculty of Dentistry Ethics Committee. Assuming a diagnostic accuracy of 70% with an error margin of 10% and a significance level of 95%, the required sample size was 80 surfaces [16].
Preparation of artificially carious teeth
Forty sound human molars and premolars were included in the study. The teeth were extracted for orthodontic and periodontal reasons matching the selection criteria: no cracks and restorations, no developmental anomalies or hypo-plastic structures, and no cavitations caries. Randomly selected 20 proximal surfaces were left sound, while other 60 proximal surfaces were prepared to possess varying degrees of artificial proximal caries. On the proximal surface of the test tooth just below the contact area, a circular piece of rubber was applied; then the tooth was coated with a fast-drying acid-resistant nail polish except for the rubber circle. After the varnish dried, the rubber circle was removed leaving a circular window of 2 mm diameter of exposed enamel. The teeth were kept individually immersed in 8 ml of 5% formic acid solution for 10 or 20 or 30 h to induce different lesion depths. After completion of demineralization time, the teeth were cleaned with acetone to remove the varnish [23].
Preparation of artifact-producing teeth
To evaluate the effects of various restorations, three molars with mesial-occlusal-distal (MOD) cavity were prepared to receive one of the following filling materials: amalgam (Cavex, Haarlem, Netherlands), composite (Valux Plus, 3 M ESPE, St Paul, MN, USA), and RMGIC (GC Fuji® II LC, GC Corporation, Tokyo, Japan). Another two molars were prepared with chamfer margin for each of 2 different full-coverage computer-aided design and computer-aided manufacture crowns: zirconia (Natura Z Block, DMAX Co., Ltd., Daegu, Korea) and lithium disilicate (IPS e.max® CAD; Ivoclar Vivadent AG, Schaan, Liechtenstein). Moreover, one non-restored molar was used as a control tooth. The non-restored and 5 restored molars served as artifact-producing teeth.
Assembling the teeth in the dry mandible
The artificially carious teeth were divided into 20 groups each composed of one premolar and one molar. Group by group, the teeth were assembled in the empty sockets of the right second premolar and second molar in proximal contact with one artifact-producing molar positioned in place of the first molar in a dry human dentate mandible. Then the whole mandible was covered with three layers of softened pink wax buccally and lingually to simulate soft tissues during exposure (Fig. 1).
CBCT scanning
Standardized CBCT scans for the mandible were obtained using i-CAT® Next Generation CBCT scanner (Imaging Sciences International, Hatfield, PA) at 120 kV, 5 mA, field of view (FOV) 16 × 5 cm, voxel size 0.2 mm, and an exposure time of 26.9 s. The mandible was stabilized using a strengthened paper box mounted on the supporting plate of the machine. The midline of the mandible was adjusted with the anterior vertical laser light, while the posterior vertical laser light was placed just anterior to the ramus of mandible. The horizontal laser light was adjusted to be parallel to the occlusal plane of the teeth.
The first scanned group of artificial carious teeth was then removed from the mandible, and the subsequent groups were placed in their positions and scanned without changing the artifact-producing molar. A total of 120 CBCT scans were obtained as each one of the six artifact-producing molars was imaged with the 20 groups of artificially carious teeth.
Radiographic image analysis
All CBCT images were reconstructed at 0.2 mm thickness to optimize proximal caries detection. Two calibrated and blinded dental radiologists with 10-year experience assessed the images using the inherent i-CAT Vision™ software viewer and the same computer monitor (15.6-inch HD LED) with a resolution of 1920 × 1080 under subdued lights conditions. The observers investigated the proximal surfaces of artificially carious teeth extending from the occlusal surface to the cemento-enamel junction by scrolling through different orthogonal and non-orthogonal sections and rated the proximal surfaces using a four-grade scale:
-
0: Sound
-
1: Radiolucency in the outer half of the enamel
-
2: Radiolucency extending more than half of the enamel up to the dentino-enamel junction (DEJ)
-
3: Radiolucency extending through enamel and outer half of dentin [24]
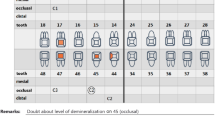
Observers were allowed to perform any needed image adjustments to improve radiographic image analysis. Each observer assessed 20 scans in each viewing session with 2-week intervals with a total of 12 separate viewing sessions 2 sessions for each artifact-producing molar. A total of 120 CBCT scans counting up to 480 proximal surfaces were rated by each observer twice. According to the proximity of the surface being investigated to the artifact-producing molar, artificially carious surfaces were divided into two groups: 240 surfaces mesial to the artifact-producing molars and 240 surfaces distal to the artifact-producing molars. Figure 2 demonstrates an example of CBCT images of the same set of artificially carious teeth in the vicinity of the studied restorations and the non-restored molar.
Microscopic examination
After completion of the radiographic assessment, each tooth was sectioned in a mesiodistal direction. Two blinded oral pathologists examined both sides of each section under a stereomicroscope (Olympus DP 10, SZ-PT, Japan) with 10 × magnification with consensus (Fig. 3). They scored caries according to the deepest spot in both sections using a four-grade scale [25]:
-
0: No caries apparent
-
1: Carious lesions in the outer half of enamel only
-
2: Carious lesions in more than half of enamel up to the DEJ
-
3: Carious lesions penetrating the DEJ and in the outer half of dentin
Data analysis
Statistical Package for the Social Sciences (SPSS®) (IBM Corporation, NY, USA) version 17 for Windows was used for data analysis. Intra- and inter-observer agreements were assessed using weighted kappa values and interpreted as follows: < 0.10 no agreement, 0.10–0.40 poor, 0.41–0.60 moderate, 0.61–0.80 strong, and 0.81–1.00 excellent agreement. For CBCT caries detection in teeth adjacent to different restorations, sensitivity, specificity, and area under the receiver operating characteristic (ROC) curve (Az) values were calculated and compared using z test The significance level was set at P < 0.05.
Results
Table 1 shows the analytical data of the artificially carious teeth based on histological examination. Strong to excellent intra-observer and moderate to excellent inter-observer agreements were found for CBCT proximal caries detection in presence of different restorations and non-restored molar (Table 2). The least inter-observer agreement was found for caries detection in teeth surfaces mesial to zirconia followed by teeth surfaces distal to amalgam.
Caries detection sensitivity in mesial and distal surfaces of teeth adjacent to studied restorations was generally high (0.87–0.99). The specificity of sound surface detection ranged from 0.45 to 1.00 for mesial surfaces and from 0.83 to 0.95 for distal surfaces (Table 3). Accuracy of CBCT-based caries detection in mesial and distal teeth surfaces ranged from 0.70 to 0.99 (Table 4).
Compared to control tooth, teeth surfaces mesial to amalgam filling showed highly significant less specificity and accuracy. Teeth surfaces distal to amalgam showed significantly less sensitivity and accuracy of CBCT-based caries detection. In addition, teeth surfaces mesial to zirconia crown showed significantly less sensitivity, specificity, and accuracy (Table 5).
Discussion
The present study investigated the potential effects of different dental fillings and permanent full crowns on the accuracy of CBCT-based proximal caries detection. Moreover, the diagnostic ability of CBCT in detection of proximal caries in absence of any restorations was assessed.
CBCT is not the investigation of choice for caries detection due to the higher radiation dose involved compared to intraoral radiography [26]. However, when CBCT is done for any other reason and if it is found to be accurate in proximal caries detection in the presence of different restorations, then it is the responsibility of the radiologist/clinician to check for presence of caries without prescribing further radiographs according to the ALARA principle.
Our study sample consisted of extracted sound human premolars and molars. Artificial proximal caries with different depths were induced using 5% formic acid as it is well accepted that chemically induced caries with acids could precisely simulate the clinical situation [19, 27]. Similar to Gaalaas et al. [6], a dry human mandible was used, and the teeth were adapted with their roots into the empty sockets in proximal contact to simulate the real dental arch as much as possible.
It is well-known that image degradation is proportional to the number of restorations in the jaws [28]. For this reason, we attempted to assess the artifacts produced by one restoration in the dental arch and avoid the effect of multiple restorations. Although radiation dose was not an issue in this ex vivo study, medium FOV 16 × 5 cm and 0.2 mm voxel size were used for CBCT scanning of a single arch as this is the most frequently used setting used for most dental diagnostic tasks.
Intra-observer agreement was better than inter-observer agreement for caries detection in the vicinity of amalgam and zirconia restorations. This might indicate that each observer was more or less consistent in differentiating caries from streaks and dark bands. Similarly, Kulczyk et al. [16] declared excellent intra-observer and moderate inter-observer agreements in CBCT detection of proximal caries in presence of amalgam filling.
Strong to excellent intra- and inter-observer agreement for proximal caries detection was found in teeth surfaces in the vicinity of composite, RMGIC fillings, lithium disilicate crown, and non-restored molar. Likewise, Cebe et al. [15] reported excellent inter-observer reliability for CBCT caries detection in teeth surfaces mesial and distal to composite and RMGIC fillings. Moreover, Aglarci et al. [22] revealed strong inter-observer consistency for recurrent caries detection under lithium disilicate crowns. Besides, Belem et al. [29] showed strong intra- and inter-observer reliability in detection of enamel proximal caries using CBCT in absence of any restoration.
Presence of amalgam filling in the FOV resulted in intense beam hardening artifacts that have a broad effect involving both mesial and distal surfaces of the two adjacent teeth. The ability to detect sound teeth surfaces mesial and carious lesions distal to amalgam restoration by CBCT is considerably compromised. A possible explanation is that the dark bands that appeared close to amalgam restoration mimicked carious lesions, which made it challenging to recognize sound teeth surfaces close to amalgam, while bright streak artifacts were more pronounced further away from the amalgam restoration and masked carious lesions in distal teeth surfaces.
Likewise, Cebe et al. [15] reported that caries detection in surfaces mesial to amalgam showed low specificity, while distal surfaces showed low sensitivity using Planmeca CBCT unit (ProMax 3D Mid, Helsinki, Finland). However, compared to our results, they obtained a much lower sensitivity of caries detection in distal surfaces and total inability (0% specificity) to detect sound surfaces mesial to amalgam. This could be explained by the low 90 kV CBCT used in that study which amplified the beam hardening artifacts.
Conversely, Kulczyk et al. [16] evaluated the influence of amalgam fillings on the detection of proximal caries by NewTom 3G CBCT (Quantitative Radiology, Verona, Italy). They observed very low sensitivity and specificity of caries detection in teeth surfaces mesial and distal to amalgam filing and ascribed these results to image intensifier tube and charge-coupled device (ITT/CCD) detector and larger FOV 15 × 13 cm which increased the beam hardening artifacts of amalgam.
Presence of zirconia crown in the FOV produced intense beam hardening artifacts that were confined and only affected mesial surfaces of adjacent teeth. These artifacts greatly reduced the sensitivity and accuracy of caries detection in mesial tooth surfaces, while caries detection in teeth surfaces distal to zirconia crown was comparable to non-restored molar and other tested restorations.
On the contrary, Cebe et al. [15] declared low sensitivity of caries detection in teeth surfaces distal to zirconia inlay and very low specificity in mesial teeth surfaces. Even though they studied zirconia inlay in MOD cavity compared to full coverage zirconia crown in the present research, they reported more widespread artifacts. Lower scanning kV could be responsible for the amplified zirconia artifact in that study.
Otherwise, the present study showed favorable sensitivity, specificity, and accuracy of CBCT in the detection of proximal caries in teeth adjacent to composite, RMGIC, and lithium disilicate. These restorations presented acceptable radiopacity within the useful range and did not affect the diagnostic ability of CBCT for proximal caries detection.
Similarly, Aglarci et al. [22] assessed the diagnostic ability of NewTom 5G CBCT in detection of natural recurrent caries left under zirconia, lithium disilicate, and metal-supported ceramic full crowns. They declared that CBCT could be used as a post-treatment diagnostic technique for detecting caries under fixed crowns.
In contrast, Cebe et al. [15], when investigating the effect of composite and RMGIC on proximal caries detection, revealed low sensitivity of caries detection in distal teeth surfaces and very low specificity of caries detection in mesial teeth surfaces. These differences could be attributed to multiple factors: low scanning kV, high filler content of the hybrid composite (68% by volume) [30] compared to the single filler type 100% zirconia/silica (66% by volume) used in the current study, besides, they assessed natural proximal carious lesions with visually intact proximal surfaces where detection of caries is even more challenging.
The present study revealed optimal sensitivity (0.97), specificity (1.00 to 0.93), and accuracy (0.98) of CBCT for proximal caries detection in absence of any restorations. Similarly, Belem et al. [29] showed high sensitivity (0.88), specificity (0.87), and accuracy (0.88) in detection of proximal enamel caries using i-CAT® CBCT unit working with high kV 120. Flat-panel CBCT-based images show limited beam hardening artifacts from the high-density nearby enamel [31, 32].
Alternatively, Wenzel et al. [4] registered high specificity (0.99) and accuracy (0.85) but low sensitivity (0.58) for detection of proximal surfaces cavitations using 3D Accuitomo CBCT (FPD 80, Morita Corp. Ltd., Tokyo, Japan). Furthermore, Krzyzostaniak et al. [10] reported a low Az value (0.63) of NewTom 3G CBCT in detection of non-cavitated proximal lesions. These differences are probably related to the IIT/CCD detector of the used CBCT machines.
Moreover, Sansare et al. [5] found relatively sub-optimal sensitivity (0.75–0.79), specificity (0.77), and accuracy (0.76–0.78) in detection of proximal caries clinically using Kodak 9000 3D CBCT system (Carestream Health Inc., Rochester, NY, USA). Like i-CAT® Next Generation CBCT used in the current work, Kodak 9000 3D CBCT system implements a flat-panel detector. The lower sensitivity and specificity reported by Sansare et al. [5] compared to our results might be due to low scanning 80 kV and their in vivo experimental design. CBCT patients’ scans have considerably more image noise than ex vivo images because soft tissues increase scattered radiation.
The limitation of the present experiment was eliminating clinical conditions that might impede diagnosis. A clinical study design would yield more realistic results, but the challenge in clinical studies is to obtain a meaningful validation gold standard for the radiographic findings. In addition, using teeth with natural caries might mimic the clinical situation more closely than obvious cavities produced chemically. The present study assessed the diagnostic ability of CBCT for proximal caries detection only in teeth adjacent to the restorations. Further studies should be performed to assess the rest of teeth in the dental arch.
Conclusion
Beam hardening artifacts produced by amalgam fillings compromise caries detection ability in the mesial and distal surfaces of adjacent teeth by CBCT. Zirconia crowns only decrease caries detection ability in the mesial surfaces of the adjacent teeth by CBCT. Otherwise, CBCT is a highly valid examination technique for proximal caries detection in absence of any restoration as well as in teeth close to composite, RMGIC fillings, and lithium disilicate crown.
References
Listl S, Galloway J, Mossey PA, Marcenes W (2015) Global economic impact of dental diseases. J Dent Res 94:1355–1361
Young DA, Featherstone JD (2005) Digital imaging fiber-optic trans-illumination, F-speed radiographic film and depth of approximal lesions. J Am Dent Assoc 136:1682–1687
Bader JD, Shugars DA, Bonito AJ (2001) Systematic reviews of selected dental caries diagnostic and management methods. J Dent Educ 65:960–968
Wenzel A, Hirsch E, Christensen J, Matzen LH, Scaf G et al (2013) Detection of cavitated approximal surfaces using cone beam CT and intraoral receptors. Dentomaxillofac Radiol 42:39458105
Sansare K, Singh D, Sontakke S, Karjodkar F, Saxena V et al (2014) Should cavitation in proximal surfaces be reported in cone beam computed tomography examination? Caries Res 48:208–213
Gaalaas L, Tyndall D, Mol A, Everett ET, Bangdiwala A (2016) Ex vivo evaluation of new 2D and 3D dental radiographic technology for detecting caries. Dentomaxillofac Radiol 45:20150281
Kayipmaz S, Sezgin OS, Saricaoglu ST, Can G (2011) An in vitro comparison of diagnostic abilities of conventional radiography, storage phosphor, and cone beam computed tomography to determine occlusal and approximal caries. Eur J Radiol 80:478–482
Senel B, Kamburoglu K, Ucok O, Yuksel SP, Ozen T et al (2010) Diagnostic accuracy of different imaging modalities in detection of proximal caries. Dentomaxillofac Radiol 39:501–511
Zhang ZL, Qu XM, Li G, Zhang ZY, Ma XC (2011) The detection accuracies for proximal caries by cone-beam computerized tomography, film, and phosphor plates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:103–108
Krzyzostaniak J, Kulczyk T, Czarnecka B, Surdacka A (2015) A comparative study of the diagnostic accuracy of cone beam computed tomography and intraoral radiographic modalities for the detection of noncavitated caries. Clin Oral Investig 19:667–672
Safi Y, Shamloo Mahmoudi N, Aghdasi MM, Eslami Manouchehri M, Rahimian R et al (2015) Diagnostic accuracy of cone beam computed tomography, conventional and digital radiographs in detecting interproximal caries. J Med Life 8:77–82
Ergucu Z, Turkun LS, Onem E, Guneri P (2010) Comparative radiopacity of six flowable resin composites. Oper Dent 35:436–440
Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E et al (2011) Artefacts in CBCT: a review. Dentomaxillofac Radiol 40:265–273
Draenert FG, Coppenrath E, Herzog P, Muller S, Mueller-Lisse UG (2007) Beam hardening artefacts occur in dental implant scans with the NewTom cone beam CT but not with the dental 4-row multidetector CT. Dentomaxillofac Radiol 36:198–203
Cebe F, Aktan AM, Ozsevik AS, Ciftci ME, Surmelioglu HD (2017) The effects of different restorative materials on the detection of approximal caries in cone-beam computed tomography scans with and without metal artifact reduction mode. Oral Surgery Oral Medicine Oral Pathology Oral Radiology 123:392–400
Kulczyk T, Konwinska MD, Owecka M, Krzyzostaniak J, Surdacka A (2014) The influence of amalgam fillings on the detection of approximal caries by cone beam CT: in vitro study. Dentomaxillofacial Radiology 43:6
Martinez-Rus F, Garcia AM, de Aza AH, Pradies G (2011) Radiopacity of zirconia-based all-ceramic crown systems. Int J Prosthodont 24:144–146
Murat S, Kamburoglu K, Isayev A, Kursun S, Yuksel S (2013) Visibility of artificial buccal recurrent caries under restorations using different radiographic techniques. Oper Dent 38:197–207
Charuakkra A, Prapayasatok S, Janhom A, Pongsiriwet S, Verochana K et al (2011) Diagnostic performance of cone-beam computed tomography on detection of mechanically-created artificial secondary caries. Imaging Sci Dent 41:143–150
Sousa Melo SL, Belem MDF, Prieto LT, Tabchoury CPM, Haiter-Neto F (2017) Comparison of cone beam computed tomography and digital intraoral radiography performance in the detection of artificially induced recurrent caries-like lesions. Oral Surg Oral Med Oral Pathol Oral Radiol 124:306–314
Baltacioglu IH, Eren H, Yavuz Y, Kamburoglu K (2016) Diagnostic accuracy of different display types in detection of recurrent caries under restorations by using CBCT. Dentomaxillofac Radiol 45:20160099
Aglarci OS, Bilgin MS, Erdem A, Ertas ET (2015) Is it possible to diagnose caries under fixed partial dentures with cone beam computed tomography? Oral Surg Oral Med Oral Pathol Oral Radiol 119:579–583
Abu El-Ela WH, Farid MM, Mostafa MS (2016) Intraoral versus extraoral bitewing radiography in detection of enamel proximal caries: an ex vivo study. Dentomaxillofac Radiol 45:20150326
Pitts NB (1984) Systems for grading approximal carious lesions and overlaps diagnosed from bitewing radiographs. Proposals for future standardization. Community Dent Oral Epidemiol 12:114–122
Russell M, Pitts NB (1993) Radiovisiographic diagnosis of dental caries: initial comparison of basic mode videoprints with bitewing radiography. Caries Res 27:65–70
SEDENTEXCT (2012) Guideline Development Panel. Radiation protection No 172. Cone beam CT for dental and maxillofacial radiology. Evidence based guidelines Luxembourg: European Commission Directorate-General for Energy
Grossman ES, Matejka JM (1999) Histological features of artificial secondary caries adjacent to amalgam restorations. J Oral Rehabil 26:737–744
Tohnak S, Mehnert AJ, Mahoney M, Crozier S (2011) Dental CT metal artefact reduction based on sequential substitution. Dentomaxillofac Radiol 40:184–190
Belem MDF, Tabchoury CPM, Ferreira-Santos RI, Groppo FC, Haiter-Neto F (2013) Performance of a photostimulable storage phosphor digital system with or without the sharpen filter and cone beam CT for detecting approximal enamel subsurface demineralization. Dentomaxillofacial Radiology 42:9
[3M ESPE] (2011) Filtek™ Z550 Nano Hybrid Universal Restorative, Technical Data Sheet. Retrieved from http://www.3MESPE.com.
Tyndall DA, Rathore S (2008) Cone-beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am 52:825–841
Rathore S, Tyndall D, Wright J, Everett E (2012) Ex vivo comparison of Galileos cone beam CT and intraoral radiographs in detecting occlusal caries. Dentomaxillofacial Radiology 41:489–493
Funding
The work was supported by the Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Ain Shams University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors. This ex vivo study was expedited from review by Ain Shams University Faculty of Dentistry Ethics Committee.
Conflict of interest
The authors declare no competing interest.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abu El-Ela, W.H., Farid, M.M. & Abou El-Fotouh, M. The impact of different dental restorations on detection of proximal caries by cone beam computed tomography. Clin Oral Invest 26, 2413–2420 (2022). https://doi.org/10.1007/s00784-021-04207-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04207-w