Abstract
Objectives
This study aimed to compare the effects of Passiflora incarnata, Erythrina mulungu, and midazolam in controlling anxiety in patients undergoing mandibular third molar extraction.
Methods
The volunteers underwent extraction of their third mandibular molars in a randomized, placebo-controlled, triple-blind, and parallel clinical trial. Passiflora incarnata (500 mg), Erythrina mulungu (500 mg), or midazolam (15 mg) was orally administered 60 min before the surgery. The anxiety level of participants was evaluated using questionnaires and measurements of physical parameters, including heart rate (HR), blood pressure (BP), and oxygen saturation (SpO2).
Results
A total of 200 volunteers were included in this clinical trial. Considering each procedure independently, no significant differences (p > 0.05) in BP, HR, and SpO2 were observed among the protocols.
Conclusions
Passiflora incarnata showed a similar effect to midazolam but differed from placebo and mulungu, which were unable to control anxiety in this situation. Therefore, the results suggest that Passiflora configures an herbal medicine with an anxiolytic effect, adequate to use in third molar extractions.
Clinical relevance
The use of Passiflora incarnata may be an alternative to benzodiazepines for controlling anxiety in patients scheduled for oral surgery under local anesthesia.
Trial registration
ClinicalTrials.gov: ANSI-388.427
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite scientific and technological advances and the improvement of techniques in dentistry to achieve pain control, dental treatment is still a reason for anxiety [1]. Anxiety can manifest as agitated behavior and changes in physical parameters. Nevertheless, calm patients may also experience anxiety during dental procedures, causing delay or even discontinuation of treatment, thereby compromising patients’ oral health and quality of life [2].
There are several pharmacological and non-pharmacological interventions for anxiety control. When non-pharmacological approaches are insufficient, sedation techniques can be used to decrease anxiety [2]. This technique is termed minimal sedation and defined by the American Dental Association as the “minimally depressed level of consciousness allowing the patient to keep his or her airway functioning independently and to respond to physical stimulation and verbal commands” [3].
Oral benzodiazepines are the most commonly used drugs by dentists to achieve minimal oral sedation owing to its ease of administration and a large margin of clinical safety [4]. As benzodiazepines are allosteric GABA-A receptor modulators, the GABA neurotransmitter should be present for the benzodiazepine effects to occur [5].
Owing to its satisfactory performance, midazolam has been used as the drug of choice in standard protocols in a few studies [6,7,8]. However, the associated side effects, such as anterograde amnesia, paradoxical reaction, and somnolence, as well as patient recommendations to bring an attender along for appointments and restrictions on operating vehicles or hazardous machinery until the drug effects cease [3, 4] have encouraged studies for new protocols for minimal sedation in the dental office [5,6,7,8,9].
The preference for herbal medicines for dental sedation is increasing [10,11,12]. Studies in countries like Brazil have demonstrated their cost-effectiveness and lower risk of side effects, along with the ease of prescription in comparison with benzodiazepines [13, 14]. Thus, sustaining their use as an alternative to benzodiazepines has been corroborated [5].
Passiflora incarnata (P. incarnata) is a plant that belongs to the Passifloraceae family used in traditional medicine for the treatment of anxiety and sleep disorders [13]. P. incarnata has also been investigated as an oral anxiolytic premedication for surgeries and demonstrated reduced anxiety without inducing sedation in outpatients [14]. The bark and seeds of another Brazilian native plant, Erythrina mulungu (E. mulungu), is used in folk medicine due to its anticonvulsant, analgesic, sedative, hypnotic, and hypotensive properties [15, 16]. E. mulungu also showed an anxiolytic effect without significant changes in the physiological parameters of adult patients undergoing third mandibular molar surgery [8].
The safety and efficacy of herbal medicines are frequently challenged by practitioners. Although this is an encouraging line of research, currently, only two published randomized clinical trials [5, 8] have reported the anxiolytic effects of P. incarnata and E. mulungu on the extraction of impacted third molars. Studies comparing midazolam with the two herbal medicines are lacking. Thus, this study aimed to assess the efficacy of E. mulungu, P. incarnata, and midazolam in controlling anxiety in patients undergoing third mandibular molar extraction.
Material and methods
Study design
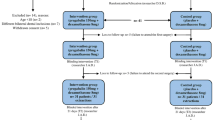
This controlled, randomized, triple-blind, parallel study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Federal University of Sergipe (protocol CAAE number 19602613.1.0000.5546) registered by ClinicalTrials.gov (ANSI-388.427). The CONSORT (consolidated standards of reporting trials) guidelines were followed for publication. This study was performed at the Department of Dentistry of the Federal University of Sergipe in Aracaju, Sergipe, Brazil. The data was collected between July 2013 and August 2014. The materials and methods used in the current study were based on the clinical trials published by Dantas et al. [5] and Silveira-Souto et al. [8].
Sample selection
The inclusion criteria were patients aged over 18 years, absence of systemic disease (ASA I), presenting asymptomatic impacted third mandibular molars, and similar difficulties classified as class II-B [17].
All participants were informed of both the risks and benefits of the study before signing an informed consent form. Exclusion criteria were history of pericoronitis or other inflammatory/infectious diseases at the time of surgery; any medication used within 15 days of study initiation, history of hypersensitivity to drugs, substances, or materials used in this experiment, and pregnancy or lactation.
The sample comprised 200 patients who required the extraction of an impacted third mandibular molar tooth. After anamnesis and an initial clinical examination, no patients were excluded from the sample and were allocated for intervention (n = 50), distributed as four groups.
Blinding and randomization
Volunteers randomly received either 15 mg of midazolam (two 7.5-mg capsules), 500 mg of P. incarnata (two 250-mg capsules), 500 mg of E. mulungu (two 250-mg capsules, Matusa®), or placebo (starch, two capsules). All the capsules were equal in size and shape and were orally administered once 1 h before the surgical procedures. Drugs were coded as “protocol 1,” “protocol 2,” “protocol 3,” or “protocol 4” and administered to volunteers by one of the researchers. Randomization was conducted by a collaborator who was not involved in the anxiety assessment through the Random Number Generator Pro 2.15 software.
To control postoperative edema and trismus, a single dose of intramuscular dexamethasone (8 mg) was administered to all the study volunteers, 30 min before surgery [5]. The patients underwent intraoral antisepsis using 0.12% chlorhexidine digluconate and extraoral antisepsis using 2% chlorhexidine digluconate, followed by placement of surgical drapes for delimitation of the contamination area.
Surgical procedure
Local anesthesia was induced using the Vazirani-Akinosi mandibular nerve block technique, to ensure effective anesthesia of the inferior alveolar nerve block regardless of any anatomical variations [18]. For completion of local anesthesia, one cartridge (1.8 mL) of 2% lidocaine with epinephrine 1:100,000 and 0.9 mL of articaine (4%) with epinephrine 1:100,000 were used for the buccal nerve block [19]. Surgical procedures were performed in one session, by a single operator, using the surgical technique previously described [20].
Patients were instructed regarding local hemostatic care, feeding, cleaning the operated region, restriction of physical exertion, and other routine recommendations. The volunteers also received four tablets of paracetamol (750 mg) with an instruction to consume one tablet every 6 h only when they experienced pain.
Assessment of anxiety
The anxiety levels in the volunteers were assessed through questionnaires and physical parameters. The procedures were divided into three phases: phase I (baseline), phase II (day of surgery), and phase III (return visit) [8].
-
Phase I—Baseline: The Modified Corah Dental Anxiety Scale in the Portuguese language was adapted and used during the initial consultation that occurred within 1 week before the scheduled first intervention [21]. This scale consisted of a questionnaire with four questions, each with five possible answers, evaluating the feelings, signs, and reactions of the volunteers related to dental treatment. Each response was scored on a 5-point scale and the patients were ultimately classified based on the total number of points as calm, moderately anxious, and very anxious.
-
Phase II—The day of surgery: The anxiety level of the subjects was classified by both the researcher and the operator who were responsible for the surgery. The anxiety categories were calm, moderately anxious, and very anxious.
-
Phase III—Return visit: After each surgical procedure, the volunteers received the same Corah Dental Anxiety Scale from baseline, to report their responses on the following day post-surgery.
Assessment of physical parameters
The patients remained at rest for 15 min before the first recording of the physical parameters, following which the blood pressure (BP) was assessed using a wrist monitor (Techline®, São Paulo, SP, Brazil). The heart rate (HR) and blood oxygen saturation (SpO2) were measured using a digital pulse oximeter (More Fitness, São Paulo, SP, Brazil). These values were recorded before drug administration, 30 min after drug administration, and during surgery at the time of local anesthesia administration, incision, tooth removal, and suturing. All measurements were made by the same researcher with a properly calibrated apparatus and served as baseline data for the physical parameters used to evaluate anxiety.
Sample size
A sample-based calculation indicated that 42 volunteers were required for a 90% chance of detecting 60% of sedation effectiveness (when the previous anxiety level was decreased) for midazolam and at least 30% for the other groups at a significance level of 5%. The overall sample comprised 200 volunteers.
Statistical analysis
The proportions of sex, previous anxiety level, and the reduction in anxiety level induced by treatment were compared between groups by the chi-square test (or Fisher’s exact test when necessary). Age, diastolic and systolic blood pressure, SpO2, and heart rate were compared using the Kruskal-Wallis (Dunn) test. The significance level was set at 5%.
Results
There were 200 volunteers, 131 women with a mean age of 24.3 (± 5.3) years and 69 men with a mean age of 25 (± 6.5) years. No differences were noted between different age groups (Kruskal-Wallis, p = 0.5684) and gender (chi-square, p = 0.9703).
Figure 1 presents charts a, b, and c showing the blood pressure (BP), heart rate (HR), and oxygen saturation (SpO2) respectively. No differences were observed in the systolic and diastolic blood pressure, HR, or SpO2 between the groups (Kruskal-Wallis, p > 0.05). However, the heart rate increased (Kruskal-Wallis, p < 0.05) during anesthesia in all groups, but decreased afterward.
Table 1 shows the distribution of patients based on the anxiety level perceived by the operator, the investigator, and the patient. There were no differences in the basal anxiety levels between treatment groups (p = 0.64). The concordance rate between the operator and investigator was 100% for midazolam and E. mulungu, 98% for P. incarnata, and 96% for placebo. The concordance rate between the investigator and the patient was 90% for midazolam, 92% for P. incarnata, 54% for E. mulungu, and 56% for placebo. The investigator also showed a trend of assessing the level of anxiety as “calm” when the patient was “moderately anxious.” Meanwhile, concordance rates of 90% and 94% were also observed between the patient and operator for the midazolam and P. incarnata groups, respectively. However, the concordance rate was similar to that found between the investigator and the patient for E. mulungu and placebo groups, which was 54% and 56%, respectively.
Table 2 compares the baseline of patients’ anxiety perception with the assessed anxiety level one day after surgery. Patients who used midazolam and P. incarnata showed lower (chi-square, p < 0.0001) levels of anxiety than those who used a placebo and E. mulungu. However, there were no differences between E. mulungu and placebo (p = 0.1585) nor between midazolam and P. incarnata (p = 0.7946). Moreover, Table 3 shows that there was a minor improvement in anxiety when E. mulungu was used when compared with that of the other treatments. More volunteers also reported worsened anxiety with E. mulungu or placebo (p < 0.0001) than with midazolam or P. incarnata. Nevertheless, there were no differences between the groups (p = 0.31) regarding improvement in anxiety.
Discussion
Oral surgery performed under local anesthesia is a routine dental procedure, which can cause a greater increase in anxiety levels compared with other dental procedures [22]. Anxiety triggers neurophysiological interactions causing changes in the respiratory rate, blood pressure, and heart rate due to the release of endogenous catecholamines [23]. Therefore, anxiety control may help maintain the stability of these parameters and can also support dentists in the development of oral treatments and maintenance of oral health [24].
Benzodiazepines are often used in dentistry to control anxiety. They act by binding to “benzodiazepine receptors” located between the α and ɣ subunits of the GABA-A receptor and modulate the action of GABA neurotransmitter, thus increasing the frequency of chloride ion channel opening. The increase of the GABA inhibitory effect on neuronal excitability in the limbic system, thalamus, and hypothalamus causes a decrease in anxiety [25].
Passiflora is also used as an anxiolytic, but its mechanism of action is still under investigation. It is believed that inhibition of the monoamine oxidase (MAO) receptor and the activation of the GABA receptor are involved in this process [25, 26]. MAO is responsible for degrading monoamines (adrenaline, tyramine, dopamine, and serotonin), and thus its inhibition increases the concentration of these monoamines in the brain.
The mechanism of action of E. mulungu is still undefined. However, neurochemical tests in animal models showed that one of the main anxiolytic alkaloids present in E. mulungu does not act on GABA pathways [16, 27]. However, an extract of Erythrina vespertilio may act on serotonergic 5HT3 receptors [27].
Despite the differences in mechanisms of action, no differences related to physical parameters were observed among the four protocols in this study, including the placebo. The herbal medicines studied here need further exploration. Nevertheless, the physical parameters were similar in comparison with those with midazolam.
The placebo group presented no detectable changes, which is interesting, since anxiety can affect physical parameters [23]. It may be related to the fact that in most volunteers, the anxiety levels at the end of the procedure remained the same as that during the initial assessment. Thus, it could influence the maintenance of the physical parameters independent of the effect of the medications administered. However, the placebo effect, despite not controlling anxiety, may have influenced the maintenance of the stability of the physical parameters. This finding corroborates with what is in a previous study [8].
Nevertheless, there was an increase in heart rate during anesthesia in all groups. Local anesthesia is considered to be one of the most apprehensive procedures in dental treatment [28,29,30] and could lead to a momentary worsening of the anxiety profile. Therefore, fear and increase of anxiety can lead to momentaneous fluctuations of endogenous catecholamines [28] resulting in an increase in heart rate in all groups. However, the fluctuations did not exceed physiologically significant values and decreased at the time of suturing, maintaining the heart rate at an acceptable range.
The safety of sedation in dentistry is associated with maintenance of heart rate, blood pressure, and SpO2 saturation. Owing to ignorance, many clinicians, mostly in developing countries such as Brazil, do not use a minimal sedation protocol [31]. The baseless associated respiratory depression side effects [6] could be a deterrence. However, in the present study, none of the medications used caused a considerable decrease in the SpO2 saturation levels, showing that they did not differ from the placebo. Similar findings were reported earlier when comparisons were made between Passiflora and midazolam or E. mulungu and placebo [5, 8].
Although all protocols in this study were safe, based on the examined vital signs, there were differences in the sedation efficacy between the groups. These results confirmed the effect of midazolam and Passiflora to control anxiety in third molar extractions, unlike E. mulungu. Thus, our results do not corroborate the success of E. mulungu in this procedure [8] since it did not differ from that of the placebo.
Our results were obtained and evaluated for uniformity of opinion between the patient, researcher, and operator. Midazolam was associated with better levels of anxiety and a better reduction in the level from the first evaluation to the last, with Passiflora showing similar results. Moreover, they were different from the results in the placebo group, which was not the case in the mulungu group. This was in disagreement with the finding reported by Silveira-Souto et al. [8].
Our results can be justified as the mechanism of action of Passiflora is possibly similar to that of benzodiazepines, which acts by modulating the GABA system [32]. However, the mechanism of action of mulungu is complex owing to the multiple alkaloid components and is not directly related to the GABA system alone. Additionally, its alkaloids have anticonvulsant activity, with mild anxiolytic activity [16]. Thus, the anxiolytic effect of Passiflora and the lesser anxiolytic effect of mulungu in this study are justified.
The study design could also contrast the previous results of mulungu reported in the literature [8]. Although it was a crossover study in which the patients received both mulungu and placebo, the patients were compared based on the effects of mulungu and placebo, which could have led to exacerbated differences. This type of misconception can be related to the placebo used as a control group when effective drugs are already available. Otherwise, it can be configured as an α error, related to a small sample size.
Considering the present study and previous literature results [5], Passiflora is a promising herbal anxiolytic medicine that can be used in dentistry. Moreover, in countries like Brazil, there are governmental guidelines on prescribing benzodiazepines and its prescription is controlled by a national organization, making its dental use difficult. Additionally, the search for herbal medicines treatments is growing. If herbal medicines are further explored and well established in the literature, dentists can offer individualized safe treatments to patients. Therefore, further studies on herbal medicines can also help controlling anxiety when benzodiazepines cannot be prescribed by professionals.
This study found promising results as it demonstrated that an herbal medicine, Passiflora incarnata, achieved sedation levels similar to the standard protocol with midazolam, a benzodiazepine. However, as is the case in scientific research, it also raised a few questions. One of the questions or limitations of this study was that the incidence of anterograde amnesia and other side effects were not assessed. Future trials should also be conducted to explore the pharmacokinetic properties of the herbal medicines studied here. Future clinical trials may establish greater safety and characterize the use of these drugs for minimal sedation in dental care procedures.
Conclusion
P. incarnata proved to be an option for controlling anxiety in third molar extraction surgeries. It showed a similar effect to midazolam and differed from placebo and mulungu, which could not control anxiety. Therefore, similar to midazolam, Passiflora has an anxiolytic effect that can be used in third molar extractions.
References
Possobon R d F, Carrascoza KC, de Moraes ABA, Costa ÁL (2007) Dental treatment as a cause of anxiety. Psicol Estud 12:609–616. https://doi.org/10.1590/S1413-73722007000300018
Gordon D, Heimberg RG, Tellez M, Ismail AI (2013) A critical review of approaches to the treatment of dental anxiety in adults. J Anxiety Disord 27:365–378. https://doi.org/10.1016/j.janxdis.2013.04.002
Mancuso CE, Tanzi MG, Gabay M (2004) Paradoxical reactions to benzodiazepines: literature review and treatment options. Pharmacotherapy 24:1177–1185. https://doi.org/10.1592/phco.24.13.1177.38089
Sebastiani FR, Dym H, Wolf J (2016) Oral sedation in the dental office. Dent Clin N Am 60:295–307. https://doi.org/10.1016/j.cden.2015.11.002
Dantas L-P, de Oliveira-Ribeiro A, de Almeida-Souza L-M, Groppo F-C (2017) Effects of Passiflora incarnata and midazolam for control of anxiety in patients undergoing dental extraction. Med Oral Patol Oral Cir Bucal 22:e95–e101. https://doi.org/10.4317/medoral.21140
de Moares MB, Barbier WS, Raldi FV et al (2019) Comparison of three anxiety management protocols for extraction of third molars with the use of midazolam, diazepam, and nitrous oxide: a randomized clinical trial. J Oral Maxillofac Surg 77:2258.e1–2258.e8. https://doi.org/10.1016/j.joms.2019.06.001
Dellovo AG, Souza LMA, de Oliveira JS, Amorim KS, Groppo FC (2018) Effects of auriculotherapy and midazolam for anxiety control in patients submitted to third molar extraction. Int J Oral Maxillofac Surg 48:669–674. https://doi.org/10.1016/j.ijom.2018.10.014
Silveira-Souto ML, São-Mateus CR, de Almeida-Souza LM, Groppo FC (2014) Effect of Erythrina mulungu on anxiety during extraction of third molars. Med Oral Patol Oral Cir Bucal 19:e518–e524. https://doi.org/10.4317/medoral.19511
Michalek-Sauberer A, Gusenleitner E, Gleiss A, Tepper G, Deusch E (2012) Auricular acupuncture effectively reduces state anxiety before dental treatment-a randomised controlled trial. Clin Oral Investig 16:1517–1522. https://doi.org/10.1007/s00784-011-0662-4
Zahn R, Perry N, Perry E, Mukaetova-Ladinska EB (2019) Use of herbal medicines: pilot survey of UK users’ views. Complement Ther Med 44:83–90. https://doi.org/10.1016/j.ctim.2019.02.007
Sarris J (2018) Herbal medicines in the treatment of psychiatric disorders: 10-year updated review. Phyther Res 32:1147–1162. https://doi.org/10.1002/ptr.6055
Yeung KS, Hernandez M, Mao JJ, Haviland I, Gubili J (2018) Herbal medicine for depression and anxiety: a systematic review with assessment of potential psycho-oncologic relevance. Phytother Res 32:865–891. https://doi.org/10.1002/ptr.6033
Villet S, Vacher V, Colas A, Danno K, Masson JL, Marijnen P, Bordet MF (2016) Open-label observational study of the homeopathic medicine Passiflora Compose for anxiety and sleep disorders. Homeopathy 105:84–91. https://doi.org/10.1016/j.homp.2015.07.002
Movafegh A, Alizadeh R, Hajimohamadi F, Esfehani F, Nejatfar M (2008) Preoperative oral Passiflora incarnata reduces anxiety in ambulatory surgery patients: a double-blind, placebo-controlled study. Anesth Analg 106:1728–1732. https://doi.org/10.1213/ane.0b013e318172c3f9
Vasconcelos SMM, Rebouças Oliveira G, Mohana de Carvalho M, Rodrigues ACP, Rocha Silveira E, Maria França Fonteles M, Florenço Sousa FC, Barros Viana GS (2003) Antinociceptive activities of the hydroalcoholic extracts from Erythrina velutina and Erythrina mulungu in mice. Biol Pharm Bull 26:946–949. https://doi.org/10.1248/bpb.26.946
Santos Rosa D, Faggion SA, Gavin AS, Anderson de Souza M, Fachim HA, Ferreira dos Santos W, Soares Pereira AM, Cunha AOS, Beleboni RO (2012) Erysothrine, an alkaloid extracted from flowers of Erythrina mulungu Mart. ex Benth: evaluating its anticonvulsant and anxiolytic potential. Epilepsy Behav 23:205–212. https://doi.org/10.1016/j.yebeh.2012.01.003
Pell GJ, Gregory GT (1933) Impacted mandibular third molars: classification and modified techniques for removal. Dent Dig 39:330–338
Haas DA (2011) Alternative mandibular nerve block techniques. J Am Dent Assoc 142:8S–12S. https://doi.org/10.14219/jada.archive.2011.0341
Da Silva-Junior GP, De Almeida Souza LM, Groppo FC (2017) Comparison of articaine and lidocaine for buccal infiltration after inferior alveolar nerve block for intraoperative pain control during impacted mandibular third molar surgery. Anesth Prog 64:80–84. https://doi.org/10.2344/anpr-64-02-06
Jansma J, Schoen PJ, Raghoebar GM, Vissink A (2004) Dentoalveolar surgery for the dentist: removal of teeth and root tips. Ned Tijdschr Tandheelkd 111:128–132
Hu LW, Gorenstein C, Fuentes D (2007) Portuguese version of Corah’s Dental Anxiety Scale: transcultural adaptation and reliability analysis. Depress Anxiety 24:467–471. https://doi.org/10.1002/da.20258
Glaesmer H, Geupel H, Haak R (2015) A controlled trial on the effect of hypnosis on dental anxiety in tooth removal patients. Patient Educ Couns 98:1112–1115. https://doi.org/10.1016/j.pec.2015.05.007
Malamed SF (2006) Sedation and safety: 36 years of perspective. Alpha Omegan 99:70–74. https://doi.org/10.1016/j.aodf.2006.06.008
Guentsch A, Stier C, Raschke GF, Peisker A, Fahmy MD, Kuepper H, Schueler I (2017) Oral health and dental anxiety in a German practice-based sample. Clin Oral Investig 21:1675–1680. https://doi.org/10.1007/s00784-016-1951-8
Campo-Soria C, Chang Y, Weiss DS (2009) Mechanism of action of benzodiazepines on GABAA receptors. Br J Pharmacol 148:984–990. https://doi.org/10.1038/sj.bjp.0706796
Kinrys G, Coleman E, Rothstein E (2009) Natural remedies for anxiety disorders: potential use and clinical applications. Depress Anxiety 26:259–265. https://doi.org/10.1002/da.20460
Flausino OA, Pereira AM, Bolzani VDS, Nunes-De-Souza RL (2007) Effects of erythrinian alkaloids isolated from Erythrina mulungu (Papilionaceae) in mice submitted to animal models of anxiety. Biol Pharm Bull 30:375–378. https://doi.org/10.1248/bpb.30.375
Armfield JM, Milgrom P (2011) A clinician guide to patients afraid of dental injections and numbness. SAAD Dig 27:33–39
Ujaoney S, Mamtani M, Thakre T, Tote J, Hazarey V, Hazarey P, Kulkarni H (2013) Efficacy trial of camouflage syringe to reduce dental fear and anxiety. Eur J Paediatr Dent 14:273–278
Vanhee T, Mourali S, Bottenberg P et al (2019) Stimuli involved in dental anxiety: what are patients afraid of?: A descriptive study. Int J Paediatr Dent. https://doi.org/10.1111/ipd.12595
Lino PA, Martins MAP, Silva ME d S e, de Abreu MHNG (2017) Anxiolytics, Sedatives, and hypnotics prescribed by dentists in Brazil in 2010. Biomed Res Int 2017:1–5. https://doi.org/10.1155/2017/2841549
Appel K, Rose T, Fiebich B, Kammler T, Hoffmann C, Weiss G (2011) Modulation of the γ-aminobutyric acid (GABA) system by Passiflora incarnata L. Phytother Res 25:838–843. https://doi.org/10.1002/ptr.3352
Acknowledgments
The corresponding author acknowledges the Department of Dentistry of the Federal University of Sergipe.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Rafael Soares da Cunha, Klinger de Souza Amorim, and Anne Caroline Gercina. The first draft of the manuscript was written by Rafael Soares da Cunha, Allan Carlos Araújo de Oliveira, and Liciane dos Santos Menezes. Conceptualization: Klinger de Souza Amorim and Liane Maciel de Almeida Souza. Methodology: Francisco Carlos Groppo and Liane Maciel de Almeida Souza. Formal analysis: Francisco Carlos Groppo. Investigation: Rafael Soares da Cunha. Writing—original draft preparation: Anne Caroline Gercina and Klinger de Souza Amorim. Writing—review and editing: Anne Caroline Gercina and Klinger de Souza Amorim. Supervision: Liane Maciel de Almeida Souza. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This clinical trial was approved by the Sergipe Federal University Human Health Research Ethics Committee (CAAE: 19602613.1.0000.5546); additionally, it was submitted to ClinicalTrials.gov (ANSI-388.427).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Cunha, R.S., Amorim, K.S., Gercina, A.C. et al. Herbal medicines as anxiolytics prior to third molar surgical extraction. A randomized controlled clinical trial. Clin Oral Invest 25, 1579–1586 (2021). https://doi.org/10.1007/s00784-020-03468-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03468-1