Abstract
Objectives
The study aimed at assessing, as primary objective, the periapical status and quality of root fillings, and, as secondary objective, the endodontic treatment need of a German urban population in a cross-sectional study 20 years after the first one.
Materials and methods
Clinical and radiographic data of 353 patients were evaluated. Descriptive and regression analyses were performed and the endodontic treatment need was calculated. Results were compared with data from the year 1993.
Results
A total of 9269 teeth were examined (26.2 teeth per patient; 1993, 24.4), of which 337 teeth were root filled (3.6%; 1993, 2.7%). Prevalence of apical periodontitis in root-filled teeth was 34% (1993, 61%). Quality of root fillings was adequate in 117 cases (35%; 1993, 14%). Minimum endodontic treatment need was estimated with 1.6% (1993, 2.3%), including teeth with clinical symptoms. Considering symptomless teeth with apical periodontitis and poor quality of root filling, the treatment need was 2.9% (1993, 3.7%). Regression analysis identified quality of root filling as a significant factor for periapical health (p = 0.01, odds ratio 3.4×, 95% CI 1.9–6.3×), likewise the type of instrumentation. Teeth treated with rotary files had a significantly better outcome (p = 0.02, odds ratio 2.0×, 95% CI 1.1–3.7×).
Conclusions
Quality of root fillings and the periapical status have improved over the last 20 years in Germany. However, there is still a need for an increase in quality of root canal treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The major goal of endodontology is the treatment and prevention of apical periodontitis [1]. Although preventive dentistry is becoming more and more important nowadays, there is still a high endodontic treatment need mainly due to deep carious lesions, long-standing coronal leakage or as a result of dental trauma. Also, people in many countries are getting older and expect the preservation of their natural teeth [2], which leads to a high prevalence of root-filled teeth in elderly patients [3, 4]. Root-filled teeth are associated with apical periodontitis in many countries [5], but it was also stated that a high technical quality of root filling is more likely to result in healthy periapical conditions [6, 7]. Two studies from Germany reported a very low technical quality of root fillings in the 1990s [8, 9]. Approximately 60% of root-filled teeth in those two studies showed radiographic signs of apical periodontitis. Although the main principle of cleaning and shaping [10] remains unchanged, endodontology has undergone some tremendous technical developments since then. Flexible nickel-titanium files were introduced to the market [11] in the 1980s and became more and more popular among general dentists. Some years later, rotary instruments were put on the market, leading to faster and superior treatment compared with stainless steel hand files [12,13,14]. Technical progress was also achieved by the use of passive ultrasonic irrigation [15] and by applying dental operating microscopes in endodontic treatment [16], both of which are integral components of the undergraduate curriculum today [17]. However, it remains unclear whether the technical quality of root canal treatment among general dentists has improved on the basis of these developments over the last two decades. Cross-sectional studies investigating similar cohorts of patients at different points in time would help to approach this question, but they are very scarce [18].
The present cross-sectional study refers to the work of Weiger et al. [9], which analysed a cohort of 323 patients in a German city in the year 1993 and which was repeated under similar conditions.
The aim of this investigation was to assess, as primary objective, the periapical status of root-filled teeth and the quality of root fillings, and, as secondary objective, the endodontic treatment need in a repeated cross-sectional study with a comparable study population of the same urban district 20 years later.
Material and Methods
All patients who consulted a general dental practice during regular consultation hours for the first time in the year 2013 or after a period of 5 years without contact with this dental practice were included in this study. The private practice is situated in Stuttgart, a city with about 600,000 inhabitants in the south-western part of Germany. All patients were examined by the owner of the practice, a general dentist with more than 20 years of professional experience. The examiner was briefed beforehand regarding the standardised procedure of the clinical examination.
A total of 353 patients were prospectively examined, 182 of those were females (52%) and 171 males (48%) with a mean age of 37.6 years. Patients were categorised into two groups: group I represented patients, who did not have prior root canal treatment, nor were they in need of; group II contained patients with at least one root canal treatment, or in need of one (Table 1). Table 1 gives also a detailed age distribution; patients under 12 years were excluded. The total number of teeth, which were clinically and radiographically inspected, was 9269 (mean = 26.25 per patient). The ethical approval was obtained by the local Research Ethics Committee (Nr. 412/2013 D) and participants gave informed consent.
Clinical and radiographic examination
The dental examination of each patient followed a standardised protocol. It included clinical signs and symptoms indicating symptomatic pulpitis or an endodontically induced periapical periodontitis, tooth sensitivity, potential causes for pulpal involvement and type and quality of coronal restoration (Table 2). Margins of restorations from patients of group II were checked visually and tactile using a dental probe. In the presence of carious lesions, over- and undercontoured margins as well as fractured and mobile restorations, restorations were rated as insufficient.
The patients were asked when and why the restorations or endodontic treatments were performed. In case of an existing root filling, the patient was asked whether the dentist had used rotary or hand files. The difference between manual and rotary instrumentation was carefully explained and demonstrated to the patient before.
The dental record was performed using a dental loupe with ×3.5 magnification (Zeiss, Oberkochen, Germany).
It was also recorded whether the patients were smokers or non-smokers and whether they have ever had a dental trauma.
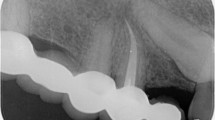
After clinical inspection, a conventional periapical radiograph was taken of all the teeth not responding to the sensitivity test and also of those showing signs or symptoms of irreversible pulpitis. In some patients, a panoramic radiograph had been taken due to various reasons (e.g. periodontitis, wisdom teeth). All periapical radiographs were taken with the same device (TROPHY Radiologie GmbH, Kehl, Germany) using Kodak Insight films (Kodak GmbH, Stuttgart, Germany); the panoramic radiographs were taken with a 10E device (Siemens, Munich, Germany). All films were processed with the XR24 developer (Dürr-Dental, Bietigheim-Bissingen, Germany).
A tooth revealing any kind of radiopaque material in the root canal system was rated as root filled. The quality and the apical extension of the root filling in relation to the radiographic apex, signs of periapical pathosis and the presence of a post were recorded (Table 2). Referring to Weiger et al. [9], the evaluated teeth were categorised into four groups (A–D) according to their endodontic status (Table 3). Table 4 shows the distribution of the teeth according to category and type of radiograph.
Assessment of radiographs
Periapical pathosis was assessed by two operators (MT and TC) using the periapical index score (PAI) [19]. The scoring system was explained beforehand by an experienced endodontist (AE) by means of exemplary radiographs for calibration purposes. Afterwards, the operators evaluated a catalogue of 100 radiographs on their own. This was repeated after 1 and 2 weeks. Agreement with the true scores as well as intra- and interrater agreement was assessed by calculating Cohen’s kappa. Agreement was achieved by a value higher than 0.61.
The PAI scores 1 and 2 were rated as healthy periapical conditions, scores 3, 4 and 5 indicated periapical pathosis. Multi-rooted teeth were categorised according to the root with the highest PAI score.
The calculated minimal need for endodontic treatment included teeth from category B and C. The estimated endodontic treatment need included also teeth of category A with a root canal treatment of poor quality and/or radiographic signs of periapical pathosis.
All radiographs from patients of group II (Table 1) were evaluated independently by the operators (MT and TC) using an illuminated viewing box and a loupe. In case of discrepancies in scoring, a consensus was tried to be established between operators. If no agreement was reached, a third operator (AE) made the final decision.
Statistical analysis
A descriptive analysis regarding the age of patients and root fillings, PAI scores, distribution of tooth type, quality of root fillings and restorations was performed for all categories. Subsequently, regression analysis was performed and the odds ratio of various potential risk factors was calculated in relation to the presence or absence of apical periodontitis as outcome variable. The variables used were quality of root filling (acceptable vs. poor), type of root canal instrumentation (hand vs. rotary files), restoration (sufficient vs. insufficient) and smoking (no vs. yes).
The minimum endodontic treatment need was calculated for all examined teeth. Therefore, the teeth of category B and C were included. The estimated endodontic treatment need was calculated by adding teeth from category A with a PAI 3–5 and teeth associated with an insufficient quality of root filling. The maximum treatment need included teeth with insufficient root fillings, but healthy periapical conditions.
All results obtained from the present study were compared with the results from Weiger et al. (1997).
The overall level of significance was set to α = 0.05. Statistical analysis was performed with JMP 10 software (SAS Institute Inc., Cary, NC, USA).
Results
In this study, 353 patients with a mean age of 37.6 years and a total of 9269 teeth (26.25 teeth per patient; 1993, 24.4) were included. Of those, 146 patients (41.4%) did not have any root-filled teeth nor had they an endodontic treatment need (group I). The number of patients with at least one root-filled tooth or in need of endodontic treatment (group II) consisted of 207 patients (58.6%). Of those, 157 patients had at least one pre-existing root canal treatment (category A, total 337 teeth, 3.6%; 1993, 215 teeth, 2.7%). Category B consisted of 82 teeth (1993, 122 teeth), category C of 69 teeth (1993, 53 teeth) and category D of 32 (1993, 18 teeth).
Five radiographs were missing in category D due to gravidity, another 27 were of unsatisfactory quality. Distribution according to type of teeth in the different categories is specified in Table 5. Maxillary molars were encountered most often with n = 117 (24%) followed by anterior teeth of the maxilla (n = 103; 21.1%). Mandibular front teeth were the exception with only 13 teeth (2.7%).
Of the evaluated participants, 149 patients were smokers (42%) and 204 non-smokers (58%).
Results of PAI score calibration
Cohen’s kappa for comparison of raters with true scores was 0.63 (MT) and 0.83 (TC).
Intrarater scores were 0.76 (MT) and 0.75 (TC), respectively. Interrater agreement was 0.75 (MT vs. TC).
Category A
Table 6 summarises the distribution of the 337 root-filled teeth according to periapical index scores related to quality of root canal treatment, coronal restoration and type of instrumentation. The average of years following primary endodontic treatment until examination was 9.9 years (STD 7.9 years).
In this category, 18 teeth appeared to have had apicoectomy surgery. Eighty-eight teeth (26%) of the root-filled teeth were restored with a post, 80 with a metal post and 8 with a fibre post. Of the 220 teeth recorded with an insufficient quality of root fillings, 156 had voids, 133 were short and 14 too long. One hundred eighty-nine root fillings had an acceptable length of 0–2 mm short of the radiographic apex.
One hundred seventy-nine teeth were restored with an indirect restoration (crown, partial crown bridge, etc.), 41 of which had an insufficient marginal seal and 146 teeth had direct restorations (composite, amalgam, etc.) with almost half of them being insufficient (n = 69). Twelve teeth had no restorations.
Quality of root filling is a statistically significant factor in periapical health (p = 0.01, odds ratio 3.4×), as is type of instrumentation. Teeth treated with rotary files had a significantly better outcome (PAI 1 and 2) (p = 0.02, odds ratio 2.0×). Quality of coronal restoration had no influence on the outcome variable (p = 0.59, odds ratio 1.1). Apical periodontitis in root-filled teeth occurred 1.3 times more likely in smokers than in non-smokers (p = 0.27). Table 7 summarises the results of the regression analysis.
Category B
Category B consisted of 82 teeth (0.88% of 9269 teeth). Mean age of patients in this category was 42 years. Seventy teeth in this category (85%) had a restoration of poor quality. Sixteen teeth were rated as healthy (PAI 1 and 2) and 66 demonstrated clear radiographic signs of apical periodontitis (PAI 3–5).
Category C
Sixty-nine teeth (0.74%) were categorised as C. Only two teeth (3%) had restorations and those were of good quality, the other 67 (97%) had either caries, or missing restorations. Most of these teeth (97%) were associated with a PAI score of 1 or 2; two teeth had a PAI score of 3.
Endodontic treatment need
The minimum endodontic treatment need (teeth from category B + C; n = 151) was 1.6% (1993, 2.3%). When adding symptomless teeth from category A with a PAI score of 3–5 (115 teeth), the estimated endodontic treatment need reached 2.9% (1993, 3.7%). In case that teeth with an insufficient root filling but otherwise healthy periapical conditions (n = 123) were submitted to retreatment, the maximum treatment need was 4.2% (1993, 4.0%). Table 8 summarises the results of the present and the repeated study.
Discussion
This study is a repeated cross-sectional study, which aimed at assessing the periapical status, the quality of root fillings and the endodontic treatment need in an urban German population. It refers to a study, which was performed under almost the same conditions two decades ago with a comparable study population [9]. In both studies, participants were acquired from a general dental practice in the same urban district of Stuttgart, a city with approximately 600,000 inhabitants in the south-western part of Germany. Although this is not a random sample of the German population, the obtained results may be more representative than in other studies dealing with a highly selected patient population from university clinics [8].
Though the conditions were almost similar, results revealed some differences 20 years later. The proportion of root-filled teeth was higher in this study with 3.6% (1997, 2.7%), so was the mean number of teeth per patient (26.2 vs. 24.4). That data indicates that preventive and endodontic treatment is becoming rather popular in Germany. This shift towards more teeth-retaining treatment was also observed in other countries. In a study from the Netherlands from the year 1993, 2.3% of teeth had a root filling [20]; 20 years later, this number was increased to 4.8% [18]. The same observations were made in Spain in 2004, where 2.1% of teeth had experienced root fillings [21] and some years later 6.4% [22]. However, it has to be considered that there are essential methodological differences in these two studies from Spain (panoramic vs. periapical radiographs, population of participants).
The highest prevalence of root-filled teeth was found in Switzerland with 26% according to an earlier investigation [3]. This outcome may be related to the fact that the age of the participants was 66 years consistently.
Prevalence of apical periodontitis and endodontic treatment need
While digital radiographs are common in dental practices nowadays, the present and the study of Weiger et al. used conventional, analogue radiographs. One methodological difference between these two studies, however, was the evaluation of apical pathosis. In 1997, a yes/no decision was made on the assumed existence of an apical periodontitis. In contrast, the periapical index score was applied in the present study, which is more sophisticated and has been used in comparable studies from other countries [21, 23, 24].
Exactly 2% of all examined teeth showed radiological signs of periapical periodontitis (PAI score 3–5), which is lower than it was 20 years ago (3.37%). Root-filled teeth (category A) showed also fewer cases of apical periodontitis. The study of 1997 demonstrated that 61% of the root-filled teeth were associated with apical periodontitis; in the present study, the percentage decreased to 34.1%. The cause for this may be that the percentage of root fillings being rated adequate increased (14.4% vs. 34.7%). Regression analysis revealed that teeth, which were treated with rotary files, had a significantly better periapical status compared with manually instrumented teeth. Participants of the study from 1997 were not asked for type of instrumentation, since it was assumed that almost all root canal treatments in Germany were performed with hand files back then. Although great effort was made to explain and demonstrate the difference between hand files and rotary files to the participants, reliability of participants’ declaration may lack precision.
While some studies reported that the quality of coronal restorations correlates with periapical health, and thus making it even more important than the quality of root fillings [24,25,26,27,28], the results of this work do not verify this assumption. The quality of the restorations had no influence on the outcome of root-filled teeth (p = 0.59, odds ratio 1.1×) in contrast to the quality of root fillings (p < 0.001, odds ratio 3.4), which is in accordance with other studies [29,30,31,32].
It has to be considered that periapical and panoramic radiographs only hint on the sealing capacity of root fillings, due to the two-dimensional character of the images. It is known that cone-beam computed tomography (CBCT) not only allows a more accurate diagnosis of apical periodontitis than periapical radiographs [33], but also differs where the assessment of the quality of root fillings is concerned [34]. Therefore, the results regarding apical periodontitis and quality of root fillings would have been less favourable, if they had been assessed by CBCT. A drawback of this technique is the increased radiation dose [35] compared with conventional radiographs. According to the “ALARA” principle (“as low as reasonably achievable”), the necessity of a CBCT should be carefully considered [36]. For the purpose of this study, benefits from CBCT would not have outweighed potential risks of the increased radiation dose.
The quality of coronal restoration remained more or less unchanged for 20 years (65.6% vs. 63.5%). Highest rate of healthy periapical conditions was seen in teeth with a good quality of root fillings and restorations, which likely had been instrumented with rotary files (PAI 1 and 2 = 92%).
Even though the mean number of teeth per patient increased from 24.4 to 26.2, the minimum endodontic treatment need was lower than 20 years ago (2.3 vs. 1.6%). In contrast, when all root fillings with unsatisfactory quality were taken into account, the maximum endodontic treatment need was higher with 4.2% compared to 4.0%.
Table 8 summarises the results of the present and the repeated study.
An aspect, which was not evaluated in the study of Weiger et al., was the effect of smoking on the prevalence of apical periodontitis. Although there was no statistically significant difference between smokers and non-smokers (p = 0.27), the odds ratio for smokers to have a root-filled tooth with apical periodontitis was 1.3× compared with non-smokers. This is in accordance with other studies dealing with this topic [37,38,39]. Possible reasons for the slightly increased risk are the impairment of the immune system [40] and delayed wound healing [41].
The results of the present study go hand in hand with the results of other countries (Table 9). The percentage of root-filled teeth ranged from 1.6 to 26% (present study, 3.6%). In other studies, the percentage of root-filled teeth with apical periodontitis ranged from 8.5 to 71.9% (present study, 34.1). The overall quality of root fillings (length and density) was 34.7% compared to 11.4–56.9% in other countries. Only a few studies assessed the quality of coronal restorations, but they reported results comparable to the present study.
Certain methodological aspects and limitations inherent to cross-sectional studies ought to be considered. The present study used a different tool to assess the periapical status on conventional radiographs than Weiger et al. Minor differences in the periapical assessment notwithstanding, the use of two-dimensional periapical radiographs ensured quantitative comparability across the two studies, which in turn allowed valuable insights into temporal changes in periapical health and standards of endodontic care at the population level. The diagnostic accuracy of two-dimensional periapical radiographs, however, is inferior to that of CBCT, and studies based on two-dimensional radiographs may therefore slightly underestimate the number of periapical lesions [33, 34]. In addition, healing processes could not be monitored in the present study. Likewise, detecting the development of periapical lesions of teeth that showed no signs or symptoms of apical pathosis at the time of the examination was unfeasible owing to the cross-sectional study design. The results of the present study should therefore be examined in the context of existing and future prospective longitudinal cohort studies that provide more precise information on the development and healing of periapical lesions.
Although the outcome as well as the technical quality of root canal treatment improved over the last two decades, it seems that more effort is still needed to improve undergraduate teaching as well as continuing education in endodontics.
Conclusions
The quality of root fillings and the periapical status have improved over the last 20 years in Germany. However, the technical standard of root canal treatment has to be improved further. Rotary instrumentation and adequate technical quality of root fillings seem to be reliable predictors for periapical health, while the quality of restorations seemed to have only a minor impact.
References
European Society of Endodontology (2006) Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 39:921–930
Johnstone M, Parashos P (2015) Endodontics and the ageing patient. Aust Dent J 60 Suppl 1:20–27
Imfeld TN (1991) Prevalence and quality of endodontic treatment in an elderly urban population of Switzerland. J Endod 17:604–607
Tsuneishi M, Yamamoto T, Yamanaka R, Tamaki N, Sakamoto T, Tsuji K, Watanabe T (2005) Radiographic evaluation of periapical status and prevalence of endodontic treatment in an adult Japanese population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100:631–635
Eriksen HM (1991) Endodontology--epidemiologic considerations. Endod Dent Traumatol 7:189–195
Estrela C, Leles CR, Hollanda AC, Moura MS, Pecora JD (2008) Prevalence and risk factors of apical periodontitis in endodontically treated teeth in a selected population of Brazilian adults. Braz Dent J 19:34–39
Toure B, Kane AW, Sarr M, Ngom CT, Boucher Y (2008) Prevalence and technical quality of root fillings in Dakar, Senegal. Int Endod J 41:41–49
Hülsmann M, Lorch V, Franz B (1991) Studies on the incidence and quality of root fillings. Evaluation by orthopantomograms. Dtsch Zahnarztl Z 46:296–299
Weiger R, Hitzler S, Hermle G, Löst C (1997) Periapical status, quality of root canal fillings and estimated endodontic treatment needs in an urban German population. Endod Dent Traumatol 13:69–74
Schilder H (1974) Cleaning and shaping the root canal. Dent Clin N Am 18:269–296
Walia HM, Brantley WA, Gerstein H (1988) An initial investigation of the bending and torsional properties of Nitinol root canal files. J Endod 14:346–351
Schäfer E, Schulz-Bongert U, Tulus G (2004) Comparison of hand stainless steel and nickel titanium rotary instrumentation: a clinical study. J Endod 30:432–435
Pettiette MT, Delano EO, Trope M (2001) Evaluation of success rate of endodontic treatment performed by students with stainless-steel K-files and nickel-titanium hand files. J Endod 27:124–127
Pettiette MT, Metzger Z, Phillips C, Trope M (1999) Endodontic complications of root canal therapy performed by dental students with stainless-steel K-files and nickel-titanium hand files. J Endod 25:230–234
van der Sluis LW, Versluis M, Wu MK, Wesselink PR (2007) Passive ultrasonic irrigation of the root canal: a review of the literature. Int Endod J 40:415–426
Carr GB (1992) Microscopes in endodontics. J Calif Dent Assoc 20:55–61
Knowles KI, Ibarrola JL, Ludlow MO (1998) The dental operating microscope as an educational tool. J Dent Educ 62:429–431
Peters LB, Lindeboom JA, Elst ME, Wesselink PR (2011) Prevalence of apical periodontitis relative to endodontic treatment in an adult Dutch population: a repeated cross-sectional study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:523–528
Orstavik D, Kerekes K, Eriksen HM (1986) The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 2:20–34
De Cleen MJ, Schuurs AH, Wesselink PR, Wu MK (1993) Periapical status and prevalence of endodontic treatment in an adult Dutch population. Int Endod J 26:112–119
Jimenez-Pinzon A, Segura-Egea JJ, Poyato-Ferrera M, Velasco-Ortega E, Rios-Santos JV (2004) Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. Int Endod J 37:167–173
Lopez-Lopez J, Jane-Salas E, Estrugo-Devesa A, Castellanos-Cosano L, Martin-Gonzalez J, Velasco-Ortega E, Segura-Egea JJ (2012) Frequency and distribution of root-filled teeth and apical periodontitis in an adult population of Barcelona, Spain. Int Endod J 62:40–46
Kirkevang LL, Horsted-Bindslev P, Orstavik D, Wenzel A (2001) Frequency and distribution of endodontically treated teeth and apical periodontitis in an urban Danish population. Int Endod J 34:198–205
Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S (2003) Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J 36:181–192
Ray HA, Trope M (1995) Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 28:12–18
Kirkevang LL, Orstavik D, Horsted-Bindslev P, Wenzel A (2000) Periapical status and quality of root fillings and coronal restorations in a Danish population. Int Endod J 33:509–515
Sidaravicius B, Aleksejuniene J, Eriksen HM (1999) Endodontic treatment and prevalence of apical periodontitis in an adult population of Vilnius, Lithuania. Endod Dent Traumatol 15:210–215
Tavares PB, Bonte E, Boukpessi T, Siqueira JF Jr, Lasfargues JJ (2009) Prevalence of apical periodontitis in root canal-treated teeth from an urban French population: influence of the quality of root canal fillings and coronal restorations. J Endod 35:810–813
Van der Veken D, Curvers F, Fieuws S, Lambrechts P (2017) Prevalence of apical periodontitis and root filled teeth in a Belgian subpopulation found on CBCT images. Int Endod J 50:317–329
Tronstad L, Asbjornsen K, Doving L, Pedersen I, Eriksen HM (2000) Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol 16:218–221
Siqueira JF Jr, Rocas IN, Alves FR, Campos LC (2005) Periradicular status related to the quality of coronal restorations and root canal fillings in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100:369–374
Segura-Egea JJ, Jimenez-Pinzon A, Poyato-Ferrera M, Velasco-Ortega E, Rios-Santos JV (2004) Periapical status and quality of root fillings and coronal restorations in an adult Spanish population. Int Endod J 37:525–530
Uraba S, Ebihara A, Komatsu K, Ohbayashi N, Okiji T (2016) Ability of cone-beam computed tomography to detect periapical lesions that were not detected by periapical radiography: a retrospective assessment according to tooth group. J Endod 42:1186–1190
Liang YH, Li G, Wesselink PR, Wu MK (2011) Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod 37:326–331
Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, Samuelson DB, Scheske MJ (2015) Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol 44:20140197
European Society of Endodontology, Patel S, Durack C, Abella F, Roig M, Shemesh H, Lambrechts P, Lemberg K (2014) European Society of Endodontology position statement: the use of CBCT in endodontics. Int Endod J 47:502–504
Kirkevang LL, Wenzel A (2003) Risk indicators for apical periodontitis. Community Dent Oral Epidemiol 31:59–67
Krall EA, Abreu Sosa C, Garcia C, Nunn ME, Caplan DJ, Garcia RI (2006) Cigarette smoking increases the risk of root canal treatment. J Dent Res 85:313–317
Rodriguez FR, Taner B, Weiger R, Walter C (2013) Is smoking a predictor of apical periodontitis? Clin Oral Investig 17:1947–1955
Ryder MI (2007) The influence of smoking on host responses in periodontal infections. Periodontol 2000 43:267–277
Silverstein P (1992) Smoking and wound healing. Am J Med 93:22S–24S
Eriksen HM, Berset GP, Hansen BF, Bjertness E (1995) Changes in endodontic status 1973-1993 among 35-year-olds in Oslo, Norway. Int Endod J 28:129–132
Marques MD, Moreira B, Eriksen HM (1998) Prevalence of apical periodontitis and results of endodontic treatment in an adult, Portuguese population. Int Endod J 31:161–165
Schulte A, Pieper K, Charalabidou O, Stoll R, Stachniss V (1998) Prevalence and quality of root canal fillings in a German adult population. A survey of orthopantomograms taken in 1983 and 1992. Clin Oral Investig 2:67–72
De Moor RJ, Hommez GM, De Boever JG, Delme KI, Martens GE (2000) Periapical health related to the quality of root canal treatment in a Belgian population. Int Endod J 33:113–120
Boucher Y, Matossian L, Rilliard F, Machtou P (2002) Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int Endod J 35:229–238
Kabak Y, Abbott PV (2005) Prevalence of apical periodontitis and the quality of endodontic treatment in an adult Belarusian population. Int Endod J 38:238–245
Loftus JJ, Keating AP, McCartan BE (2005) Periapical status and quality of endodontic treatment in an adult Irish population. Int Endod J 38:81–86
Chen CY, Hasselgren G, Serman N, Elkind MS, Desvarieux M, Engebretson SP (2007) Prevalence and quality of endodontic treatment in the Northern Manhattan elderly. J Endod 33:230–234
Gulsahi K, Gulsahi A, Ungor M, Genc Y (2008) Frequency of root-filled teeth and prevalence of apical periodontitis in an adult Turkish population. Int Endod J 41:78–85
Covello F, Franco V, Schiavetti R, Clementini M, Mannocci A, Ottria L, Costacurta M (2010) Prevalence of apical periodontitis and quality of endodontic treatment in an Italian adult population. Oral Implantol 3:9–14
Kamberi B, Hoxha V, Stavileci M, Dragusha E, Kuci A, Kqiku L (2011) Prevalence of apical periodontitis and endodontic treatment in a Kosovar adult population. BMC oral health 11:32
Matijevic J, Cizmekovic Dadic T, Prpic Mehicic G, Ani I, Slaj M, Jukic Krmek S (2011) Prevalence of apical periodontitis and quality of root canal fillings in population of Zagreb, Croatia: a cross-sectional study. Croat Med J 52:679–687
Al-Omari MA, Hazaa A, Haddad F (2011) Frequency and distribution of root filled teeth and apical periodontitis in a Jordanian subpopulation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:59–65
Mukhaimer R, Hussein E, Orafi I (2012) Prevalence of apical periodontitis and quality of root canal treatment in an adult Palestinian sub-population. Saudi Dent J 24:149–155
Jersa I, Kundzina R (2013) Periapical status and quality of root fillings in a selected adult Riga population. Stomatologija 15:73–77
Moreno JO, Alves FR, Goncalves LS, Martinez AM, Rocas IN, Siqueira JF Jr (2013) Periradicular status and quality of root canal fillings and coronal restorations in an urban Colombian population. J Endod 39:600–604
Dutta A, Smith-Jack F, Saunders WP (2014) Prevalence of periradicular periodontitis in a Scottish subpopulation found on CBCT images. Int Endod J 47:854–863
Hebling E, Coutinho LA, Ferraz CC, Cunha FL, Queluz Dde P (2014) Periapical status and prevalence of endodontic treatment in institutionalized elderly. Braz Dent J 25:123–128
Song M, Park M, Lee CY, Kim E (2014) Periapical status related to the quality of coronal restorations and root fillings in a Korean population. J Endod 40:182–186
Oginni AO, Adeleke AA, Chandler NP (2015) Root canal treatment and prevalence of apical periodontitis in a Nigerian adult subpopulation: a radiographic study. Oral Health Prev Dent 13:85–90
Alfouzan K, Baskaradoss JK, Geevarghese A, Alzahrani M, Alhezaimi K (2016) Radiographic diagnosis of periapical status and quality of root canal fillings in a Saudi Arabian subpopulation. Oral Health Prev Dent 14:241–248
Dawson VS, Petersson K, Wolf E, Akerman S (2016) Periapical status of root-filled teeth restored with composite, amalgam, or full crown restorations: a cross-sectional study of a Swedish adult population. J Endod 42:1326–1333
Huumonen S, Suominen AL, Vehkalahti MM (2017) Prevalence of apical periodontitis in root filled teeth: findings from a nationwide survey in Finland. Int Endod J 50:229–236
Acknowledgments
We would like to thank Carmen Buckley for the help with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. Ethical approval was obtained by the local Research Ethics Committee (Nr. 412/2013 D). The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Clinical Relevance
Rotary instrumentation and a good technical quality of root fillings were reliable predictors for periapical health.
Rights and permissions
About this article
Cite this article
Connert, T., Truckenmüller, M., ElAyouti, A. et al. Changes in periapical status, quality of root fillings and estimated endodontic treatment need in a similar urban German population 20 years later. Clin Oral Invest 23, 1373–1382 (2019). https://doi.org/10.1007/s00784-018-2566-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2566-z