Abstract
Objectives
The objective of this study was to evaluate the effect of gamma irradiation on the wear behavior of human tooth dentin in terms of possible alterations in crystallinity, grain size, and composition.
Materials and methods
Human premolars (n = 19) were collected to obtain the perpendicular or parallel to the direction of the dentin tubule specimens. Each specimen was subjected to 60 Gy of gamma irradiation, in daily increments of 2 Gy. The nanoscratch tests were conducted. The scratch traces were observed via scanning electron microscope (SEM) and surface profilometer. X-ray diffraction (XRD) and Fourier transform infrared spectroscopy (FTIR) were used to investigate the alteration of crystallography and chemical composition of dentin after irradiation. The change of surface microhardness (SMH) was also evaluated.
Results
The nanoscratch results showed that the friction coefficient of dentin after irradiation became higher, and the depths and widths of scratch were greater than that of dentin before irradiation. Additionally, irradiation decreased the crystallinity of dentin and induced the formation of bigger crystals. The carbonate/mineral ratio was increased. Furthermore, a significant reduction in microhardness after irradiation was observed. The main damage mechanisms consisted of the formation of delamination and crack in both the specimens cut perpendicular and parallel to tubule dentin after irradiation.
Conclusion
Irradiation affected directly the wear behavior of tooth dentin, accompanied by the alterations in crystallography, chemical composition, and surface microhardness of dentin.
Clinical relevance
This would help extend understanding the influence of irradiation on dentin and provide suggestions for selecting more suitable materials for irradiated tooth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiation therapy, a primary therapy to surgical treatment in conjunction with chemotherapy, is widely used for the treatment of head and neck cancer patients [1]. Despite a careful planning, it is inevitable that radiotherapy would cause some damage to healthy tissues located in the field of radiation [2].
The post-irradiation caries has been accepted as the most common clinically observed side effect after radiotherapy [2, 3]. Meanwhile, numerous studies also demonstrated that the change of physical and composition component in human teeth after irradiation would influence the mechanical properties, such as the reduction in surface microhardness of dentin [4, 5], and ultimate tensile strength of dentin [6]. Dental friction and wear, a natural and unavoidable process, is of extreme significance to the physiology function of human teeth. As discovered in our previous studies, the wear resistance of enamel was significantly decreased after gamma irradiation [10]. Compared to enamel, dentin shows a decreased hardness [7], accompanied by inferior wear resistance [8] and decreased resistance against external stimulation [9]. However, till now, no relative study has been reported about the effect of gamma irradiation on the wear behavior of dentin. In addition, our previous study revealed that the wear behavior of enamel after irradiation may be related to the modification of crystallography and composition of enamel induced by irradiation. The crystal size of hydroxyapatite in dentin is smaller than that in enamel while more organic and water exist in the dentin; whether this alteration would influence the wear behavior of dentin after irradiation is also needed to be investigated. Furthermore, patients who are diagnosed with oral cancer are mostly aging people when most enamel is frequently worn out due to normal dental friction and wear [11]. Meanwhile, enamel will be easily lost because of the rampant process occurring in the enamel after irradiation [2]. As a result, superficial dentin of a patient who receive radiotherapy will be directly exposed to the irradiation, Thus, an understanding of the friction and wear behavior of dentin caused by irradiation would not only add new evidence about the effect of irradiation on dental hard tissue but also provide new insights into the indication for the effective clinical treatment for irradiated teeth and finally improve the life quality of a patient with oral cancer.
Therefore, the aim of present study was to evaluate the effect of gamma irradiation on the wear behavior of human tooth dentin in relation to the dentin tubule orientation. In addition, the effect of mineral characteristics and composition changes was evaluated. Our null hypothesis was that irradiation has no effect on the tribological properties of dentin.
Materials and methods
Specimen preparation
Nineteen sound human premolars without caries, from individuals aged between 13 and 20 years for orthodontic reason, were prepared after patients signed informed consent approved by the Ethics Committee of the West China College of Stomatology, Sichuan University (WCHSIRB-D-2013-152). After extraction, the teeth were stored in normal saline (4 °C) (Normal saline, Huaxing Kono Biotechnology Company, Beijing, China) immediately before use. The crowns were removed at the cementoenamel junction using a diamond-coated band saw (Minitom; Struers, Copenhagen, Denmark). Thus, dentin was collected. When the dentin specimens were prepared, the cutting direction was adjusted to be perpendicular (two specimens) or parallel (two specimens) to the direction of the dentin tubule (Fig. 1). Thirteen human teeth were randomly selected for scratch resistance and microhardness test. These dentin blocks were embedded into polymethyl methacrylate (Denture Base Material, Alpha Dental Equipment Company, Shanghai, China) with an exposed window of about 2 mm × 2 mm. Another six human teeth dentin, which were not imbedded in polymethyl methacrylate, were prepared for X-ray diffraction (XRD) and Fourier transform infrared spectroscopy (FTIR) analysis. All the slabs were hand-ground polished using silicon carbide papers with grit size of 500, 800, 1200, 2000, 3000, and 4000 (Sharpness, Hubei Yuli Abrasive Belts Group Company, Hubei, China) in turn, followed by polishing with 10, 5, and 2.5 μm (Laihua, Laizhou Laihua Test Instrument Company, Laizhou, China) diamond paste in sequence. Cutting, grinding, and polishing were all conducted under water-cooling conditions to avoid dehydration and changes in both the microstructure and chemistry of human teeth caused by local overheat. Finally, all the specimens were ultrasonically cleaned in distilled water (KQ218, Kunshan Ultrasonic Instruments Company, Kunshan, China) for 10 min to remove the debris according to our previous studies [12, 13].
Gamma irradiation procedure
The dentin specimens directly received a total of 60 Gy of gamma radiation in a 60Co irradiation unit (GWXJ80 60Co radiotherapy treatment unit, Nuclear Power Institute of China, Chengdu, China), in daily increments of 2 Gy, 5 days a week, and for 6 weeks. This dose was defined on the irradiation unit. The total dosage of radiation and the course of therapy were in agreement with the radiotherapy used for oral cancer patients [14, 15]. All the samples were immersed in artificial saliva (Keda, Dongguan Kehong Chemical Company, Dongguan, China) changed daily, apart from testing at room temperature without artificial saliva. After finishing irradiation, deionized water was used to rinse thoroughly each specimen for further testing.
Nanoscratch tests
With a nanoscratch tester (NST, CSEM Instruments, Peseux, Switzerland), all scratch tests were conducted with a conical diamond tip of a radius of 2 μm. The dentin samples before and after irradiation were tested without the application of artificial saliva at room temperature. The scratch test was firstly performed with a progressive load range from 0.1 to 80 mN. The sliding velocity was 500 μm/min. The scratch distance was set to 500 μm. At least two scratches were made in each specimen region. Each scratch was at least 2 μm away from the other scratch. Afterwards, three normal constant loads of 20, 40, and 60 mN were used. This scratch length was 200 μm. After the scratch tests, the remnant depths and width of the scratch grooves were measured by a surface profilometer (XP-2, Ambios Technology, CA, USA). The morphologies were observed using a scanning electron microscope (INSPECT F, FEI, Eindhoven, Holland) [16].
X-ray diffraction
X-ray diffraction (XRD, X’pert PRO, Panalytical, Almelo, Netherlands) was used to investigate the crystal structure of dentin specimens before and after irradiation. The parameters were adjusted according to our previous studies: CuKα radiation is at 35 kV/25 mA, 10°–70° scanning angle [17]. Both the crystallinity and crystallite size were calculated via the software Jade 5 (MDI, Materials Data Inc., USA). The crystallite size was also calculated using Scherrer’s formula [18, 19]: D = 0.89 λ/β cos θ. λ is the wavelength (CuKα), β represents the full width at the half-maximum of the HA (211), and θ is the diffraction angle.
Fourier transform infrared spectroscopy detection
The FTIR spectrometer used in the present study was a spectrometer (IRPRestige-21, Shimadzu, Japan). The machine was set at a resolution of 4 cm−1, a spectra range of 650 to 4000 cm−1. To keep measurement at the same region before and after irradiation, one mark was made in the reverse side of the testing surfaces. Each testing surface was carefully positioned against the diamond crystal of the FTIR unit and a constant pressure was applied so as to facilitate contact.
The infrared spectra of dentin before and after treatment were collected. The band between 810 and 885 cm−1 represents CO3 2− v2, while the band between 885 and 1090 cm−1 gave informations about PO4 3− v1, v3. After baseline correction and normalization, the ratio of the integrated areas of CO3 2− v2 contour to the PO4 3− v1, v3 contour which indicates the carbonate/mineral ratio (C/M ratio) was examined using OMNIC 8.0 software (Nicolet, Madison, WI, USA) [20].
Microhardness test
The surface microhardness (SMH) of dentin specimens were measured via a Knoop diamond indenter (Duramin-1/-2, Struers, Copenhagen, Denmark) with a load of 25 g for 10 s [8, 20]. Surface microhardness between 50 and 80 Knoop hardness number (KHN) were selected for further nanoscratch resistance [7]. The measurements after irradiation treatment were made near the initial indentations (100 μm space). The mean values of all measurements before and after treatment were recorded and compared.
Statistical analysis
Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) Version 13.0 software (SPSS Inc., Chicago, IL, USA). The residual depth, residual width, crystallinity, crystal size value, C/M ratio, and Knoop surface microhardness of specimens before and after irradiation were analyzed by paired t test. A P value of <0.05 was considered to represent statistical significance.
Results
Microwear behaviors
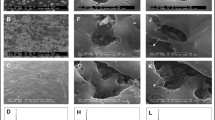
The typical micrographs of scratches conducted with normal loads on the dentin specimens perpendicular to tubule orientation before and after irradiation are presented in Fig. 2. There existed distinct differences between the scratch morphologies of dentin before and after treatment. At the load of 20 mN, plastic deformation formed on the surface of dentin before (Fig. 2a1) and after irradiation (Fig. 2b1). When the load was increased to 40 mN, trace of the deformed grooves with little debris formed at one edge was observed in dentin before irradiation (Fig. 2a2), while a small amount of debris at the edges of the scratch trace appeared in dentin after irradiation (Fig. 2b2). Under a load of 60 mN, a little debris with some crack formation in the scratch trace before irradiation (Fig. 2a3) and more debris accumulated on edges along the length of the scratch traces, accompanied with more crack formation seen in dentin after irradiation (Fig. 2b3). At the ultimate load levels, the more partial packing with cracks occurred in the load before irradiation (Fig. 2a4). Some delamination along with obvious cracks appeared at the edges of the scratch after irradiation (Fig. 2b4).
When the scratch was tested on specimens parallel to the dentin tubule orientation, trace groove of dentin before and after irradiation can also be observed in Fig. 3. Plastic deformation appeared in both dentin before (Fig. 3a1) and after irradiation (Fig. 3b1). As the load increased to 40 mN, a wider scratch trace was seen in dentin before irradiation (Fig. 3a2), whereas a wider trace with a little debris occurred at one edge of trace after irradiation (Fig. 3b2). Under a high load of 60 mN, some debris piled up at the edges of the scratch trace before irradiation (Fig. 3a3), while debris with a little delamination and some cracks emerged after irradiation (Fig. 3b3). At the ultimate load, more debris formation together with some cracks in trace was observed before irradiation (Fig. 3a4) and several obvious cracks propagated along the trace after irradiation (Fig. 3b4).
Friction coefficient
Figure 4a, b shows the typical curve of the friction coefficient in a progressively increasing load mode in both specimens cut perpendicular and parallel to dentin tubule orientation before and after irradiation, respectively.
With the dentin specimens cut perpendicular to tubule orientation section (Fig. 4a), the friction coefficients of dentin before and after treatment demonstrated obvious oscillation at the beginning. The coefficient of friction became stable when the load approached about 5 mN in dentin before irradiation and 2 mN in dentin after irradiation. Then, with the normal load increasing further, the friction curve increased slowly along with the appearance of some fluctuations. In general, the friction curve of dentin after irradiation was similar to those in dentin before irradiation, apart from the higher friction coefficient than that of dentin before irradiation at the same load.
Both the curve of friction coefficient of dentin specimens cut parallel to tubule orientation before and after irradiation oscillated significantly at the beginning (Fig. 4b). When the load increased to 5 mN in dentin before treatment and 3 mN in dentin after treatment, the friction coefficient turned smooth. As the load increased further, both the coefficient of friction of dentin before and after treatment increased slowly, accompanied by some fluctuations. The dentin after irradiation presented a friction coefficient higher than that of the dentin before irradiation.
Residual depth and residual width
Table 1 shows the variations of remnant depth and width of the scratch with three constant loads along tubule orientation. In both two directions to tubule orientation, the scratch depth has a statistically significant increase in the dentin after irradiation when compared to dentin before irradiation at the load of 40 and 60 mN, but the depth did not achieve statistical significance when the load was 20 mN. Meanwhile, the scratch widths of dentin after irradiation were statistically significantly greater than that of dentin before irradiation at the load of 20, 40, and 60 mN.
XRD results
Figure 5a, b presents the XRD spectra of dentin specimens cut perpendicular or parallel to tubule orientation before and after irradiation, respectively. The XRD analysis indicated that the crystalline phase in dentin before and after irradiation was also hydroxyapatite just as some previous studies described [21]. Meanwhile, the reduction in crystallinity and the increase in crystal size caused by irradiation can be seen in both the dentin cut perpendicular or parallel to tubule orientation (Table 2).
FTIR analysis
In both the dentin samples cut perpendicular to tubule orientation (Fig. 6a) as well as parallel to tubule orientation (Fig. 6b), the absorbance and the integrated area of CO3 2− v2 and PO4 3− v1, v3 significantly decreased after irradiation. In addition, the PO4 3− v1, v3 integrated area reduced more than the CO3 2− v2 area. The C/M ratio after irradiation increased significantly in both orientation groups (Table 2).
Microhardness test results
The changes in the microhardness values of dentin in both the perpendicular and parallel to tubule orientation are presented in Table 3. There was no significant difference between dentin specimens before irradiation. A significant reduction of SMH with statistical significance was observed in the perpendicular and parallel to tubule orientation dentin specimens after irradiation, respectively.
Discussion
Based on the results given above, it is reasonable to conclude that gamma irradiation reduces the wear resistance of dentin. This obviously is related to both microstructure and composition in dentin. Therefore, our null hypothesis was rejected.
Radiotherapy is a widely used treatment for oral cancer. Therefore, some factors were taken into consideration to standardize the evaluation and approximately close to clinical conditions in our present study. The total dosage of 60 Gy irradiation for 6 weeks was consistent with the treatment for patients diagnosed with oral cancer [14, 15]. The daily incremental dose of 2 Gy was set to simulate the same dose that patients receive. Meanwhile, specimens were stored in artificial saliva changed daily during radiation. However, some other storage media such as distilled water and buffered phosphate solution were used to store teeth. Artificial saliva was the most suitable storage media for some similar experiments [6, 22]. Although the data were obtained in a laboratory setup, the experiment model used in this study provides a better simulation condition of clinical irradiation for patients diagnosed with oral cancer and more closely to patients’ oral environment.
Human tooth is composed of a hierarchical structure with important features down to the nanometer or micrometer scale, while the changes in dentin after irradiation would be slight at the beginning. Thereby, the wear behavior of dentin should be observed promptly at nanoscale. Nanoscratch technique can push a diamond tip with micrometer-scale curvature radius at a controlled load range of 1 μN to 500 mN over the material surface to investigate the microscopic wear behavior and mechanism of material wear [23, 24]. Thus, it was accepted as a powerful and effective tool for detecting the microtribological properties of human tooth enamel and dentin under different clinical conditions (caries development, EDTA treatment or Nd:YAG laser irradiation) according to our previous studies [12, 13, 16, 25]. Thus, nanoscratch tests were applied to investigate the wear behavior of dentin before and after irradiation in the present study.
From the results of nanoscratch tests, we clearly found that the coefficient of friction in dentin after irradiation in two directions became higher than that of dentin before irradiation. Earlier studies reported that the wear resistance decreased with the increase in friction coefficient [26, 27]. This suggested that irradiation resulted in a deleterious effect on the wear behavior of dentin. Moreover, irradiation significantly increased the scratch depth and width of dentin, which further confirmed the above conclusion. Furthermore, although both the main damage mechanism of the dentin specimens cut perpendicular or parallel to tubule orientation were delamination and formation of crack, more debris and obvious crack formation in dentin after irradiation in comparison to dentin before irradiation were observed. Considering the higher friction coefficient, more debris, crack formation, and deeper scratch depth and wider width, we may speculate that irradiation weakens the anti-wear properties of dentin.
As a hydrated biological tissue, the mechanical properties of dentin vary with its microstructure and composition [28]. Among numerous detecting techniques, XRD was the most used application for measuring crystalline structure of human dentin while FTIR is an absorption spectroscopy technique to examine inorganic materials and measure the quantitative alterations in the composition of mineralized tissue. Based on the outcomes of both the XRD and FTIR analyses, we could obviously find that irradiation decreases the crystallinity, PO43− v1, v3 integrated area and increase the crystal size and C/M ratio in dentin. These results were in agreement with our previous experiment results in irradiated enamel. Some earlier articles also showed that irradiation would soften human tooth dentin [4, 29], as confirmed by our study. The decreased microhardness in dentin indicated inferior wear resistance after irradiation [25]. It is also revealed that irradiation would induce the presence of cracks and the formation of obliteration in dentin structure. Additionally, the increasing destruction of collagen fibril reinforced with a nanocrystalline would occur after irradiation. These defect of structure after irradiation cause the dentin tissue to be dry and friable [30], which would result in the occurrence of inferior wear resistance. Indeed, for teeth exposed to ≥60 Gy, irradiation had a direct effect on teeth structure as described in another previous research [31]. Therefore, the effect of irradiation on the microstructure and composition and these changes in related to the wear behavior would be proven again.
In general, our in vitro study demonstrated that the crystallography and composition alterations in dentin after irradiation may account for the inferior wear resistance. However, the present study design has some limitations, and there are interesting questions needing to be answered with future studies. In the current study, we just analyze the effect of gamma irradiation on the wear behavior of human tooth dentin, while linear accelerator, another widely used method for irradiation, will be added in the future study. The morphological changes of the whole dentin and the microstructure, including collagen and hydroxyapatite crystal after irradiation, should be observed directly via atomic force microscope (AFM) or even transmission electron microscope (TEM). Previous studies have showed irradiation influenced the organic materials of dentin [32, 33]. Further studies should be done to investigate the exact alteration of composition of dentin through Raman spectroscopic detection or even immunohistochemistry for collagen in dentin. Additional studies showed the water content in dentin influence its mechanical properties [34]. Therefore, the dentin’s water loss during experiment should be taken into consideration in our future study.
Conclusions
Based on the findings of the present study, it can be concluded that the gamma irradiation radiotherapy would weaken the wear resistance of dentin. Meanwhile, the alterations in crystallography and composition of dentin after irradiation may induce the occurrence of inferior wear behavior.
References
Rosales AC, Esteves SC, Jorge J, Almeida OP, Lopes MA (2009) Dental needs in Brazilian patients subjected to head and neck radiotherapy. Braz Dent J 20:74–77
Kielbassa AM, Hinkelbein W, Hellwig E, Meyer-Lückel H (2006) Radiation-related damage to dentition. Lancet Oncol 7:326–335
Eliasson L, Carlén A, Almstrál A, Wikström M, Laingström P (2006) Dental plaque pH and micro-organisms during hyposalivation. J Dent Res 85:334–338
Kielbassa AM, Beetz I, Schendera A, Hellwig E (1997) Irradiation effects on microhardness of fluoridated and non-fluoridated bovine dentin. Eur J Oral Sci 105:444–447
Kielbassa AM, Munz I, Bruggmoser G, Schulte-Monting J (2002) Effect of demineralization and remineralization on microhardness of irradiated dentin. J Clin Dent 13:104–110
Soares CJ, Castro CG, Neiva NA, Soares PV, Santos-Fillho PCF, Naves LZ, et al. (2010) Effect of gamma irradiation on ultimate tensile strength of enamel and dentin. J Dent Res 89:159–164. doi:10.1177/0022034509351251
Meredith N, Sherriff M, Setchell DJ, Swanson SA (1996) Measurement of the microhardness and Young’s modulus of human enamel and dentine using an indentation technique. Arch Oral Biol 41:539–545
Zheng J, Zhou ZR, Zhang J, Li H, Yu HY (2003) On the friction and wear behaviour of human tooth enamel and dentin. Wear 255:967–974. doi:10.1016/S0043-1648(03)00079-6
Faraoni-Romano JJ, Turssi CP, Serra MC (2009) Effect of a 10 % carbamide peroxide on wear resistance of enamel and dentine: in situ study. J Dent 37:273–278. doi:10.1016/j.jdent.2008.12.001
Qing P, Huang SB, Gao SS, Qian LM, Yu HY (2015) Effect of gamma irradiation on the wear behavior of human tooth enamel. Sci Rep 23:11568. doi:10.1038/srep11568
Anand P, Sundaram C, Jhurani S, Kunnumakkara AB, Aggarwal BB (2008) Curcumin and cancer: an “old-age” disease with an “age-old” solution. Cancer Lett 18:133–164. doi:10.1016/j.canlet.2008.03.025
Gao SS, Huang SB, Qian LM, Yu HY, Zhou ZR (2009) Wear behavior of early carious enamel before and after remineralization. Wear 267:726–733. doi:10.1016/j.wear.2008.11.018
Gao SS, Qian LM, Huang SB, Yu HY (2009) Effect of gallic acid on the wear behavior of early carious enamel. Biomed Mater 4:034101. doi:10.1088/1748-6041/4/3/034101
Soares CJ, Neiva NA, Soares PB, Dechichi P, Novais VR, Naves LZ, et al. (2011) Effects of chlorhexidine and fluoride on irradiated enamel and dentin. J Dent Res 90:659–664. doi:10.1177/0022034511398272
Rashid UN, Shyamoli M, Arefuddin A (2013) Evaluation of response to radiotherapy in early stage laryngeal carcinoma. IOSR-JDMS 6:112–116
Gao SS, Huang SB, Qian LM, Yu HY (2010) Nanoscratch resistance of human tooth enamel treated by Nd:YAG laser irradiation. P I Mech Eng J-J Eng 224:529–537. doi:10.1243/13506501JET668
Huang SB, Gao SS, Yu HY (2009) Effect of nano-hydroxyapatite concentration on remineralization of initial enamel lesion in vitro. Biomed Mater 4:034104. doi:10.1088/1748-6041/4/3/034104
Azaroff LA (1968) Elements of X-ray crystallography. McGraw-Hill, New York, pp. 38–42
Huang SB, Gao SS, Cheng L, Yu HY (2010) Combined effects of nano-hydroxyapatite and Galla chinensis on remineralisation of initial enamel lesion in vitro. J Dent 38:811–819. doi:10.1016/j.jdent.2010.06.013
Sun LL, Liang SS, Sa Y, Wang ZJ, Ma X, Jiang T, et al. (2011) Surface alteration of human tooth enamel subjected to acidic and neutral 30 % hydrogen peroxide. J Dent 39:686–692. doi:10.1016/j.jdent.2011.07.011
Lee B-S, Hung Y-L, Lan W-H (2003) Compositional and morphological changes of human dentin after Er:YAG laser irradiation. Int Congr Ser 1248:143–152. doi:10.1016/S0531-5131(02)01299-2
Amaechi BT, Higham SM, Podoleanu AG, Rogers JA, Jackson DA (2006) Use of optical coherence tomography for assessment of dental caries: quantitative procedure. J Oral Rehabil 28:1092–1093
Bhushan B (1999) Handbook of micro/nanotribology (2nd edition). CRC Press, Boca Raton
Bhushan B (2004) Springer handbook of nanotechnology. Springer, Heidelberg
Gao SS, Cai ZB, Huang SB, Qian LM, Yu HY (2013) Nano-scratch behavior of human root canal wall dentin lubricated with EDTA pastes. Tribol Int 63:169–176. doi:10.1016/j.triboint.2012.03.010
Zheng J, Xiao F, Qian LM, Zhou ZR (2009) Erosion behavior of human tooth enamel in citric acid solution. Tribol Int 42:1558–1564. doi:10.1016/j.triboint.2008.12.008
Zheng J, Huang H, Shi MY, Zheng L, Qian LM, Zhou ZR (2011) In vitro study on the wear behaviour of human tooth enamel in citric acid solution. Wear 271:2313–2321. doi:10.1016/j.wear.2010.11.027
Mjör IA (1972) Human coronal dentine: structure and reactions. Or Surg Or Med Or Pa 33:810–823
Kielbassa AM, Wrbas KT, Schulte-Mönting J, Hellwig E (1999) Correlation of transversal microradiography and microhardness on in situ-induced demineralization in irradiated and nonirradiated human dental enamel. Arch Oral Biol 44:243–251
Gonçalves LM, Palma-Dibb RG, Paula-Silva FW, Oliveira HF, Nelson-Filho P, Silva LA, et al. (2014) Radiation therapy alters microhardness and microstructure of enamel and dentin of permanent human teeth. J Dent 42:986–992. doi:10.1016/j.jdent.2014.05.011
Walker MP, Wichman B, Cheng AL, Coster J, Williams KB (2011) Impact of radiotherapy dose on dentition breakdown in head and neck cancer patients. Pract Radiat Oncol 1:142–148
Açil Y, Springer IN, Niehoff P, Gassling V, Warnke PH, Açmaz S, et al. (2007) Proof of direct radiogenic destruction of collagen in vitro. Strahlenther Onkol 183:374–379
Springer IN, Niehoff P, Warnke PH, Böcek G, Kovács G, Suhr M, et al. (2005) Radiation caries–radiogenic destruction of dental collagen. Oral Oncol 41:723–728
Jameson MW, Tidmarsh BG, Hood JA (1994) Effect of storage media on subsequent water loss and regain by human and bovine dentine and on mechanical properties of human dentine in vitro. Arch Oral Biol 39:759–767
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This experiment was approved by the Ethics Committee of the West China College of Stomatology, Sichuan University (WCHSIRB-D-2013-152).
Conflict of interest
The authors declare that they have no financial or personal conflicts of interest in relation to this study. All authors approved the publication of the manuscript.
Funding
This work was supported by the State Key Laboratory of Oral Diseases, Sichuan University, China (SKLODSCU20130044), and Specialized Research Fund for the Doctoral Program of Higher Education (20110181110056).
Informed consent
This experiment was prepared after all involved patients signed informed consent.
Additional information
Ping Qing and Shengbin Huang contributed equally to this work.
Electronic supplementary material
ESM 1
(PDF 684 kb)
Rights and permissions
About this article
Cite this article
Qing, P., Huang, S., Gao, S. et al. Effect of gamma irradiation on the wear behavior of human tooth dentin. Clin Oral Invest 20, 2379–2386 (2016). https://doi.org/10.1007/s00784-016-1731-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1731-5