Abstract
Background and objective
Subepithelial connective tissue grafts (SeCTG) in conjunction with a coronally advanced flap (CAF) or with tunneling technique (TT) are common periodontal procedures with similar indications for the treatment of a denuded root surface; however, it is unclear whether patient discomfort and postoperative morbidity are comparable in both approaches. The aim of this randomized controlled clinical trial was to compare the patient morbidity and root coverage outcomes of a SeCTG used in combination with a CAF or TT.
Materials and methods
For this single-center, randomized, clinical trial, patients were randomly assigned to receive SeCTG + CAF (control group) or SeCTG + TT (test group). Postoperative questionnaires at 3 days post intervention were administered to evaluate postoperative discomfort, bleeding, and inability to masticate. Evaluation of patients’ perception of pain was performed using a visual analog scale (VAS). Clinical outcomes including percentage of root coverage (RC) and complete root coverage (CRC) were recorded 12 months postoperatively.
Results
Fifty patients (25 SeCTG + CAF and 25 SeCTG + TT) completed the study. Healing was uneventful for all test and control patients. The SeCTG + TT group showed a longer chair time (33.6 (3.6) and 23.6 (4.2) min for the SeCTG + TT and the SeCTG + CAF, respectively), as well as more painkiller consumption: 2736 vs. 1536 mg (p < 0.001). At the same time, the SeCTG + CAF group reported less pain or discomfort in all four sections of the questionnaire: pain experienced within the mouth as a whole, pain experienced throughout the day, pain experienced at night, and edema experienced after the surgery (p = 0.002, p = 0.001, p = 0.001, and p = 0001, respectively). Both treatments showed clinical efficacy in terms of root coverage as no differences per group were observed in the percentage of root coverage (87 vs. 85 %, p = 704) or patients with complete root coverage (60 vs. 52 %, p = 0.569).
Conclusions
SeCTG + TT is associated with a greater incidence of pain and discomfort compared to SeCTG + CAF in early postoperative periods, as well as a longer chair time. Both treatments showed similar clinical efficacy in terms of root coverage.
Clinical relevance
The results of this study may influence the surgeon’s choice on which root coverage procedure should be performed considering the need of more chair time and more painkiller assumption with the tunneling technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background and objectives
Over the years, several surgical techniques have been introduced to correct labial, gingival recession defects [1]. Recession of the gingival margin remains a highly prevalent problem for its impact on both aesthetics and dentine hypersensitivity [1]. Although different techniques have shown a consistent potential for root coverage, meta-analyses from several systematic reviews revealed great variability of clinical outcomes [2–6]. These reviews showed a greater recession reduction and a larger amount of roots completely covered following bilaminar techniques (coronally advanced flap + subepithelial connective tissue graft [7] [SeCTG + CAF] as compared with regenerative procedures [8] or coronally advanced flap alone [9, 10]). More recently, several authors have proposed the application of a SeCTG using a tunneling technique (TT), which has recently gained popularity in periodontal mucogingival therapy [11, 12]. In all surgical procedures, fast and uneventful wound healing is a fundamental prerequisite for successful treatment outcomes [13, 14]. In this context, it is generally acknowledged that microsurgical tunneling flap procedures are associated with more favorable postoperative patient-reported outcomes [11, 15]. This notion is based on the assumption that flap elevation without surgical papilla dissection and without vertical releasing incisions contributes to a comparatively low impairment of the local blood supply, as well as to a minimal risk of postoperative scar tissue formation [16].
Mucogingival surgery was shown to cause postoperative pain more frequently than osseous surgery and periodontal flap surgery [17].
In most instances, the focus of pain assessment revolves around the tissue donor site, which is normally the palatal region proximal to the maxillary premolars.
Minimal attention has been paid to the exclusive perception of pain emanating from the recipient area or overall oral cavity. More trivial postoperative symptoms such as pain, discomfort, swelling, and mild bleeding are experienced routinely by patients undergoing mucogingival surgery [18, 19]. In general, such manifestations are short lived and occur over the early postoperative period (3 days) [20].
However, there is scarce data available regarding postoperative patient-centered outcomes after TT as compared to other surgical procedures for the treatment of gingival recession.
Specific objectives or hypotheses
Therefore, the primary aim of this randomized controlled clinical trial was to assess any differences in the postoperative morbidity following two of the most conventional and routinely indicated mucogingival procedures: SeCTG + CAF and SeCTG + TT. The secondary aim was to assess clinical outcomes in terms of root coverage for both techniques.
Materials and methods
Trial design and ethics committee approval
The present article is reported in accordance with the CONSORT 2010 statement for improving the quality of reporting on randomized controlled trials [21, 22].
Description of the trial design
The study was designed as a single-center, randomized, clinical trial on the treatment of single gingival recessions. Two different treatment modalities were assessed: the coronally advanced flap with a subepithelial connective tissue graft (SeCTG + CAF) (control group) was compared to the tunneling technique with a subepithelial connective tissue graft (SeCTG + TT) (test group) in terms of clinical outcomes and postoperative morbidity. The study protocol was review approved by the Institutional Review Board at the University of Padova, Padua, Italy (Ethics Committee No.: 2566P), and it was registered in clinicaltrials.org (ID: NCT02269748). Informed consent was obtained from all participants included in the study. In obtaining the informed consent, administering the questionnaires, and conducting the study, the principles outlined in the Declaration of Helsinki, as revised in 2000, were strictly followed.
Participants
Eligibility criteria for participants
Patients were selected, on a consecutive basis, among individuals referred to the University of Padova School of Dental Medicine, Department of Periodontology. All patients agreed to participate in the study and signed a written informed consent.
All participants met the study inclusion criteria: single or multiple Miller’s class I and II recession defects [23] (≥2 mm in depth, not exceeding 5 mm in depth); presence of identifiable cemento-enamel junction (CEJ); presence of a step ≤1 mm at the CEJ level and/or presence of a root abrasion, but with an identifiable CEJ; and periodontally and systemically healthy, with full mouth plaque and bleeding scores [24] <20 %. During recruitment of the patients, the following exclusion criteria were employed: contraindications for periodontal surgery, taking medications known to interfere with periodontal tissue health or healing, anti-inflammatory drugs or antibiotics for the last 6 months, and participants who underwent periodontal surgery on the involved sites; smokers were also excluded from the study. Excluded sites were recession defects associated with caries or restoration as well as teeth with evidence of a pulpal pathology, molar teeth, teeth showing any kind of malpositioning (rotation or extrusion), as well as teeth with any history of mucogingival or periodontal surgery. In case of multiple recessions, only an area of no more than three consecutive teeth was considered eligible for the study.
The study protocol involved a screening appointment to verify eligibility, followed by initial periodontal therapy to establish optimal plaque control and gingival health conditions, surgical therapy, evaluation of patient morbidity 3 days after the surgery, maintenance phase, and postoperative clinical evaluation 1 year after the surgery.
Settings and locations where the data were collected
The same operator (L.G.) performed all surgical procedures at the University of Padova, Padua, Italy. Data collection included clinical measurements at baseline and 12 months post intervention. Questionnaires were given to the participants before scheduling the surgery. To insure that the forms were completed, patients were reminded by a telephone call when their form needed completion. Clinical measurements were undertaken at the same clinic by a trained examiner (E.B.). Statistical analyses were performed at the Universitat Internacional de Catalunya, Barcelona, Spain.
Interventions
Pre-surgical preparations
Following the screening examination, all participants received a session of prophylaxis including oral hygiene instructions, scaling, and professional tooth cleaning with the use of a rubber cup and a low-abrasive polishing paste. A coronally directed roll technique, using a soft toothbrush, was recommended for teeth with recession-type defects in order to eliminate wrong habits associated with the etiology of gingival recessions. Surgical treatment of the recession defects was not scheduled until the patient could demonstrate an adequate standard of supragingival plaque control.
Surgical procedures
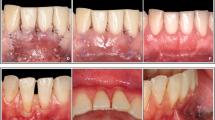
The control group (CAF + SeCTG) was treated with a coronally advanced flap procedure combined with a subepithelial connective tissue graft (Fig. 1a–e), whereas in the test group, the TT with subepithelial connective tissue graft was performed (Fig. 2a–d).
a Miller class I recession defects on the mandibular left premolars. b Full-thickness flap elevation. c The SeCTG is secured in position with continuous sling. d The overlying flap is coronally advanced over the donor tissue covering the latter as much as possible. e Clinically stable results 12 months post intervention
a Miller class I recession defects on the mandibular left premolars. b A subperiosteal tunnel was created extending through the gingival sulci of the lower premolars and beyond the mucogingival junction. c After the insertion, the subepithelial connective tissue graft (SeCTG) was secured in place with continuous sling sutures. d Clinically stable results 12 months post intervention
Following local anesthesia, the exposed root surfaces were polished with a rubber cup and pumice powder prior to flap elevation. The premolar area of the palate was injected with local anesthesia (2 % lidocaine with epinephrine at a concentration of 1:100,000). The surgical technique adopted for harvesting the SeCTG in both groups was the approach described by John F. Bruno [25].
Briefly, the first incision on the palate was made perpendicular to the long axis of the teeth, approximately 2 to 3 mm apical to the gingival margin of the maxillary teeth. The mesiodistal length of the incision was determined by the length of the graft necessary for the recipient site. The second incision was made parallel to the long axis of the teeth, 1 to 2 mm apical to the first incision. The incision was carried far enough apically to provide a sufficient height of connective tissue to cover the denuded root and the adjacent periosteum of the recipient site. The thickness of the graft was maintained uniform while proceeding apically with the blade. The donor tissue was then removed from the palate as atraumatically as possible. Care was taken not to remove the periosteum protecting the underlying bone. Once the graft was removed, the fatty tissue (yellow in color) was eliminated as well as the 1–2-mm band of epithelium at the coronal aspect of the graft. The primary flap was repositioned, and interrupted single 5-0 suturesFootnote 1 were made to achieve primary closure of the palatal wound.
Control group
In the control group (SeCTG + CAF), the incision for the flap advancement was performed as described by Zucchelli [26]. In brief, following local anesthesia, a horizontal incision was made with a scalpel to design an envelope flap. The horizontal incision of the envelope flap consisted of oblique submarginal incisions in the interdental areas, incisions that continued with the intrasulcular incision at the recession defects. The envelope flap was raised a split-full-split approach in the coronal-apical direction. Flap mobilization was considered “adequate” when the marginal portion of the flap was able to passively reach a level coronal to the CEJ at each single tooth in the surgical site. The root surface (only that portion of the root exposure) was mechanically treated with the use of curettes. After the flap was elevated, the donor connective tissue was secured in position with continuous sling suture 5-0 suturesFootnote 2. The overlying flap was then coronally advanced over the donor tissue covering the latter as much as possible. The flap was secured in placed with 5-0 suturesFootnote 3.
Test group
In the test group, SeCTG + TT treatment was performed in accordance with the description on a microsurgical tunneling technique by Allen [27]. Following initial sulcular incisions with a microsurgical blade, tunneling knives were used to undermine the buccal gingiva by means of a split-thickness flap preparation, aiming for the preparation of a continuous tunnel in the buccal soft tissues of the recessed area. The supraperiosteal dissection was extended well into the mucosal tissues in order to gain sufficient flap mobility. The adjacent papillary tissues were carefully detached by means of a full-thickness preparation in their buccal aspect, thus to allow for a coronal displacement of the mobilized buccal soft tissue complex. A subepithelial connective tissue graft (SeCTG) was trimmed to a thickness of 1–1.5 mm and then inserted into the tunnel. Double-crossed suturesFootnote 4 were applied to stabilize the buccal soft tissue complex in a coronal position about 1–2 mm above the CEJ. Small parts of the CTG were left uncovered when necessary to achieve a harmonious line of the gingival margin.
Surgical chair time was measured using a chronometer from the first incision to the last suture in both groups.
Postsurgical protocol
Patients were instructed to avoid any mechanical trauma or tooth brushing in the surgical sites for 2 weeks. They received 600 mg ibuprofen directly at the end of the surgical intervention and were instructed to take additional analgesic-antiphlogistic medication as required (ibuprofen). 0.12 % chlorhexidine rinses were prescribed two times per day for 2 weeks. Sutures were removed after 7 days. Two weeks after surgery, patients were instructed to resume mechanical tooth cleaning with a soft toothbrush. Patients were recalled at 1, 3, 6, and 12 months for professional oral hygiene procedures.
Outcomes
The primary aim of this randomized controlled clinical trial was to assess any differences in the postoperative morbidity following two of the most conventional and routinely indicated mucogingival procedures: SeCTG + CAF and SeCTG + TT. The secondary aim was to assess clinical outcomes in terms of root coverage for both techniques.
Patient morbidity
Postoperative pain was indirectly evaluated on the basis of the mean consumption (in mg) of analgesics (ibuprofen) [20, 28].
All patients were asked to complete a questionnaire designed to evaluate pain experience at early (3 days) stages following surgical procedure such as postoperative discomfort, bleeding, and inability to chew. To insure that the forms were completed, patients were reminded by a telephone call when their form needed completion. The survey utilized was a visual analog scale (VAS) scores from 1 to 10, with 1 indicating minimal pain and 10 indicating severe pain. If a patient indicated that no pain was present, a score of 0 was given. Each question allowed the patient to rate their pain experience from “NO PAIN” to “WORST POSSIBLE PAIN” in response to various stimuli, activities, and times of day. Different parameters were investigated (dichotomous fashion, yes or no): postoperative bleeding, quantity and type of analgesic medication taken, and patient eventually undergoing a similar procedure in the future if recommended by their dentist. Discomfort was defined as the level of soreness/pain experienced by the patients during the first 3 days in the grafted area. Bleeding was considered to be a prolonged hemorrhaging during the first 3 days post surgery, reported by the patients.
Inability to chew was described as the level of variation of the patient’s eating and drinking habits due to the presence of the wound.
Clinical measurements at baseline and 12 months
The following clinical parameters were assessed to the nearest 0.5 mm with the use of a PCP-UNC 15 periodontal probeFootnote 5 by a single masked examiner:
-
Gingival recession height (GH), measured from the CEJ to the most apical extension of the gingival margin.
-
Probing depth (PD), measured from the gingival margin to the bottom of the gingival sulcus at the central buccal site.
-
Clinical attachment level (CAL), measured from the CEJ to the bottom of the gingival sulcus at the central buccal site.
-
Height of keratinized tissue (KTH): the distance between the gingival margin and the mucogingival junction (MGJ). The MGJ was identified by means of Lugol staining.
Sample size calculation
Sample size was calculated based on the primary outcome (i.e., painkiller consumption) reported in a previous study with similar techniques [20]. Accepting an alpha risk of 5 % and a beta risk of 15 % in a two-sided test, 25 participant pregroups were considered necessary to recognize as statistically significant a difference greater than or equal to 1800 mg. The common standard deviation is assumed to be 2000 mg. A dropout rate of 10 % was anticipated.
Randomization and allocation concealment
Each patient was assigned to one of the two treatment groups using a computer-generated randomization table to ensure a balanced allocation of treatments. All patients participated in the study with a single tooth. Twenty-five teeth were assigned to the control group (SeCTG + CAF) and 25 teeth to the test group (SeCTG + TT). In the case of patients presenting with multiple recessions, the deepest one was selected; in the case of two or more recessions of the same depth, tossing a coin performed the selection. Allocation concealment was performed by opaque, sealed, coded envelopes that were opened immediately prior to the surgical interventions.
Implementation
A computer generated the random allocation sequence; L.G. enrolled the participants and F.M. assigned participants to interventions.
Blinding
A single masked examiner carried out all clinical measurements at baseline and 1 year after the surgery. The examiner did not perform surgery and was unaware of the treatment assignment. Before the study, the examiner was calibrated to reduce intra-examiner error: measurement of the distance between the CEJ and gingival margin was repeated three times by the examiner for a total of 50 defects with a K coefficient >0.75.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS Inc., v. 20 software, Chicago, IL, USA) was used for all analyses. The Kolmogorov-Smirnov test was used to analyze the distribution of continuous variables. Continuous variables are expressed as means ± standard deviation (SD) and compared at baseline by the Mann-Whitney U test. This test was also used to compare mean changes post vs. baseline measurements between groups. The Wilcoxon test was used to compare post vs. baseline measurements. Spearman correlation was used to evaluate associations. Complete coverage was evaluated after 1 year by calculating the percentage of cases, in each treatment group, with the gingival margin at the level or coronal to the CEJ. Percentage of root coverage was calculated after 12 months according to the following formula:
Unadjusted and adjusted associations between groups and pain or discomfort were calculated with linear regression models. Study group was included in each model as an independent variable. In adjusted models, painkiller doses were included as a confounder factor. The dependent variable was pain, according to the items of the questionnaire with statistical differences between groups in the bivariate analysis. The level of significance was set at 0.05.
Results
Recruitment
Fifty patients were recruited and treated between April 2012 and May 2013. All 50 patients completed the study. Patients were recalled at 1, 3, 6, and 12 months for professional oral hygiene procedures.
Numbers analyzed
In the SeCTG + CAF group, the mean age of the 25 patients (12 males and 13 females) was 27.6 (SD 6.0) years (range 20–35). Seventeen maxillary (four lateral incisors, seven canines, and six premolars) and eight mandibular (three incisors, three canines, and two premolars) teeth with gingival recession were treated. Four cases were single recession, nine multiple recession involving two adjacent teeth, and 12 involving three continuous teeth. In the SeCTG + TT group, the mean age of the 25 patients (14 males and 11 females) was 28.2 (SD 5.80) years (range 21–37). Eight maxillary (three central incisors, three canines, and two premolars) and 17 mandibular (11 central incisors, two canines, and four premolars) teeth with gingival recession were treated. Four cases were single recession, 12 multiple recession involving two adjacent teeth, and nine involving three continuous teeth.
Baseline data
Table 1 reports the baseline patient and defect-related characteristics. The two groups were well balanced in terms of age, GH, PD, CAL, and KTH. Most of the treated recessions were classified as Miller class I. No difference was noted for any of the collected measurements between the two groups. The descriptive statistics for the clinical parameters measured at baseline, as well as the mean differences within and between groups, are shown in Table 2. At baseline, there were no statistically significant differences between the two groups for any of the considered clinical parameters, indicating that the randomization process had been effective.
Outcomes and estimation
Baseline measurements were similar in both groups. Only differences in surgical time (min) and painkiller use during the first 3 days post surgery were observed between groups. Both cases were higher in the SeCTG + TT group (p < 0.001) (Table 2).
As reported by the stratified analysis (Table 3), the SeCTG + TT group measurements decreased statistically in GH (from 3.44 to 0.52; p < 0.001) and CAL (from 4.72 to 1.84; p < 0.001). A statistical increase was observed in KTH (from 2.24 to 4.84; p < 0.001). No difference was observed in PD (p = 0.705).
Similar results were found in the SeCTG + CAF groups; measurements decreased significantly in GH (from 3.48 to 0.56; p < 0.001) and CAL (from 4.72 to 1.8; p < 0.001). A statistically significant increase was observed in KTH (from 2.24 to 3.92; p < 0.001). No difference was observed in PD (p = 1.000) (Table 4).
GH, PD, and CAL reduction were similar in both groups. A statistical difference was observed in KTH: a higher increase in the SeCTG + TT group (2.6 vs. 1.68; p = 0.002). No differences were observed in the percentage of root coverage (87 vs. 85 %; p = 0.704) or patients with complete root coverage (60 vs. 52 %; p = 0.569) (Table 5).
In the entire sample, GH and CAL measurements decreased 12 months post intervention (p < 0.001), while KTH measurements increased 12 months post intervention (p < 0.001). Only PD measurements did not change during the follow-up period (p = 0.808). The amount of root coverage was 86 % (SD 17 %), and 28 (56 %) patients were with complete root coverage in the entire sample. A positive linear correlation was observed between surgical time and use of analgesic medication (r = 0.456, p = 0.001) (Table 6).
Patient morbidity
Healing was uneventful for all test and control patients. The mean painkiller consumption (in addition to the 600-mg ibuprofen given before the surgery) in the SeCTG + TT and the CAF + SeCTG groups was 2736 (±1460.3) and 1536 mg (±832), respectively. The difference was statistically significant (p < 0.001) (Table 2).
As reported in Table 7, statistical differences related to the VAS value were observed between groups in terms of general pain experienced within the mouth as a whole: higher in the SeCTG + TT group (5.2 vs. 4.3; p < 0.001); pain experienced during the day: higher in the SeCTG + TT group (3.1 vs. 1.7; p < 0.001); pain experienced at night: higher in the SeCTG + TT group (2.6 vs. 1.5; p < 0.001); and edema experienced after the surgery: higher in the SeCTG + TT group (3.8 vs. 1.4; p < 0.001).
No statistically significant difference was demonstrated between the control and the test patients in terms of the other VAS-related parameters: pain expressed while drinking (p = 0.686), pain expressed while chewing (p = 0.202), and pain expressed in the morning (p = 0.788). The percentage of patients that would be willing to go through this surgery again is similar in both groups (76 vs. 84 %; p = 0.724) and the percentage of patients that did experience bleeding is higher in CAF + SeCTG, but no significant differences were observed between groups (p = 0.667).
Ancillary analyses
Multivariate analysis to pain or discomfort
Positive linear relations were observed between pain and use of painkillers (r = 0.660, p < 0.001). On the other hand, patients in the SeCTG + TT group used more doses of painkillers.
In unadjusted associations, the SeCTG + CAF group has less pain or discomfort in four aspects of the questionnaire: pain experienced within the mouth as a whole, pain experienced throughout the day, pain experienced at night, and edema experienced after the surgery (p = 0.002, p = 0.001, p = 0.001, and p = 0.001, respectively). In adjusted models, the SeCTG + CAF group has 1.318 points less in pain experienced throughout the day (model 2), 0.825 points less in pain experienced at night (model 3), and 2.540 points less in edema experienced after the surgery (model 4) than the SeCTG + TT group, with independence to painkiller use. VAS pain experienced within the mouth as a whole (model 1) did not show significant differences between groups after adjusting for painkiller use (p = 0.237) despite that in the unadjusted analysis statistical difference was observed (Table 8).
Harms
Healing was uneventful for all test and control patients. No clinical complications were reported.
Discussion
Limitations
Differences in patient perceptions can influence the levels of reported postoperative pain [29].
A crossover study design, in which patients have SeCTG + CAF and SeCTG + TT procedures performed at different times, all by the same operator, may support the results presented in this paper.
This study utilized a VAS scale in an effort to accurately extract data regarding the patients’ pain and other experiences during early and late postoperative phases.
Common risks of undergoing periodontal surgical therapy include, but are not limited to, swelling, bleeding, pain, and infection [18]. Efforts have been made in the literature to compare different surgical interventions and the prevalence of such complications [17, 30, 31, 32]. An investigation by Curtis [17] found that patients undergoing osseous resective surgery had the highest occurrence of bleeding, infection, swelling, or adverse tissue changes. Although over half the study population reported minimal to no postoperative pain, mucogingival surgery was significantly more associated with pain and was 3.5 times more likely to cause pain when compared to osseous surgery. When analyzing a number of patient outcomes including postoperative pain following various periodontal procedures, Matthews and McCulloch [32] found soft tissue graft surgery to cause the most postoperative discomfort.
In spite of these findings and anecdotal inferences implying a great deal of discomfort or morbidity associated with mucogingival procedures, the present study showed contrasting results. Our findings are in agreement with those of Harris [19] who reported a minimal degree of complications when mucogingival procedures are performed.
Generalizability
The subepithelial connective tissue graft procedure is one of the most effective and predictable surgical procedures for the treatment of denuded root surfaces [2, 4]. In most of the available literature, pain assessment focused mostly on the tissue donor site [18, 20, 33] which is normally the palatal region proximal to the maxillary premolars. Minimal attention has been paid to the exclusive perception of pain emanating from the recipient area or overall oral cavity. No studies so far have addressed the patient morbidity when two different mucogingival surgical techniques were performed at the recipient site. Improving patient outcomes is important in clinical practice.
The postoperative sequelae induced by the microsurgical tunneling flap procedure and the coronally advanced flap in combination with a subepithelial connective tissue graft have been investigated in this paper. The tunneling technique has recently gained popularity in mucogingival surgery both around dental implants and natural dentition [11, 12]. Only one randomized controlled clinical trial is reported in the literature comparing the clinical efficacy of the tunneling technique and the coronally advanced flap (in conjunction with enamel matrix derivate) in terms of root coverage [11]. The aforementioned study shows significantly better clinical outcomes of the tunneling technique when compared to the CAF. Twelve months post intervention, the mean percentage of root coverage achieved in the tunnel group was 98.4 vs. 71.8 % in the CAF group and the complete root coverage was 78.6 % of sites treated with the tunneling technique compared to 21.4 % in CAF-treated sites. The evidence in the published literature supports that the presence of the SeCTG is a prerequisite for a higher predictability in the treatment of gingival recession [34].
The tunneling technique needs to be combined with a SeCTG or soft tissue substitute. In order to overcome the certain limitations in flap mobility and advancement of the TT, it is possible to leave a small collar of the SeCTG uncovered without risking the necrosis of the entire graft. The TT provides a good option for the treatment of gingival recession; however, it has clinical limitations in regard to the treatment of deep single recession defects: in these instances, due to the limited flap mobility, an unfavorable high amount of the graft would have to be left uncovered, presumably undergoing subsequent necrosis. For this reason, defects deeper than 5 mm were excluded from this clinical trial.
Interpretation
In the present study, both techniques were shown to be clinically effective in the treatment of gingival recessions. The percentage of root coverage was 86 % (SD 17 %), and the number of patients with complete root coverage in the entire sample was 28 (56 %).
In the SeCTG + TT group, measurements decreased significantly in GH (from 3.48 to 0.56; p < 0.001) and CAL (from 4.72 to 1.84; p < 0.001). A significant increase was observed in KTH (from 2.24 to 4.84; p < 0.001). No difference was observed in PD (p = 0.705).
Similar results were found in the SeCTG + CAF groups; measurements decreased significantly in GH (from 3.44 to 0.52; p < 0.001) and CAL (from 4.72 to 1.8; p < 0.001). A significant increase was observed in KTH (from 2.24 to 3.92; p < 0.001). No difference was observed in terms of PD (p = 1.000). No differences were observed in the percentage of root coverage (87 vs. 85 %; p = 704) or patients with complete root coverage (60 vs. 52 %; p = 0.569).
The surgical chair time required to develop a tunnel has been shown to be significantly higher than that in the SeCTG + CAF group. On average, the surgeon required 33.6 (3.6) and 23.6 (4.2) min for the SeCTG + TT and the SeCTG + CAF, respectively. A positive linear correlation was observed between surgical time and use of analgesic medication (r = 0.456, p = 0.001). In other words, the longer the surgery, the greater the dosage of the painkillers consumed. This may be explained in that the preparation of an adequate tunnel requires extreme care and attention in particular in patients with a thin gingival soft tissue. The dissection is made through the gingival sulcus, making the procedure more complicated and time consuming rather than the coronally advanced procedure. In addition, in order to adequately prepare a tunnel, the area of interest has to be extended at least one tooth mesial and one tooth distal; this could explain why the SeCTG + CAF group has less pain or discomfort in all four aspects of the questionnaire: pain experienced within the mouth as a whole, pain experienced throughout the day, pain experienced at night, and edema experienced after the surgery (p = 0.002, p = 0.001, p = 0.001, and p = 0.001, respectively).
No significant difference was demonstrated between the control and the test patients in terms of the other VAS-related parameters: pain expressed while drinking (p = 0.686), pain expressed while chewing (p = 0.202), and pain expressed in the morning (p = 0.788). The percentage of patients that would be willing to go through this surgery again is similar in both groups (76 vs. 84 %; p = 0.724) and the percentage of patients that did experience bleeding is higher in SeCTG + CAF, but no statistically significant difference was observed between groups (p = 0.667), suggesting that both treatments are well tolerated by patients. The pain perception and oral function gradually improved during the first week, but social and recreational activities and daily routines are affected, especially during the first three postoperative days [35–37]; that is why in the current study, the authors asked the patients to record the pain perception and the discomfort during the first 3 days post intervention.
Conclusions
Both SeCTG + TT and CAF + SeCTG rendered satisfactory clinical outcomes. Both treatments showed similar efficacy in terms of percentage of root coverage (87 vs. 85 %; p = 704) or patients with complete root coverage (60 vs. 52 %; p = 0.569). Healing was uneventful for both test and control patients.
The SeCTG + TT group required longer chair time and higher painkiller assumption. Patients treated with SeCTG + CAF reported significantly less pain or discomfort in all four sections of the questionnaire: pain experienced within the mouth as a whole, pain experienced throughout the day, pain experienced at night, and edema experienced after the surgery (p = 0.002, p = 0.001, p = 0.001, and p = 0.001, respectively).
Notes
Vicryl, Johnson & Johnson; Woluwe, Belgium
Vicryl, Johnson & Johnson; Woluwe, Belgium
Vicryl, Johnson & Johnson; Woluwe, Belgium
Vicryl, Johnson & Johnson; Woluwe, Belgium
Hu-Friedy, Chicago, IL, USA
References
Bouchard P, Malet J, Borghetti A (2001) Decision-making in aesthetics: root coverage revisited. Periodontol 2000 27:97–120
Roccuzzo M, Bunino M, Needleman I, Sanz M (2002) Periodontal plastic surgery for treatment of localized gingival recessions: a systematic review. J Clin Periodontol 29:178–194
Clauser C, Nieri M, Franceschi D, Pagliaro U, Pini-Prato G (2003) Evidence-based mucogingival therapy. Part 2: ordinary and individual patient data meta-analyses of surgical treatment of recession using complete root coverage as the outcome variable. J Periodontol 74:741–756
Cairo F, Pagliaro U, Nieri M (2008) Treatment of gingival recession with coronally advanced flap procedures: a systematic review. J Clin Periodontol 35:136–162
Oates TW, Robinson M, Gunsolley JC (2003) Surgical therapies for the treatment of gingival recession. A systematic review. Ann Periodontol 8:303–320
Pagliaro U, Nieri M, Franceschi D, Clauser C, Pini-Prato G (2003) Evidence-based mucogingival therapy. Part 1: a critical review of the literature on root coverage procedures. J Periodontol 74:709–740
Langer B, Langer L (1985) Subepithelial connective tissue graft technique for root coverage. J Periodontol 56(12):715–720
Zucchelli G, Clauser C, De Sanctis M, Calandriello M (1998) Mucogingival versus guided tissue regeneration procedures in the treatment of deep recession type defects. J Periodontol 69:138–145
Zucchelli G, Amore C, Sforza NM, Montebugnoli L, De Sanctis M (2003) Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J Clin Periodontol 30:862–870
Allen EP, Miller Jr PD (1989) Coronal positioning of existing gingiva: short term results in the treatment of shallow marginal tissue recession. J Periodontol 60:316–319
Zuhr O, Rebele SF, Schneider D, Jung RE, Hürzeler MB (2014) Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part I. Clinical and patient-centred outcomes. J Clin Periodontol 41:582–592
Rebele SF, Zuhr O, Schneider D, Jung RE, Hürzeler MB (2014) Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part II. Volumetric studies on healing dynamics and gingival dimensions. J Clin Periodontol 41:593–603
Burkhardt R, Lang NP (2005) Coverage of localized gingival recessions: comparison of micro- and macrosurgical techniques. J Clin Periodontol 32:287–293
Bittencourt S, Del Peloso Ribeiro E, Sallum EA, FH NJ, Casati MZ (2012) Surgical microscope may enhance root coverage with subepithelial connective tissue graft: a randomized-controlled clinical trial. J Periodontol 83:721–730
Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, Etienne D (2010) Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol 37:88–97
Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M (2009) Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: a comparative controlled randomized clinical trial. J Periodontol 80:1083–1094
JW Jr Curtis, McLain JB, Hutchinson RA. The incidence and severity of complications and pain following periodontal surgery. J Periodontol 1985;56: 597–601
Griffin TJ, Cheung WS, Zavras AI, Damoulis PD (2006) Postoperative complications following gingival augmentation procedures. J Periodontol 77:2070–2079
Harris RJ, Miller R, Miller LH, Harris C (2005) Complications with surgical procedures utilizing connective tissue grafts: a follow-up of 500 consecutively treated cases. Int J Periodontics Restorative Dent 25:449–459
Wessel JR, Tatakis DN (2008) Patient outcomes following subepithelial connective tissue graft and free gingival graft procedures. J Periodontol 79:425–430
Schulz KF, Altman DG, Moher D, CONSORT Group (2011) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 9:672–677
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 23(340):c869
Jr MPD (1985) A classification of marginal tissue recession. Int J Periodontics Restorative Dent 5:8–13
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38
Bruno JF (1994) Connective tissue graft technique assuring wide root coverage. Int J Periodontics Restorative Dent 14:126–137
Zucchelli G, De Sanctis M (2000) Treatment of multiple recession-type defects in patients with esthetic demands. J Periodontol 71:1506–1514
Allen EP (1988) Use of mucogingival surgical procedures to enhance esthetics. Dent Clin N Am 32:307–330
Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M (2009) Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 36:868–876
Saroff SA, Chasens AI, Eisen SF, Levey SH (1982) Free soft tissue autografts. Hemostasis and protection of the palatal donor site with a microfibrillar collagen preparation. J Periodontol 53:425–428
Marchi A, Vellucci R, Mameli S, et al. (2009) Pain biomarkers. Clin Drug Investig 29:41–46
Pulvers K, Hood A (2013) The role of positive traits and pain catastrophizing in pain perception. Curr Pain Headache Rep 17:330
Matthews DC, McCulloch CA (1993) Evaluating patient perceptions as short-term outcomes of periodontal treatment: a comparison of surgical and non-surgical therapy. J Periodontol 64:990–997
Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, de Sanctis M (2010) Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: a comparative randomized-controlled clinical trial. J Clin Periodontol 37:728–738
Cortellini P, Tonetti M, Baldi C, Francetti L, Rasperini G, Rotundo R, Nieri M, Franceschi D, Labriola A, Prato GP (2009) Does placement of a connective tissue graft improve the outcomes of coronally advanced flap for coverage of single gingival recessions in upper anterior teeth? A multi-centre, randomized, double-blind, clinical trial. J Clin Periodontol 36:68–79
Conrad SM, Blakey GH, Shugars DA, Marciani RD, Phillips C, Jr WRP (1999) Patients’ perception of recovery after third molar surgery. J Oral Maxillofac Surg 57:1288–1294
Snyder M, Shugars DA, White RP, Phillips C (2005) Pain medication as an indicator of interference with lifestyle and oral function during recovery after third molar surgery. J Oral Maxillofac Surg 63:1130–1137
Sato FRL, Asprino L, de Araújo DES, de Moraes M (2009) Short-term outcome of postoperative patient recovery perception after surgical removal of third molars. J of Oral and Maxillofac Surg 67:1083–1091
Acknowledgments
The authors would like to thank Cristiano Tomasi, DDS, MSc, Odont Dr. (PhD), Department of Periodontology, Institute of Odontology, the Sahlgrenska Academy at the University of Gothenburg, for his guidance and invaluable assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This prospective study was performed in accordance with the guidelines of the 1964 Declaration of Helsinki, and the research protocol was approved by the Ethics Committee of the University of Padova (No.: 2566P), prior to patient enrollment. Additionally, this clinical study was registered at the US National Institutes of Health Clinical Trials Registry (NCT02269748). Patients were notified that their data would be collected and used for a statistical analysis. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
The authors declare that they have no competing interests.
Funding
The authors declare that they received no funds or reimbursements for the completion of the study. The authors report no financial and personal relationships with other people or organizations that could inappropriately influence this paper.
Informed consent
A signed informed consent was obtained from all patients enrolled in this study.
Rights and permissions
About this article
Cite this article
Gobbato, L., Nart, J., Bressan, E. et al. Patient morbidity and root coverage outcomes after the application of a subepithelial connective tissue graft in combination with a coronally advanced flap or via a tunneling technique: a randomized controlled clinical trial. Clin Oral Invest 20, 2191–2202 (2016). https://doi.org/10.1007/s00784-016-1721-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1721-7