Abstract
Bone metastasis is a common complication in several solid cancers, including breast, prostate, and lung. In the bone microenvironment, metastatic cancer cells disturb bone homeostasis leading to osteolytic or osteosclerotic lesions. Osteolytic lesions are characterized by an increased osteoclast-mediated bone resorption while osteosclerotic lesions are caused by enhanced activity of osteoblasts and formation of poor-quality bone. A common feature in bone metastasis is the complex interplay between the cancer cells and the cells of the bone microenvironment, which can occur already before the cancer cells enter the distant site. Cancer cells at the primary site can secrete soluble factors and extracellular vesicles to bone to create a “pre-metastatic niche” i.e., prime the microenvironment permissive for cancer cell homing, survival, and growth. Once in the bone, cancer cells secrete factors to activate the osteoclasts or osteoblasts and the so called “vicious cycle of bone metastases”. These pathological cell–cell interactions are largely dependent on secreted proteins. However, increasing evidence demonstrates that secreted RNA molecules, in particular small non-coding microRNAs are critical mediators of the crosstalk between bone and cancer cells. This review article discusses the role of secreted miRNAs in bone metastasis development and progression, and their potential as non-invasive biomarkers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone is the preferred site of metastatic growth for many different cancers. Bone metastases are associated with pathological fractures, pain, hypercalcemia, and an increased morbidity and mortality [1]. Bone is highly vascularized and rich in growth factors, which makes it an attractive and supporting milieu for cancer cells to home to and grow in. According to the “seed and soil theory” proposed by Sir Stephen Paget already in 1889, the bone (soil) provides an ideal microenvironment for cancer cells (seed) to colonize, survive and proliferate [2]. He also hypothesized that metastasis is not a random process but occurs in a coordinated manner. Indeed, later studies have shown that the primary tumor can send signals to the future metastatic site to prepare a “pre-metastatic niche” for the arriving cancer cells [3]. During this process, cancer-derived soluble factors and extracellular vesicles disturb the homeostasis of the distant organ to make it conductive to the survival of tumor cells.
Bone homeostasis is maintained by the coordinated actions of bone resorbing osteoclasts and bone forming osteoblasts. Osteoclasts are multinucleated cells derived from the hematopoietic lineage precursors. Osteoclast differentiation is induced by macrophage colony stimulating factor (M-CSF) as well as receptor-activator of nuclear kappa-B ligand (RANKL), which binds on the receptor RANK on monocytes. Mature active osteoclasts demineralize bone by creating an acidic environment in the so-called resorption lacuna through release of protons. This is followed by secretion of proteases including cathepsin K and matrix metalloproteases, which degrade organic bone matrix [4]. New bone is then formed by osteoblasts. Osteoblasts differentiate from mesenchymal precursors through a regulated process involving transcription factors Runt-related transcription factor 2 (Runx2) and Osterix (Osx), among others. Mature osteoblasts are characterized by expression alkaline phosphatase, osteocalcin, and type I collagen and deposit organic matrix during bone formation [5]. As long as new bone is formed to the same extent old bone is removed, bone mass remains constant. However, in various pathological processed, including bone metastases, the balance is disturbed leading to bone loss or abnormal bone formation.
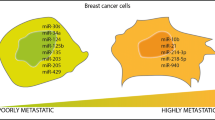
Although the basic principles of physiological and pathological bone remodeling are well established, novel regulatory molecules are still being revealed. The discovery of non-coding RNAs as key regulators of various biological processes raised the question whether they are also implicated in bone homeostasis. Indeed, during the last decade short and long non-coding RNAs have been emerged as key regulators of bone development, homeostasis, and pathology [6]. The best characterized non-coding RNAs are microRNAs (miRNAs), short RNAs that post-transcriptionally reduce mRNA abundance. miRNAs are dysregulated in various bone disorders and individual miRNAs functionally maintain/disturb bone remodeling in disease conditions, such as bone metastases. Several miRNAs have been shown to be up- or downregulated in primary breast cancer and/or bone metastases. Future studies will show whether matched primary tumors and bone metastases have a similar miRNA profile like shown in gastrointestinal tumors [7] or whether the distant microenvironment induces changes in the miRNA profile as shown in patients with primary breast cancer and matched lymph node metastases [8]. The function of miRNAs in bone metastases as well as their role as potential therapeutic targets has been reviewed elsewhere [9,10,11,12]. This manuscript will focus on secreted miRNAs and discuss their relevance in bone metastasis development and progression. In addition, the potential of using circulating miRNAs as non-invasive biomarkers in metastatic bone disease will be discussed (Fig. 1).
Circulating miRNAs in bone metastases. A miRNAs can be secreted from the primary tumor in extracellular vesicles or bound to proteins. In bone, these miRNAs can contribute to the early stages of bone metastases, for instance by preparing the “pre-metastatic niche”. B Secreted miRNAs contribute to osteosclerotic metastases by promoting (green letters) or inhibiting (red letters) osteoblast differentiation. C Several miRNAs promote osteoclast differentiation and facilitate the progression of osteolytic bone metastases. The figure was created using Biorender.com
Bone metastasis
Bone is the most common site of metastasis in breast and prostate cancer. In addition, other solid cancers, including lung and kidney frequently metastasize to bone. Bone metastases can cause severe pain, pathological fractures, hypercalcemia, and reduced mobility. Due to these complications, patients with bone metastases suffer from a rapid decline in the quality of life. The most frequent skeletal sites of metastases are the spine, pelvis, ribs, proximal femur, and the skull. Patients with bone metastases have increased mortality, with a median survival varies between 6 and 7 months in lung cancer up to 53 months in prostate cancer [13]. Treatment of bone metastases requires a multidisciplinary team and is aimed at reducing pain, preventing and treating fractures, controlling local tumor and maintaining the quality of life of the patients. Current therapies include radiotherapy, chemotherapy, and bone-targeted therapies. In addition, orthopedic interventions such as kyphoplasty or spinal decompression may be needed. Despite the improved treatment options, treatment is palliative and the disease incurable.
In physiological conditions, bone homeostasis is maintained by highly coordinated actions of osteoclasts that resorb old bone and osteoblasts that build new bone. Cancer cells disturb the tight regulation between osteoclast and osteoblasts, leading to pathologically increased activation of osteoclasts or osteoblasts and consequently to osteolytic or osteoblastic lesions, respectively. Osteolytic lesions are often more aggressive than osteoblastic lesions. Osteolytic lesions are more common in lung, kidney, and breast cancer while prostate cancer metastases are characterized by osteoblastic lesions. However, often mixed osteoblastic and osteolytic lesions are found in patients with breast and prostate cancer metastases [14]. Osteoblastic and osteolytic lesions differ in their clinical presentation and molecular characteristics [13]. However, the common feature for both types of lesions is that imbalance between osteoclasts and osteoblasts occurring in response to the tumor. This imbalance is mediated by numerous factors secreted by the cancer cells as well as the cells of the bone microenvironment. Besides the well-established contribution of proteins and peptides in the cellular crosstalk in the bone marrow microenvironment, recently also RNA molecules have been recognized as important intercellular mediators.
MicroRNA biogenesis and mode of action
microRNAs (miRNAs) are a class of short non-coding RNAs that function as crucial regulators of mRNA and protein abundance [15]. MiRNAs were originally discovered in Caenorhabditis Elegans in 1993 by two independent groups. They proposed that lin-4 is a small non-coding RNA, which regulates lin-14 at a post-transcriptional level through complementary binding on its 3’ untranslated region (UTR) [16, 17]. Since this fundamental discovery, miRNA-mediated mechanisms were found to be highly conserved, and miRNAs have been identified in all animal systems. To date, over 2000 miRNAs have been detected in humans and they are estimated to regulate one third of the genes. In the canonical miRNA biogenesis pathway, miRNAs are transcribed from the DNA into primary miRNAs (pri-miRNAs), which are processed by the microprocessor complex (Drosha and DiGeorge Syndrome Critical Region (DGCR8) to precursor-miRNAs (pre-miRNAs). The pre-miRNA molecule is exported to the cytoplasm via Exportin5 and processed by the RNAse III endonuclease Dicer to produce the mature miRNA duplex [17]. The miRNA duplex consists of 3’ and 5’ strands, of which both can be loaded into the Argonaute (AGO) family of proteins to form an RNA-induced silencing complex (RISC). The unloaded strand will be unwound and degraded. In addition to the canonical biogenesis, miRNAs can be also processed through multiple non-canonical biogenesis pathways, which are reviewed elsewhere [18]. Both canonical and non-canonical maturation pathways lead to a functional RISC complex, which binds to the target mRNA through complementary binding. Usually miRNAs bind to the 3’UTR of the target to induce mRNA decay or interfere with protein translation. However, miRNAs have also been shown to interact with the 5’UTR, coding regions and promotes of their target [19].
While the main function of miRNAs is intracellular interference with mRNA, miRNAs can also be secreted and have been identified in various biological fluids including plasma, serum and urine. Extracellular miRNAs are protected from the extracellular environment and thus resist temperature and pH-induced degradation. The protection of miRNAs is often provided by extracellular vesicles (EVs). Indeed, miRNAs have been isolated from exosomes, microvesicles and apoptotic bodies. Another form miRNAs circulate is bound to proteins, such as AGO2 or high-density lipoprotein (HDL) [20]. Recent evidence shows that circulating miRNAs can be delivered to other, even distant cells and act in autocrine and paracrine manners to regulate recipient cell function. The following chapters will discuss the role of extracellular miRNAs in different stages and types of bone metastases.
Secreted miRNAs in early stages of bone metastases
The role of various proteins in early and late stages of bone metastases is well established [21]. For instance, in very early stages of the disease, lysyl oxidase (LOX), secreted by hypoxic breast cancer cells in the primary site has been shown to recruit bone marrow cells to create a fertile soil (called “pre-metastatic niche”) for disseminated tumor cells [22]. Interestingly, increasing evidence suggests that tumor-derived exosomes can also contribute to this process and guide organotrophic metastasis [23]. Studies with prostate cancer further demonstrated that the miRNA cargo of cancer -derived EVs plays a key role in the communication between cancer cells and the bone marrow stroma [24]. While prostate cancer cell-derived EVs increased osteoblast proliferation, depletion of Dicer and thus miRNA maturation abrogated the effect, indicating that EV-derived mature miRNAs are transferred and exhibit a biological function in the recipient cells. Indeed, when the nascent RNA was labelled with 5-Ethynyl Uridine in PC3 prostate cancer cells and EVs collected from these cells were incubated with osteoblasts, 5-EU labelled miR-21 was detected in the recipient cells [24]. Further functional studies demonstrated that miR-21 regulates cell viability in osteoblasts. Interestingly, breast cancer-derived exosomal miR-21 has been shown to activate osteoclasts very early during disease progression, which likely contributes to preparation of the pre-metastatic niche [25]. The importance of exosomes in bone colonization has also been shown in lung cancer. Lung cancer cell -derived exosomes enriched in miR-192 prevented angiogenesis in the bone marrow through inhibition of the pro-angiogenic proteins CXCL1 and Interleukin 8 resulting in reduced bone colonization and metastatic growth [26]. Together these studies indicate that circulating miRNAs play an important role in early stages of bone metastasis.
MiRNAs as mediators of tumor growth in bone
Similarly, proteins mediating cellular interactions in the bone marrow during metastasis progression are relatively well established. Breast cancer and other cancers inducing osteolytic lesions secrete cytokines, such as parathyroid hormone-related peptide (PTHrP) that stimulate the osteoblasts to produce excessive amounts of RANKL. RANKL in turn activates the osteoclasts and upon increased bone destruction, transforming growth factor beta (TGF-β) and other growth factors are released from the bone matrix. These factors further support tumor growth, creating the so-called vicious cycle of bone metastases [21]. Similarly, osteoblastic lesions are initiated by tumor-derived factors, including platelet-derived growth factor (PDGF), insulin-like growth factors (IGFs) and adrenomedullin that induce abnormal osteoblast activity [14]. Recent findings have revealed that not only proteins but also miRNAs mediate these complex interactions between cancer cells and the cells of the bone microenvironment. The following two sections discuss how secreted miRNAs regulate tumor growth in bone leading to osteosclerotic and osteolytic lesions, respectively.
MiRNAs in osteosclerotic metastases
Osteosclerotic metastases are due to an increased proliferation and differentiation of osteoblasts. Several studies have shown that prostate cancer cell-derived exosomes increase osteoblast survival, proliferation, differentiation, and mineralization [27]. Further characterization of the exosomes revealed that several miRNAs contribute to this phenotype, including miR-940 and miR-141-3p [28, 29]. miR-141-3p is highly expressed and secreted by prostate cancer cells that cause osteoblastic lesions and transferred into osteoblasts in vitro. Functionally, exosomal miR-141-3p increased osteoblast activity in vitro by targeting a Rho GTPase activating protein DLC1 (deleted in lung cancer 1) and consequently activating the MAPK pathway. Consistently, prostate cancer-derived exosomal miR-141-3p increased osteoblast activity in vivo and increased the development of osteoblastic lesions in the bone [29]. In addition to miR-141, miR-940 is highly abundant in exosomes isolated from osteoblastic phenotype-inducing prostate cancer cells compared to cell lines inducing an osteolytic phenotype [28] Exosomal miR-940 was further shown to stimulate osteoblast differentiation by targeting another Rho GTPase-activating protein ARHGAP1 and FAM134A. Interestingly, implantation of osteolytic MDA-MB-231 breast cancer cells overexpressing miR-940 in mice increased osteoblast differentiation of host mesenchymal stromal cells resulting in abundant osteoblastic lesions in these animals [28]. These results show that exosomal miRNAs are not only able to promote the intrinsic phenotype but also revert the lesion type in the host microenvironment.
Interestingly, prostate cancer cell-derived exosomal miRNAs have also been reported to reduce osteoblast differentiation and function. Although human prostate cancer cell line MDA PCa 2b is known to induce osteoblastic lesions, exosomal miR-92-1-5p was shown to reduce osteoblast mineralization in vitro. In contrast, it increased mRNA expression of osteoclast markers and increased TRAP activity of an osteoclast precursor cell line RAW 264.7 in vitro, which was reversed by miR-92-1-5p treatment [30]. In vivo, miR-92-1-5p degraded extracellular matrix and promoted tumor growth by targeting collagen Type 1 alpha 1 (COL1A1). Similarly, exosomal miR-26a-5p, miR-28a-3p and miR-30e-5p derived from RM1-BM prostate cancer cells reduced osteoblast mineralization in vitro and in vivo [31]. However, prostate cancer cell-derived exosomes increased metabolic activity, viability, and proliferation of osteoblast precursors, suggesting that at least in this model, exosomal miRNAs might increase the initial osteoblast activity required for osteosclerotic lesions, while other mechanisms might be at play during disease progression.
MiRNAs in osteolytic metastases
Osteoclasts are the key drivers of osteolytic metastases and target cells of several secreted miRNAs. For instance, miR-20a is highly abundant in exosomes derived from MDA-MB-231 breast cancer cells. Exosomal miR-20a enhanced osteoclast differentiation by direct targeting of src kinase inhibitor 1 (SRCIN1), a negative regulator of cancer cells growth and osteoclast differentiation [32]. While some miRNAs are specific to certain cell types, conserved mechanisms have also been unraveled. For instance, miR-21 is expressed and secreted by metastatic breast cancer cells as well as in lung adenocarcinoma cells [25, 33]. Exosomal miR-21 derived from both cell types enhanced osteoclast differentiation by down-regulating programmed cell death 4 (PDCD4), an inhibitor of osteoclast differentiation and function [25, 33]. Consequently, breast cancer cell-derived miR-21 increased bone metastatic burden and accelerated bone lesions in vivo [25]. Similarly, miR-214, which is expressed and secreted by lung and breast cancer cells activates osteoclast differentiation, thereby fueling the vicious cycle and promoting tumor growth in bone [34]. In mice bearing breast cancer bone metastases, exosomal miR-214-3p increased osteoclast number in the bones and bone resorption as indicated by an increased serum bone resorption marker type I collagen cross-linked C-telopeptide (CTX-1). Mechanistically, miR-214-3p directly targets TNF receptor-associated factor 3 (TRAF3), a negative regulator of RANKL-induced osteoclast differentiation [35].
Secreted miRNAs and proteins can also act synergistically to induce osteolytic metastases. Recently, exosomes derived from estrogen receptor -positive (ER +) breast cancer cells were shown to contain high amounts of integrin-binding sialoprotein (IBSP) and miR-19a, which cooperated to promote bone metastases [36]. First, IBSP created an osteoclast-rich environment in bone by recruiting osteoclast precursors cells. Exosomal miR-19a is taken up by the osteoclasts, in which miR-19a directly targets PTEN and activates the AKT pathway to promote osteoclast differentiation. Ectopic expression of both PTEN and miR-19a in breast cancer cells increased bone metastasis and bone destruction without affecting breast cancer growth in the mammary fat pad. Furthermore, depletion of miR-19a in ER+ breast cancer cells protected from breast cancer-induced bone destruction and reduced tumor growth [36]. Intriguingly, pharmacological inhibition of miR-19a/b using anti-sense oligonucleotides was recently demonstrated to prevent bone loss in osteoporosis [37]. This was due to a concomitant increase in osteoblast differentiation and function and reduced osteoclast-mediated bone resorption. These findings together suggest that inhibiting miR-19 could provide an attractive novel therapeutic approach to treat bone metastases and other bone loss conditions.
Circulating miRNAs as biomarkers
An important translational aspect of extracellular miRNAs is their potential use as circulating biomarkers in various diseases. Although a clinically relevant miRNA-based biomarker for bone metastasis has not been established yet, aberrant expression of circulating miRNAs has been associated with metastatic bone disease.
In breast cancer patients, miR-21 in serum exosomes was detected at significantly higher level in patients with bone metastasis compared with patients with no metastasis or patients with non-bone metastasis. However, further analysis revealed no association between serum miR-21 and age of the patients, cancer subtype (invasive breast cancer vs. invasive ductal carcinoma, HER2+ vs. luminal HER+) or stage (stage II vs. stage III) [25]. In contrast, miR-19a was found to be increased in the circulation specifically in patients with ER+ breast cancer [36]. Kaplan–Meier analysis revealed that high miR-19a level was positively associated with metastatic disease in patients with ER+ breast cancer. No correlation was found between miR-19a and metastasis free survival in patients with ER- breast cancer. These findings were further confirmed when exosomal miR-19a was analyzed in patients with ER+ , Her+ and triple negative breast cancer without metastasis, ER+ and ER- breast cancer with non-bone metastases and ER+ and ER- breast cancer with bone metastases. Interestingly, miR-19a was elevated in blood exosomes only in patients with ER+ cancer with bone metastases compared to all other groups [36]. Similarly, circulating IBSP, which was shown to co-operate with miR-19a to promote bone metastases, was upregulated in the in the bone tissue and in the serum of patients with ER+ breast cancer and bone metastases. Interestingly, when the patients were stratified in three groups miR-19alow; IBSPlow, miR-19a or IBSP high and miR-19high; IBSPhigh, ER+ breast cancer patients with bone metastases were significantly associated with miR-19high; IBSPhigh. Finally, the median recurrence free survival in patients with ER+ breast cancer was markedly lower in patients with high expression of both miR-19a and IBSP compared to patients with high expression of either miR-19a or IBSP or low expression of both. The relevance of using a miRNA-protein combination as a circulating determinant of bone metastasis was also shown with miR-16, miR-378 and soluble intracellular adhesion molecule 1 (sICAM1) [38]. Osteoclast-derived miR-16 and miR-378 were shown to be elevated in the serum of patients with bone metastases compared to healthy individuals, possibly reflecting the hyperactivation of osteoclasts in these patients. Interestingly, the expression of miR-16 and miR-378 correlated with serum sICAM1, a tumor-derived factor associated with miRNA changes during bone metastases. Similar to miR-16 and miR-378, sICAM1 was elevated in serum of breast cancer patients with bone metastases compared to healthy donors or breast cancer patients showing no occurrence of bone metastasis. A strong correlation was observed between miR-16 and sICAM1 as well as miR-378 and sICAM in patients with bone metastases but not in healthy individuals [38]. These results provide very promising perspectives of using miRNAs as biomarkers for bone metastasis either alone or in combination with other circulating markers.
References
Weilbaecher KN, Guise TA, McCauley LK (2011) Cancer to bone: a fatal attraction. Nat Rev Cancer 11:411–425. https://doi.org/10.1038/nrc3055
Paget S (1889) The distribution of secondary growths in cancer of the breast. Lancet 133:571–573
Peinado H, Zhang H, Matei IR et al (2017) (2017) Pre-metastatic niches: organ-specific homes for metastases. Nat Rev Cancer 17:302–317. https://doi.org/10.1038/nrc.2017.6
Kim JM, Lin C, Stavre Z et al (2020) Osteoblast-osteoclast communication and bone homeostasis. Cells. https://doi.org/10.3390/CELLS9092073
Ponzetti M (2021) Rucci N (2021) Osteoblast differentiation and signaling: established concepts and emerging topics. Int J Mol Sci 22:6651. https://doi.org/10.3390/IJMS22136651
Taipaleenmäki H (2018) Regulation of bone metabolism by microRNAs. Curr Osteoporos Rep 16:1–12. https://doi.org/10.1007/s11914-018-0417-0
Elango R, Alsaleh KA, Vishnubalaji R et al (2020) MicroRNA expression profiling on paired primary and lymph node metastatic breast cancer revealed distinct microRNA profile associated with LNM. Front Oncol 10:756. https://doi.org/10.3389/FONC.2020.00756/BIBTEX
Ravegnini G, Serrano C, Ricci R et al (2021) miRNA landscape in primary tumors and matched metastases in gastrointestinal stromal tumors. Epigenomics 13:369–377. https://doi.org/10.2217/EPI-2020-0303
Hesse E, Taipaleenmäki H (2019) MicroRNAs in bone metastasis. Curr Osteoporos Rep 17:122–128. https://doi.org/10.1007/s11914-019-00510-4
Haider M-T, Taipaleenmäki H (2018) Targeting the metastatic bone microenvironment by microRNAs. Front Endocrinol (Lausanne) 9:202. https://doi.org/10.3389/fendo.2018.00202
Haider MT, Smit DJ, Taipaleenmäki H (2022) MicroRNAs: emerging regulators of metastatic bone disease in breast cancer. Cancers (Basel). https://doi.org/10.3390/CANCERS14030729
Browne G, Taipaleenmäki H, Stein GS et al (2014) MicroRNAs in the control of metastatic bone disease. Trends Endocrinol Metab 25:320–327. https://doi.org/10.1016/j.tem.2014.03.014
Fang J, Xu Q (2015) Differences of osteoblastic bone metastases and osteolytic bone metastases in clinical features and molecular characteristics. Clin Transl Oncol 17:173–179. https://doi.org/10.1007/S12094-014-1247-X
Guise TA, Mohammad KS, Clines G et al (2006) Basic mechanisms responsible for osteolytic and osteoblastic bone metastases. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-06-1007
Puppo M, Taipaleenmäki H, Hesse E, Clézardin P (2021) Non-coding RNAs in bone remodelling and bone metastasis: mechanisms of action and translational relevance. Br J Pharmacol 178:1936–1954. https://doi.org/10.1111/BPH.14836
Lee RC, Feinbaum RL, Ambros V (1993) The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell 75:843–854. https://doi.org/10.1016/0092-8674(93)90529-Y
Zhang H, Kolb FA, Jaskiewicz L et al (2004) Single processing center models for human Dicer and bacterial RNase III. Cell 118:57–68. https://doi.org/10.1016/j.cell.2004.06.017
O J, H H, Z Y, P C (2018) Overview of microRNA Biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne). https://doi.org/10.3389/FENDO.2018.00402
Broughton JP, Lovci MT, Huang JL et al (2016) Pairing beyond the seed supports microRNA targeting specificity. Mol Cell 64:320–333. https://doi.org/10.1016/J.MOLCEL.2016.09.004
Vickers KC, Palmisano BT, Shoucri BM et al (2011) MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat Cell Biol 13:423–435. https://doi.org/10.1038/NCB2210
Zarrer J, Haider M-T, Smit DJ, Taipaleenmäki H (2020) Pathological crosstalk between metastatic breast cancer cells and the bone microenvironment. Biomolecules. https://doi.org/10.3390/biom10020337
Erler JT, Bennewith KL, Cox TR et al (2009) Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the pre-metastatic niche. Cancer Cell 15:35. https://doi.org/10.1016/J.CCR.2008.11.012
Hoshino A, Costa-Silva B, Shen TL et al (2015) (2015) Tumour exosome integrins determine organotropic metastasis. Nature 527:329–335. https://doi.org/10.1038/nature15756
Probert C, Dottorini T, Speakman A et al (2019) Communication of prostate cancer cells with bone cells via extracellular vesicle RNA; a potential mechanism of metastasis. Oncogene 38:1751. https://doi.org/10.1038/S41388-018-0540-5
Yuan X, Qian N, Ling S et al (2021) Breast cancer exosomes contribute to pre-metastatic niche formation and promote bone metastasis of tumor cells. Theranostics 11:1429–1445. https://doi.org/10.7150/THNO.45351
Valencia K, Luis-Ravelo D, Bovy N et al (2014) miRNA cargo within exosome-like vesicle transfer influences metastatic bone colonization. Mol Oncol 8:689–703. https://doi.org/10.1016/J.MOLONC.2014.01.012
Ollodart J, Contino KF, Deep G, Shiozawa Y (2022) The impacts of exosomes on bone metastatic progression and their potential clinical utility. Bone Rep. https://doi.org/10.1016/J.BONR.2022.101606
Hashimoto K, Ochi H, Sunamura S et al (2018) Cancer-secreted hsa-miR-940 induces an osteoblastic phenotype in the bone metastatic microenvironment via targeting ARHGAP1 and FAM134A. Proc Natl Acad Sci U S A 115:2204–2209. https://doi.org/10.1073/PNAS.1717363115
Ye Y, Li SL, Ma YY et al (2017) Exosomal miR-141–3p regulates osteoblast activity to promote the osteoblastic metastasis of prostate cancer. Oncotarget 8:94834–94849. https://doi.org/10.18632/ONCOTARGET.22014
Yu L, Sui B, Fan W et al (2021) Exosomes derived from osteogenic tumor activate osteoclast differentiation and concurrently inhibit osteogenesis by transferring COL1A1-targeting miRNA-92a-1–5p. J Extracell Vesicles. https://doi.org/10.1002/JEV2.12056
Furesi G, de Jesus Domingues AM, Alexopoulou D et al (2022) Exosomal miRNAs from prostate cancer impair osteoblast function in mice. Int J Mol Sci. https://doi.org/10.3390/IJMS23031285
Guo L, Zhu Y, Li L et al (2019) Breast cancer cell-derived exosomal miR-20a-5p promotes the proliferation and differentiation of osteoclasts by targeting SRCIN1. Cancer Med 8:5687–5701. https://doi.org/10.1002/CAM4.2454
Xu Z, Liu X, Wang H et al (2018) Lung adenocarcinoma cell-derived exosomal miR-21 facilitates osteoclastogenesis. Gene 666:116–122. https://doi.org/10.1016/J.GENE.2018.05.008
Zhang J, Wu J (2021) The potential roles of exosomal miR-214 in bone metastasis of lung adenocarcinoma. Front Oncol. https://doi.org/10.3389/FONC.2020.611054
Liu J, Li D, Dang L et al (2017) Osteoclastic miR-214 targets TRAF3 to contribute to osteolytic bone metastasis of breast cancer. Sci Rep. https://doi.org/10.1038/SREP40487
Wu K, Feng J, Lyu F et al (2021) Exosomal miR-19a and IBSP cooperate to induce osteolytic bone metastasis of estrogen receptor-positive breast cancer. Nat Commun. https://doi.org/10.1038/S41467-021-25473-Y
Taipaleenmäki H, Saito H, Schröder S et al (2022) Antagonizing microRNA-19a/b augments PTH anabolic action and restores bone mass in osteoporosis in mice. EMBO Mol Med. https://doi.org/10.15252/EMMM.202013617
Ell B, Mercatali L, Ibrahim T et al (2013) Tumor-induced osteoclast miRNA changes as regulators and biomarkers of osteolytic bone metastasis. Cancer Cell 24:542–556. https://doi.org/10.1016/j.ccr.2013.09.008
Acknowledgements
This work was funded by Deutsche Forschungsgemeinschaft (DFG), grant numbers TA 1154/1-2, and TA 1154/2-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Taipaleenmäki, H. Secreted microRNAs in bone metastasis. J Bone Miner Metab 41, 358–364 (2023). https://doi.org/10.1007/s00774-023-01424-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01424-z