Abstract
Introduction
Relationship of quantitative ultrasound (QUS) with high-resolution peripheral quantitative computed tomography (HR-pQCT), dual-energy X-ray absorptiometry (DXA), and bone-related biochemical markers was analyzed.
Materials and methods
The subjects were 480 individuals. Speed of sound (SOS) was measured by calcaneal QUS. Volumetric bone mineral density (vBMD) and microarchitecture of trabecular and cortical bone in the distal radius and tibia were assessed by HR-pQCT. Areal bone mineral density (aBMD) in the lumbar spine and proximal femur were measured by DXA. TRACP-5b, P1NP, 25 (OH) vitamin D, and pentosidine were evaluated by biochemical tests. The correlation of each parameter was analyzed for all subjects and by sex and age group.
Results
QUS was moderately correlated with Tb.vBMD and Tb.BV/TV in the radius and tibia. No correlation was seen with Ct.vBMD or cortical porosity (Ct.Po). Although a correlation was seen with cortical thickness (Ct.Th) in the tibia in all subjects, no correlation was seen in women aged ≥ 60 years.
QUS showed moderate correlations with aBMD in the proximal femur. Although moderate correlation was seen with aBMD in the lumbar spine in all subjects, no correlation was seen in subjects aged ≥ 60 years. No significant correlations were seen between QUS and biochemical markers.
Conclusions
Moderate correlations were seen between QUS and Tb.vBMD and microarchitecture in the radius and tibia and aBMD of the proximal femur. On the other hand, practically no correlations were seen with Ct.vBMD or Ct.Po and the bone-related biochemical markers. Only in middle age, moderate correlations were seen with Ct.Th in the tibia and with aBMD of the lumbar spine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures markedly reduce the activities of daily living of elderly persons and substantially increase healthcare costs. Screening for the early detection of patients with osteoporosis is therefore important to increase the healthy life expectancy of elderly persons and reduce healthcare costs.
To diagnose osteoporosis, measurements of the areal bone mineral density (aBMD) of the lumbar spine and proximal femur by dual-energy X-ray absorptiometry (DXA) are currently used [1, 2]. However, DXA requires a large space and is therefore not performed in many clinics. It also involves X-ray exposure, although at a very low dose.
Quantitative ultrasound (QUS) is a method of assessing bone strength using ultrasound mainly in the calcaneus. The device is small and portable, and the measurements can be performed easily and quickly and involve no X-ray exposure. However, QUS is considered to be of limited use in assessing fracture risk, and it is therefore not used to diagnose osteoporosis.
High-resolution peripheral quantitative computed tomography (HR-pQCT) has enabled human bone microarchitecture to be analyzed in vivo, which previously had not been possible [3]. Second-generation HR-pQCT, developed in 2014, has a voxel size of 61 μm, enabling bone microarchitecture to be evaluated more precisely, and it allows the trabecular structure to be measured directly [4]. By analyzing volumetric bone mineral density (vBMD), microarchitecture, and estimated bone strength, HR-pQCT enables fracture risk assessment superior to that allowed by DXA [5]. However, HR-pQCT is expensive, and facilities that can perform it are therefore limited in number. Consequently, it is used mainly for research rather than in routine clinical practice.
To the best of our knowledge, no large studies have examined the relationship between the measurements obtained with calcaneal QUS and the bone microarchitecture analyzed by HR-pQCT.
The purpose of this study were to examine the correlations between calcaneal QUS and vBMD and bone microarchitecture of the radius and tibia as analyzed by HR-pQCT, aBMD in the lumbar spine and proximal femur as evaluated by DXA, and bone-related biochemical markers.
Materials and methods
Study participants
The study participants were 480 individuals who participated in a cohort study conducted in Nagasaki City, Japan, that began in December 2015 (Japanese Study of Bone Microstructure and Mineral Density in a Normative Cohort Measured by HR-pQCT: J-CaraT study).
The inclusion criteria of the cohort study were age ≥ 20 years of either sex, and the exclusion criteria were as follows: history of fragility fractures of the proximal femur or vertebra (excluding occult vertebral fractures); conditions that causes secondary osteoporosis such as use of a corticosteroid, rheumatoid arthritis, paralysis resulting from stroke, severe renal impairment, early menopause, and hyperparathyroidism; and current use of an anti-osteoporosis drug (excluding vitamin D and calcium preparations). The participants were recruited by distributing flyers to local communities (companies, offices in hospitals, public halls, etc.).
The participants of the present study consisted of 240 men and 240 women, with 80 men and 80 women each in the age ranges from 20 to 39 years, 40 to 59 years, and 60 to 89 years. 80 participants from each age group were selected in the order of registration of the cohort study.
This study was approved by the Nagasaki University Hospital Clinical Research Ethics Committee (Registration Number: 15083105), and informed consent was obtained from all participants before enrollment.
QUS
Speed of sound (SOS) (m/s) of right calcaneus was measured using a QUS system (CM-200, Furuno Electric Co., Ltd., Hyogo, Japan).
DXA
aBMD (mg/cm2) was measured in the lumbar spine and proximal femurs using a DXA system (Lunar Prodigy Advance, GE Lunar, Madison, WI, USA). In the lumbar spine, aBMD was measured at L1–L4. Vertebrae that were fractured or severely deformed were excluded. For the proximal femurs, aBMD of the total hip and of the femoral neck was measured.
Biochemical tests
The following were measured in biochemical tests: serum calcium (Ca), serum phosphorus (P), the bone resorption marker tartrate-resistant acid phosphatase-5b (TRACP-5b), and the bone formation markers total type I procollagen N-terminal propeptide (total P1NP) and 25(OH) vitamin D. In addition, pentosidine was measured as a marker of bone collagen degradation [6].
Serum calcium was corrected if the serum albumin level was < 4 g/dL. The following formula was used for the correction: corrected serum calcium = serum calcium + (4 − serum albumin). TRACP-5b was measured by enzyme immunoassay (EIA) (Osteolinks TRAP-5b, SB Bioscience Co., Ltd., Tokyo, Japan) and total P1NP by electrochemiluminescence immunoassay (ECLIA) (Elecsys Total P1NP, Roche Diagnostics K.Ks., Tokyo, Japan). Measurement of 25 (OH) vitamin D was performed by chemiluminescent immunoassay (CLIA) (LIAISON 25 OH Vitamin D TOTAL, Hitachi Chemical Diagnostics Systems Co., Ltd., Tokyo, Japan), and pentosidine was measured by high-performance liquid chromatography (HPLC) using a laboratory developed test. The above tests were outsourced to a clinical laboratory testing company (LSI Medience Corporation, Tokyo, Japan).
HR-pQCT
The vBMD and bone microarchitecture of the distal radius and tibia were measured on the subject’s nondominant side using a second-generation HR-pQCT system (XtreamCT II, Scanco Medical, Brüttisellen, Switzerland). For the radius measurements, scanning was performed over a 10.2-mm range centered on the position at a distance equal to 4% of the forearm length proximal to the ulnar aspect of the surface of the distal radial joint. For the tibia measurements, scanning was performed over a 10.2-mm range centered on the position at a distance equal to 7.3% of the lower leg length proximal to the surface of the distal tibial joint [7]. The following imaging conditions were used based on the standard protocol: tube voltage, 68 kVp; tube current, 1460 µA; integration time, 43 ms; number of projections, 900; field of view, 140 mm; matrix, 2304 × 2304; voxel size, 60.7 μm; total number of slices, 168 [7]. The scanning time was 2 min, and the effective dose was 5 µSv. All images were evaluated for motion artifacts, and those with artifacts of grade 3 or higher were excluded [8].
The following parameters were measured: total bone mineral density (Tt.BMD, mg/cm3), total area (Tt.Ar, mm2), trabecular bone mineral density (Tb.vBMD, mg/cm3), trabecular bone volume fraction (Tb.BV/TV, %), trabecular number (Tb.N, 1/mm), trabecular thickness (Tb.Th, mm), trabecular separation (Tb.Sp, mm), trabecular area (Tb.Ar, mm2), cortical bone mineral density (Ct.vBMD, mg/cm3), cortical porosity (Ct.Po, %), cortical thickness (Ct.Th, mm), cortical area (Ct.Ar, mm2), and cortical perimeter (Ct.Pm, mm).
Statistical analysis
The correlations between SOS measured by QUS and the measurement values for DXA, the biochemical tests, and HR-pQCT were determined using Pearson's correlation coefficients. Because SOS was highly correlated with age (age: r = 0.61, height: r = 0.26, weight: r = 0.15), partial correlations adjusted by age was used between SOS and the measurement values for DXA, the biochemical tests, and HR-pQCT. The subjects were divided into 6 groups consisting of a male group and a female group that were each divided into 3 subgroups of subjects aged 20–39 years, 40–59 years, and 60–89 years, and the age-adjusted partial correlations were determined in each group. In all of the analyses, a difference was considered significant if the p-value was < 0.01 (IBM SPSS Statistics, version 22.0, IBM Corp, Armonk, NY).
Results
Characteristics of the study participants
The characteristics of the study participants are shown in Table 1. The mean height, weight, and body mass index were 169.3 ± 6.5 cm, 67.8 ± 10.1 kg, 23.6 ± 3.1 kg/m2 for the men and 156.3 ± 5.4 cm, 53.4 ± 9.1 kg, and 21.8 ± 3.5 kg/m2 for women. The mean Ca, P, TRACP-5b, and total P1NP are within normal range for both men and women, meanwhile the mean 25 (OH) vitamin D showed low values with 18.1 ± 6.2 for men and 13.8 ± 5.1 for women.
Simple correlations and partial correlations for all participants
The simple correlations and age-adjusted partial correlations between QUS and DXA, the biochemical tests, and HR-pQCT for all subjects are shown in Table 2.
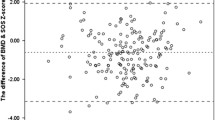
SOS was strongly negatively correlated with age for both men and women (overall: r = − 0.61, men: r = − 0.53, women: r = − 0.70). Scatterplots of age and SOS are shown in Fig. 1.
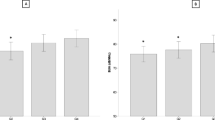
SOS showed moderate age-adjusted partial correlations with aBMD of the lumbar spine and the proximal femur measured by DXA (L1–L4: r = 0.42, total hip: r = 0.49, femoral neck: r = 0.46; Table 2, Fig. 2A).
In contrast, no significant correlations were seen between SOS and the biochemical test for Ca, P, TRACP-5b, total P1NP, 25 (OH) vitamin D, and pentosidine.
In the age-adjusted partial correlations with trabecular bone measured by HR-pQCT, SOS was moderately correlated with Tb.vBMD and Tb.BV/TV in the radius and tibia (r = 0.45, 0.44, 0.52, and 0.52; Table 2, Fig. 2B and C). In cortical bone, although moderate correlations with Ct.vBMD in either the radius or tibia were seen in the simple correlation analysis (r = 0.34, 0.48), no correlations were seen in age-adjusted partial analysis. There were weak age-adjusted partial correlations with Ct.Th and Ct.Ar in the tibia (r = 0.39 and r = 0.35), however, virtually no correlations were seen with the cortical bone parameters for the radius.
Partial correlations for subgroups by sex and age
The age-adjusted partial correlation between QUS and DXA, the biochemical tests, and HR-pQCT are shown according to sex and age group in Table 3.
Moderate correlations were seen between SOS and aBMD of the proximal femur measured by DXA when men and women were examined separately (r = 0.43–0.48; Fig. 3A, B). Although a weak correlation was seen with aBMD of the lumbar spine in both men and women (r = 0.38, 0.36), no significant correlation was seen for either men or women in the 60–89 years age group.
No correlations were seen between SOS and the biochemical test parameters when the results were examined by sex and age group.
In the correlations with trabecular bone by HR-pQCT, SOS was moderately correlated with Tb.vBMD and Tb.BV/TV in the radius and tibia when men and women were examined separately (r = 0.41–0.53; Fig. 3C, D, E, and F). In particular, strong correlations were seen with Tb.vBMD and Tb.BV/TV of the radius in women aged 40–59 years (r = 0.64, 0.63).
In cortical bone, no correlations were seen for Ct.vBMD or Ct.Po in either the radius or tibia when the results were examined by sex and age group. Although weak correlations were seen with Ct.Th and Ct.Ar of the tibia when men and women were examined separately (r = 0.35–0.40), no or weak correlations were seen with Ct.Th and Ct.Ar of the tibia in women aged 60–89 years (r = 0.13–0.38).
Discussion
In this study, QUS, DXA, bone-related biochemical markers, and HR-pQCT were assessed in 480 men and women ranging in age from young to elderly, and the correlations between the measurement values were examined. To the best of our knowledge, no large studies have examined the relationships between QUS and HR-pQCT.
The results are summarized in Fig. 4. Although QUS was moderately correlated with aBMD of the lumbar spine in men and women aged 40–59 years (r = 0.47, 0.56), no correlation was seen in subjects aged ≥ 60 years. QUS was moderately correlated with aBMD of the proximal femur in men aged 40–59 years and in women of all age groups (r = 0.42–0.57).
QUS was moderately correlated with Tb.vBMD in the radius and tibia in men aged 40–59 years and in women of all age groups (r = 0.42–0.64). However, no correlations were seen with Ct.vBMD in the radius and tibia in men and women for any of the age groups. Although moderate correlations were seen with Ct.Th at the tibia in men aged 40–59 years and in women aged 20–59 (r = 0.44–0.50), no correlations were seen in those aged ≥ 60 years.
(1) QUS and DXA
Significant correlation between calcaneal QUS and femoral aBMD in this study (r = 0.31–0.57) indicates that calcaneal QUS is useful in screening for decreased aBMD of the femur. Previous studies have also found correlations between QUS and aBMD of the femur (r = 0.35–0.72) [9,10,11,12]. In addition, there have been numerous reports indicating that calcaneal QUS can be used to predict hip fractures [13,14,15,16,17]. The EPIDOS study examined 5662 women aged ≥ 75 years for an average of 2 years and found that the risk ratio for hip fracture was from 1.7 to 2.0 for every 1 SD decrease in the QUS measurement value [15]. Krieg et al. reported that, in postmenopausal women and men aged ≥ 65 years, QUS predicted fragility hip fractures and non-vertebral fractures independently of aBMD measured by DXA [16].
On the other hand, no correlation between calcaneal QUS and aBMD of the lumbar spine was seen in subjects aged ≥ 60 years. This might be attributed to the effect of spinal osteoarthritis and aortic calcification on aBMD of the lumbar spine in elderly subjects. Significant correlation only in men and women aged 40–59 years (r = 0.47, 0.56) suggests that calcaneal QUS is useful for early screening of decreased aBMD of the lumbar spine in individuals in middle age.
(2) QUS and biochemical tests
No correlations were seen between calcaneal QUS and bone turnover markers (TRACP-5b and P1NP) in this study. Predicting the status of bone turnover is difficult with calcaneal QUS. There is a 5-year longitudinal study in women aged ≥ 75 years examining the correlations between QUS and the annual percent change in bone turnover markers. The correlation coefficients were − 0.10 for both TRACP-5b and serum cross-linked C-telopeptide of type I collagen (CTX) and − 0.16 for osteocalcin [18].
In the present study, no correlation was seen between calcaneal QUS and 25 (OH) vitamin D or pentosidine. In a cross-sectional study investigating the relationship between calcaneal QUS and 25 (OH) vitamin D conducted by Kauppi et al. [19] the multiple regression coefficients obtained in a multiple regression analysis adjusted for factors such as height, weight, menopause status, and lifestyle were 0.18 for SOS and 0.07 for broadband ultrasound attenuation (BUA) in men and 0.11 for SOS and 0.07 for BUA in women. To the best of our knowledge, there have been no previous studies investigating the relationship between calcaneal QUS and pentosidine.
(3) QUS and HR-pQCT
Significant correlations between calcaneal QUS and Tb.vBMD in the radius and tibia (r = 0.32–0.64) indicate that QUS is useful for screening of deterioration of the trabecular bone microarchitecture in the extremities (Fig. 5). Many previous studies have reported postmenopausal women with a history of fragility fracture had low values of Tb.vBMD measured by HR-pQCT, [20,21,22,23,24] indicating that QUS has a potential ability to indirectly predict fragility fracture.
On the other hand, no correlations between calcaneal QUS and Ct.vBMD or Ct.Po in the radius and tibia indicate that current calcaneal QUS cannot predict deterioration in the cortical bone. Because the calcaneus consists largely of trabecular bone, calcaneal QUS may not truly reflect the status of cortical bone. In recent years, the axial transmission technique, which selectively evaluates cortical bone by ultrasound, has been investigated [25,26,27,28].
In the present study, calcaneal QUS was moderately correlated with Ct.Th of the tibia only in men and women aged 40–59 years (r = 0.49, 0.50). Calcaneal QUS may therefore be useful for early screening of decreased Ct.Th at the tibia in individuals in middle age. A previous study of HR-pQCT found that Ct.Th at the tibia was 15% lower in postmenopausal women with a history of bone fracture as compared with women with no such history [21].
Limitations
There are several limitations in the present study. First, this study recruited participants by distributing flyers to local communities. Therefore, self-selection bias and healthy worker bias were inevitable. Second, measurement values of calcaneal QUS can be affected by the temperature, size, and edema of the heel [29,30,31]. Measurement values of vitamin D are affected by season and diet. The data in the present study were collected from young and elderly individuals of varying body types without specifying the season or time when the examinations were performed. Consequently, these factors may have contributed to variability in the measurement values.
In conclusion, calcaneal QUS showed moderate correlations with trabecular vBMD and bone microarchitecture in the radius and tibia measured by HR-pQCT and with aBMD of the proximal femur measured by DXA. However, QUS showed no correlations with cortical vBMD or porosity in the radius and tibia and with bone turnover markers, 25 (OH) vitamin D, or pentosidine. QUS showed moderate correlations with cortical thickness in the tibia and with aBMD of the lumbar spine only in subjects aged 40–59 years.
References
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Soen S, Fukunaga M, Sugimoto T, Sone T, Fujiwara S, Endo N, Gorai I, Shiraki M, Hagino H, Hosoi T, Ohta H, Yoneda T, Tomomitsu T (2013) Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab 31:247–257
Burghardt AJ, Link TM, Majumdar S (2011) High-resolution computed tomography for clinical imaging of bone microarchitecture. Clin Orthop Relat Res 469:2179–2193
Manske SL, Zhu Y, Sandino C, Boyd SK (2015) Human trabecular bone microarchitecture can be assessed independently of density with second generation HR-pQCT. Bone 79:213–221
Samelson EJ, Broe KE, Xu H, Yang L, Boyd S et al (2019) Cortical and trabecular bone microarchitecture as an independent predictor of incident fracture risk in older women and men in the Bone Microarchitecture International Consortium (BoMIC): a prospective study. Lancet Diabetes Endocrinol 7:34–43
Saito M, Marumo K (2010) Collagen cross-links as a determinant of bone quality: a possible explanation for bone fragility in aging, osteoporosis, and diabetes mellitus. Osteoporos Int 21:195–214
Whittier DE, Boyd SK, Burghardt AJ, Paccou J, Ghasem-Zadeh A, Chapurlat R, Engelke K, Bouxsein ML (2020) Guidelines for the assessment of bone density and microarchitecture in vivo using high-resolution peripheral quantitative computed tomography. Osteoporos Int 31:1607–1627
Pialat J, Burghardt AJ, Sode M, Link TM, Majumdar S (2012) Visual grading of motion induced image degradation in high resolution peripheral computed tomography: Impact of image quality on measures of bone density and micro-architecture. Bone 50:111–118
Herd RJM, Blake GM, Miller CG, Parker JC, Fogelman I (1994) The ultrasonic assessment of osteopenia as defined by dual X-ray absorptiometry. Br J Radiol 67:631–635
Lees B, Stevenson JC (1993) Preliminary evaluation of a new ultrasound bone densitometer. Calcif Tissue Int 53:149–152
Rosenthall L, Tenenhouse A, Caminis J (1995) A correlative study of ultrasound calcaneal and dual-energy X-ray absorptiometry bone measurements of the lumbar spine and femur in 1000 women. Eur J Nucl Med 22:402–406
Schott AM, Hans D, Sornay-Rendu E, Delmas PD, Meunier PJ (1993) Ultrasound measurements on os calcis: Precision and age-related changes in a normal female population. Osteoporos Int 3:249–254
Bauer DC, Glüer CC, Cauley JA, Vogt TM, Ensrud KE, Genant HK, Black DM (1997) Broadband ultrasound attenuation predicts fractures strongly and independently of densitometry in older women. A prospective study. Study of osteoporotic fractures research group. Arch Intern Med 157:629–634
Fujiwara S, Sone T, Yamazaki K, Yoshimura N, Nakatsuka K, Masunari N, Fujita S, Kushida K, Fukunaga M (2005) Heel bone ultrasound predicts non-spine fracture in Japanese men and women. Osteoporos Int 16:2107–2112
Hans D, Dargent-Molina P, Schott A, Sebert J, Cormier C, Kotzki P, Delmas P, Pouilles J, Breart G, Meunier P (1996) Ultrasonographic heel measurements to predict hip fracture in elderly women: the EPIDOS prospective study. Lancet 348:511–514
Krieg M-A, Barkmann R, Gonnelli S, Stewart A, Bauer DC, Del Rio Barquero L, Kaufman JJ, Lorenc R, Miller PD, Olszynski WP, Poiana C, Schott A-M, Lewiecki EM, Hans D (2008) Quantitative ultrasound in the management of osteoporosis: the 2007 ISCD official positions. J Clin Densitom 11:163–187
Marín F, González-Macías J, Díez-Pérez A, Palma S, Delgado-Rodríguez M (2006) Relationship between bone quantitative ultrasound and fractures: a meta-analysis. J Bone Miner Res 21:1126–1135
Lenora J, Gerdhem P, Obrant KJ, Ivaska KK (2009) Bone turnover markers are correlated with quantitative ultrasound of the calcaneus: 5-year longitudinal data. Osteoporos Int 20:1225–1232
Kauppi M, Impivaara O, Mäki J, Heliövaara M, Marniemi J, Montonen J, Jula A (2009) Vitamin D status and common risk factors for bone fragility as determinants of quantitative ultrasound variables in a nationally representative population sample. Bone 45:119–124
Cohen A, Liu XS, Stein EM, McMahon DJ, Rogers HF, LeMaster J, Recker RR, Lappe JM, Guo XE, Shane E (2009) Bone microarchitecture and stiffness in premenopausal women with idiopathic osteoporosis. J Clin Endocrinol Metab 94:4351–4360
Stein EM, Liu XS, Nickolas TL, Cohen A, Thomas V, McMahon DJ, Zhang C, Yin PT, Cosman F, Nieves J, Guo XE, Shane E (2010) Abnormal microarchitecture and reduced stiffness at the radius and tibia in postmenopausal women with fractures. J Bone Miner Res 25:2572–2581
Sornay-Rendu E, Boutroy S, Duboeuf F, Chapurlat RD (2017) Bone microarchitecture assessed by HR-pQCT as predictor of fracture risk in postmenopausal women: the OFELY study. J Bone Miner Res 32:1243–1251
Vico L, Zouch M, Amirouche A, Frère D, Laroche N, Koller B, Laib A, Thomas T, Alexandre C (2008) High-resolution pQCT analysis at the distal radius and tibia discriminates patients with recent wrist and femoral neck fractures. J Bone Miner Res 23:1741–1750
Liu XS, Stein EM, Zhou B, Zhang CA, Nickolas TL, Cohen A, Thomas V, McMahon DJ, Cosman F, Nieves J, Shane E, Guo XE (2012) Individual trabecula segmentation (ITS)-based morphological analyses and microfinite element analysis of HR-pQCT images discriminate postmenopausal fragility fractures independent of DXA measurements. J Bone Miner Res 27:263–272
Chiba K, Suetoshi R, Cretin D, Arai T, Kawajiri T, Okayama A, Tsuji S, Okazaki N, Osaki M, Yoh K (2021) Development of a QUS device to evaluate deterioration of cortical bone: verification by HR-pQCT and measurements in healthy individuals and dialysis patients. J Clin Densitom 24:94–105
Muller M, Moilanen P, Bossy E, Nicholson P, Kilappa V, Timonen J, Talmant M, Cheng S, Laugier P (2005) Comparison of three ultrasonic axial transmission methods for bone assessment. Ultrasound Med Biol 31:633–642
Schneider J, Ramiandrisoa D, Armbrecht G, Ritter Z, Felsenberg D, Raum K, Minonzio J-G (2019) In vivo measurements of cortical thickness and porosity at the proximal third of the tibia using guided waves: comparison with site-matched peripheral quantitative computed tomography and distal high-resolution peripheral quantitative computed tomography. Ultrasound Med Biol 45:1234–1242
Tatarinov A, Egorov V, Sarvazyan N, Sarvazyan A (2014) Multi-frequency axial transmission bone ultrasonometer. Ultrasonics 54:1162–1169
Chappard C, Berger G, Roux C, Laugier P (1999) Ultrasound measurement on the calcaneus: influence of immersion time and rotation of the foot. Osteoporos Int 9:318–326
Iki M, Kajita E, Mitamura S, Nishino H, Yamagami T, Nagahama N (1999) Precision of quantitative ultrasound measurement of the heel bone and effects of ambient temperature on the parameters. Osteoporos Int 10:462–467
Paggiosi MA, Blumsohn A, Barkmann R, Eastell R (2005) Effect of temperature on the longitudinal variability of quantitative ultrasound variables. J Clin Densitom 8:436–444
Acknowledgements
We would like to thank Mitsuru Doi, Choko Kondo, Kazuaki Yokota for collecting data, Rika Arai, Rena Komatsubara, Midori Motoi, Miki Sakimoto, Yukari Hayashida, Arisa Fujiwara, Noriko Yoshitake, Yoko Sato, Naoko Uchida, and Kayoko Ota for coordinating participants and managing data, and Mika Kono and Yasue Michikoshi for performing DXA analysis.
Author information
Authors and Affiliations
Contributions
Study design: KC; data acquisition: RN and NO; data analysis: RN; statistical analysis: RN; data interpretation: RN, KC, and MO; drafting of the manuscript: RN and KC; revision of the manuscript content: AY, MT, and MO.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Niimi, R., Chiba, K., Okazaki, N. et al. Relationships between QUS and HR-pQCT, DXA, and bone turnover markers. J Bone Miner Metab 40, 790–800 (2022). https://doi.org/10.1007/s00774-022-01346-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-022-01346-2